Abstract
Background
To evaluate anatomical and functional outcomes of patients with large submacular hemorrhage (SMH) who treated by pars plana vitrectomy (PPV) in combination with subretinal tissue plasminogen activator (TPA) injection, intraocular gas tamponade, and with additional post-operative interventions.
Methods
Medical records of 9 patients who presented with large SMH secondary to age-related macular degeneration (AMD) and underwent PPV, subretinal TPA injection, and gas tamponade at Chiang Mai university hospital between January 2012 and January 2020 were reviewed. Collected data included preoperative visual acuity (VA), SMH extent and duration, intraoperation and post-operation complications, post-operative anatomical and VA responses, and the need for administer post-operation additional treatments.
Results
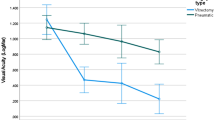
Overall, five patients were male and four patients were female with a mean (SD) age of 66.9 (7.7) years and a mean (SD) follow-up of 21.1 (16.1) months. A mean (SD) duration of SMH was 15.1 (10.9) days with a mean (SD) extent of SMH was 6.2 (3.4) disc diameters. At 1-month post-operation, complete SMH displacement was noted in eight (88.9%) patients. The mean (SD) VA significantly improved from LogMAR 1.9 (0.4) to 1.1 (0.4), (P = 0.004). During follow-up, eight patients (88.9%) were given additional therapy (anti-vascular endothelial growth factor (anti-VEGF) monotherapy, photodynamic therapy, or in combination). At final follow-up, a mean (SD) LogMAR VA of 0.9 (0.4) was significantly improved compared to baseline (P = 0.004). For intra- and post-operation complications, none developed intraoperative retinal break and retinal detachment.
Conclusions
Vitrectomy with subretinal TPA injection, intraocular gas tamponade, and additional post-operation treatments provide benefit for anatomical and visual outcomes for patients with large SMH. It may consider as one of effective treatment in this group of patients.
Similar content being viewed by others
Background
Based on evidence from many randomized controlled trials, the current mainstay treatment for neovascular age-related macular degeneration (AMD) is intravitreal anti-vascular endothelial growth factor (anti-VEGF) injection [1,2,3,4,5,6,7]. However, for an uncommon neovascular AMD complicated with a large submacular hemorrhage (SMH), the optimal therapeutic approaches remain uncertain. In this subgroup, an accumulation of blood underneath a foveal center could increase the risk of irreversible photoreceptor and outer retinal damage. Previous studies reported that if left untreated, a high proportion of patients with large SMH developed permanent and severe visual impairment [8, 9].
Due to a lack of convincing evidence from comparative studies, various treatment strategies were investigated as either mono- or combination therapy. These maneuvers included pneumatic displacement, intravitreal or subretinal tissue plasminogen activator (TPA) injection, using tamponade agents (including perfluorocarbon liquid (PFCL), silicone oil, or gas), subretinal surgery for blood clot removal, intravitreal or subretinal anti-VEGF injection, and photodynamic therapy (PDT) [10,11,12,13,14,15,16,17,18,19,20,21,22]. Therefore, the visual and anatomical responses were variably reported between publications.
This study aims to describe outcomes of patients with large SMH secondary to exudative AMD who underwent pars plana vitrectomy (PPV), subretinal TPA injection, or/and gas tamponade, with/or without postoperative additional interventions in a single tertiary referral center.
Methods
This retrospective observational case series was approved and the informed consent was waived by the Research Ethics Committee, Faculty of Medicine, Chiang Mai University, Thailand. The protocol was conducted in accordance with the Declaration of Helsinki. We identified medical and operative records of consecutive patients diagnosed with large SMH, at least 4-disc diameter, secondary to exudative AMD, who underwent PPV, subretinal TPA injection, and gas tamponade at Chiang Mai University Hospital between January 2012 and January 2020. All patients with at least one post-operative follow-up were included.
Surgical techniques and post-operative posturing
The operations were performed under local anesthesia using a 3-port 23-gauge vitrectomy system. The procedures were initiated by core vitrectomy, posterior hyaloid induction, and peripheral shaving. Then, a 39-gauge subretinal injection cannula tip (Synergetics, USA) was placed into the subretinal space, and TPA (concentration of 100 µg in 1 ml) [23] was injected by a viscous fluid controlling system. The volume and amount of TPA administered varied according to the extent and thickness of the SMH but was within a range of 25 to 50 µg (to detach the retina from the hemorrhage and cover the entire hemorrhage area). After that, air-fluid and gas-air exchange was partially performed. At the end of surgery, intravitreal anti-VEGF injection was administered at the physician’s discretion. The operations were performed by an experienced vitreoretinal surgeon (DP). After the surgery, the patients were instructed to lie down on their backs for 30 min to allow clot liquefaction [21, 24]. Then, the patients were asked to perform chin down 45 degrees positioning for 12 h, followed by face down positioning until the gas was gone. Additional postoperative treatments were given pro re nata at the discretion of the treating physician.
The data were reviewed for age, gender, systemic comorbidities, and duration of visual loss. In addition, at baseline and each follow-up visit, ophthalmic data including Snellen visual acuity (VA), anterior and posterior segment findings by slit-lamp biomicroscopy, color fundus photography, fluorescein (FFA) and indocyanine green angiography (ICGA), and optical coherence tomography (OCT), if available, were collected.
Statistical analysis
Descriptive statistics were used to analyze the data and reported as mean (SD) and range for continuous data and percentage for categorical data. Snellen VA was converted to the logarithm of the minimum angle of resolution (LogMAR) and assigned light perception as 2.7 LogMAR, hand movement as 2.3 LogMAR, and counting finger as 1.9 LogMAR [25].
At month 1 post-operation, displacement of SMH was categorized based on color fundus photograph and fundus examination into complete displacement (scarce amount of blood within one disc diameter of foveal center), partial displacement (visible amount of blood underneath the fovea with retinal elevation), and no displacement (unchanged blood amount underneath the fovea) [26]. Pre- and post-operative VA comparison was performed by the Wilcoxon signed-rank test. Statistical significance was set at P value less than 0.05. Data analysis was performed using STATA version 16.0 software.
Results
Overall, there were nine patients (5 male and 4 female) with a mean (SD) age of 66.9 (7.7) years and a mean (SD) follow-up of 21.1 (16.1) months (range, 3 to 38 months) included in this study. All patients had large SMH involving the fovea and were treatment naïve. None were taking systemic anticoagulant medications. The mean (SD) presenting LogMAR VA was 1.9 (0.4) (Snellen equivalent 20/1588). The mean (SD) duration of symptoms before surgery was 15.1 (10.9) days (range, 4 to 30 days) with four patients (44.4%) presenting later than 14 days. The mean (SD) extent of SMH was 6.2 (3.4) disc diameter (DD) (range, 4 to 15 DD). Two patients (22.2%) were noted as pseudophakia.
Intraoperatively, non-expansile sulfurhexafluoride (SF6) was used as a tamponade in seven (77.8%) patients, while non-expansile perfluoropropane (C3F8) was used in two (22.2%) patients. At the end of surgery, intravitreal bevacizumab was administered to five (55.6%) patients.
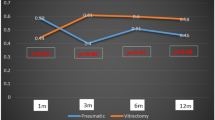
At one-month post-operation, based on additional information from cross-sectional OCT, FFA, and/or ICGA, five patients (55.6%) were diagnosed with polypoidal choroidal vasculopathy (PCV) when a branching neovascular network (BNN) lying between retinal pigment epithelium (RPE) and Bruch’s membrane, a sharp-peaked pigment epithelium detachment (PED), and a hyperfluorescence spot corresponding to polypoidal lesion were detected. Among the remaining patients, three (33.3%) were diagnosed with AMD when BNN without an accompanying complex or multilobular PED were observed. Of note, data for one patient could not be obtained. Vision significantly improved to a mean (SD) LogMAR VA of 1.1 (0.4) (Snellen equivalent, 20/251) compared to before surgery (P = 0.004). Displacement of SMH was categorized as complete in eight (88.9%) patients (three out of four patients who presented > 14 days and all of five patients who presented within 14 days from symptoms). One (11.1%) patient had partial SMH displacement. During follow-up with angiography and OCT, eight patients (88.9%) were given additional therapy: six received intravitreal anti-VEGF injections, one received combination PDT with intravitreal anti-VEGF injections, and one received PDT monotherapy. At final follow-up, a mean (SD) LogMAR VA of 0.9 (0.4) (Snellen equivalent, 20/158) was significantly improved compared to before surgery (P = 0.004), but there was a non-significant difference compared to post-operative month 1 (P = 0.063). Seven patients (77.8%) achieved a VA of 20/200 and better. Table 1 summarizes baseline characteristics of each patient.
Regarding intraoperative complications, none developed retinal and retinal pigment epithelium (RPE) tear. One patient (case 1) developed an early post-operative hemorrhage in the anterior chamber and vitreous cavity requiring a PPV and washing procedure. During follow-up, three of seven phakic patients had progressions of lens opacities and underwent cataract surgery. One patient (case 8) developed a recurrence of a large SMH and PPV with subretinal TPA injection was re-performed at month 36 after the initial surgery. One patient (case 1) developed epiretinal membrane. Other complications, including rhegmatogenous retinal detachment, macular hole, and high intraocular pressure were not observed. Figure 1 and 2 illustrate the baseline and clinical results of 2 patients with large SMH who underwent PPV and subretinal TPA injection in this study.
A 62-year-old Thai male presented with decreased vision in his right eye for 7 days (case 1). Color fundus photograph at initial presentation shows a large submacular hemorrhage (SMH) measuring 5.5-disc diameter in size (A). One month after pars plana vitrectomy with subretinal tissue plasminogen activator injection and fluid-gas exchange, a partial displacement of SMH is noted (B). Indocyanine green angiography reveals a branching vascular network underneath a foveal area (C). Optical coherence tomography (OCT) reveals branching neovascular network lying between retinal pigment epithelium and Bruch’s membrane and multilobular sharp-peaked retinal pigment epithelial detachment (D). At the final visit, submacular fibrosis is shown on the color fundus photograph (E) and regression of sharp-peaked PED is observed on the OCT following intravitreal anti-vascular endothelial growth factors injections (F)
A 54-year-old Thai male presented with blurred-vision in his left eye for 21 days. A breakthrough vitreous hemorrhage accompanied by submacular hemorrhage (SMH) is observed on fundus examination (A). Intraoperatively, a large thick SMH is found (B). At one month after pars plana vitrectomy, a hyperfluorescence spot corresponding to polypoidal lesion is observed on indocyanine green angiography (C). Optical coherence tomography (OCT) reveals a sharp-peaked retinal pigment epithelial detachment with subretinal pigment epithelial ring-like lesions (D). At the final follow-up, macular fibrosis is noted over the previous hemorrhage area on color the fundus photograph (E) and partial regression of a sharp-peaked PED is noted on the OCT following intravitreal anti-vascular endothelial growth factors injections (F)
Discussion
Large SMH is one of the uncommon manifestations of several retinal and choroidal diseases but mainly accompanies AMD. Various therapeutic approaches have been described to manage this condition. This study reviews the efficacy of PPV, subretinal TPA injection, and pneumatic displacement, with or without additional postoperative treatments to successfully remove a subfoveal hemorrhage and sustain visual improvement in patients with a large SMH secondary to exudative AMD.
At present, even with advances in medical innovation, the management of SMH complicating exudative AMD remains challenging. In this condition, an accumulation of subretinal blood may further accelerate RPE and photoreceptor damage beyond a preexisting destruction caused by a neovascular complex. Therefore, to minimize the risk of permanent and severe visual and structural alterations, several treatment strategies have been reported to clear and/or displace blood clots away from the foveal center and to minimize disease activity of underlying etiologies [18,19,20, 27, 28].
Surgical-based intervention by vitrectomy is one of the treatment options that has been widely investigated. However, with differences in patients and lesion characteristics, surgical techniques and adjunctive procedures such as post-operative intravitreal anti-VEGF injection, various outcomes were noted. In the Subretinal Surgery Trial, patients with predominantly hemorrhagic subfoveal choroidal neovascularization who underwent PPV to mechanically remove subretinal blood clots and/or neovascular complexes showed no significant difference in stabilization or vision improvement compared to observation [9].
Nevertheless, for patients with a massive bullous subretinal hemorrhage (SRH) exceeding two or more quadrants of peripheral retina, either with or without complicating vitreous hemorrhage, the efficacy of PPV for improving vision has been demonstrated in several studies [22, 29, 30]. Among those, Oshima et al. reported that by undergoing pre-operative intravitreal TPA injection with subsequent PPV, small peripheral retinotomy, PFCL, SMH drainage, and long-acting gas tamponade, 88% of patients had visual improvement, and all of these improving eyes achieved a final VA of 20/400 or better [22]. Likewise, Wei et al. [29] reported that following PPV with 360-degree retinotomy, PFCL displacement, and silicone oil tamponade, 90% of patients with massive SMH achieved visual improvement, and 52% of patients attained a visual acuity of 20/400 or better. Additionally, anatomical success following two-stage PPV with subretinal TPA and PFCL tamponade for displacing massive SMH involving subretinal and sub-RPE hemorrhage has also been described [31].
For large SMH, PPV combined with subretinal TPA injection and intraocular gas tamponade was one of the frequent procedures performed with a relatively high success rate, ranging from 64 to 100%, for complete subretinal hemorrhage displacement [20, 21, 24, 32,33,34]. Several influencing factors for the efficacy of PPV and subretinal TPA for large SMH were investigated including the extent and thickness of SMH, duration of symptoms, and baseline VA; however, the controversial associations remain [24, 32, 35,36,37,38]. Jeong et al. [33] explored associations between treatment modalities, lesion size, and responses for patients with SMH. Their study compared three treatment options (intravitreal anti-VEGF injection, pneumatic displacement combined with anti-VEGF injection, and PPV with subretinal TPA and gas tamponade), and found favorable outcomes for patients having small lesions (less than four-disc diameters) regardless of treatment groups. However, in patients with large SMH, better results were shown in patients who underwent PPV compared to patients in the pneumatic displacement group.
Our study confirmed a promising efficacy of PPV combined with TPA and gas tamponade for displacing subretinal blood in patients presenting with a large SMH. Complete displacement was achieved in almost 90% of patients within one month. This may partly refer to a short presentation period, a maximum of 30 days, for patients in this study. However, the use of intraocular gas tamponade with a long duration of face down positioning as described in this study might be one of the significant barriers for patients undergoing PPV. A 40-degree gaze down positioning over 1 to 2 weeks post-operation might facilitate better blood displacement and be better tolerated by patients [39]. In addition to anatomical success, few operative complications were encountered in this study.
Regarding visual outcome, the role of intra and/or post-operative intravitreal anti-VEGF injection, theoretically, offers potential benefit for treating underlying neovascular complex without being delayed by an obscuring detailed fundus view. Chang et al. [26] demonstrated that patients with large SMH who underwent PPV without receiving post-surgical anti-VEGF treatment had vision improvement in early postoperative visits, but the amount of visual gain slightly declined over time. However, maintenance of improved vision in patients who received post-operative anti-VEGF treatment was observed throughout the study period.
A progression of underlying conditions and/or a recurrence of SMH may relate to several factors. The ability to control pathological processes might play a role in maintaining post-operative vision. In our study, based on the discretion of treating physicians, further post-operative treatments with anti-VEGF and/or PDT were given to eight patients. In this group, the maintenance of improved vision was observed during the follow-up period. Recurrence of SMH occurred in 1 patient; however, it was successfully managed by re-operation. One patient who had no active intra/subretinal fluid and did not receive post-operative anti-VEGF treatment during follow-up visits, gradually developed submacular scarring and decreased visual gain at the final visit. Nevertheless, with the small sample size, the impact of associated factors related to disease progression could not be explored.
Limitations of this study included the retrospective nature of this study that contained variations in follow-up duration and post-operative treatments. In addition, though encouraging results were noted, the efficacy of PPV could not compare to other surgical techniques and/or other treatment modalities. However, this study supports the evidence that in patients with large SMH complicating exudative AMD, the high proportion of vision improvement with a relatively low incidence of serious postoperative complications could be achieved following PPV, subretinal TPA injection, and gas tamponade, with additional PDT and /or anti-VEGF therapy. The results from several ongoing comparative clinical trials are warranted.
Conclusions
PPV, subretinal TPA injection, intraocular gas tamponade, and additional post-operative treatments seem valuable for patients with large SMH in terms of an early subfoveal hemorrhage displacement and sustaining post-operative visual gain.
Availability of data and materials
The datasets analyzed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMD:
-
Age-related macular degeneration
- Anti-VEGF:
-
Anti-vascular endothelial growth factor
- C3F8:
-
Perfluoropropane
- FFA:
-
Fluorescein angiography
- ICGA:
-
Indocyanine green angiography
- LogMAR:
-
Logarithm of the minimum angle of resolution
- OCT:
-
Optical coherence tomography
- PCV:
-
Polypoidal choroidal vasculopathy
- PDT:
-
Photodynamic therapy
- PFCL:
-
Perfluorocarbon liquid
- PPV:
-
Pars plana vitrectomy
- RPE:
-
Retinal pigment epithelium
- SD:
-
Standard deviation
- SF6:
-
Sulfurhexafluoride
- SMH:
-
Submacular hemorrhage
- TPA:
-
Tissue plasminogen activator
- VA:
-
Visual acuity
References
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, Kim RY, Group MS. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–31.
Martin DF, Maguire MG, Fine SL, Ying GS, Jaffe GJ, Grunwald JE, Toth C, Redford M, Ferris FL. Group CoA-rMDTTCR: Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119:1388–98.
Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Wordsworth S, Reeves BC, Investigators IS. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology. 2012;119:1399–411.
Schmidt-Erfurth U, Kaiser PK, Korobelnik JF, Brown DM, Chong V, Nguyen QD, Ho AC, Ogura Y, Simader C, Jaffe GJ, et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: ninety-six-week results of the VIEW studies. Ophthalmology. 2014;121:193–201.
Li X, Xu G, Wang Y, Xu X, Liu X, Tang S, Zhang F, Zhang J, Tang L, Wu Q, et al. Safety and efficacy of conbercept in neovascular age-related macular degeneration: results from a 12-month randomized phase 2 study: AURORA study. Ophthalmology. 2014;121:1740–7.
Lim TH, Lai TYY, Takahashi K, Wong TY, Chen LJ, Ruamviboonsuk P, Tan CS, Lee WK, Cheung CMG, Ngah NF, et al. Comparison of Ranibizumab With or Without Verteporfin Photodynamic Therapy for Polypoidal Choroidal Vasculopathy: The EVEREST II Randomized Clinical Trial. JAMA Ophthalmol. 2020;138:935–42.
Ogura Y, Iida T, Lee WK, Cheung CMG, Mitchell P, Leal S, Schmelter T, Ishibashi T. Efficacy and safety of intravitreal aflibercept for polypoidal choroidal vasculopathy: 96-week outcomes in the Japanese subgroup of the PLANET study. Jpn J Ophthalmol. 2021;65:344–53.
Scupola A, Coscas G, Soubrane G, Balestrazzi E. Natural history of macular subretinal hemorrhage in age-related macular degeneration. Ophthalmologica. 1999;213:97–102.
Bressler NM, Bressler SB, Childs AL, Haller JA, Hawkins BS, Lewis H, MacCumber MW, Marsh MJ, Redford M, Sternberg P, et al. Surgery for hemorrhagic choroidal neovascular lesions of age-related macular degeneration: ophthalmic findings: SST report no. 13. Ophthalmology. 2004;111:1993–2006.
Moriarty AP, McAllister IL, Constable IJ. Initial clinical experience with tissue plasminogen activator (tPA) assisted removal of submacular haemorrhage. Eye (Lond). 1995;9:582–8.
Kamei M, Tano Y, Maeno T, Ikuno Y, Mitsuda H, Yuasa T. Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol. 1996;121:267–75.
Hassan AS, Johnson MW, Schneiderman TE, Regillo CD, Tornambe PE, Poliner LS, Blodi BA, Elner SG. Management of submacular hemorrhage with intravitreous tissue plasminogen activator injection and pneumatic displacement. Ophthalmology. 1999;106:1900–6.
Thompson JT, Sjaarda RN. Vitrectomy for the treatment of submacular hemorrhages from macular degeneration: a comparison of submacular hemorrhage/membrane removal and submacular tissue plasminogen activator-assisted pneumatic displacement. Trans Am Ophthalmol Soc. 2005;103:98–107.
Treumer F, Klatt C, Roider J, Hillenkamp J. Subretinal coapplication of recombinant tissue plasminogen activator and bevacizumab for neovascular age-related macular degeneration with submacular haemorrhage. Br J Ophthalmol. 2010;94:48–53.
Arias L, Monés J. Transconjunctival sutureless vitrectomy with tissue plasminogen activator, gas and intravitreal bevacizumab in the management of predominantly hemorrhagic age-related macular degeneration. Clin Ophthalmol. 2010;4:67–72.
Sandhu SS, Manvikar S, Steel DH. Displacement of submacular hemorrhage associated with age-related macular degeneration using vitrectomy and submacular tPA injection followed by intravitreal ranibizumab. Clin Ophthalmol. 2010;4:637–42.
Fine HF, Iranmanesh R, Del Priore LV, Barile GR, Chang LK, Chang S, Schiff WM. Surgical outcomes after massive subretinal hemorrhage secondary to age-related macular degeneration. Retina. 2010;30:1588–94.
Ohji M, Saito Y, Hayashi A, Lewis JM, Tano Y. Pneumatic displacement of subretinal hemorrhage without tissue plasminogen activator. Arch Ophthalmol. 1998;116:1326–32.
Hesse L, Schmidt J, Kroll P. Management of acute submacular hemorrhage using recombinant tissue plasminogen activator and gas. Graefes Arch Clin Exp Ophthalmol. 1999;237:273–7.
Haupert CL, McCuen BW, Jaffe GJ, Steuer ER, Cox TA, Toth CA, Fekrat S, Postel EA. Pars plana vitrectomy, subretinal injection of tissue plasminogen activator, and fluid-gas exchange for displacement of thick submacular hemorrhage in age-related macular degeneration. Am J Ophthalmol. 2001;131:208–15.
Olivier S, Chow DR, Packo KH, MacCumber MW, Awh CC. Subretinal recombinant tissue plasminogen activator injection and pneumatic displacement of thick submacular hemorrhage in Age-Related macular degeneration. Ophthalmology. 2004:111:1201-8.
Oshima Y, Ohji M, Tano Y. Pars plana vitrectomy with peripheral retinotomy after injection of preoperative intravitreal tissue plasminogen activator: a modified procedure to drain massive subretinal haemorrhage. Br J Ophthalmol. 2007;91:193-8.
Kim LA, Eliott D. Management of submacular hemorrhage in age-related macular degeneration. Ophthalmol Retina. 2018;2:177–9.
Juncal VR, Hanout M, Altomare F, Chow DR, Giavedoni LR, Muni RH, Wong DT, Berger AR. Surgical management of submacular hemorrhage: experience at an academic Canadian centre. Can J Ophthalmol. 2018;53:408–14.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the freiburg visual acuity test. Invest Ophthalmol Vis Sci. 2006;47:1236–40.
Chang W, Garg SJ, Maturi R, Hsu J, Sivalingam A, Gupta SA, Regillo CD, Ho AC. Management of thick submacular hemorrhage with subretinal tissue plasminogen activator and pneumatic displacement for age-related macular degeneration. Am J Ophthalmol. 2014;157:1250–7.
Vander JF, Federman JL, Greven C, Slusher MM, Gabel VP. Surgical removal of massive subretinal hemorrhage associated with age-related macular degeneration. Ophthalmology. 1991;98:23–7.
Peyman GA, Nelson NC, Alturki W, Blinder KJ, Paris CL, Desai UR, Harper CA. Tissue plasminogen activating factor assisted removal of subretinal hemorrhage. Ophthalmic Surg. 1991;22:575–82.
Wei Y, Zhang Z, Jiang X, Li F, Zhang T, Qiu S, Yang Y, Zhang S. A surgical approach to large subretinal hemorrhage using pars plana vitrectomy and 360° retinotomy. Retina. 2015;35:1631–9.
Choi YJ, Hyun J, Choi KS, Rhee MR, Lee SJ. Bullous hemorrhagic retinal detachment because of massive subretinal hemorrhage in patients with age-related macular degeneration. Retina. 2013;33:1365–74.
Fleissig E, Barak A, Goldstein M, Loewenstein A, Schwartz S. Massive subretinal and subretinal pigment epithelial hemorrhage displacement with perfluorocarbon liquid using a two-step vitrectomy technique. Graefes Arch Clin Exp Ophthalmol. 2017;255:1341–7.
Kimura S, Morizane Y, Hosokawa M, Shiode Y, Kawata T, Doi S, Matoba R, Hosogi M, Fujiwara A, Inoue Y, et al. Submacular hemorrhage in polypoidal choroidal vasculopathy treated by vitrectomy and subretinal tissue plasminogen activator. Am J Ophthalmol. 2015;159:683–9.
Jeong S, Park DG, Sagong M. Management of a submacular hemorrhage secondary to age-related macular degeneration: a comparison of three treatment modalities. J Clin Med. 2020;9:3088.
Tranos P, Tsiropoulos GN, Koronis S, Vakalis A, Asteriadis S, Stavrakas P. Comparison of subretinal versus intravitreal injection of recombinant tissue plasminogen activator with gas for submacular hemorrhage secondary to wet age-related macular degeneration: treatment outcomes and brief literature review. Int Ophthalmol. 2021;41:4037–46.
Schulze SD, Hesse L. Tissue plasminogen activator plus gas injection in patients with subretinal hemorrhage caused by age-related macular degeneration: predictive variables for visual outcome. Graefes Arch Clin Exp Ophthalmol. 2002;240:717–20.
Hirashima T, Moriya T, Bun T, Utsumi T, Hirose M, Oh H. Optical coherence tomography findings and surgical outcomes of tissue plasminogen activator-assisted vitrectomy for submacular hemorrhage secondary to age-related macular degeneration. Retina. 2015;35:1969–78.
González-López JJ, McGowan G, Chapman E, Yorston D. Vitrectomy with subretinal tissue plasminogen activator and ranibizumab for submacular haemorrhages secondary to age-related macular degeneration: retrospective case series of 45 consecutive cases. Eye (Lond). 2016;30:929–35.
Avcı R, Mavi Yıldız A, Çınar E, Yılmaz S, Küçükerdönmez C, Akalp FD, Avcı E. Subretinal coapplication of tissue plasminogen activator and bevacizumab with concurrent pneumatic displacement for submacular hemorrhages secondary to neovascular age-related macular degeneration. Turk J Ophthalmol. 2021;51:38–44.
Lincoff H, Kreissig I, Stopa M, Uram D. A 40 degrees gaze down position for pneumatic displacement of submacular hemorrhage: clinical application and results. Retina. 2008;28:56–9.
Acknowledgements
We would like to thank Mrs. Pat Scott (Chiang Mai University English Language Team) for help with manuscript editing.
Disclosure
The author reports no conflicts of interest in this work.
Funding
This study received funding support from the Faculty of Medicine Endowment Fund, Chiang Mai University, Thailand. The authors have no commercial interest in any materials discussed in this article.
Author information
Authors and Affiliations
Contributions
DP, PW, and JC designed the study, collected, and analysed the data, and wrote the draft paper. VC, NW, and PK contributed to study methodology and wrote the draft paper. All authors discussed the results and commented on the final manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study adhered to the tenets of the Declaration of Helsinki. This study was approved by the Research and Ethics Committee, Faculty of Medicine, Chiang Mai University, Thailand (Approval number: 253/2561). Due to the retrospective medical records review and the use of deidentified patient data, a written informed consent was waived by the committee.
Consent for publication
Not applicable.
Competing interests
The authors report no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Patikulsila, D., Winaikosol, P., Choovuthayakorn, J. et al. Pars plana vitrectomy and subretinal tissue plasminogen activator for large exudative submacular hemorrhage: a case series. BMC Ophthalmol 22, 411 (2022). https://doi.org/10.1186/s12886-022-02639-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02639-w