Abstract
Objective
This study aimed to establish the dose-response relationship between volume base dose and tumor local control for vaginal cancer, including primary vaginal cancer and recurrent gynecologic malignancies in the vagina.
Materials and methods
We identified studies that reported volume base dose and local control by searching the PubMed, the Web of Science, and the Cochrane Library Database through August 12, 2023. The regression analyses were performed using probit model between volume based dose versus clinical outcomes. Subgroup analyses were performed according to stratification: publication year, country, inclusion time of patients, patients with prior radiotherapy, age, primaries or recurrent, tumor size, concurrent chemoradiotherapy proportion, dose rate, image modality for planning, and interstitial proportion.
Results
A total of 879 patients with vaginal cancer were identified from 18 studies. Among them, 293 cases were primary vaginal cancer, 573 cases were recurrent cancer in the vagina, and 13 cases were unknown. The probit model showed a significant relationship between the HR-CTV (or CTV) D90 versus the 2-year and 3-year local control, P values were 0.013 and 0.014, respectively. The D90 corresponding to probabilities of 90% 2-year local control were 79.0 GyEQD2,10 (95% CI: 75.3–96.6 GyEQD2,10).
Conclusions
A significant dependence of 2-year or 3-year local control on HR-CTV (or CTV) D90 was found. Our research findings encourage further validation of the dose-response relationship of radical radiotherapy for vaginal cancer through protocol based multicenter clinical trials.
Similar content being viewed by others
Introduction
Primary vaginal cancer is a rare cancer, with an estimated 17,600 new cases and 8,062 deaths worldwide in 2020 [1]. Due to the relative rarity of primary vaginal cancer, prospective evaluation of its management is difficult. Fortunately, retrospective studies have demonstrated successful treatment of primary vaginal cancer with definitive radiotherapy, including external beam radiotherapy (EBRT) followed by image-guided brachytherapy (IGBT) [2,3,4,5]. For patients with early gynecological malignancies, such as cervical cancer and endometrial cancer, etc., radical hysterectomy achieved excellent cure rates. Radiotherapy is an important treatment option for medically inoperable endometrial cancer and locally advanced cervical cancer [6, 7]. However, after radical hysterectomy or radiotherapy, 10–20% of patients experience recurrence, with the majority still limited to the pelvis [8, 9]. The vagina is an important site of recurrence. Vaginal recurrences from gynecological malignancies pose clinical challenges. Organ-preserving approaches with EBRT and IGBT play an important roles in the treatment of vaginal recurrence from endometrial cancer and cervical cancer [10,11,12,13]. It has been shown that brachytherapy (BT) can improve survival and is an important component of definitive radiotherapy in vaginal cancer [14, 15].
Since 2005, GEC-ESTRO has released recommendations for three-dimensional brachytherapy of cervical cancer, which not only had a profound impact on the brachytherapy of cervical cancer, but also its methods have been borrowed by vaginal cancers [16,17,18,19]. The consensuses on target volume delineation for primary vaginal cancer [20] and recurrent endometrial and cervical tumors in the vagina [10] have only recently been reached. The high risk clinical target volume (HR-CTV) includes the residual gross tumor volume (GTV) and areas on imaging and/or clinical examination that are concerning for harboring macroscopic pathologic disease. It is admirable that before reaching these consensuses, many medical institutions had already started image-guided vaginal cancer brachytherapy and reported volume related doses. Although some researchers did not use names like HR-CTV and only used clinical target volume (CTV), the two names point to similar definitions. After analyzing the data of 91 cases of primary squamous cell carcinoma (SCCA) of the vagina treated with definitive radiotherapy, Hiniker et al. concluded that the optimal dose for definitive treatment of SCCA of the vagina lies between 70 and 80 Gy [21]. Nevertheless, the optimal volume based dose and fractionation plans have not been well-known up till now.
For cervical cancer, we have previously analyzed the dose-response relationships in image-guided BT [22], three-dimensional intracavitary combined with interstitial BT [23], and four-dimensional adaptive BT [24], and obtained results consistent with current consensus of dose constraints [25]. The purpose of this study is to identify articles that reported volume base dose and local control in definitive radiotherapy for vaginal cancer through systematic literature screening, and to conduct probit model analysis in an attempt to find the optimal dose for definitive radiotherapy for vaginal cancer.
Materials and methods
Data sources and search strategy
We performed a comprehensive literature search using the PubMed, the Web of Science, and the Cochrane Library Database to identify full articles reported the volume base dose and local control of brachytherapy in patients with vaginal cancer, including primary vaginal cancer and vaginal recurrence from gynecologic malignancies. The last search of this systematic search was performed on August 12, 2023. We searched MeSH terms “Vaginal Neoplasms” and “brachytherapy” or their all Entry terms in the title or abstract, and the search was restricted for English-language, see Supplemental Table 1. References from system reviews, guidelines, or recommendations are also included in the literature screening and eligibility process. We contacted the corresponding authors when full-text articles were not available.
Inclusion criteria were as follows
-
1.
Original articles reported EBRT with or without concurrent chemotherapy and IGBT for patients with vaginal cancer, including primary vaginal cancer and vaginal recurrence from gynecologic malignancies;
-
2.
Articles reported sufficient data for probit regression analysis, including equivalent dose in 2 Gy per fraction (EQD2), using the linear quadratic model, with α/β = 10 Gy, for minimum doses delivered to 90% (D90) of HR-CTV (or CTV) and local control rate;
-
3.
There was no limitation on nationality, race, age, stage.
Exclusion criteria were as follows
-
1.
Conference abstracts without full-text;
-
2.
Review articles, articles about recommendations, consensuses or guidelines;
-
3.
Irrelevant literature or literature focused on technique, dosimetry, side effect, quality of life etc.;
-
4.
Insufficient data;
Data extraction
Two authors screened the titles, abstracts and full-texts independently. Data in all enrolled studies were extracted according to the following procedures: (1) study information: first author, publication year and country; (2) patients characteristics: inclusion time of patients, sample size, patients number with prior radiotherapy and median age; (3) tumors characteristics: primary or recurrent, median tumor size prior to BT; (4) treatment characteristics: technique of EBRT, concurrent chemotherapy proportion, dose rate, fractionation, applicator, image modality for planning, interstitial proportion; (5) dose-volume histogram (DVH) parameters: EBRT dose, HR-CTV or CTV D90; (6) clinical outcomes: median follow-up, local control rate, disease-free survival (DFS) rate, and overall survival (OS) rate. Data were independently extracted by two authors from all eligible studies following the inclusion criteria and the exclusion criteria. Discrepancies were resolved by consultation with a third author.
Data analysis
The regression analyses between volume based dose and clinical outcomes were performed using probit model by XLSTAT 2016 (Addinsoft, Paris, France). Mean or median value was selected as the quantitative dose. The number of patients reported was selected as an Observation Weight to consider the influence of sample size. Statistical significance set at the P < 0.05 level.
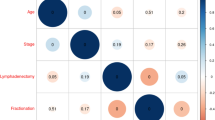
Subgroup analyses were performed according to stratification: publication year, country, inclusion time of patients, patients with prior radiotherapy, age, primaries or recurrent, tumor size, concurrent chemoradiotherapy proportion, dose rate, image modality, and interstitial proportion.
Results
Description of the included studies
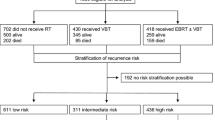
After comprehensive searching, no published regression analyses on dose-response relationship between dose and local control was identified. We used the systematic literature search strategy, and 1,232 potentially relevant studies were identified.
Prior to screening the title and abstract and reviewing the full-text, duplications were checked, 18 studies were enrolled in the dose-response analysis, see Supplemental Fig. 1.
Probit analyses
One of the 18 included studies in our analysis was a multicenter study from Denmark, France, the Netherland, and Vienna [5]. Besides, the others studies were from 7 countries, with most publications being from the United States of American (n = 10) [11, 26,27,28,29,30,31,32,33,34], followed by the India (n = 2) [12, 13], Austria [35], Canada [3], Denmark [36], France [4], and Japan [37] (one each). The main characteristics of the 18 included studies are presented in Tables 1 and 2.
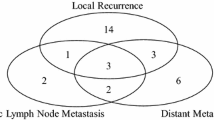
The mean or median of HR-CTV D90 or CTV D90 were reported from 59.8 to 86.0 GyEQD2,10, and actuarial or crude 2-year, 3-year, and 5-year local control rates were reported to be 61.0–100.0%, 65.8–100.0%, and 82.0–95.5%, respectively. The probit model showed significant relationships between the HR-CTV (or CTV) D90 versus the 2-year and 3-year local control, P value were 0.013 and 0.014, respectively (Figs. 1 and 2). According to this model, the D90 corresponding to probabilities of 80%, 90%, and 95% local control were 65.1 GyEQD2,10 (95% confidence interval (CI): 28.9–70.2 GyEQD2,10), 79.0 GyEQD2,10 (95% CI: 75.3–96.6 GyEQD2,10) and 90.5 GyEQD2,10 (95% CI: 83.0–149.1 GyEQD2,10), respectively. The prescribed dose to HR-CTV (CTV) D90 of 75 and 80 GyEQD2,10 would in theory warrant a 2-year local control rate of 87.1% (95% CI: 91.8% − 90.0%) and 90.4%, (95% CI: 83.7 − 93.0%), respectively. There was no significant dose response relationship between HR-CTV or CTV D90 versus DFS and OS probability, P values were 0.167 and 0.788, respectively (Table 3). The results of subgroup analysis based on stratification are shown in Table 4.
Discussion
Definitive radiotherapy is one of important treatment options for vaginal cancer, whether primary or recurrent, as it can preserve organ function and improve quality of life. However, so far, there is no consensus on the optimal prescription dose of definitive radiotherapy for vaginal cancer. Our study fills the gap in this regard. The studies of the dose toxicity relationship of the vagina as a normal tissue have provided dose constraints for clinical practice [38,39,40]. Combined with the results of this study, radiation oncologists can seek an optimal window for achieving high local tumor control while maintaining low side effects for OARs.
Our study demonstrated that two-year tumor control probability of > 90% can be expected at doses > 79.0 GyEQD2,10. This result is consistent with previous study by Hiniker et al [21]. After retrospectively analyzed the data of 91 patients with primary squamous cell carcinoma (SCCA), Hiniker et al. concluded that the optimal dose for definitive treatment of SCCA of the vagina lies between 70 and 80 Gy. In their study, a total radiation dose of > 70 Gy was associated with improved local disease control and a trend towards improved OS. It is worth noting that the dose used in their study is the prescription dose, which is the dose at depth of 5 mm or at vaginal mucosa, while the dose used in our study is volume based dose, which is D90. However, there was no significant dose-response relationship observed in our probit model analysis of the subgroup of primary vaginal cancer. This may come from two reasons. On the one hand, there was only 5 studies with a proportion of patients with primary vaginal cancer exceeding 20% in the included studies, involving 306 patients. On the other hand, the concentration of data is a reason why probit model analysis is not easy to achieve.
In vaginal cancer, there are several guidelines that provide prescription doses that are consistent with the optimized dose provided by the probit model in our study. The American Brachytherapy Society consensus guidelines for interstitial brachytherapy for vaginal cancer in 2012 stated that for disease involving the distal vagina in close proximity to the vulva or rectovaginal septum, consideration should be given to a total dose of 70–75 Gy; patients who have had poor response to EBRT or have large residual disease may benefit from higher total dose of 80–85 Gy [41]. The doses here are still prescription dose, not volume based dose. Moreover, the setting of prescription dose is mainly based on the consideration of dose tolerance to OARs, rather than considering the probability of tumor control. In the ESTRO/ESGO/SIOPe guidelines for the management of patients with vaginal cancer, the planning aim for the total dose of EBRT + BT was equal to or greater than 75 to 85 Gy to HR-CTV D90 [42]. Our probit model aligns well with this planning aim. According to our model, the HR-CTV D90 of 75 Gy to 85 Gy was expected to achieve a 2-year local control of 87–93%. The French recommendation for primary vaginal cancer stated that the dose of HR-CTV D90 should be at least 70–75 Gy, and the dose should be escalated to 80 Gy on a case-by-case basis, particularly for tumors in the upper third of the vagina [43].
In our study, there was no significant dose-response correlation between volume based dose and DFS and OS, whether it was 2-year, 3-year, or 5-year. This may be due to the heterogeneity of enrolled patients. After all, radiotherapy is a local physical therapy method, so it has the strongest correlation with local control. In the study of dose-response relationship for cervical cancer, there were also significant dose-response relationships between volume based dose and OS and cancer specific survival (CSS). Zhang et al. conducted a dose-response analysis on the data of 110 patients with locally advanced cervical cancer treated with radical concurrent chemo-radiotherapy combined with intracavitary and interstitial brachytherapy, and still obtained the dose-response correlation between HR-CTV based dose and OS and CSS [44]. Similarly Ke et al. obtained the significant dose-response relationship between GTV based dose and OS and CSS [45].
Our study included 573 patients with recurrent vaginal cancer, of which 67 had a history of radiotherapy. This made us have to think about a question, which is whether patients with a history of radiotherapy can accept the prescribed dose obtained from the probit model analysis? In terms of tumor control, newly grown tumors after previous radiotherapy have not been exposed to previous radiation, so the recurrent vaginal cancer patients with a history of radiotherapy should accept the optimized prescribed dose. However, the surrounding OARs were severely hit by both two courses of radiotherapy. When evaluating the risk of side effects, a comprehensive consideration should be given to the cumulative dose from two courses of radiotherapy and the interval time between two courses of radiotherapy to avoid serious side effects. Zolciak-Siwinska et al. [46] found that a cumulative EQD2 of approximately 100 Gy was safely delivered to D2cc of the bladder and the rectum. Ling et al.‘s study once again confirmed that re-irradiation with 3D conformal brachytherapy for vaginal recurrence was feasible and safe as long as cumulative dose to surrounding normal organs was limited [32] 0. A recent multicenter survey from Japan showed that a higher cumulative EQD2 was significantly associated with severe complications [47]. In term of interval time, Paradis et al. [48] proposed a systematic approach to the re-irradiation special medical physics consult process, which provided a previous dose discount related to interval time. Taking the bladder and rectum as an example, interval time of < 3 months, 3 months − 6 months, 6 months − 1 year, and 1 year − 3 years correspond to previous dose discount 0%, 10%, 25%, and 50%, respectively.
In radiotherapy, dose-response relationships were objective and widely recognized. Before the establishment of the dose-response curve, the optimal prescription dose for the target volumes was unclear, and it was more or less influenced by the dose constraints of the OARs. Our study derived significant dose-response relationships between volume based dose and local control based on published research results. The establishment of this dose-response relationship clears the fog for future clinical practice, striving to achieve the optimal dose recommended by the dose-response relationship while maintaining a controllable risk of OARs. Although our results are preliminary, to our knowledge, it is the first dose-response relationship study for radical radiotherapy of vaginal cancer.
Like many other studies, this study has some limitations. Firstly, there were certain differences in the delineation and naming of target volumes for included studies, which was due to the consensuses had only been reached in recent years regarding the delineation of target volumes for vaginal cancer [10, 20]. Secondly, the total number of patients included in the probit analysis was not high due to the relative rarity of vaginal cancer, and they were all observational studies. Finally, the heterogeneity of the data remains an important limitation of this study, as previously stated [22,23,24].
In conclusion, a significant dependence of 2-year or 3-year local control on HR-CTV (or CTV) D90 was found. Two-year tumor control probability of > 90% can be expected at doses > 79.0 GyEQD2,10 based on meta-regression analysis. Our research findings encourage further validation of the dose-response relationship of radical radiotherapy for vaginal cancer through protocol based multicenter clinical trials.
Data availability
All data, models, or code generated or used during the study are available from the corresponding author by request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71(3):209–49.
Westerveld H, Nesvacil N, Fokdal L, Chargari C, Schmid MP, Milosevic M, et al. Definitive radiotherapy with image-guided adaptive brachytherapy for primary vaginal cancer. Lancet Oncol. 2020;21(3):e157–67.
Goodman CD, Mendez LC, Velker V, Weiss Y, Leung E, Louie AV, et al. 3D image-guided interstitial brachytherapy for primary vaginal cancer: a multi-institutional experience. Gynecol Oncol. 2021;160(1):134–9.
Huertas A, Dumas I, Escande A, Rivin del Campo E, Felefly T, Canova C-H, et al. Image-guided adaptive brachytherapy in primary vaginal cancers: a monocentric experience. Brachytherapy. 2018;17(3):571–9.
Westerveld H, Schmid M, Nout R, Chargari C, Pieters B, Creutzberg C, et al. Image-guided adaptive brachytherapy (IGABT) for primary vaginal Cancer: results of the International Multicenter RetroEMBRAVE Cohort Study. Cancers. 2021;13(6):1459.
Reshko LB, Gaskins JT, Rattani A, Farley AA, McKenzie GW, Silva SR. Patterns of care and outcomes of radiotherapy or hormone therapy in patients with medically inoperable endometrial adenocarcinoma. Gynecol Oncol. 2021;163(3):517–23.
Pötter R, Tanderup K, Schmid MP, Jürgenliemk-Schulz I, Haie-Meder C, Fokdal LU, et al. MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): a multicentre prospective cohort study. Lancet Oncol. 2021;22(4):538–47.
Laterza RM, Uccella S, Casarin J, Morosi C, Serati M, Koelbl H, et al. Recurrence of early stage cervical Cancer after laparoscopic Versus Open Radical surgery. Int J Gynecol Cancer. 2016;26(3):547–52.
Reijntjes B, van Suijlichem M, Woolderink JM, Bongers MY, Reesink-Peters N, Paulsen L, et al. Recurrence and survival after laparoscopy versus laparotomy without lymphadenectomy in early-stage endometrial cancer: long-term outcomes of a randomised trial. Gynecol Oncol. 2022;164(2):265–70.
Kamrava M, Leung E, Bachand F, Beriwal S, Chargari C, D’Souza D, et al. GEC-ESTRO (ACROP)–ABS–CBG Consensus Brachytherapy Target Definition guidelines for recurrent endometrial and cervical tumors in the Vagina. Int J Radiation Oncology*Biology*Physics. 2023;115(3):654–63.
Kamran SC, Manuel MM, Catalano P, Cho L, Damato AL, Lee LJ, et al. MR- versus CT-based high-dose-rate interstitial brachytherapy for vaginal recurrence of endometrial cancer. Brachytherapy. 2017;16(6):1159–68.
Engineer R, Chopra S, Shukla R, Mahantshetty U, Phurailatpam R, Ghadi Y, et al. Computed tomography-based interstitial brachytherapy for recurrent cervical carcinoma in the vaginal apex. Clin Oncol. 2022;34(1):e1–6.
Chopra S, Engineer R, Shah S, Shukla R, Dora T, Gupta P, et al. MRI- and PET-Guided interstitial brachytherapy for Postsurgical Vaginal recurrences of Cervical Cancer: results of phase II study. Int J Radiation Oncology*Biology*Physics. 2020;106(2):310–9.
Orton A, Boothe D, Williams N, Buchmiller T, Huang YJ, Suneja G, et al. Brachytherapy improves survival in primary vaginal cancer. Gynecol Oncol. 2016;141(3):501–6.
Rajagopalan MS, Xu KM, Lin J, Hansen K, Sukumvanich P, Krivak TC, et al. Patterns of care and brachytherapy boost utilization for vaginal cancer in the United States. Practical Radiation Oncol. 2015;5(1):56–61.
Haie-Meder C, Pötter R, Van Limbergen E, Briot E, De Brabandere M, Dimopoulos J, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group☆ (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74(3):235–45.
Pötter R, Haie-Meder C, Limbergen EV, Barillot I, Brabandere MD, Dimopoulos J, et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy—3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78(1):67–77.
Hellebust TP, Kirisits C, Berger D, Pérez-Calatayud J, De Brabandere M, De Leeuw A, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group: considerations and pitfalls in commissioning and applicator reconstruction in 3D image-based treatment planning of cervix cancer brachytherapy. Radiother Oncol. 2010;96(2):153–60.
Dimopoulos JCA, Petrow P, Tanderup K, Petric P, Berger D, Kirisits C, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother Oncol. 2012;103(1):113–22.
Schmid MP, Fokdal L, Westerveld H, Chargari C, Rohl L, Morice P, et al. Recommendations from gynaecological (GYN) GEC-ESTRO working group – ACROP: target concept for image guided adaptive brachytherapy in primary vaginal cancer. Radiother Oncol. 2020;145:36–44.
Hiniker SM, Roux A, Murphy JD, Harris JP, Tran PT, Kapp DS, et al. Primary squamous cell carcinoma of the vagina: prognostic factors, treatment patterns, and outcomes. Gynecol Oncol. 2013;131(2):380–5.
Tang X, Mu X, Zhao Z, Zhao H, Mao Z. Dose–effect response in image-guided adaptive brachytherapy for cervical cancer: a systematic review and meta-regression analysis. Brachytherapy. 2020;19(4):438–46.
Li F, Lu S, Zhao H, Mu X, Mao Z. Three-dimensional image-guided combined intracavitary and interstitial high-dose-rate brachytherapy in cervical cancer: a systematic review. Brachytherapy. 2021;20(1):85–94.
Li F, Shi D, Bu M, Lu S, Zhao H. Four-dimensional image-guided adaptive brachytherapy for cervical Cancer: a systematic review and Meta-regression analysis. Front Oncol. 2022;12:870570.
Pötter R, Tanderup K, Kirisits C, de Leeuw A, Kirchheiner K, Nout R, et al. The EMBRACE II study: the outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin Translational Radiation Oncol. 2018;9:48–60.
Beriwal S, Rwigema J-CM, Higgins E, Kim H, Houser C, Sukumvanich P, et al. Three-dimensional image-based high-dose-rate interstitial brachytherapy for vaginal cancer. Brachytherapy. 2012;11(3):176–80.
Lee LJ, Damato AL, Viswanathan AN. Clinical outcomes following 3D image-guided brachytherapy for vaginal recurrence of endometrial cancer. Gynecol Oncol. 2013;131(3):586–92.
Vargo JA, Kim H, Houser CJ, Berhane H, Sukumvanich P, Olawaiye AB, et al. Definitive salvage for vaginal recurrence of endometrial cancer: the impact of modern intensity-modulated-radiotherapy with image-based HDR brachytherapy and the interplay of the PORTEC 1 risk stratification. Radiother Oncol. 2014;113(1):126–31.
Vargo JA, Kim H, Houser CJ, Sukumvanich P, Olawaiye AB, Kelley JL, et al. Image-based multichannel vaginal cylinder brachytherapy for vaginal cancer. Brachytherapy. 2015;14(1):9–15.
Chapman CH, Maghsoudi K, Littell RD, Chen L-M, Hsu IC. Salvage high-dose-rate brachytherapy and external beam radiotherapy for isolated vaginal recurrences of endometrial cancer with no prior adjuvant therapy. Brachytherapy. 2017;16(6):1152–8.
Gebhardt BJ, Vargo JA, Kim H, Houser CJ, Glaser SM, Sukumvanich P, et al. Image-based multichannel vaginal cylinder brachytherapy for the definitive treatment of gynecologic malignancies in the vagina. Gynecol Oncol. 2018;150(2):293–9.
Ling DC, Vargo JA, Glaser SM, Kim H, Beriwal S. Outcomes after definitive re-irradiation with 3D brachytherapy with or without external beam radiation therapy for vaginal recurrence of endometrial cancer. Gynecol Oncol. 2019;152(3):581–6.
Patel P, Deufel C, Haddock M, Petersen I. Preliminary results of modified interstitial MIAMI brachytherapy applicator for treatment of upper and apical vaginal tumors. J Contemp Brachytherapy. 2020;12(6):562–71.
Alban G, Cheng T, Adleman J, Buzurovic I, Pretz J, Singer L, et al. Definitive radiotherapy for vaginal recurrence of early-stage endometrial cancer: survival outcomes and effect of mismatch repair status. Int J Gynecologic Cancer. 2021;31(7):1007–13.
Dimopoulos JCA, Schmid MP, Fidarova E, Berger D, Kirisits C, Pötter R. Treatment of locally Advanced Vaginal Cancer with Radiochemotherapy and magnetic resonance image-guided adaptive brachytherapy: dose–volume parameters and first clinical results. Int J Radiation Oncology*Biology*Physics. 2012;82(5):1880–8.
Fokdal L, Ørtoft G, Hansen ES, Røhl L, Pedersen EM, Tanderup K, et al. Toward four-dimensional image-guided adaptive brachytherapy in locally recurrent endometrial cancer. Brachytherapy. 2014;13(6):554–61.
Murofushi KN, Tanaka R, Ohkawa A, Numajiri H, Okumura T, Sakurai H. Outcomes and dose—volume parameters for computed tomography-based brachytherapy planning for vaginal recurrence of uterine cancer primarily treated with surgery. Clin Exp Obstet Gynecol. 2021;48(3):601.
Kirchheiner K, Nout RA, Lindegaard JC, Haie-Meder C, Mahantshetty U, Segedin B, et al. Dose–effect relationship and risk factors for vaginal stenosis after definitive radio(chemo)therapy with image-guided brachytherapy for locally advanced cervical cancer in the EMBRACE study. Radiother Oncol. 2016;118(1):160–6.
Singh R, Chopra S, Engineer R, Paul S, Kannan S, Mohanty S, et al. Dose-volume correlation of cumulative vaginal doses and late toxicity after adjuvant external radiation and brachytherapy for cervical cancer. Brachytherapy. 2017;16(4):855–61.
Dankulchai P, Harn-utairasmee P, Prasartseree T, Nakkasae P, Trikhirhisthit K, Sittiwong W, et al. Vaginal 11-point and volumetric dose related to late vaginal complications in patients with cervical cancer treated with external beam radiotherapy and image-guided adaptive brachytherapy. Radiother Oncol. 2022;174:77–86.
Beriwal S, Demanes DJ, Erickson B, Jones E, De Los Santos JF, Cormack RA, et al. American Brachytherapy Society consensus guidelines for interstitial brachytherapy for vaginal cancer. Brachytherapy. 2012;11(1):68–75.
Nout RA, Calaminus G, Planchamp F, Chargari C, Lax S, Martelli H, et al. ESTRO/ESGO/SIOPe guidelines for the management of patients with vaginal cancer. Int J Gynecologic Cancer. 2023;33(8):1185–202.
Chargari C, Peignaux K, Escande A, Lafond C, Peiffert D, Petit A, et al. Role of radiotherapy in the treatment of primary vaginal cancer: recommendations of the French society for radiation oncology. Cancer/Radiothérapie. 2022;26(1–2):292–7.
Zhang N, Tang Y, Guo X, Mao Z, Yang W, Cheng G. Analysis of dose-effect relationship between DVH parameters and clinical prognosis of definitive radio(chemo)therapy combined with intracavitary/interstitial brachytherapy in patients with locally advanced cervical cancer: a single-center retrospective study. Brachytherapy. 2020;19(2):194–200.
Ke T, Wang J, Zhang N, Zhao H, Guo X, Zhao Z, et al. Dose–effect relationship between dose–volume parameters of residual gross tumor volume and clinical prognosis in MRI-guided adaptive brachytherapy for locally advanced cervical cancer: a single-center retrospective study. Strahlenther Onkol. 2022;199(2):131–40.
Zolciak-Siwinska A, Bijok M, Jonska-Gmyrek J, Kawczynska M, Kepka L, Bujko K, et al. HDR brachytherapy for the reirradiation of cervical and vaginal cancer: analysis of efficacy and dosage delivered to organs at risk. Gynecol Oncol. 2014;132(1):93–7.
Isohashi F, Yoshida K, Murakami N, Masui K, Ishihara S, Ohkubo Y, et al. Reirradiation for recurrent gynecologic cancer using high-dose-rate brachytherapy in Japan: a multicenter survey on practice patterns and outcomes. Radiother Oncol. 2024;195:110269.
Paradis KC, Mayo C, Owen D, Spratt DE, Hearn J, Rosen B, et al. The Special Medical Physics consult process for Reirradiation patients. Adv Radiation Oncol. 2019;4(4):559–65.
Acknowledgements
Not applicable.
Funding
Horizontal Project of Jilin University 2023YX0188.
Author information
Authors and Affiliations
Contributions
W.Z. and G.X. conducted literature retrieval; W.Z. and G.X. screened the literature; W.Z. and G.X. probit analysis; G.X. and Z.H. wrote the original draft preparation; Z.H. reviewed and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Z., Guo, X. & Zhao, H. Dose-response relationship between volume base dose and tumor local control in definitive radiotherapy for vaginal cancer. BMC Cancer 24, 707 (2024). https://doi.org/10.1186/s12885-024-12486-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12486-1