Abstract
Background
Lung cancer (LC) has poor survival outcomes mainly due to diagnosis at late stages. This study explored the anticipated time to seek medical advice for possible LC symptoms and barriers to early presentation in Palestine.
Methods
This cross-sectional study recruited adult participants from hospitals, primary healthcare centers, and public spaces of 11 governorates using convenience sampling. A modified, translated-into-Arabic version of the validated LC awareness measure was used to assess LC symptom awareness, the time needed to seek medical advice and barriers to early presentation.
Results
A total of 4762 participants were included. The proportion that would immediately seek medical advice for possible LC symptoms varied according to the symptoms’ nature. For respiratory symptoms, this ranged from 15.0% for ‘painful cough’ to 37.0% for ‘coughing up blood’. For non-respiratory symptoms, this ranged from ‘4.2% for ‘unexplained loss of appetite’ to 13.8% for ‘changes in the shape of fingers or nails’. Participants with good LC symptom awareness were more likely to seek medical advice within a week of recognizing most LC symptoms. About 13.0% would delay their visit to see a doctor after recognizing an LC symptom. The most reported barriers were emotional with ‘disliking the visit to healthcare facilities’ (59.8%) as the leading barrier.
Conclusion
LC respiratory symptoms were more likely to prompt early seeking of medical advice. Good LC symptom awareness was associated with a higher likelihood of help-seeking within a week. Educational interventions are needed to promote LC awareness and address the perceived barriers to early presentation in low-resource settings, such as Palestine.
Similar content being viewed by others
Introduction
Globally, lung cancer (LC) is the leading cause of cancer-related deaths with estimations of 1,796,144 deaths in 2020 [1]. LC is the third most common cancer in Palestine, following breast and colorectal cancers [2]. LC accounts for 7.8% of all recorded cancer cases in West Bank and 7.4% in Gaza Strip [2]. Furthermore, LC was the leading cause of cancer-related fatalities in 2021, accounting for 16.6% of those recorded [2]. High LC-related mortality could be attributed to delayed presentation and diagnosis at advanced stages [3, 4]. Thus, early diagnosis of LC is critical to improve treatment outcomes and to reduce the impact of disease burden [4]. This is particularly critical in low-resource countries like Palestine because of limited treatment options, fragile healthcare systems, and financial constraints [5, 6].
Previous studies have shown that the seriousness and nature of the symptoms were associated with earlier time to seek medical advice for LC symptoms [7,8,9,10,11,12,13,14]. For example, hemoptysis was perceived as an urgent symptom that led to immediate help-seeking [15,16,17,18,19]. A previous study from Nigeria showed that good LC awareness was associated with shorter time intervals to seek medical advice [20]. A recent national study from Palestine demonstrated that 51.8% of the surveyed participants displayed good awareness of LC symptoms [21].
Presentation at advanced stages is linked to various barriers that could be emotional, practical, or service-related [22]. Having a good awareness of the symptoms related to LC is associated with a higher probability of promptly seeking medical advice [23]. This suggests that through the implementation of campaigns aimed at raising awareness, it is possible to diminish the delay in seeking medical advice, ultimately leading to more positive treatment outcomes [22, 23]. To date, no studies have examined the association between LC symptom awareness and seeking medical advice for possible symptoms of LC in Palestine. Therefore, this national study aimed to (i) describe the time interval to seek medical advice for a possible LC symptom among Palestinians, (ii) examine the association between LC symptom awareness and the anticipated time to seek medical advice, and (iii) explore the barriers to early presentation and their association with LC symptom awareness in Palestine.
Materials and methods
Study design and population
This national cross-sectional study was conducted from July 16th, 2019 through to March 29th, 2020. Adult Palestinians, who make up 62% of the approximately five million residents in the Gaza Strip and the West Bank and Jerusalem (WBJ), were the target population [24]. There are 16 governorates in Palestine: five in the Gaza Strip and 11 in the WBJ [24]. Participants were recruited from 11 governorates: four in the Gaza Strip and seven in the WBJ.
Sample size calculation
In 2019, there were 3,108,852 Palestinians who aged 15 years or older in Palestine [25]. We hypothesized that 40% of study participants at most would immediately seek medical advice for a possible LC symptom. With a confidence level of 95.0%, a type I error rate of 5.0% and an absolute error of 1.0%, the minimum required sample size to detect a 40% proportion of immediate help-seeking for a possible LC symptom was 2399 participants.
Sampling methods
Most patients in Palestine receive free or low-cost healthcare at governmental hospitals and primary healthcare centers [26]. Using convenience sampling, healthy participants (i.e., without diagnosis of cancer) were recruited from governmental hospitals, primary healthcare centers, and public places including mosques, churches, downtown districts, parks, streets, malls, and public transportation stations in 11 governorates. Recruiting participants from different geographic locations was meant to increase the representativeness of the study cohort [21, 27,28,29,30,31,32,33,34,35,36,37].
Inclusion and exclusion criteria
Adult (≥ 18 years) Palestinian males and females without history of cancer visiting one of the data collection sites were included in this study. Participants were excluded if they held a nationality other than Palestinian, visited an oncology department at the time of data collection, studied or worked in healthcare, and were unable to complete the questionnaire.
Validation of study questionnaire
A modified version of the LC awareness measure (LCAM), a validated assessment tool for public awareness of LC, was used for data collection. The original LCAM was translated from English into Arabic and then back translated into English. Each step was done by two different bilingual healthcare professionals who had expertise in clinical research and survey design. To ensure content validity, the questionnaire was reviewed by five independent experts who were specialized in thoracic oncology and public health. This was followed by conducting a pilot study (n = 25) to assess the clarity of questions in the Arabic questionnaire. Data collected in the pilot study were not included in the final analysis. Internal consistency was evaluated using Cronbach's Alpha, which reached an acceptable value of 0.85 for the second and third sections in the questionnaire.
Measurement tool and data collection
The questionnaire comprised three sections. The first section described participant socio-demographic information including age, gender, marital status, employment status, monthly income, educational level, place of residence, having a chronic disease, knowing someone with cancer, site of data collection. The second section assessed the participants’ awareness of 14 LC symptoms based on a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = not sure, 4 = agree, and 5 = strongly-agree). All 14 LC symptoms were adapted from the original LCAM with yes/no/unknown responses converted into the aforementioned Likert scale to minimize the likelihood of answering questions randomly [21, 27,28,29,30,31,32,33,34,35,36,37]. The second section also assessed the anticipated time to seek medical advice if a possible LC symptom was recognized using an open-ended question. The third section explored the potential barriers for early presentation on the basis of the aforementioned 5-point Likert scale. Out of 21 barriers, 10 were adopted from the original LCAM, whereas the remaining were deemed important to be included based on related previous studies [8, 24, 38,39,40].
The data collection was done utilizing Kobo Toolbox, a safe and user-friendly data collection software for smartphones. It provides a pre-designed data collection form with check boxes and dropdown options [41]. Participants were invited to complete the questionnaire in a face-to-face interview with the presence of the data collectors, who had a background in healthcare and received special training on how to utilize the electronic tool, approach participants, and facilitate their completion of the questionnaire.
Statistical analysis
Starting from the age of 45, there is a significant increase in the likelihood of develo** LC [42]. Consequently, using this cutoff, the continuous variable of age was divided into two groups: 18–44 years and ≥ 45 years. The minimum wage in Palestine is 1450 NIS (about $450). Therefore, the continuous variable of monthly income was categorized using this cutoff into two categories: < 1450 NIS and ≥ 1450 NIS. [43].
Descriptive statistics were utilized to summarize participant characteristics. The continuous variable of age was non-normally distributed and was described using the median and interquartile range (IQR). Categorical variables were described using frequencies and percentages. Comparisons between baseline characteristics of participants recruited from the Gaza Strip versus the WBJ were performed utilizing Kruskal–Wallis or Pearson's Chi-square test if the characteristic was continuous or categorical, respectively.
LC symptoms were categorized into two categories: (i) respiratory and (ii) non-respiratory symptoms. The anticipated time needed to seek medical advice was categorized into four main categories: immediately (less than 24 h), 1–7 days, > 7 days, and never. Frequencies and percentages were used to describe the anticipated time and Pearson's Chi-Square test with Bonferroni correction was utilized to compare it between participants recruited from the Gaza Strip and those recruited from the WBJ. LC symptom awareness was evaluated as previously described [21, 27,28,29,30,31,32,33,34,35,36,37]. Participants' answers with ‘agree’ or ‘strongly agree’ were considered correct; all other answers were considered incorrect. Each correctly identified LC symptom was given one point. LC symptom awareness level was determined based on the number of symptoms recognized, where the total score (ranged from 0 to 14) was calculated and categorized into three categories: poor (0 to 4), fair (5 to 9), and good awareness (10 to 14). Multivariable logistic regression was used to examine the association between LC symptom awareness and anticipated time to seek medical advice for a possible LC symptom. The multivariable analysis adjusted for age group, gender, education, employment status, monthly income, place of residency, marital status, having a chronic disease, knowing someone with cancer, and site of data collection. This model was determined a priori based on previous studies [21, 27,28,29,30,31,32,33,34,35,36,37].
In consistence with the original LCAM [17], barriers to early presentation were categorized into three main categories: emotional, service, and practical barriers. The displayed barriers (i.e., answering with ‘agree’ or ‘strongly agree’) were described using frequencies and percentages. Comparisons in barriers between participants recruited from the Gaza Strip and those recruited from the WBJ were performed using Pearson’s Chi-Square test. The median number of barriers in each category (overall, emotional, service, and practical) was utilized as a cutoff to dichotomize the number of displayed barriers. This was followed by running a multivariable logistic regression to examine the association between LC symptom awareness and displaying at least the median number of barriers in each category. The same aforementioned multivariable model was used in all those analyses.
A complete case analysis was used to handle missing data, which were hypothesized to be missed completely at random. Stata software, version 17.0 (Stata Corp, College Station, Texas, United States) was used in all statistical analyses.
Results
Participant characteristics
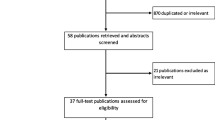
Of 5174 participants approached, 4817 agreed and completed the questionnaire (response rate = 93.1%). A total of 4762 questionnaires were included in the final analysis; 2742 from the WBJ and 2020 were from the Gaza Strip, while 55 were excluded; 31 had missing data and 24 did not meet the inclusion criteria. Participants from the WBJ were older, gained higher monthly incomes, but had lower education levels, smoked cigarettes or shisha more frequently, and suffered from more frequent chronic diseases than participants from the Gaza Strip (Table 1). However, participants from both the WBJ and the Gaza Strip had a similar likelihood to display good awareness of LC symptoms (50.6% vs. 52.6%).
Immediate seeking of medical advice for a possible LC symptom
The proportion of study participants who reported that they would immediately seek medical advice for a possible LC respiratory symptom varied based on the nature of the symptom. For respiratory symptoms, it ranged from 15.0% (n = 719) for ‘painful cough’ to 37.0% (n = 1763) for ‘coughing up blood’ (Table 2). Participants from the WBJ were more likely than participants from the Gaza Strip to immediately visit a doctor when asked about five out of nine respiratory symptoms.
For non-respiratory symptoms, the proportion of immediate help-seeking ranged from 4.2% (n = 202) for ‘unexplained loss of appetite’ to 13.8% (n = 656) for ‘changes in the shape of fingers or nails’. There were no associated differences in the proportion of immediate seeking of medical advice between participants from the WBJ and those from the Gaza Strip except for ‘unexplained weight loss’, where participants from the WBJ were more likely to immediately visit a doctor.
Association between LC symptom awareness and immediate seeking of medical advice
Compared to participants with poor LC symptom awareness, those who displayed good LC symptom awareness were more likely to report immediate seeking of medical advice for all respiratory symptoms except for ‘persistent shortness of breath’ and ‘persistent chest pain’, where no associated differences were observed (Table 3). There was no association between displaying good LC symptom awareness and seeking immediate medical advice for all non-respiratory symptoms.
Association between LC symptom awareness and seeking medical advice within a week
Compared to participants with poor LC symptom awareness, those who displayed fair LC symptom awareness were more likely to seek medical advice within a week for all LC symptoms except for ‘persistent tiredness or lack of energy’, ‘persistent shoulder pain’, and ‘unexplained loss of appetite’, where no associated differences were observed (Table 4). Additionally, there was a further associated increase in the likelihood of seeking medical advice within a week for all LC symptoms among participants who displayed good LC symptom awareness except for ‘unexplained weight loss,’ where no associated difference was found.
Barriers to early presentation and their association with LC symptom awareness
When participants were asked if they would delay their visit to the doctor when an LC symptom was recognized, 615 (12.9%) answered with ‘yes’ and reported at least one barrier to early presentation. The most frequent emotional barrier was ‘disliking the visit to healthcare facilities’ (n = 368, 59.8%) (Table 5). The most frequent service barrier was ‘the thought that there is a small number of qualified doctors in the Palestinian Ministry of Health facilities’ (n = 263, 42.8%). The most frequent practical barriers were ‘would think the symptom is not something important to see the doctor’ (n = 353, 57.4%) and ‘would try some herbs first’ (n = 348, 56.6%). All these findings were consistent in both the Gaza Strip and the WBJ with the exception that the most reported practical barrier in the Gaza Strip was ‘would try some herbs first’ (n = 137, 58.3%) followed by ‘financial hardship that will not allow seeing the doctor’ (n = 121, 51.5%). On the multivariable analysis, displaying a fair or good awareness of LC symptoms was not associated with reporting all, emotional, service, or practical barriers (Table 6).
Discussion
In this study, participants would more often seek medical advice earlier if LC respiratory symptoms were recognized compared with non-respiratory symptoms, however, less than half reported immediate help-seeking. Displaying good LC awareness was associated with a higher likelihood of seeking medical advice within a week from recognizing most LC symptoms. About 13% would delay help-seeking after recognizing an LC symptom and displayed different barriers. Individuals' approaches to seeking healthcare services, particularly when faced with LC symptoms, play a pivotal role in determining the timeliness and effectiveness of interventions [22]. Understanding health-seeking behaviors helps identify barriers and facilitators that influence when and how individuals access cancer care [24, 44].
Similar to previous studies from Australia, England, Ireland, and Denmark, ‘coughing up blood’ was one of the most frequently reported respiratory symptoms that led most participants to seek medical advice immediately [18, 19, 24, 45, 46]. Furthermore, previous studies from Palestine showed that patients were more likely to associate their symptoms with cancer if blood is present [27, 37]. This could be explained by the tendency of people to associate bleeding with ominous diagnoses and evidence of cancer [16, 45]. In contrast, ‘painful cough’ prompted immediate help-seeking only by a small proportion of study participants, which comes in concordance with findings of a previous study by Caswell and colleagues [7]. Cough is a common complaint with a wide range of differential diagnosis such as chest infections, seasonal changes, smoking, occupational exposure to environmental hazards, chronic obstructive pulmonary disease, asthma, or tuberculosis. Most participants may have experienced cough previously due to various causes, leading them to suspect possible benign causes to be more likely reasons for their cough [8, 20, 38,39,40]. A previous study conducted in Palestine reported that ‘worsening in an existing cough’ was the most recognized respiratory LC symptom [21]. Similarly, Shankar and colleagues found that two thirds of participants would seek medical help for persistent cough [47]. This suggests that the public may perceive persistence and change in character of the cough as more ominous signs, which might drive them to seek medical advice earlier. Moffat and colleagues demonstrated the impact of national cancer awareness campaigns for LC on key symptom awareness and showed that the proportion of people recognizing ‘chronic cough’ as a definite warning sign of LC rose from 18% pre-intervention to 33% post-intervention [4]. Therefore, educational interventions should incorporate the nature and character of LC symptoms.
Having good LC symptom awareness is associated with a higher likelihood of seeking medical advice earlier, as evidenced by the UK's national "Be Clear on Cancer" campaign, which significantly increased LC awareness and thus medical advice seeking and achieved better therapeutic outcomes [23]. Our results support this as we found that good LC symptom awareness was generally associated with an increase in the likelihood of seeking medical advice within a week compared to poor awareness. Likewise, a study from Nigeria showed that 76% of participants, who were able to recognize one or more of LC warning signs, would seek medical advice in less than 2 weeks compared to only 24% of those who did not recognize any [20]. Thus, by implementing campaigns that aim to increase public awareness, it appears to be possible to reduce time to seek medical advice and improve LC outcomes [22, 23]. It is also important to mention that there were regional variations in the willingness to seek immediate medical advice among participants from the WBJ versus those from the Gaza Strip, where the former group were more likely to report immediate help-seeking for more than half of LC respiratory symptoms. A possible explanation for this could be the poorer economic circumstances in the Gaza Strip. Approximately 53% of individuals in the Gaza Strip were identified as poor in 2017, reflecting a poverty rate more than four times higher than that of the West Bank and Jerusalem [48].
One of the contributing factors to delays in seeking medical advice is the experience people may have made with the healthcare system [24, 44, 49]. According to a survey conducted in the United States, more than one-third of participants had 'unfavorable evaluations of seeking medical care' due to factors such as problems with doctors and/or healthcare institutions [50]. Moreover, 12% felt that they did not need to seek medical attention as often, because they thought their illness or symptoms will resolve spontaneously [50]. This was also found in this study, where a large proportion reported barriers such as ‘dislike to visit healthcare facilities’ or ‘distrust in the competence of the local healthcare providers’ and ‘would think the symptom is not something important to see the doctor’ as well as ‘would try some herbs first’. Moreover, an Australian study found that participants with an Arabic culture had a lower level of trust in doctors compared to other study groups [16]. This demonstrates that good relationships between healthcare providers and patients may facilitate help-seeking and possibly also overcome mistrust if present [44, 51].
This is especially important among patients who smoke. Although smoking is frequently recognized as an LC risk factor, smokers were found to be less likely to seek medical advice while having possible LC symptoms as they tended to relate them to smoking [52]. Furthermore, beliefs that doctors have negative attitudes towards smokers have been found to impede help-seeking behavior [16, 24, 44, 53,54,55,56]. Alleviating these factors should be integrated in future interventions aiming to facilitate effective communication between healthcare providers and patients [55].
Future directions
The results of this study demonstrate the critical need to improve the public knowledge about LC symptoms and importance of early presentation in Palestine. Educational interventions to improve LC awareness and to address barriers to early presentation are crucial to enhance early presentation and thus improve LC outcomes. Healthcare professionals should encourage early seeking of medical advice in case LC symptoms are recognized. There is also a need for a multidisciplinary and culturally tailored approach to help individuals rationalize their presumptions, distrust and dislike towards healthcare providers. This could probably promote help-seeking and strengthen physician–patient interpersonal relationship.
Limitations
This study has some limitations. First, the convenience sampling utilized does not guarantee the generalizability of the results. However, the large number of participants, high response rate, and recruitment from various geographic locations may have mitigated this limitation. Second, potential participants with backgrounds in healthcare and patients in the oncology departments were excluded from the study, which might have impacted our interpretations. However, their exclusion was intended to make this study more relevant to the public. Lastly, participants were asked about their anticipated help-seeking behavior while they did not have any of the examined LC symptoms. It is plausible that their response and help-seeking behavior could be altered by actual experience of LC symptoms.
Conclusion
In this study, LC respiratory symptoms more often prompted immediate help-seeking with coughing up blood as the most alarming symptom. Participants with good LC symptom awareness had a higher likelihood of seeking medical advice within a week of recognizing most LC symptoms. About 13% would delay their doctor visit after recognizing an LC symptom due to various perceived barriers. Educational campaigns are needed to increase public awareness, reduce barriers to early presentation, and make positive impact on health behaviors.
Availability of data and materials
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- LC:
-
Lung cancer
- MOH:
-
Ministry of Health
- WBJ:
-
West Bank and Jerusalem
- LCAM:
-
Lung Cancer Awareness Measure
- CI:
-
Confidence interval
- OR:
-
Odds ratio
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Ministry of Health. Health Annual Report, Palestine 2021. https://rb.gy/ufaxb. Accessed 28 Dec 2023.
Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks JD. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409.
Moffat J, Bentley A, Ironmonger L, Boughey A, Radford G, Duffy S. The impact of national cancer awareness campaigns for bowel and lung cancer symptoms on sociodemographic inequalities in immediate key symptom awareness and GP attendances. Bri J Cancer. 2015;112(Suppl 1):S14-21.
Gale RP, Halahleh K. Cancer Care in the Palestinian Territories 2018. https://ascopost.com/issues/october-25-2018/cancer-care-in-the-palestinian-territories/. Accessed 28 Dec 2023.
Elshami M, Bottcher B, Alkhatib M, Ismail I, Abu-Nemer K, Hana M, Qandeel A, Abdelwahed A, Yazji H, Abuamro H, et al. Perceived barriers to seeking cancer care in the Gaza Strip: a cross-sectional study. BMC Health Serv Res. 2021;21(1):28.
Caswell G, Seymour J, Crosby V, Hussain A, Manderson C, Farnan S, Freer S, Freemantle A, Littlewood F, Wilcock A. Lung cancer diagnosed following an emergency admission: exploring patient and carer perspectives on delay in seeking help. Support Care Cancer. 2017;25(7):2259–66.
Birt L, Hall N, Emery J, Banks J, Mills K, Johnson M, Hamilton W, Walter FM. Responding to symptoms suggestive of lung cancer: a qualitative interview study. BMJ Open Respir Res. 2014;1(1):e000067.
Walton L, McNeill R, Stevens W, Murray M, Lewis C, Aitken D, Garrett J. Patient perceptions of barriers to the early diagnosis of lung cancer and advice for health service improvement. Fam Pract. 2013;30(4):436–44.
Murray SR, Kutzer Y, Habgood E, Murchie P, Walter FM, Mazza D, Shahid S, Emery JD. Reducing barriers to consulting a General Practitioner in patients at increased risk of lung cancer: a qualitative evaluation of the CHEST Australia intervention. Fam Pract. 2017;34(6):740–6.
Sharf BF, Stelljes LA, Gordon HS. “A little bitty spot and I’m a big man”: patients’ perspectives on refusing diagnosis or treatment for lung cancer. Psychooncology. 2005;14(8):636–46.
Scott N, Crane M, Lafontaine M, Seale H, Currow D. Stigma as a barrier to diagnosis of lung cancer: patient and general practitioner perspectives. Prim Health Care Res Dev. 2015;16(6):618–22.
Emery JD, Walter FM, Gray V, Sinclair C, Howting D, Bulsara M, Bulsara C, Webster A, Auret K, Saunders C, et al. Diagnosing cancer in the bush: a mixed-methods study of symptom appraisal and help-seeking behaviour in people with cancer from rural Western Australia. Fam Pract. 2013;30(3):294–301.
Hall SE, Holman CD, Threlfall T, Sheiner H, Phillips M, Katriss P, Forbes S. Lung cancer: an exploration of patient and general practitioner perspectives on the realities of care in rural Western Australia. Aust J Rural Health. 2008;16(6):355–62.
Power E, Wardle J. Change in public awareness of symptoms and perceived barriers to seeing a doctor following Be Clear on Cancer campaigns in England. Bri J Cancer. 2015;112(Suppl 1):S22-26.
Scott N, Donato-Hunt C, Crane M, Lafontaine M, Varlow M, Seale H, Currow D. Knowledge, attitudes and beliefs about lung cancer in three culturally and linguistically diverse communities living in Australia: a qualitative study. Health Promot J Australia. 2014;25(1):46–51.
Simon AE, Juszczyk D, Smyth N, Power E, Hiom S, Peake MD, Wardle J. Knowledge of lung cancer symptoms and risk factors in the U.K.: development of a measure and results from a population-based survey. Thorax. 2012;67(5):426–32.
Haastrup PF, Jarbøl DE, Balasubramaniam K, Sætre LMS, Søndergaard J, Rasmussen S. Predictive values of lung cancer alarm symptoms in the general population: a nationwide cohort study. NPJ Prim Care Respir Med. 2020;30(1):15.
Walter FM, Rubin G, Bankhead C, Morris HC, Hall N, Mills K, Dobson C, Rintoul RC, Hamilton W, Emery J. Symptoms and other factors associated with time to diagnosis and stage of lung cancer: a prospective cohort study. Brit J Cancer. 2015;112(Suppl 1):S6-13.
Desalu OO, Fawibe AE, Sanya EO, Ojuawo OB, Aladesanmi AO, Salami AK. Lung cancer awareness and anticipated delay before seeking medical help in the middle-belt population of Nigeria. Int J Tuberculosis Lung Dis. 2016;20(4):560–6.
Elshami M, Al-Slaibi I, Ghithan RJ, Alser M, Shurrab NR, Ismail IO, Mahfouz II, Fannon AA, Qawasmi MA, Hawa MR, et al. Women’s awareness of breast cancer symptoms: a national cross-sectional study from Palestine. BMC Public Health. 2022;22(1):801.
Saab MM, FitzGerald S, Noonan B, Kilty C, Collins A, Lyng Á, Kennedy U, O’Brien M, Hegarty J. Promoting lung cancer awareness, help-seeking and early detection: a systematic review of interventions. Health Promot Int. 2021;36(6):1656–71.
Ironmonger L, Ohuma E, Ormiston-Smith N, Gildea C, Thomson CS, Peake MD. An evaluation of the impact of large-scale interventions to raise public awareness of a lung cancer symptom. Br J Cancer. 2015;112(1):207–16.
Saab MM, Noonan B, Kilty C, FitzGerald S, Collins A, Lyng Á, Kennedy U, O’Brien M, Hegarty J. Awareness and help-seeking for early signs and symptoms of lung cancer: A qualitative study with high-risk individuals. Eur J Oncol Nurs. 2021;50:101880.
Palestinian Central Bureau of Statistics. The Palestinians at the end of the year 2019. https://bit.ly/2WBXVBO. Accessed 28 Dec 2023.
Halahleh KA-RN, Abusrour MM. General oncology care in Palestine. In: Al-Shamsi HO, Abu-Gheida IH, Iqbal F, Al-Awadhi A, editors. Cancer in the Arab World. Singapore: Springer Singapore; 2022. p. 195–213.
Elshami M, Al-Slaibi I, Abukmail H, Alser M, Radaydeh A, Alfuqaha A, Thalji M, Khader S, Khatib L, Fannoun N, et al. Knowledge of Palestinian women about cervical cancer warning signs: a national cross- sectional study. BMC Public Health. 2021;21(1):1779.
Elshami M, Tuffaha A, Yaseen A, Alser M, Al-Slaibi I, Jabr H, Ubaiat S, Khader S, Khraishi R, Jaber I, et al. Awareness of ovarian cancer risk and protective factors: A national cross-sectional study from Palestine. Plos One. 2022;17(3):e0265452.
Elshami M, Ayyad MM, Alser M, Al-Slaibi I, Ahmed Naji S, Mohamad BM, Sudki Isleem W, Shurrab A, Yaghi B, Qabaja YA, et al. Awareness of colorectal cancer signs and symptoms: a national cross-sectional study from Palestine. BMC Public Health. 2022;22(1):866.
Elshami M, Usrof FD, Alser M, Al-Slaibi I, Okshiya HM, Ghithan RJ, Shurrab NRS, Ismail IO, Mahfouz II, Fannon AA, et al. Awareness of Palestinian women about breast cancer risk factors: a national cross-sectional study. JCO Glob Oncol. 2022;8:e2200087.
Elshami M, Abukmail H, Al-Slaibi I, Alser M, Radaydeh A, Alfuqaha A, Thalji M, Khader S, Khatib L, Fannoun N, et al. Awareness of human papillomavirus and acceptability of the vaccine among women in Palestine: is it time for policy adjustment? BMC Womens Health. 2022;22(1):352.
Elshami M, Ahmad M, Mohammed A, Ibrahim A-S, Hanan A, Hanan S, Shahd Q, Faten Darwish U, Malik A, Wafa A, et al. Current situation and future directions of lung cancer risk factor awareness in Palestine: a cross-sectional study. BMJ Open. 2023;13(1):e061110.
Elshami M, Dwikat MF, Al-Slaibi I, Alser M, Mohamad BM, Isleem WS, Shurrab A, Yaghi B, Qabaja YA, Naji SA, et al. Awareness of colorectal cancer risk factors in Palestine: where do we stand? JCO Glob Oncol. 2022;8:e2200070.
Elshami M, Thalji M, Abukmail H, Al-Slaibi I, Alser M, Radaydeh A, Alfuqaha A, Khader S, Khatib L, Fannoun N, et al. Knowledge of cervical cancer risk factors among Palestinian women: a national cross-sectional study. BMC Womens Health. 2021;21(1):385.
Elshami M, Yaseen A, Alser M, Al-Slaibi I, Jabr H, Ubaiat S, Tuffaha A, Khader S, Khraishi R, Jaber I, et al. Knowledge of ovarian cancer symptoms among women in Palestine: a national cross-sectional study. BMC Public Health. 2021;21(1):1992.
Elshami M, Abukmail H, Aqel W, Alser M, Al-Slaibi I, Shurrab H, Qassem S, Usrof FD, Alruzayqat M, Nairoukh R, et al. Awareness of Palestinians about lung cancer symptoms: a national cross-sectional study. BMC Pulm Med. 2022;22(1):135.
Elshami M, Ayyad M, Hamdan FK, Alser M, Al-Slaibi I, Naji SA, Mohamad BM, Isleem WS, Shurrab A, Yaghi B, et al. Perceived barriers to early presentation and symptom-specific time to seek medical advice for possible colorectal cancer symptoms among Palestinians. Sci Rep. 2023;13(1):6871.
Corner J, Hopkinson J, Roffe L. Experience of health changes and reasons for delay in seeking care: a UK study of the months prior to the diagnosis of lung cancer. Soc Sci Med (1982). 2006;62(6):1381–91.
Smith SM, Campbell NC, MacLeod U, Lee AJ, Raja A, Wyke S, Ziebland SB, Duff EM, Ritchie LD, Nicolson MC. Factors contributing to the time taken to consult with symptoms of lung cancer: a cross-sectional study. Thorax. 2009;64(6):523–31.
Kaushal A, Waller J, von Wagner C, Kummer S, Whitaker K, Puri A, Lyratzopoulos G, Renzi C. The role of chronic conditions in influencing symptom attribution and anticipated help-seeking for potential lung cancer symptoms: a vignette-based study. BJGP Open. 2020;4(4):bjgpopen20X101086.
Harvard Humanitarian Initiative. KoBoToolbox. https://www.kobotoolbox.org. Accessed 28 Dec 2023.
Smith SG, Beard E, McGowan JA, Fox E, Cook C, Pal R, Waller J, Shahab L. Development of a tool to assess beliefs about mythical causes of cancer: the cancer awareness measure mythical causes scale. BMJ Open. 2018;8(12):e022825.
Awad O. The labor reality in Palestine for 2019 on the occasion of International Workers' Day.https://bit.ly/3n84Uw6. Accessed 28 Dec 2023.
Cassim S, Chepulis L, Keenan R, Kidd J, Firth M, Lawrenson R. Patient and carer perceived barriers to early presentation and diagnosis of lung cancer: a systematic review. BMC Cancer. 2019;19(1):25.
Crane M, Scott N, O’Hara BJ, Aranda S, Lafontaine M, Stacey I, Varlow M, Currow D. Knowledge of the signs and symptoms and risk factors of lung cancer in Australia: mixed methods study. BMC Public Health. 2016;16:508.
Chowienczyk S, Price S, Hamilton W. Changes in the presenting symptoms of lung cancer from 2000–2017: a serial cross-sectional study of observational records in UK primary care. Brit J Gen Pract. 2020;70(692):e193–9.
Shankar A, Roy S, Malik A, Rath GK, Julka PK, Kamal VK, Barnwal K, Upadhyaya S, Singh R, Srivastava V. Level of awareness of various aspects of lung cancer among college teachers in India: impact of cancer awareness programmes in prevention and early detection. J Cancer Educ. 2016;31(4):709–14.
Palestinian Central Bureau of Statistics, Poverty Profile in Palestine, 2017. https://rb.gy/6htkaa. Accessed 28 Dec 2023.
Saab MM, O’Driscoll M, FitzGerald S, Sahm LJ, Leahy-Warren P, Noonan B, Kilty C, Lyons N, Burns HE, Kennedy U, et al. Primary healthcare professionals’ perspectives on patient help-seeking for lung cancer warning signs and symptoms: a qualitative study. BMC Primary Care. 2022;23(1):119.
Taber JM, Leyva B, Persoskie A. Why do people avoid medical care? A qualitative study using national data. J Gen Intern Med. 2015;30(3):290–7.
McCutchan G, Weiss B, Quinn-Scoggins H, Dao A, Downs T, Deng Y, Ho H, Trung L, Emery J, Brain K. Psychosocial influences on help-seeking behaviour for cancer in low-income and lower middle-income countries: a mixed-methods systematic review. BMJ Glob Health. 2021;6(2):e004213.
Friedemann Smith C, Whitaker KL, Winstanley K, Wardle J. Smokers are less likely than non-smokers to seek help for a lung cancer “alarm” symptom. Thorax. 2016;71(7):659–61.
Burgess CC, Potts HW, Hamed H, Bish AM, Hunter MS, Richards MA, Ramirez AJ. Why do older women delay presentation with breast cancer symptoms? Psychooncology. 2006;15(11):962–8.
LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093–105.
Powell W, Richmond J, Mohottige D, Yen I, Joslyn A, Corbie-Smith G. Medical mistrust, racism, and delays in preventive health screening among African-American Men. Behav Med (Washington, DC). 2019;45(2):102–17.
Pedersen AF, Forbes L, Brain K, Hvidberg L, Wulff CN, Lagerlund M, Hajdarevic S, Quaife SL, Vedsted P. Negative cancer beliefs, recognition of cancer symptoms and anticipated time to help-seeking: an international cancer benchmarking partnership (ICBP) study. BMC Cancer. 2018;18(1):363.
Acknowledgements
The authors would like to thank all participants who took part in the survey.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
ME, NS and AM contributed to the design of the study, data analysis, data interpretation, and drafting of the manuscript. MA1, IA, HA, WA, HS, SQ, FU, MA2, RN, RK, YH, OG, WA2, OO, MD, JA, RE, AZ, HH, MoA, and SIA contributed to the design of the study, data collection, data entry, and data interpretation. NAE and BB contributed to the design of the study, data interpretation, drafting of the manuscript, and supervision of the work. All authors have read and approved the final manuscript. Each author has participated sufficiently in the work to take public responsibility for the content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical approval was obtained from: (i) the Helsinki Committee in the Gaza Strip, a committee within the MoH that gives study approvals, (ii) the Islamic University of Gaza Ethics Committee and (iii) the Human Resources Development department at the Palestinian MoH. All the methods of the study were carried out in accordance with relevant local guidelines and regulations. A detailed explanation of the study was given to all participants with the emphasis that their participation was completely voluntary, and their decision would not affect the medical care they receive. A written informed consent was obtained from all study participants. Data confidentiality was maintained throughout the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Elshami, M., Sawafta, N., Mansour, A. et al. Anticipated time to seek medical advice for possible lung cancer symptoms and barriers to timely presentation in Palestine: a national cross-sectional study. BMC Cancer 24, 183 (2024). https://doi.org/10.1186/s12885-024-11935-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-11935-1