Abstract
Background
The aim of this study was to report the clinical profile and outcomes of retinal pigment epithelial detachment (PED) in Vogt-Koyanagi-Harada (VKH) disease, and to evaluate the correlation between PED and the subsequent development of central serous chorioretinopathy (CSC) throughout the whole corticosteroid treatment course.
Methods
The retrospective study enrolled a total of 470 eyes with VKH, and 12 eyes with VKH and PED were recruited. Patients were divided into two groups according to the CSC onset or not throughout the whole course (the CSC group and non-CSC group). Best-corrected visual acuity (BCVA) improvement, and PED angle (PEDA, the angle between the two lines of the vertex of the lifted retinal pigment epithelium to the two edge points of the Bruch membrane) were compared between the two groups.
Results
CSC developed at the site of the PED in 5 of the 12 eyes with PED, while in the remaining 7 eyes PED gradually resolved following therapy. The prevalence of PED and CSC in VKH was 2.55% (12/470) and 1.06% (5/470), respectively. BCVA improvement in the non-CSC group was greater than that in the CSC group, but without a statistical difference (P = 0.25). PEDA was significantly smaller in the CSC group than in the non-CSC group (P = 0.03).
Conclusion
PEDA is an ideal parameter to reflect hydrostatic pressure and stretches for RPE. As PED predisposes to the development of CSC in selected VKH eyes, PEDA may be a valuable predictive factor for the development of classic CSC in VKH cases.
Similar content being viewed by others
Background
Vogt-Koyanagi-Harada (VKH) disease is an immune-mediated multisystem disorder characterized by bilateral panuveitis, neurological (meningeal), auditory, and dermatological manifestations [1]. The hallmarks of posterior ocular manifestations at the acute stage are bilateral multiple exudative retinal detachments (ERD), optic disc swelling, and choroid thickening [1]. Multimodal imaging examinations, such as fundus fluorescein angiography (FFA), indocyanine green angiography (ICGA), and optical coherence tomography (OCT), aid in diagnosis and change evaluations [2]. The mainstream therapeutic regimen is a rapid and aggressive high-dose systemic corticosteroid to suppress acute intraocular inflammation, followed by gradual tapering. Timely and aggressive systemic corticosteroids are the cornerstone of preliminary therapy. The subsequent oral corticosteroid should be gradually tapered off and sustained for at least 6 months to avoid a high recurrence rate and poor prognosis, at the same time, the initiation of immunosuppressive agents (such as azathioprine [AZA], cyclosporin A [CsA], mycophenolate mofetil [MMF]) has proven to be a great complement for corticosteroids in controlling the inflammation [1,2,3,4]. Moreover, some newer biologic agents (such as rituximab, infliximab, interferon alpha 2A, and adalimumab [ADA]) have been effective in small sample size of cases with poor response to both corticosteroid and immunosuppressive agents [1,2,3].
The anatomical separation between the basement membrane of the retinal pigment epithelium (RPE) and the inner collagenous layer of the Bruch membrane is known as pigment epithelial detachment (PED) [5]. Isolated serous PED is frequently associated with choroidal hyperpermeability on ICGA and is regarded as a transitional stage between pachychoroid and classic central serous chorioretinopathy (CSC) [6]. Nonetheless, serous PED is an unusual finding in acute VKH characterized by choroidal thickening [7]. Although VKH and CSC diseases are different in nature, they occasionally require differentiation because they share some common clinical features, including bullous serous retinal detachment on OCT and multifocal leakage on FFA. Sometimes CSCs can also develop in VKH patients [8]. Early diagnosis of CSC in VKH patients is important because the therapeutic strategies for these two diseases are contradictory, and adjustment of treatment is imperative once CSC occurs.
Few studies have investigated the clinical value of PED in VKH and its relationship with subsequent CSC development. Therefore, we conducted the first longitudinal analysis to describe the outcomes of PED in VKH cases and searched for a simple predictive factor for different clinical prognoses based on the PED contour. Hence, we hypothesized that the contour of PED between the lifted edge of the RPE and Bruch membrane could be a predictor for subsequent development of CSC in VKH cases with corticosteroid treatment.
Methods
Institutional review board approval (No.2020KY (L)-37) was obtained from Tian** Medical University Eye Hospital (TMUEH) for the retrospective review of clinical records for all VKH patients at the Uveitis & Ocular Immune Department from August 1, 2011, to August 31, 2020. Informed consent was exempt as it was a retrospective study. This research adhered to the tenets of the Declaration of Helsinki. According to the 2001 diagnostic criteria [9], all VKH patients were identified via medical records and were included if OCT presented well-demarcated, abrupt elevations of the RPE with a homogeneously hyporeflective sub-RPE space and diagnosed with PED by two different ophthalmologists. The retrieved data included demographics, the best-corrected visual acuity (BCVA) at baseline and every follow-up visit, details of the ocular and systemic examination, imaging details of OCT scans, FFA and ICGA, therapeutic regimen, treatment response and complications, long-term anatomical outcomes, and clinical outcomes.
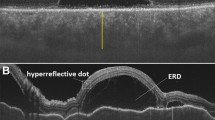
We conceived PED angle (PEDA) based on the contour of PED as a useful parameter for predicting the prognosis of PED, under the enlightenment of the macular hole angle [10]. The PEDA was defined as the angle between the two lines of the vertex of the lifted RPE to the two edge points of the Bruch membrane (Fig. 1). PEDA was measured using Digimizer software (Version 5.4.4). For standardization purposes, the average of three measurements was used for analysis. Eyes were classified into two groups: CSC and non-CSC groups. The PEDA and clinical outcomes for each group were evaluated and recorded. The CSC diagnosis criteria in our VKH patients included: there was no active inflammation in both anterior chamber and vitreous cavity when ERD reoccurred; FFA disclosed the intense leakage at the RPE level with an “ink-blot’’ or “smokestack” pattern, which was colocalized with the neurosensory retinal detachment on OCT; slight hyperfluorescence and leakage was allowed on FFA, due to the incomplete resolution of intraocular inflammation in VKH; the VKH patient responded well to the corticosteroid treatment before CSC development, and the neurosensory retinal detachment resulted from CSC could subside with the cessation of corticosteroid therapy.
The SPSS program was used for statistical analysis. BCVA measurements were transferred to the logarithm of the minimum resolution angle (LogMAR) for statistical analysis. Descriptive statistics included mean and standard deviation for normally distributed continuous variables as well as median and range for non-normally distributed continuous variables. Owing to the small sample sizes in our study, all statistical analyses were conducted using the nonparametric Wilcoxon (paired samples) or Mann–Whitney (independent samples) signed rank sum tests. Statistical significance was set at P < 0.05.
Results
A total of 470 eyes (235 patients) with VKH were identified, 44 patients were diagnosed with complete VKH disease, 144 with incomplete VKH, and 77 with probable VKH. The population consisted of 128 female (54.5%) and 107 male (45.5%) patients aged a mean of 46.7 ± 15.6 years (range: 7–85). The most frequent extraocular finding was meningismus. The characteristic fundus manifestations were multiple ERDs at the posterior pole and optic edema. Auxiliary examinations were used to provide aid for diagnosis and evaluate relevant changes in eyes. FFA revealed multifocal regions of pinpoint leakage, pooling, and staining of optic disc. ICGA disclosed numerous hyperfluorescent areas and hypofluorescent dark dots. OCT presented serous retinal detachment with choroidal thickening, and the typical manifestations of RPE were undulating RPE line and RPE bumps. Based on empirical findings, first choice of treatment was systemic high dose corticosteroids. For those patients who were intolerant or resistant to corticosteroids, immunosuppressive agents and/or biological agents were employed to suppress the ocular inflammation.
A total of 12 eyes (10 patients) developed serous PED (12/470, 2.55%), it occurred in 10 eyes (8 patients) at the onset of VKH, and in other 2 eyes (2 patients) during the treatment follow-up. The demographic and clinical data of the 12 eyes (10 patients) are summarized in Tables 1 and 2. In the 10 eyes with PED occurring at the onset of the disease, it gradually resolved in 6 eyes, and developed into CSC in the remaining 4 eyes. Among the 4 eyes with CSC development, the CSC occurred after the resolution of inflammation in both anterior chamber and vitreous cavity in two eyes (case 5 and case 9), on the other hand, the CSC were considered to occur simultaneously with initial PED and VKH in another two eyes (bilateral eyes of case 10). Over the course of systemic corticosteroid therapy, there were two VKH eyes developed PED, but it gradually resolved in one eye and developed into CSC in the other one. Overall, fundus photography, OCT, and FFA images indicated that 5 eyes of 4 VKH patients with PED experienced superimposed CSC (5/470, 1.06%). Interestingly, OCT revealed that the all the neurosensory retinal detachments of CSC colocalized with PEDs; meanwhile, the microrips of RPE at the margin of PED was clearly seen in the bilateral eyes of case 10, in which the CSC, PED and VKH were considered to occur simultaneously.
We divided the 12 eyes into two groups according to whether CSC developed or not: the CSC group and the non-CSC group. The average time taken between PED and CSC occurrence was 2.2 ± 2.5 months (range 0–6 months). Upon CSC diagnosis, corticosteroid was rapidly tapered off, and alternative therapies were applied, including immunosuppressants and biologics (AZA, CsA, MMF, ADA), continuous-wave laser photocoagulation for outside foveal leakage, and subthreshold micropulse laser photocoagulation (577 nm) for foveal leakage. After the treatment was adjusted, all PED and subretinal fluid resolved completely, except for the PED in case 5.
BCVA with a statistical difference was observed between the initial visit and the last follow-up in the 12 eyes (P = 0.02) (Table 1). There was no difference in BCVA at baseline between the two groups, but BCVA improvement until the last visit in the non-CSC group was greater than that in the CSC group, although the difference was not statistically significant due to the small sample size (P = 0.25) (Table 3). The PEDA values ranged from 59.92 to 133.87 in the 12 eyes, which in the CSC group was significantly smaller than that in the non-CSC group (77.69 ± 11.06 VS 106.87 ± 22.62, P = 0.03) (Table 3).
Representative three eyes of CSC group with clear choroidal morphology on OCT recordings were displayed here.
Case 5
A 40-year-old man presented with progressive vision loss in both eyes accompanied by a headache for five days. His BCVA was 20/50 in the right eye and 20/200 in the left eye. Fundus photography revealed multiple bubble-like elevations at the posterior pole in both eyes (Fig. 2A). FFA revealed optic disc hyperfluorescence and multiple pinpoint leakage at the level of RPE, with subsequent pooling of dye in the subretinal space of both eyes. ICGA showed bilateral hypofluorescent areas corresponding to overlying ERD, multiple hypofluorescent dark dots and disseminated spotted choroidal hyperfluorescence, and blurred choroidal vessels (Fig. 2B). OCT presented multilobular ERD and hyperreflective dots, colocalized PED, and undulating RPE in the left eye (Fig. 2C). A diagnosis of acute VKH disease was made based on extraocular and ocular manifestations. The multiple ERD gradually subsided, and ocular inflammation was controlled under systemic prednisone treatment with a starting dose of 1 mg/kg/day followed by gradual tapering. Three weeks after presentation, BCVA improved to 20/20 in the right eye and 20/25 in the left eye. Only a slit-like neurosensory retinal detachment on OCT remained in the left eye, without any changes in PED; meanwhile, the thinned inner choroidal layer and dilated large choroidal vessel under the PED was noticeable (Fig. 2D). However, dome-shaped neurosensory retinal detachment reoccurred in the macular region at the two-month follow-up, while both the anterior chamber and vitreous cavity were quiet (Fig. 2E), FFA showed multiple punctate leakages in the left eye, which increased in size and intensity as the angiogram progressed (Fig. 2F), and barely visible hyperfluorescent spots in the right eye, OCT revealed neurosensory retinal detachment of the macular region and colocalized PED, the thinned inner choroidal layer and dilated large choroidal vessel under the PED (Fig. 2G). A diagnosis of steroid-induced multiple CSC was made. Oral prednisone was rapidly tapered to a low dose, and mycophenolate mofetil was added. Continuous-wave laser photocoagulation was performed for outside fovea leakage, and subthreshold micropulse laser photocoagulation was used for foveal leakage. One month after the adjusted therapy, bilateral BCVA was 20/20, and complete resolution of subretinal fluid was observed on OCT of the left eye; however, the PED, thinned inner choroidal layer and dilated large choroidal vessel persisted until the end of follow-up (Fig. 2H).
Disease progression and outcomes of case 5. A-C Multimodal imaging examinations of case 5 at initial indicating the diagnosis of Vogt-Koyanagi-Harada disease (VKH). A Wide field fundus photography demonstrated multiple exudative retinal detachment (ERD) in the left eye. B Fundus fluorescein angiography (FFA) and indocyanine green angiography (ICGA) revealed typical acute VKH. C OCT presented multilobular ERD and hyperreflective dots, a single PED, and undulating RPE. The PED angle (PEDA) was 82.55°.D OCT, taken 3 weeks after systemic corticosteroid treatment, showed a quiet shallow neurosensory retinal detachment, the thinned inner choroidal layer and dilated large choroidal vessel (red pentagram) beneath the persisted PED in the left eye. The PEDA increased to 89.13°. E–G Development of central serous chorioretinopathy (CSC) during the systemic corticosteroid treatment period. E Fundus photography showed dome-shaped macular (white arrows). F Multiple leakages with “ink-blot’’ pattern was noted on FFA (yellow arrows). G OCT showed sensory retinal detachment corresponding dome-shaped macular, persisted PED, thinned inner choroidal layer and dilated large choroidal vessel (red pentagram). The PEDA increased to 112.17°. H Persisted PED and dilated choroidal large vessels (red pentagrams) were noted on OCT after macular subretinal fluid of CSC resolved completely at the last follow-up. The PEDA of the persisted PED was 104.44
Case 10
A 47-year-old woman presented with bilateral acute vision loss for 1 day, accompanied by metamorphopsia and headache. She delayed prior systemic or ocular history. On examination, BCVA was 20/32 in the right eye and 20/40 in the left eye. The anterior segment examination showed bilateral shallow anterior chamber. Ultrasound biomicroscopy revealed bilateral ciliary body detachment. Fundus examination revealed multiple ERDs at the posterior pole in both eyes (Fig. 3A-B). The wide-field FFA demonstrated bilateral optic disc hyperfluorescence and multilobular dye pooling in the late period (Fig. 3C-D). On OCT, serous subretinal fluid accumulation with subretinal septa, hyperreflective dots, and multiple PEDs were evident in both eyes. Simultaneously, the attenuation of inner choroidal vessels below the RPE and dilation of the outer large choroidal vessels below PED were prominent (Fig. 3E-F). Based on the above clinical examinations, a provisional diagnosis of acute VKH was made and the patient was treated with 500 mg/day of methylprednisolone intravenously for 3 days, followed by oral prednisolone. The number of posterior multiple ERDs decreased significantly and optic disc swelling improved in 3 weeks. However, there was no improvement in some certain ERDs and PEDs, and the patient’s BCVA continuously deteriorated to hand movement in the right eye and 20/160 in the left eye, despite the addition of ADA and MMF. An FFA combined with an ICGA was performed. Compared with her first FFA, the classic features of VKH that late optic disc staining and multilobular dye pooling disappeared, but the multifocal leakage at the macula followed by pooling into the subretinal space in the form of an ‘ink-blot’ was present, and the location of the ‘ink-blot’ coincided with the intense hyper-fluorescence on her first FFA. ICGA showed apparent dilatation of large choroidal vessels (Fig. 3K-L). Furthermore, we carefully checked the OCT performed with the line scan pattern of 256 images at her first visit and found obviously microrips of the RPE at the margin of the PED (Fig. 3G-J). These findings strongly suggest that VKH and CSC might have simultaneously occurred in this patient. Subsequently, oral prednisone taper was accelerated and withdrawn in 15 days, adalimumab and mycophenolate mofetil were maintained, cyclosporine was added, and the subthreshold micropulse laser was used to seal the RPE microrips. The persisted ERDs and PEDs in both eyes subsided gradually in one month. On the last examination, eight months after the disease onset, BCVA improved to 20/63 in both eyes. OCT indicated complete remission of neurosensory retinal detachment and PED in both eyes, but the thinned inner choroidal layer and dilated large choroidal vessel still existed in bilateral eyes (Fig. 3M-N).
Disease progression and outcomes of case 10. A-J Multimodal imaging examinations of case 5 at initial indicating the diagnosis of VKH and CSC. Widefield fundus photos (A and B) of acute VKH. Widefield late-phase fluorescein angiography of acute VKH (C and D). E-J OCT of revealed the presence of subretinal fluid, septae, PED, dilatated large choroidal vessels (yellow polyline) and RPE microrips (yellow circle). K-L Three weeks after treatment with rapid and aggressive high-dose systemic corticosteroid, adalimumab and mycophenolate mofetil, FFA demonstrated ‘ink-blot’ and ICGA showed large choroidal venous dilatation. M–N Eight months after the presentation, OCT showed complete remission of neurosensory retinal detachment and PED, and dilated large choroidal vessels in bilateral eyes (red pentagrams)
Discussion
To the best of our knowledge, the association between PED, CSC, and VKH has not been reported. For the first time, our study revealed that the occurrence of PED might be associated with CSC development in VKH cases. PED with high choroidal hydrostatic pressure predisposes to the later development of CSC in VKH cases with corticosteroid therapy. Notably, our results indicated that PEDA might be a significant predictive factor for CSC development in VKH cases.
CSC can develop following the administration of corticosteroids via diverse routes [11]. Corticosteroids could elicit or aggravate CSC by inducing choroidal enlargement, which may be caused by the inappropriate mineralcorticoid receptor activation and upregulation of endothelial vasodilatory potassium channel KCa2.3 (calcium-dependent channel) [12]. However, the pilot study demonstrated that steroid-induced CSC might be an idiosyncratic response in selected vulnerable individuals rather than a dose-dependent effect [13]. CSC induced by corticosteroids has been reported to occur in a wide variety of ocular inflammatory conditions but with a relatively low incidence. Majumder et al. revealed that the prevalence of CSC in uveitis was approximately 0.13% in a large retrospective study involving 22,721 patients in India [14]. We found that the specific incidence rate of CSC in VKH was 1.06% in our cohort of 235 patients. This rate is much higher than that revealed in the Indian uveitis population, which included patients with all types of uveitis.
VKH disease and CSC are considered to be completely different diseases with different pathophysiologies. However, CSC may clinically mimic VKH or develop in VKH cases. Hence, it is of paramount importance to differentiate CSC from the relapse of inflammation once dome-shaped neurosensory retinal detachment reoccurs or worsens in VKH, as the management of these two conditions is paradoxical. Delayed diagnosis of CSC lead to permanent retinal damage with subsequent poor visual prognosis [15, 16]. Multimodal imaging examinations are useful in discriminating CSCs from VKH. On OCT, fluctuations of ILM, subretinal septa, subretinal membranous structures and hyperreflective dots, bulges of RPE, folds of RPE, and a resultant high RPE undulation index are characteristics of VKH. However, isolated serous PED always points to CSC because of its high prevalence in CSC, and it is regarded as an intermediate stage between pachychoroid and classic CSC [15, 17,14, 31]. CSC leakage points outside the fovea could be treated with continuous-wave laser photocoagulation [14]. In our series, four CSC eyes received subthreshold micropulse laser photocoagulation for foveal leakage and yielded favorable results. In contrast to the traditional continuous-wave laser, the subthreshold micropulse can provide the required activation energy of the RPE cells without damaging the retina [32, 33].
The retrospective nature of the present study brings some limitations. First, these results only provided preliminary conclusions due to a small sample size and low incidence. Second, the application of PEDA was restricted since it could not be calculated in cases where severe vitreous opacities, mature cataracts, or other conditions that prevent the presence of clear OCT recordings. Third, details of the choroid cannot be obtained in every case due to the limited penetration of OCT and poor delineation of the deeper posterior border of the choroid, and it is better to use enhanced depth imaging mode scans of OCT for precise measurement in future clinical cases. Despite its limitations, the study certainly adds to our understanding of the associations between PED in VKH patients and CSC development. Further research is needed to confirm the predictive value of PEDA and to clarify the mechanism of classic CSC development in VKH cases.
Conclusion
The present study provides the first assessment of PED and its relationship with CSC development in VKH patients. Our results indicate that PED predisposes to the development of CSC in selected VKH eyes, systemic corticosteroid treatment may promote the occurrence of classic CSC. We believe that PEDA is a simple parameter to present PED configuration and hydrostatic pressure, it might be an efficient predictive factor for the subsequent development of classic CSC.
Availability of data and materials
The data and materials are available upon request from the corresponding author at xzhang08@tmu.edu.cn.
Abbreviations
- VKH:
-
Vogt-Koyanagi-Harada
- ERD:
-
Exudative retinal detachments
- FFA:
-
Fundus fluorescein angiography
- ICGA:
-
Indocyanine green angiography
- OCT:
-
Optical coherence tomography
- RPE:
-
Retinal pigment epithelium
- PED:
-
Pigment epithelial detachment
- CSC:
-
Central serous chorioretinopathy
- TMUEH:
-
Tian** Medical University Eye Hospital
- BCVA:
-
Best-corrected visual acuity
- PEDA:
-
PED angle
- AZA:
-
Azathioprine
- CsA:
-
Cyclosporin A
- MMF:
-
Mycophenolate mofetil
- ADA:
-
Adalimumab
References
Du L, Kijlstra A, Yang P. Vogt-Koyanagi-Harada disease: Novel insights into pathophysiology, diagnosis and treatment. Prog Retin Eye Res. 2016;52:84–111.
O’Keefe GA, Rao NA. Vogt-Koyanagi-Harada disease. Surv Ophthalmol. 2017;62(1):1–25.
Silpa-Archa S, Silpa-Archa N, Preble JM, Foster CS. Vogt-Koyanagi-Harada syndrome: Perspectives for immunogenetics, multimodal imaging, and therapeutic options. Autoimmun Rev. 2016;15(8):809–19.
Lai TY, Chan RP, Chan CK, Lam DS. Effects of the duration of initial oral corticosteroid treatment on the recurrence of inflammation in Vogt-Koyanagi-Harada disease. Eye (Lond). 2009;23(3):543–8.
Tan ACS, Simhaee D, Balaratnasingam C, Dansingani KK, Yannuzzi LA. A Perspective on the Nature and Frequency of Pigment Epithelial Detachments. Am J Ophthalmol. 2016;172:13–27.
Arif F, Pryds A, Larsen M. Isolated pigment epithelium detachment: evidence for relation to central serous chorioretinopathy and effect of photodynamic therapy. Acta Ophthalmol. 2018;96(8):821–7.
Khochtali S, Ksiaa I, Megzari K, Khairallah M. Retinal Pigment Epithelium Detachment in Acute Vogt-Koyanagi-Harada Disease: An Unusual Finding at Presentation. Ocul Immunol Inflamm. 2019;27(4):591–4.
Takayama K, Obata H, Takeuchi M. Efficacy of Adalimumab for Chronic Vogt-Koyanagi-Harada Disease Refractory to Conventional Corticosteroids and Immunosuppressive Therapy and Complicated by Central Serous Chorioretinopathy. Ocul Immunol Inflamm. 2020;28(3):509–12.
Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, Arellanes-Garcia L, et al. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am J Ophthalmol. 2001;131(5):647–52.
Chhablani J, Khodani M, Hussein A, Bondalapati S, Rao HB, Narayanan R, et al. Role of macular hole angle in macular hole closure. Br J Ophthalmol. 2015;99(12):1634–8.
Ge G, Zhang Y, Zhang Y, Xu Z, Zhang M. Corticosteroids usage and central serous chorioretinopathy: a meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2020;258(1):71–7.
Zhao M, Celerier I, Bousquet E, Jeanny JC, Jonet L, Savoldelli M, et al. Mineralocorticoid receptor is involved in rat and human ocular chorioretinopathy. J Clin Invest. 2012;122(7):2672–9.
Han JM, Hwang JM, Kim JS, Park KH, Woo SJ. Changes in choroidal thickness after systemic administration of high-dose corticosteroids: a pilot study. Invest Ophthalmol Vis Sci. 2014;55(1):440–5.
Majumder PD, Menia N, Sudharshan S, Rao C, Ganesh SK, Biswas J. Clinical profile of uveitis patients develo** central serous chorioretinopathy: An experience at a tertiary eye care center in India. Indian J Ophthalmol. 2019;67(2):247–51.
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, et al. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Prog Retin Eye Res. 2015;48:82–118.
Asano KS, Asaoka R, Asano S, Azuma K, Inoue T, Obata R. Elongated Photoreceptor Outer Segment Length and Prognosis of Chronic Central Serous Chorioretinopathy. Retina. 2020;40(4):750–7.
Shin WB, Kim MK, Lee CS, Lee SC, Kim H. Comparison of the Clinical Manifestations between Acute Vogt-Koyanagi-Harada Disease and Acute Bilateral Central Serous Chorioretinopathy. Korean J Ophthalmol. 2015;29(6):389–95.
Liu XY, Peng XY, Wang S, You QS, Li YB, **ao YY, et al. Features of Optical Coherence Tomography for the Diagnosis of Vogt-Koyanagi-Harada Disease. Retina. 2016;36(11):2116–23.
Lin D, Chen W, Zhang G, Huang H, Zhou Z, Cen L, et al. Comparison of the optical coherence tomographic characters between acute Vogt-Koyanagi-Harada disease and acute central serous chorioretinopathy. BMC Ophthalmol. 2014;14:87.
Zhao GL, Li RZ, Pang YH, Wang XQ, Peng HJ, Wei JF, et al. Diagnostic Function of 3D Optical Coherence Tomography Images in Diagnosis of Vogt-Koyanagi-Harada Disease at Acute Uveitis Stage. Med Sci Monit. 2018;24:687–97.
Gupta V, Gupta P, Dogra MR, Gupta A. Spontaneous closure of retinal pigment epithelium microrip in the natural course of central serous chorioretinopathy. Eye (Lond). 2010;24(4):595–9.
Lee H, Bae K, Kang SW, Woo SJ, Ryoo NK, Kim SJ, et al. Morphologic Characteristics of Choroid in the Major Choroidal Thickening Diseases, Studied by Optical Coherence Tomography. PLoS ONE. 2016;11(1):e0147139.
Yang L, Jonas JB, Wei W. Optical coherence tomography-assisted enhanced depth imaging of central serous chorioretinopathy. Invest Ophthalmol Vis Sci. 2013;54(7):4659–65.
Yang L, Jonas JB, Wei W. Choroidal vessel diameter in central serous chorioretinopathy. Acta Ophthalmol. 2013;91(5):e358–62.
Komuku Y, Iwahashi C, Yano S, Tanaka C, Nakagawa T, Gomi F. En Face Optical Coherence Tomography Imaging of the Choroid in a Case with Central Serous Chorioretinopathy during the Course of Vogt-Koyanagi-Harada Disease: A Case Report. Case Rep Ophthalmol. 2015;6(3):488–94.
Miyanaga M, Kawaguchi T, Miyata K, Horie S, Mochizuki M, Herbort CP. Indocyanine green angiography findings in initial acute pretreatment Vogt-Koyanagi-Harada disease in Japanese patients. Jpn J Ophthalmol. 2010;54(5):377–82.
Zayit-Soudry S, Moroz I, Loewenstein A. Retinal pigment epithelial detachment. Surv Ophthalmol. 2007;52(3):227–43.
van Rijssen TJ, van Dijk EHC, Yzer S, Ohno-Matsui K, Keunen JEE, Schlingemann RO, et al. Central serous chorioretinopathy: Towards an evidence-based treatment guideline. Prog Retin Eye Res. 2019;73:100770.
Ersoz MG, Karacorlu M, Arf S, Sayman Muslubas I, Hocaoglu M. Retinal pigment epithelium tears: Classification, pathogenesis, predictors, and management. Surv Ophthalmol. 2017;62(4):493–505.
Yang P, Ren Y, Li B, Fang W, Meng Q, Kijlstra A. Clinical characteristics of Vogt-Koyanagi-Harada syndrome in Chinese patients. Ophthalmology. 2007;114(3):606–14.
Khairallah M, Kahloun R, Tugal-Tutkun I. Central serous chorioretinopathy, corticosteroids, and uveitis. Ocul Immunol Inflamm. 2012;20(2):76–85.
Gawecki M. Micropulse Laser Treatment of Retinal Diseases. J Clin Med. 2019;8(2):242.
Scholz P, Altay L, Fauser S. A Review of Subthreshold Micropulse Laser for Treatment of Macular Disorders. Adv Ther. 2017;34(7):1528–55.
Acknowledgements
Not applicable
Funding
This work was supported by a grant from the National Natural Science Foundation of China (NSFC: 81870651) and the Natural Science Foundation of Tian** (20JCZDJC00100). The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Literature screening and selection was performed by CZ, XZ and XL participated in the design of the study. CZ and KW drafted the manuscript. MZ and QT carried out the statistical analysis. XZ have given final approval of the version to be published. All authors read and approved. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Tian** Medical University Eye Hospital (No.2020KY (L)-37). Informed consent was waived by the Ethics Committee of Tian** Medical University Eye Hospital because the retrospective nature of the study.
Consent for publication
Not Applicable.
Competing interests
The authors declare that there is no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, C., Wang, K., Zhang, M. et al. Outcomes of retinal pigment epithelial detachment in Vogt-Koyanagi-Harada disease: a longitudinal analysis. BMC Ophthalmol 22, 446 (2022). https://doi.org/10.1186/s12886-022-02675-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02675-6