Abstract
Background
Ocular trauma is a leading cause of vision loss. Penetrating ocular injury is a major type of open globe injury(OGI), while its epidemiology and clinical characteristics are still uncertain. The aim of this study is to reveal the prevalence and prognostic factors of penetrating ocular injury in the Shandong province.
Methods
A retrospective study of penetrating ocular injury was performed at the Second Hospital of Shandong University, from January 2010 to December 2019. Demographic information, injury causes, ocular trauma types, and initial and final visual acuity(VA) were analyzed. To obtain more precise characteristics of penetrating injury, the eye global was divided into three zones and analyzed.
Results
Among 210 OGI, there are 83 penetrating injuries which account for 39.5% of all. In addition, the final VA of 59 penetrating injuries recovered to 0.1 or better, which possesses the highest frequency among OGI. In order to research the relationship between the wound location and the final VA, we took 74 cases of penetrating injuries without retina or optic nerve damage for analysis. Results show that 62 were male and 12 were female. The average age was 36.01 ± 14.15. The most frequent occupation is the worker followed by the peasant. Statistics show that there is an obvious deviation in the Ocular trauma score (OTS) predicting the final VA and the actual final VA in the 45–65 score group (p < 0.05). Results suggest that the commonest penetrating injury zone is zone III (32 cases, 43.8%). Zone III, which is farthest from the center of the visual axis, has the largest improvement of the final VA (p = 0.0001). On the contrary, there is no statistical difference in the visual improvement in zone I and zone I + II that involves the injury of the central visual axis.
Conclusion
This study describes the epidemiology and clinical characteristics of patients hospitalized for penetrating ocular injury without retina damage in Shandong province. It can be concluded that larger size and closer location to the visual axis of damage are accompanied by worse prognosis improvement. The study provides a better understanding of the disease and enlightenment for the prediction of visual prognosis.
Similar content being viewed by others
Background
Ocular trauma is a major cause of vision loss and blindness [1, 2]. Around the world, there are approximately 55 million patients suffering from ocular trauma each year, and about 1.6 million of them will result in blindness finally [3, 4]. Mechanical ocular trauma could be subdivided into open and closed globe injuries by the Birmingham Eye Trauma Terminology (BETT) [5,6,7]. OGI is a major cause of visual impairment among all kinds of ocular injuries [8,9,10]. Penetrating ocular injuries is a major type of OGI that can cause severe visual impairment [1, 11]. The epidemiological statistics of penetrating ocular trauma have been reported in developed countries such as the USA [3, 12,13,14], Europe [15] and Australia [16], and some develo** countries including India, Iran, and Egypt [9,10,11,12]. Although the statistical data on ocular trauma in several southern provinces of China are available, the statistics on ocular trauma in China are still insufficient [1, 4, 17].
Assessment of visual functions of penetrating wounds is important for patient management, surgical operation, and the prediction of the prognosis of penetrating injury. Kuhn et al. [18] developed the prognostic OTS model to predict the visual outcome of patients after ocular trauma. The initial vision, eyeball rupture, endophthalmitis, eyeball perforation, retinal detachment, and presence/absence of relative afferent pupillary defects (RAPD) are identified as the main influencing factors. OTS is widely used to predict the prognosis by summing up the scores of the six factors mentioned above. Schmidt et al. [19] proposed another prognostic model, the classification and regression tree (CART), to predict visual function in patients after OGI. However, there are several limitations in those methods: both models have been proposed for more than 10 years; the size and location of the wound are ignored by those methods; some pathological factors or symptoms such as endophthalmitis and RAPD are difficult to evaluate at the early stage of ocular trauma [4].
Pure penetrating injury without retina and optic nerve damage usually results in better final VA [20], so the assessment of visual functions of wounds is important for patient management and the prediction of the prognosis of such diseases. Therefore, we collected and analyzed the data of penetrating ocular injury, in order to illuminate the relationship between the wound location and the final VA and provide a better understanding of the disease and enlightenment for the prediction of visual prognosis.
Methods
The research was approved by the Ethics Committee of our Institute and followed the guidance of the Helsinki Declaration. Data were collected from all patients with a principal diagnosis of ocular trauma (ICD code: S05.600) admitted to the Department of Ophthalmology in the Second Hospital of Shandong University, **an, Shandong province, China, from January 2010 to December 2019. All cases of ocular trauma were diagnosed according to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Ocular trauma cases were searched using ICD-10 code S05 in the electronic medical records.
Aim
The aim of this study is to illuminate the prevalence and potential factors that affects the prognosis of patients with penetrating ocular injury in Shandong province.
Study design and patients
Penetrating ocular injury is specifically divided into three zones by the location of the global injury in this study. The center of 3 mm in diameter of the cornea is defined as zone I, and the posterior 1.5 mm next to zone I is defined as zone II. Furthermore, the border of zone II to 6 mm posterior of the corneoscleral limbus is defined as zone III. The number of cases, initial VA, and final VA of each zone are collected and analyzed respectively. Ocular Trauma Score (OTS) is calculated to assess the extent of the globe injury. Final VA is obtained after the 6-month follow-up.
The OGI and closed-global injury are distinguished based on the BETT [16] and the degree of injury is classified according to Ocular Trauma Classification System (OTCS) [17]. The types of OGI are classified as penetrating injury, intraocular foreign body injury, perforating injury, and global rupture. Visual acuity is classified into five grades: NLP (no light perception), LP/ HM (light perception/ hand move),0.005–0.095, 0.1–0.4, and ≥ 0.5 [21].
Patients who meet the following criteria are included in this study. (1) Patients with penetrating ocular injury. (2) Patients who could comply with the vision examination. (3) Patients who did not suffer from any eye diseases before.
Meanwhile, patients who meet the following criteria are excluded from this study. (1) Patients who can not comply with the ophthalmic examination. (2) Patients who can not comply with the doctor's advice and follow-up. (3) Patients who have previous treatment history of eye disease. (4) Patients suffering trauma that affected the retina or optic nerve.
Details of all patients are collected from the medical records system including age, gender, occupational classification, place of residence, cause and location of ocular trauma, classification and distribution of ocular trauma, and initial and final VA. The final visual acuity recovered to 0.1 or better was defined as a success [8]. All the data are analyzed by grou**.
Statistical analysis
Statistical analysis of all quantitative data including descriptive Statistical analyses were performed using SPSS (Version 27.0; IBM Corporation, Armonk, NY, USA). Demographics and patient characteristics are reported as percentages and cases in each group and include type of ocular trauma, distribution of age, initial VA, OTS predicted VA, corneal partition of the wound. P < 0.05 was considered a statistically significant difference.
Kruskal–Wallis test was used to compare differences in postoperative VA in patients with different types of eye trauma. The difference analysis of preoperative and postoperative VA in patients with penetrating eye injuries that do not injure the retina were performed using Wilcoxon signed-rank test. Wilcoxon signed-rank test was used to evaluate differences in OTS prediction of VA and actual final VA, the method was also been used to compare preoperative and postoperative VA improvement in different corneal partitions.
Results
Penetrating ocular injuries possess a high proportion and fine final VA in all open-globe injuries
A total of 210 open-globe injuries were hospitalized from 1 January 2010 to 31 December 2019 at the Second Hospital of Shandong University. Among the 210 open-globe injuries, as shown in Table 1, rupture injury demonstrated the highest frequency (119 cases, 56.7%) followed by penetrating injury (83 cases, 39.5%) and intraocular foreign body (IOFB) (8 cases, 3.8%). No perforating cases were exhibited in our study. It was noticeable that 59 cases of 83 penetrating injuries (71.1%) could improve their final VA to 0.1 or better, which was higher than rupture (9 cases, 7.6%) (p = 0.000, < 0.05). Due to the high proportion and fine final VA of penetrating injuries, this type of ocular injury was selected for further study.
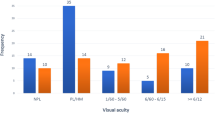
The final VA penetrating injuries improved significantly compared with the initial VA
The frequency and the percentage of the final VA and initial VA of penetrating injuries were shown in Table 2. There was a significantly different distribution between the initial VA and final VA (p = 0.0001, p < 0.05). LP/HM accounted for the highest proportion in initial VA (30 cases, 40.54%). After medical treatment, the proportion of LP/HM in final VA was reduced to 6.76% (5 cases), and a large proportion of patients demonstrated a best-corrected final VA exceeding 0.1(59 cases, 79.73%). Moreover, 41 cases of those patients could improve the final VA to 0.5. It could be concluded that the final VA penetrating injuries improved significantly compared with the initial VA.
Demographics and characteristics of hospitalized penetrating ocular injuries over 10 years period
Then, the demographics and characteristics of penetrating injuries without optic nerve and retina damage were analyzed (Table 3). Among 74 patients taken into our study, there were no binocular injury case in our study, and no significant difference in laterality with a ratio of 44.6:55.4 between the left and right eyes (Table 3). The ratio between the male and female patients attains 5.17:1, namely, 62 (83.8%) were male and 12 (16.2%) were female. The average age was 36.01 ± 14.15. The age distribution showed that the peak occurrence of ocular trauma occurred in the 21–30 age group (21 cases, 28.4%), followed by the 31–40 age group (20 cases, 27%), 41–50 age group (11 cases, 14.9%) and 51–60 age group (11 cases, 14.9%) in sequence. Of these 74 patients with penetrating ocular injury, the most common occupation was worker (48 cases, 64.86%), followed by peasant (19 cases, 25.28%). Ocular trauma occurred more frequently in rural areas (42 cases, 57%) than in urban areas (32 cases, 43%). Most of the penetrating injuries occurred during working (54 cases, 72.97%).
The final VA predicted by OTS had a deviation compared with the actual final VA in the OTS score 45–65 group at the last follow-up
To examine whether OTS could be applied to the VA prediction of penetrating ocular injury, we compared the OTS-predicted final VA with the actual final VA.
Results of statistical analysis showed that OTS predicted final VA was consistent with actual VA in the OTS score 66–80 group (p = 0.108, p > 0.05) and 81–91 group (p = 1, p > 0.05) respectively. But there was a large deviation in the prediction of the OTS score 45–65 group, with 29 cases, 39.2% of all patients (p = 0.001, p < 0.05). In this group, final VA predicted by the OTS method were NLP (28%), LP-HM (26%), 0.005–0.095 (18%), 0.1–0.4 (13%), and > 0.5 (15%) respectively, while the actual final VA were NLP (3.4%), LP-HM (3.8%), 0.005–0.095(24.1%), 0.1–0.4(13.8%) and ≥ 0.5(44.8%) respectively. There are no patients in the 0–44 group and 92–100 group, so the two groups couldn’t be analyzed (Table 4).
Larger size and closer location to the visual axis of damage accompany worse improvement
To better understand the character of penetrating ocular injury, we divided the anterior ocular into three zones in this study specifically. The center of 3 mm in diameter of the cornea was defined as zone I, and the posterior 1.5 mm next to zone I was defined as zone II. Furthermore, the border of zone II to 6 mm posterior of the corneoscleral limbus was defined as zone III.
Results show that zone III was the commonest site being wounded (33 cases, 44.6%), followed by zone II + III (13 cases, 17.6%), zone I + II + III (13 cases, 17.6%), zone II (7 cases, 9.5%), zone I (5 cases, 6.8%) and zone I + II (3 cases, 4%) (Fig. 1a).
The distribution of final VA in different zones of all cases was shown in Fig. 1b. Furthermore, we analyzed the final VA after therapy better than 0.1 and defined it as success. As shown in Table 5, wound location in zone I (5/5 = 100%) owned the highest rate of success, followed by zone III (30/33 = 90.9%), zone II (6/7 = 85.7%), zone II + III (6/13 = 46%), and zone I + II + III (8/13 = 61.5%), while the zone with the worst final VA was zone I + II (1/3 = 33.3%). However, statistical results of VA improvement showed that there were statistically significant between the initial VA and the final VA in Zone II (p = 0.003), zone III (p = 0.0001), zone II + III (p = 0.016), and zone I + II + III (p = 0.0004) (Table 5). On the contrary, there was no statistical difference in the visual improvement in zone I and zone I + II that involves the injury of the central visual axis. It could be concluded that zone III, the commonest site being wounded, had the largest improvement of final VA. Larger size and closer location to the visual axis of damage accompany worse improvement.
Discussion
The penetrating injury is a common type of OGI [1, 11]. This retrospective study presents data concerning the prevalence and clinical characteristics of patients who were hospitalized for penetrating ocular injuries in the second hospital of Shandong University.
Penetrating ocular injury is important in OGI
According to the results, we found that penetrating ocular injuries possess a high proportion (83 cases, 39.5%) and highest proportion (59 cases, 71.1%) of final VA > 0.1 among OGI (p < 0.05) (Table 1). This is also in accord with previous studies which reported that penetrating injuries usually preserved better final VA than IOFB injuries after medical treatment [4]. Due to the full-thickness injury of the cornea or sclera induced by blunt trauma, rupture injuries usually trigger severe complications and result in a worse prognosis than penetrating injuries. Since IOFB injuries are often accompanied by endophthalmitis and retinal damage after ocular trauma, the final VA of IOFB injuries is usually worse than penetrating injuries.
Due to the high proportion and fine final VA, penetrating injuries without retina and optic nerve damage are selected for further research with the aim to provide a better understanding of the disease and enlightenment for the prediction of visual prognosis.
Demographics
Our study demonstrates that age and gender are strongly associated with the incidence of penetrating injury. The rates of penetrating injury were higher in patients ranging from the 21–40 age group, especially in males. These findings are consistent with other studies which reported that ocular trauma often occurred in the dominant labor force ranging from 30–50 years old in China [17, 22, 23].
As involved in our study, the workplace is the most frequent place of injury. The incidence of work-related ocular trauma (54 cases, 72.97%) revealed in our research is conform to results from previous research, which reported the range of work-related ocular trauma is from 25.4% to 73.7% [24,25,26]. Since more and more peasants turning into migrant workers, the incidence of penetrating injuries may increase furthermore [1]. The main contributing factor to the higher proportion of work-related ocular trauma is the workers’ lack of safety awareness. Therefore, safety awareness must be cultivated, and workers must be educated to effectively protect their eyes during work [17, 27, 28].
The final VA of penetrating injuries predicted by OTS had obvious deviation compared with the actual final VA in OTS score 45–65 group
We compared the OTS-predicted final VA with the actual final VA to evaluate the accuracy of the OTS method. Of the three groups being analyzed, OTS predicting final VA is consistent with actual VA in the OTS score 66–80 group and 81–91 group respectively, but there is a large deviation in 45–65 group (p = 0.001, p < 0.05). The OTS method is not accurate when used to evaluate the final VA of penetrating injury. As reported in Korean research, the positive predictive value of OTS in OGI is as low as 75.3% [8, 29]. The following limitations may contribute to the deviation. (1) The OTS method has been more than 20 years since it was developed. (2) Some factors are difficult to describe such as RAPD, especially for OGI patients with pain and scare brought by the ocular trauma. (3) The location and size of the wound which are regarded as important factors in descript the final VA of OGI were not considered in the OTS method [4].
The final VA of penetrating injury related to the wound size and location
To better understand the character of penetrating ocular injury, we divided the anterior ocular into three zones in this study specifically. Zone III was the most popular affected area in our study. Besides the largest area among the three zones, escape instinct is a possible reason that most injuries are away from the center of the visual axis.
The success rates of the single zone (zones I, II, and III) are 100%, 85.7%, and 90.9% respectively. Slight astigmatism triggered by the small size of the scar located in one single zone may attribute to the final VA outcome mentioned above.
However, the success rates in patients with extended injury in zone I + II, II + III, and zone I + II + III are 33.3%, 46%, and 61.5% respectively, which is worse than that in a single zone. In terms of patients involved in zone I + II, the proportion of success is the lowest (33.3%) of all the zones. Because the injuries involved in multi-zone are usually large, the visual axis is frequently blocked by large corneal scars, and the VA is often affected by severe astigmatism triggered by large scars.
Statistical analysis shows that there are significant differences between the initial VA and the final VA in zone II, zone III, zone II + III, and zone I + II + III. Since the location of zone I is close to the visual axis, the affection of the scar to the transparency of the central corneal area and astigmatism near the central area may contribute to the weak improvement of injuries involved in zone I. However, for the injury in zone I + II + III which has a relatively large wound, astigmatism near the central area can be ameliorated by adjusting the position and tightness of the suture. It may account for the improvement of final VA in zone I + II + III while the detailed reason requires further investigations.
Overall, we demonstrated that the final VA of penetrating injury is usually related to the wound size and location. Larger size and closer location to the visual axis of damage accompany a worse prognosis.
Shortcomings
In order to study the effect of simple corneoscleral injury on visual acuity, we excluded cases with retinal or optic nerve damage, vitreous hemorrhage, endophthalmitis, so the number of cases taking into statistical analysis ultimately is not abundant enough.
Since the injury site of ocular trauma involves wide range, we systematically divided the patient's injury range into different zones and analysis the visual acuity of different zones. Due to the detailed corneal divisions, the cases falling into each zone is a little small, so the sensitivity and specificity of OTS score could not be statistically analyzed.
In the further study, we intent to cooperate with other hospitals to enlarge the sample size and verify our conclusion about the prognosis of penetrating ocular injury in this manuscript.
Conclusion
This study describes the epidemiology and clinical characteristics of patients hospitalized for penetrating ocular injury without retina and optic nerve damage in Shandong province. Penetrating ocular injuries possess a high proportion and better final VA among all types of OGI. Age, gender, and profession are strongly associated with the incidence of penetrating injury. Moreover, larger size and closer location to the visual axis of damage accompany the worse prognosis. The epidemiological investigation and detailed division of penetrating ocular injury provide a better understanding of the disease and enlightenment for the prediction of visual prognosis.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Abbreviations
- BETT:
-
Birmingham Eye Trauma Terminology
- CART:
-
Classification and regression tree
- IOFB:
-
Intraocular foreign body
- LP/ HM:
-
Light perception/ hand move
- NLP:
-
No light perception
- OGI:
-
Open-globe injury
- OTCS:
-
Ocular Trauma Classification System
- OTS:
-
Ocular trauma score
- RAPD:
-
Relative afferent pupillary defects
- VA:
-
Visual acuity
References
Cao H, Li L, Zhang M. Epidemiology of patients hospitalized for ocular trauma in the Chaoshan region of China, 2001–2010. PLoS ONE. 2012;7(10): e48377.
Moharana B, Gupta R, Sharma B. Commentary: Open globe injury: The Indian perspective. Indian J Ophthalmol. 2022;70(3):864–5.
Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5(3):143–69.
Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South-Central China. Acta Ophthalmol. 2017;95(6):e503–10.
Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol. 1996;234(6):399–403.
Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham Eye Trauma Terminology system (BETT). J Fr Ophtalmol. 2004;27(2):206–10.
Kuhn F, Morris R. A quarter of a century of the Birmingham Eye Trauma Terminology (BETT) system. Graefes Arch Clin Exp Ophthalmol. 2021;259(10):2867–8.
Choi S, Park J, Park S, Byon I, Choi HY. Establishment of a prediction tool for ocular trauma patients with machine learning algorithm. Int J Ophthalmol. 2021;14(12):1941–9.
Gulati S, Hanebrink KA, Henry M, Munro M, Chan RVP, Edward DP. Open globe injury and intraocular foreign body following crossbow-related penetrating ocular trauma. Am J Ophthalmol Case Rep. 2022;26: 101441.
Vingopoulos F, Wang Y, Grob S, Li CYL, Eliott D, Kim LA, Vavvas DG, Miller JB. Open Globe Injury with Intraocular Foreign Body. J Vitreoretin Dis. 2021;5(4):288–94.
Silva-Filho GV, Morgan-Kanada AM, Kasahara N. Predictive values of the Pediatric Penetrating Ocular Trauma Score and the Toddler/Infant Ocular Trauma Score in Brazilian children with open globe injury. Clin Exp Emerg Med. 2022;9(1):41–6.
Ramirez DA, Porco TC, Lietman TM, Keenan JD. Ocular Injury in United States Emergency Departments: Seasonality and Annual Trends Estimated from a Nationally Representative Dataset. Am J Ophthalmol. 2018;191:149–55.
Haring RS, Canner JK, Haider AH, Schneider EB. Ocular injury in the United States: Emergency department visits from 2006–2011. Injury. 2016;47(1):104–8.
D’Antone V, Florez DCP, Garcia CJL, Manrique FMC, Barbosa NL. Epidemiological findings of childhood ocular trauma in a public hospital in Colombia. BMC Ophthalmol. 2021;21(1):248.
Belmonte-Grau M, Garrido-Ceca G, Marticorena-Alvarez P. Ocular trauma in an urban Spanish population: epidemiology and visual outcome. Int J Ophthalmol. 2021;14(9):1327–33.
Desai P, Morris DS, Minassian DC, MacEwen CJ. Trends in serious ocular trauma in Scotland. Eye (Lond). 2015;29(5):611–8.
Cai M, Zhang J. Epidemiological Characteristics of Work-Related Ocular Trauma in Southwest Region of China. Int J Environ Res Public Health. 2015;12(8):9864–75.
Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15(2):163–165, vi.
Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115(1):202–9.
Fujikawa A, Mohamed YH, Kinoshita H, Matsumoto M, Uematsu M, Tsuiki E, Suzuma K, Kitaoka T. Visual outcomes and prognostic factors in open-globe injuries. BMC Ophthalmol. 2018;18(1):138.
Puodziuviene E, Valeisaite G, Zemaitiene R. Clinical Characteristics, Visual Outcomes, and Prognostic Factors of Open Globe Injuries. Medicina. 2021;57:1198. https://doi.org/10.3390/medicina57111198.
Wu M, Ye J. Hospitalized eye injury in a Chinese urban population: a 7-year retrospective analysis. Int J Ophthalmol. 2010;3(2):179–81.
Qi Y, Zhang FY, Peng GH, Zhu Y, Wan GM, Wang WZ, Ma J, Ren SJ. Characteristics and visual outcomes of patients hospitalized for ocular trauma in central China: 2006–2011. Int J Ophthalmol. 2015;8(1):162–8.
Ho CK, Yen YL, Chang CH, Chiang HC, Shen YY, Chang PY. Epidemiologic study on work-related eye injuries in Kaohsiung Taiwan. Kaohsiung J Med Sci. 2007;23(9):463–9.
Limbu B, Moore G, Marvasti AH, Poole ME, Saiju R. Work Related Ocular Injury: Nepal. Nepal J Ophthalmol. 2018;10(19):47–56.
Sahraravand A, Haavisto AK, Puska P, Leivo T. Work tool-related eye injuries: Helsinki Ocular Trauma Study. Int Ophthalmol. 2020;40(3):753–61.
Lubis RR, Limanto V, Putri R, Lubis AN, Arrasyid NK. Epidemiological Characteristics of Work-Related Ocular Trauma among the Carpenters in Medan, Indonesia. Open Access Maced J Med Sci. 2018;6(11):2119–22.
Mansouri MR, Hosseini M, Mohebi M, Alipour F, Mehrdad R. Work-related eye injury: the main cause of ocular trauma in Iran. Eur J Ophthalmol. 2010;20(4):770–5.
Shrestha SM, Anthony CL, Justin GA, Thapa M, Shrestha JB, Khatri A, Hoskin AK, Agrawal R. Factors affecting final functional outcomes in open-globe injuries and use of ocular trauma score as a predictive tool in Nepalese population. BMC Ophthalmol. 2021;21(1):69.
Acknowledgements
We are grateful to Guoyong Ding of Shandong Provincial Hospital Affiliated with Shandong First Medical University for the guidance on the statistical methods of this study and Huandi Liu of The Second Hospital of Shandong University for the help in the collection of electronic medical records in this study.
Funding
The present study was supported by the National Natural Science Foundation of China (no.81873677), and the Shandong Natural Science Foundation (no. ZR2020QH147).
Author information
Authors and Affiliations
Contributions
XF.Z and HZ were responsible for the initial idea and study design. The draft of this manuscript was written by XG and revised by QQ. Z and FW. XW. Li, CL. Ma, and YX. L promoted the study, including examination at the last follow-up, data collection, and data analysis. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to particate
The research was approved by the Ethics Committee of the second hospital of Shandong University and followed the guidance of the Helsinki Declaration. Informed consent was obtained from the participants or a parent of the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, X., Zhang, Q., Wang, F. et al. Wound size and location affect the prognosis of penetrating ocular injury. BMC Ophthalmol 23, 257 (2023). https://doi.org/10.1186/s12886-023-03015-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-03015-y