Abstract
Background
Extrahepatic cholangiocarcinoma (ECC) has become one of the most rapidly increasing malignancies in China during recent decades. The relationship between tobacco exposure and ECC epidemics is unclear; this study aimed to explore this relationship.
Methods
We included 55,806 participants aged 30 years or older from the National Mortality and Smoking Survey of China. Smoking in participants and spouses was defined as 1 cigarette or more per day for up to 1 year. Spouses’ smoking was taken as a measure of exposure to passive smoking. Smoking information in 1980 was ascertained and outcomes were defined as ECC mortality during 1986–1988.
Results
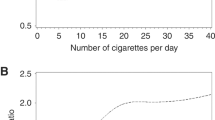
We found that either passive or active smoking increased the risk of death from ECC by 20% (risk ratio [RR], 1.20; 95% confidence interval [CI], 0.99–1.47), compared with no exposure to any tobacco. This risk was a notable 98% (RR, 1.98; 95% CI, 1.49–2.64) for individuals exposed to passive plus active smoking. These findings were highly consistent among men and women. Pathology-based analyses showed dose-response relationships of ECC with pack-years for all types of smoking exposure (Ps for trend < 0.05); the RR reached 2.75 (95% CI, 1.20–6.30) in individuals exposed to combined smoking with the highest exposure dose. The findings were similar for non-pathology-based analysis.
Conclusions
This study indicates that tobacco exposure increases ECC risk. Given the dramatic increase of exposure to secondhand smoke and patients with ECC, an inadequate provision of smoke-free environments could be contributing to ECC epidemics and could further challenge public health and medical services, based on the current disease spectrum.
Similar content being viewed by others
Background
High incidence rates of cholangiocarcinoma (CC) (> 6 per 100,000 people) have been reported in countries of Eastern Asia, such as in China, though this cancer is relatively rare worldwide [1]. CC accounts for 10–20% of deaths owing to hepatobiliary malignancies, which are the second most common cause of death from cancer in China [2, 3]. Given its resistance to current treatments and poor prognosis, the mortality and incidence of CC are virtually the same. From an anatomical viewpoint, CCs are classified as intrahepatic (ICC) or extrahepatic (ECC). ECC has been documented to account for about 90% of CCs [4]. In the Americas, 65% of ECC cases occur in the seventh decade of life [5]. By contrast, our data suggest that there are many middle-aged people with ECC cases among the Chinese population. Compared with a rising trend in ICC, the incidence of ECC seems to be decreasing or remaining constant in most developed countries, such as the United Kingdom and the United States (US) [6, 7]. However, for reasons that are unclear, the ECC appears to be one of the most rapidly increasing cancers in China, in areas such as urban Shanghai [8, Full size image
Definitions of exposure and grou**
Spouses or other relatives of all deceased persons were interviewed, to obtain information on participants’ smoking history during this mortality survey. Interviewees retrospectively described the smoking habits of the deceased participants, as well as their own, in the year 1980; this guaranteed to minimize effects of behavior changes after the participant was diagnosed with ECC. Smoking in participants and spouses was defined as ≥1 cigarette per day for up to 1 year. Spouses’ smoking was taken as a measure of exposure to passive smoking among participants. To define exposure-years of passive smoking, we used 20 years as the cut-off age for beginning smoking because we had no data on the participants’ date of marriage. Age 20 years is an acceptable and likely cut-off because this was a common age for marriage before the foundation of the People’s Republic of China in 1949 [30]. For spouses who began to smoke at age 20 years or older, we defined years of passive smoking as the age at death for cases or controls minus the age at onset of daily smoking. For spouses who began to smoke before age 20 years, the number of years of smoking before this age was further subtracted [27]. Accordingly, these participants were divided into control and exposure groups (20,128 vs. 35,678 participants), according to smoking information in 1980. The control group was defined as participants with no exposure to tobacco, including passive smoking and active smoking. Individuals exposed to any tobacco use were defined as the exposure group, including nonsmokers exposed to passive smoking (12,215 participants, 21.9% in total), smokers unexposed to passive smoking (19,026 participants, 34.1%), and smokers exposed to passive smoking (4437 participants, 7.9%).
Ascertainment of ECC
Outcomes were defined as ECC deaths during 1986–1988 after exposure to tobacco (prior to 1980). In this national mortality survey, we ascertained 451 cases of ECC (ICD-9 code: 156.1–156.9), accounting for 97.2% of all CC. These ECC cases were confirmed by autopsy, histological examination, surgical procedure, clinical assessment including imaging and laboratory testing, and clinical manifestations (0.7, 29.7, 12.2, 54.3, and 3.1% of total cases, respectively). Pathology-based diagnoses—including autopsy, histological examination, and surgical procedure which are authorized as the highest category of diagnosis in the national death surveillance system of China—were performed with 42.6%. 50.3, 32.4, and 12.9% of diagnoses were determined at provincial-, prefectural-, and county-level hospitals, respectively. Among 451 deaths owing to ECC, 24 patients have other digestive diseases including 19 related to the gallbladder and biliary tract (ICD-9 codes: 574–576, 188), 3 related to the liver (ICD-9 codes: 571, 573), and 2 related to the gastrointestinal tract (ICD-9 codes: 538, 560). A total 150, 98, 131, and 72 of the 451 deaths occurred in the control group and the three exposure groups listed above.
Statistical methods
Mean ± standard deviation and person-number (percentage in total) were used for presenting continuous and categorical variables, respectively. We calculated risk ratios (RRs) with 95% confidence intervals (CIs) comparing smokers and nonsmokers. RRs were estimated using unconditional logistic regression models [24, 25]. The initial models (Model 1) were adjusted for age as well as gender if applicable. The fully adjusted models (Model 2) further included variables that could affect association with both exposure and outcomes, including age, gender, urban or rural residence, ethnicity, and education; if applicable, the model also included either passive or active smoking and presence or absence of pathology-based diagnoses. In the interest of investigating a dose-response relationship, we defined 1 pack-year as 20 cigarettes smoked per day for 1 year. For smokers exposed to passive smoking, pack-years of passive plus active smoking were defined as active smoking multiplied by passive smoking; this was owing to the likely weak effect of each single variable on outcomes, including passive or active smoking, years of exposure, and cigarettes smoked per day.
Sensitivity analysis was used to assess the robustness of validity. First, ECC-free status at baseline was considered. The 5-year survival rate for ECC was approximately 10% during 1979–2004 in the US [31]; this rate was likely lower in China. In other words, among all ECC deaths in our survey, there were very few participants with ECC (e.g., < 10%) in 1980, when their smoking status was affirmed. Accordingly, 10% of deaths owing to ECC in each subgroup by gender and 10-year age span were randomly deleted from the participant database and a reanalysis was carried out. In addition, non-pathology-based diagnoses or digestive diseases other than ECC are factors that likely lead to misclassification of outcomes; therefore, in a random stepwise manner, we changed 10, 20, 30%, …, 100% of these ECC deaths to non-outcomes and recalculated the effect values. Lastly, to elaborate the variable of exposure to passive smoking, we showed the results considering the assumed age of marriage.
All analyses were performed using SAS 9.2 statistical software (SAS Institute, Inc., Cary, NC, USA). All P-values were two sided except P trend tests based on unconditional logistic regression, in which one-sided P values were used. A P-value < 0.05 was considered statistically significant.