Abstract
Background
BRCA1 and BRCA2 mutations explain approximately one-fifth of the inherited susceptibility in high-risk Finnish hereditary breast and ovarian cancer (HBOC) families. EMSY is located in the breast cancer-associated chromosomal region 11q13. The EMSY gene encodes a BRCA2-interacting protein that has been implicated in DNA damage repair and genomic instability. We analysed the role of germline EMSY variation in breast/ovarian cancer predisposition. The present study describes the first EMSY screening in patients with high familial risk for this disease.
Methods
Index individuals from 71 high-risk, BRCA1/2-negative HBOC families were screened for germline EMSY sequence alterations in protein coding regions and exon-intron boundaries using Sanger sequencing and TaqMan assays. The identified variants were further screened in 36 Finnish HBOC patients and 904 controls. Moreover, one novel intronic deletion was screened in a cohort of 404 breast cancer patients unselected for family history. Haplotype block structure and the association of haplotypes with breast/ovarian cancer were analysed using Haploview. The functionality of the identified variants was predicted using Haploreg, RegulomeDB, Human Splicing Finder, and Pathogenic-or-Not-Pipeline 2.
Results
Altogether, 12 germline EMSY variants were observed. Two alterations were located in the coding region, five alterations were intronic, and five alterations were located in the 3'untranslated region (UTR). Variant frequencies did not significantly differ between cases and controls. The novel variant, c.2709 + 122delT, was detected in 1 out of 107 (0.9%) breast cancer patients, and the carrier showed a bilateral form of the disease. The deletion was absent in 897 controls (OR = 25.28; P = 0.1) and in 404 breast cancer patients unselected for family history. No haplotype was identified to increase the risk of breast/ovarian cancer. Functional analyses suggested that variants, particularly in the 3'UTR, were located within regulatory elements. The novel deletion was predicted to affect splicing regulatory elements.
Conclusions
These results suggest that the identified EMSY variants are likely neutral at the population level. However, these variants may contribute to breast/ovarian cancer risk in single families. Additional analyses are warranted for rare novel intronic deletions and the 3'UTR variants predicted to have functional roles.
Similar content being viewed by others
Background
Breast cancer (BC) is the most common cancer among women in Western countries. In Finland, 4694 new BC cases were diagnosed in 2012 (Finnish Cancer Registry). Ovarian cancer (OC) is the most lethal gynaecologic malignancy in developed countries [1]. In 2012, 466 new OC cases were diagnosed, making OC the tenth most common cancer among Finnish women (Finnish Cancer Registry). The genetic predisposition to both of these diseases has been well recognized. Approximately 5–10% of all of breast and ovarian cancer cases reflect inherited genetic defects primarily in two well-known high-penetrance breast and ovarian cancer genes, BRCA1 (breast cancer 1, early onset) and BRCA2 (breast cancer 2, early onset) [2,3,4]. Both of these genes encode large proteins that play critical roles in the DNA repair pathway (reviewed in [5]). Mutations in BRCA1 and BRCA2 predispose to hereditary breast and ovarian cancer (HBOC) syndrome characterized by multiple family members affected with breast or ovarian cancer or both, early onset of BC, bilateral form of cancer, and the appearance of other cancers in family members, including prostate, pancreatic and male BC [6]. Among Finnish HBOC families, BRCA1/2 mutations are explain approximately 20% [7, 8]. Additionally, a low proportion of additional HBOC predisposition in the Finnish families reflects defects in other DNA repair pathway genes, including CHEK2 (Checkpoint kinase 2), PALB2 (Partner and localizer of BRCA2), RAD51C (RAD51 (S. cerevisiae) Homologue C), and Abraxas [9,10,11,12]. Nevertheless, additional HBOC predisposing genetic factors remains unknown, and one potential approach is to screen the candidate genes of proteins that interact with either BRCA1 or BRCA2 in the DNA repair pathway.
One of the interacting proteins of BRCA2 is EMSY (C11orf30) [13]. EMSY is located at chromosomal region 11q13 (11q13.5), which is associated with BC, particularly the hormone receptor-positive form of the disease [14]. EMSY encodes a protein with an evolutionary conserved EMSY N-terminal domain that is unique in the human genome [13]. The EMSY N-terminal domain has a structure similar to the DNA-binding motif found in transcription factors [15].
EMSY has been implicated in DNA repair and transcriptional regulation. The interaction with BRCA2 correlates EMSY to DNA repair with the observation that EMSY localizes at DNA damage sites [13]. In addition, the over-expression of a truncated form of EMSY results in a chromosome instability phenotype in human mammary epithelial cells, similar to that of cells showing a loss of BRCA2 function [16]. The binding of EMSY to the BRCA2 exon 3-encoding transcriptional activation domain represses the function of this domain [13]. In addition, EMSY interacts with the chromatin remodelling proteins Heterochromatin protein 1 β (HP1 β) and BS69 [13]. EMSY has been implicated in the regulation of nuclear receptor-mediated transcription [17], the transcription of interferon-stimulated genes with BRCA2 [18], and the transcription of antimetastatic microRNA miR-31 [19].
EMSY is amplified in breast tumours [13, 20,21,22,23], and this amplification is associated with the poor outcome of BC [13, 20,21,22]. EMSY copy number changes have also been observed in male breast tumours, but the copy number gains are comparatively more frequent in female breast tumours [24]. In addition to breast cancer, EMSY is overexpressed in high-grade ovarian cancer [13, 25, 26] and pancreatic cancer [27]. Previously, we examined the association of EMSY single-nucleotide polymorphisms (SNPs) in relation to prostate cancer predisposition and identified a rare intronic SNP that increases the risk of aggressive prostate cancer [28].
In the present study, we identified germline sequence alterations in the EMSY gene, encoding a BRCA2-interacting protein partner, which could contribute to HBOC susceptibility by disrupting critical functions in the DNA repair pathway. Thus, we sequenced the EMSY coding region and exon-intron boundaries in a cohort of 71 Finnish BRCA1/2-negative HBOC patients pre-screened for mutations in seven known breast cancer genes and copy-number alterations at the genome-wide scale [29, 30] and further analysed the identified variants in additional HBOC patients and healthy controls. To our knowledge, the present study is the first to analyse germline EMSY alterations in susceptibility to HBOC in high-risk families.
Methods
Patients and controls
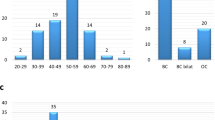
Germline EMSY sequence alterations were screened in index patients from 71 high-risk Finnish HBOC families. Study material was collected from the Tampere University Hospital Genetics Outpatient Clinic between January 1997 and May 2008. Patients belonging to a cohort of 82 high-risk HBOC individuals previously well characterized and screened for germline alterations in BRCA1, BRCA2, CHEK2, PALB2, BRIP1, RAD50, and CDH1 genes and germline copy number alterations at the genome-wide scale [29, 30]. From the previously described cohort, we included only the 71 affected index individuals in the present study, including 57 females with BC, 8 females with bilateral BC, 1 female with OC, and 5 females with both BC and OC. Originally, all patients were determined as negative for 28 Finnish BRCA1/2 founder-mutations based on minisequencing and protein truncation tests (PTTs) for BRCA1 exon 11 and BRCA2 exons 10 and 11. Additionally, the exons and exon-intron boundaries of BRCA1 and BRCA2 have previously been analysed using Sanger sequencing and Multiplex Ligation-dependent Probe amplification (MLPA) to exclude other mutations [29]. All of the identified EMSY sequence alterations were screened from the DNA samples of 36 additional index patients from HBOC families collected from the Turku region and from anonymous healthy female blood donors (n = 380–904) (referred as controls) obtained from the Finnish Red Cross. Additionally, a rare novel c.2709 + 122delT variant was further screened in a cohort of 404 BC cases unselected for family history from the Tampere region [31]. All patients were informed of the analyses and provided written consent to the use of existing DNA samples in the present study. The Ethical Committees of Tampere and Turku University Hospitals and the National Authority for Medicolegal Affairs approved this research project.
Sample preparation and mutation screening
Genomic DNA from control samples was extracted from peripheral leukocytes using the Puregene Kit according to the manufacturer’s instructions (Gentra Systems, Inc., Minneapolis, MN, USA). Mutation screening was achieved through Sanger sequencing. Reference sequence NM_020193.3 was obtained from the USCS genome browser [32, 33]. The genome build GRCh37 (hg19) was used. Whole coding regions and exon-intron boundaries were analysed. EMSY primer sequences and PCR conditions are available upon request. Sequencing was performed using the Big Dye Terminator v.3.1 Cycle Sequencing Kit and the ABIPRISM 3130xl Genetic Analyser (Applied Biosystems, Foster City, CA, USA). The sequences were analysed using Sequencher v.5.1 software (Gene Codes Corporation, Ann Arbor, MI, USA). The RefSNP number for the identified variants was obtained from the NCBI Single Nucleotide Polymorphism database (dbSNP) [34]. Two variants, rs1044265 and rs2513513, were analysed from controls using TaqMan SNP Genoty** Assays according to the manufacturer’s instructions with the ABI Prism® 7900HT instrument and SDS2.2.2 software (Applied Biosystems). The genoty** call rates of the SNPs were ≥0.98.
Statistical and bioinformatics analyses
Observed variants were tested for Hardy-Weinberg equilibrium in the controls. The association of variants with breast/ovarian cancer was examined using Fisher’s exact test. P values were two-sided, and P < 0.05 was considered statistically significant. The association of the minor allele was examined. Odds ratios (OR) and confidence intervals (CI) were calculated using PLINK v1.07 [35]. If the variant was not observed in cases or controls, then the OR was calculated using GraphPad Prism version 5.02 for Windows (GraphPad Software, San Diego, CA, USA) by adding 0.5 to each value to obtain numeric values. Linkage disequilibria (LD) between variants, haplotype blocks and the association of haplotypes with breast/ovarian cancer were analysed using Haploview v4.2 [36]. Haplotype blocks were defined using 107 cases and 380 controls via Gabriel’s method, which includes by default SNPs with minor allele frequencies (MAFs) > 0.05 [37].
The effect of the amino-acid changing variant, c.2861 T > G (Leu954Arg), was predicted using the Pathogenic-or-Not-Pipeline (PON-P2) programme [38]. The functionality of the observed SNPs with rs IDs was analysed using HaploReg v2 [39], including conserved region, open chromatin, regulatory chromatin state from the Encyclopaedia of DNA Elements (ENCODE) [40], protein binding, and altered motifs. The four alternative positions of the deletion c.2709 + 122delT (chr11 76,253,530–76,253,533) were analysed for functional elements using RegulomeDB [41], which includes data for predicted and known regulatory elements, such as regions of DNA hypersensitivity, binding sites of transcription factors, and regions with enhancer activity.
The effect of the deletion c.2709 + 122delT on splicing was analysed using Human Splicing Finder (HSF) v2.4.1 [42]. The alternative deletion locations were analysed using HSF to detect potential splice sites (HSF matrices), potential branch points, enhancer motifs (ESE Finder) and hnRNP motifs (experimental) of SR proteins.
Results
In the present study, we identified 12 different germline EMSY sequence alterations in index patients from 71 HBOC families, and the alterations were further screened in a cohort of 36 HBOC patients and healthy controls. Variant frequencies are presented in Table 1. Two of the identified alterations were located in the protein-coding region, five alterations were intronic, and five variants were located in the 3′UTR. With the exception of one alteration, c.2709 + 122delT, all of the identified variants are reported in the NCBI Single Nucleotide Polymorphism (SNP) database with rs-numbers (Table 1).
All SNPs were in Hardy Weinberg equilibrium in controls. The allele frequencies did not significantly differ between cases and controls (Table 1). One of the SNPs, rs2508740, was triallelic. Interestingly, the T allele, observed in one control sample, has not previously been reported in the SNP database. However, this control sample was not included in the association testing of the SNP. One of the two variants observed in the protein-coding region rs184345272 resulted in an amino acid substitution of a hydrophobic leucine with a positively charged arginine at position 954. The heterozygous rs184345272 variant was identified in two patients (2 of 106, 1.9%) and three controls (3 of 376, 0.8%) (OR = 2.40; P = 0.3). PON-P2 predicts the unknown effects of substitutions.
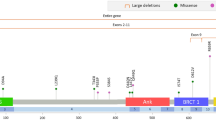
The most interesting finding was the rare novel sequence alteration, c.2709 + 122delT (Fig. 1). The precise location of the deleted T could not be determined based on the sequence because of a stretch of four T bases in the reference sequence (chr11 76,253,530–76,253,533). This deletion has been named according to the Human Genome Variation Society (HGVS) nomenclature (http://varnomen.hgvs.org, v.15.11). The heterozygous deletion was identified in one patient (1 of 107, 0.9%) with bilateral BC diagnosed at 39 and 42 years of age. However, none of the controls (0 of 897, 0%) had this deletion (OR = 25.28; P = 0.1) (Table 1), and it was not observed in a cohort of 404 BC cases unselected for family history (data not shown). The deletion carrier patient died of BC at age 52. The clinical features of the patient included invasive ductal type grade 1 tumour in the left breast and invasive ductal type grade 2 tumour in the right breast. Both the tumours had oestrogen and progesterone receptor positive and human epidermal growth factor receptor 2 negative statuses. The patient’s mother had BC diagnosed at age 51, and the father had pancreatic cancer diagnosed at age 64. The patient had one healthy brother. Additionally, the deletion carrier patient had four other heterozygous EMSY variants, rs42445443, rs2508740, rs2513513, and rs1044265.
Based on haplotype block analysis, seven observed variants (rs4245443, rs2508740, rs11363199, rs3753051, rs2513513, rs187735484 and rs1044265) formed a haplotype block (Fig. 2). A total of six haplotypes were observed. The haplotype AAATAAA was more common in controls (2.6%) than cases (0.5%) with a borderline significance difference (P = 0.05). The SNP rs2508740 was in high LD (r2 ≥ 0.8) with rs3753051, rs11363199, rs2513513, and rs4245443 (Fig. 2). In addition, high LD was observed for SNPs rs4245443 and rs2513513 and SNPs rs11363199 and rs3753051 (Fig. 2).
The haplotype block structure. Haplotype analysis included the genotypes of the observed variants from 107 breast and/or ovarian cancer cases and 380 controls. The first alternative marker position was used for c.2079 + 122delT. Linkage disequilibrium (LD) values (r2 × 100) are represented in the chart in shades of black. The figure was obtained using Haploview [36]
The functionality of the identified SNPs with rs IDs (all but c.2709 + 122delT) was analysed in silico using HaploReg v.2 [39] (Table 2). Some differences were observed in conserved regions between GERP and SiPhy approaches, but the conserved regions primarily overlapped with the SNPs located in exonic and 3′UTR regions. The 3′UTR SNPs were located within open chromatin in several cell lines and coincided with the chromatin states of strong enhancers. In addition, two intronic variants (rs11600501 and rs11363199) were located within chromatin states of weak enhancers. Nine of the 11 analysed variants were predicted to affect regulatory motifs. None of the variants were located within protein binding sites.
The functionality of the c.2709 + 122delT variant was examined using the Regulome DB [41], and the four alternative locations of the deletion coincided with the same functional elements, including the open chromatin and transcription factor binding site of GATA6 (Additional file 1: Table S1). In addition, the four-base location coincides with three regulation motif positions.
The effect of c.2709 + 122delT on splicing regulatory elements was analysed using Human Splicing Finder [42] (Additional file 1: Table S2), which indicates both the introduction and deletion of an acceptor splice site as a result of the deletion of either one of the alternative nucleotides. The deletion of the third or fourth nucleotide introduced and abolished a potential branch point. No enhancer motifs of SR proteins or silencer motifs of hnRNP were affected by this deletion.
Discussion
Genetic factors predisposing to breast and ovarian cancer primarily remain unknown in HBOC families negative for BRCA1 and BRCA2 mutations. Here, we screened the EMSY gene, encoding the BRCA2-interacting protein, for germline sequence alterations and analysed the association of the observed variants with breast/ovarian cancer risk. We utilized a cohort of index individuals from 71 high-risk BRCA1/2-negative HBOC families previously screened for germline alterations in seven known BC genes and copy number alterations at the genome-wide scale [29, 30]. According to previous analyses, no known predisposing variants have been identified in a majority (87%) of the screened high-risk families [29, 30], indicating the existence of yet unknown gene variants contributing to breast/ovarian cancer susceptibility. To our knowledge, this study is the first to screen the EMSY gene for germline variations in relation to breast/ovarian cancer in high-risk families.
We identified 12 different variants in the coding regions and exon-intron boundaries, but none of these variants showed a statistically significant association with breast/ovarian cancer risk at the population level, which may reflect the limited sample size in the present study. Moreover, haplotype analysis identified one haplotype as more common in controls compared to cases but with borderline significance difference. However, the identified variants, particularly the rare novel deletion, c.2709 + 122delT, could be important predisposing factors in individual patients and in a few cancer families. Interestingly, the deletion carrier patient was affected with bilateral BC, which may indicate that this deletion contributes to a poor clinical outcome of the disease. The deletion carrier patient did not have deleterious mutations or copy number changes in the previously screened BC genes, BRCA1, BRCA2, CHEK2, PALB2, BRIP1, RAD50, and CDH1 [29, 30]. Unfortunately, we did not obtain blood samples from the relatives of the deletion carrier patient to examine the segregation of the deletion with the disease. Although this deletion is located in an intronic region, it may represent a functional variant, according to the results of the in silico functional analyses. Thus, further studies of this deletion are warranted. Of note, during the review process of this manuscript, the deletion was published in the dbSNP and received reference SNP id number 983125332.
Only one missense variant (rs184345272) was identified in the protein-coding region of EMSY, suggesting that mutations are either rare or not tolerated. The rs184345272 variant, predicted to have unknown effect on protein function, was 2.4 times more common in cases compared to controls, but obviously a larger number of samples should be screened to determine whether this variant could be a low-risk allele. Interestingly, five of the 12 (41.6%) alterations occurred in the 3′UTR and were predicted to play functional roles. Further screening of these variants would be interesting, particularly for the rs148932730 variant, which was detected as 1.4 times more common in cases vs. controls.
No truncating mutations, such as frameshift or nonsense mutations, were detected. Because EMSY is amplified or over-expressed in breast and ovarian cancer tumours [13, 20,21,22,23, 25, 26], predisposing germline alterations are expected to result in the gain-of-function rather than the loss-of-function of EMSY. Based on the in silico functional annotation, either of the alternatives can be ruled out, since, for example, the potential effect of the c.2709 + 122delT deletion on splicing might affect the function of EMSY. Unfortunately, tumour DNA was not available from the deletion patient for additional analysis, for example, loss of heterozygosity (LOH). Therefore, further functional studies are needed to clarify these findings and characterize the effects of the variants on the functions of other genes through gene regulation.
Common EMSY variations associated with breast and ovarian cancer risks have previously been examined in British population-based studies [43]. Three out of the six SNPs observed in the British study [43] (rs4245443, rs2508740, and rs11600501) were also identified in the cohort in the present study. We did not observe an association of these SNPs with breast/ovarian cancer risk, consistent with previous results [43].
We previously examined the association of EMSY SNPs with prostate cancer predisposition and identified a rare intronic SNP that increases the risk of aggressive prostate cancer (referred to as aggressive SNP) [28]. Interestingly, the aggressive SNP was segregated with breast cancer in a prostate cancer family [28]. However, in the present study, we did not detect the aggressive SNP. Since we only screened one individual per breast/ovarian cancer family, we cannot rule out that the other affected family members in the examined cohort could be carriers of the previously detected aggressive SNP.
Conclusions
In conclusion, this study is the first to analyse the role of germline EMSY sequence alterations in HBOC predisposition in Finnish families. None of the observed EMSY variants showed statistically significant associations with breast/ovarian cancer risk at the population level. Based on the results, we cannot exclude the likelihood variants contributing to cancer risk in certain high-risk families, perhaps as private mutations. The variants could be used to determine cancer risk with other predisposing mutations in these families. Further analyses are warranted, particularly for the rare novel intronic deletion and 3′UTR variants predicted to have functional roles.
Abbreviations
- BC:
-
Breast cancer
- BRCA1 :
-
Breast cancer 1, early onset
- BRCA2 :
-
Breast cancer 2, early onset
- CHEK2 :
-
Checkpoint kinase
- CI:
-
Confidence interval
- HBOC:
-
Hereditary breast and ovarian cancer
- HGVS:
-
Human Genome Variation Society
- HP1 β:
-
Heterochromatin protein 1 β
- LD:
-
Linkage disequilibria
- LOH:
-
Loss of heterozygosity
- MAF:
-
Minor allele frequency
- MLPA:
-
Multiplex Ligation-dependent Probe amplification
- OC:
-
Ovarian cancer
- OR:
-
Odds ratio
- PALB2 :
-
Partner and localizer of BRCA2
- PTT:
-
Protein truncation test
- RAD51C :
-
RAD51 (S. cerevisiae) Homologue C
- SNP:
-
Single-nucleotide polymorphism
- UTR:
-
Untranslated region
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77(11):2318–24.
Miki Y, Swensen J, Shattuck-Eidens D, Futreal PA, Harshman K, Tavtigian S, Liu Q, Cochran C, Bennett LM, Ding W. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science. 1994;266(5182):66–71.
Wooster R, Neuhausen SL, Mangion J, Quirk Y, Ford D, Collins N, Nguyen K, Seal S, Tran T, Averill D. Localization of a breast cancer susceptibility gene, BRCA2, to chromosome 13q12-13. Science. 1994;265(5181):2088–90.
Ciccia A, Elledge SJ. The DNA damage response: making it safe to play with knives. Mol Cell. 2010;40(2):179–204.
Petrucelli N, Daly MB, Feldman GL. Hereditary breast and ovarian cancer due to mutations in BRCA1 and BRCA2. Genet Med. 2010;12(5):245–59.
Vehmanen P, Friedman LS, Eerola H, McClure M, Ward B, Sarantaus L, Kainu T, Syrjakoski K, Pyrhonen S, Kallioniemi OP, Muhonen T, Luce M, Frank TS, Nevanlinna H. Low proportion of BRCA1 and BRCA2 mutations in Finnish breast cancer families: evidence for additional susceptibility genes. Hum Mol Genet. 1997;6(13):2309–15.
Hartikainen JM, Kataja V, Pirskanen M, Arffman A, Ristonmaa U, Vahteristo P, Ryynanen M, Heinonen S, Kosma VM, Mannermaa A. Screening for BRCA1 and BRCA2 mutations in Eastern Finnish breast/ovarian cancer families. Clin Genet. 2007;72(4):311–20.
Vahteristo P, Bartkova J, Eerola H, Syrjakoski K, Ojala S, Kilpivaara O, Tamminen A, Kononen J, Aittomaki K, Heikkila P, Holli K, Blomqvist C, Bartek J, Kallioniemi OP, Nevanlinna H. A CHEK2 genetic variant contributing to a substantial fraction of familial breast cancer. Am J Hum Genet. 2002;71(2):432–8.
Erkko H, **a B, Nikkila J, Schleutker J, Syrjakoski K, Mannermaa A, Kallioniemi A, Pylkas K, Karppinen S, Rapakko K, Miron A, Sheng Q, Li G, Mattila H, Bell DW, Haber DA, Grip M, Reiman M, Jukkola-Vuorinen A, Mustonen A, Kere J, Aaltonen LA, Kosma V, Kataja V, Soini Y, Drapkin RI, Livingston DM, Winqvist R. A recurrent mutation in PALB2 in Finnish cancer families. Nature. 2007;446(7133):316–9.
Pelttari LM, Heikkinen T, Thompson D, Kallioniemi A, Schleutker J, Holli K, Blomqvist C, Aittomaki K, Butzow R, Nevanlinna H. RAD51C is a susceptibility gene for ovarian cancer. Hum Mol Genet. 2011;20(16):3278–88.
Solyom S, Aressy B, Pylkas K, Patterson-Fortin J, Hartikainen JM, Kallioniemi A, Kauppila S, Nikkila J, Kosma VM, Mannermaa A, Greenberg RA, Winqvist R. Breast cancer-associated Abraxas mutation disrupts nuclear localization and DNA damage response functions. Sci Transl Med. 2012;4(122):122ra23.
Hughes-Davies L, Huntsman D, Ruas M, Fuks F, Bye J, Chin SF, Milner J, Brown LA, Hsu F, Gilks B, Nielsen T, Schulzer M, Chia S, Ragaz J, Cahn A, Linger L, Ozdag H, Cattaneo E, Jordanova ES, Schuuring E, Yu DS, Venkitaraman A, Ponder B, Doherty A, Aparicio S, Bentley D, Theillet C, Ponting CP, Caldas C, Kouzarides T. EMSY links the BRCA2 pathway to sporadic breast and ovarian cancer. Cell. 2003;115(5):523–35.
Lambrechts D, Truong T, Justenhoven C, Humphreys MK, Wang J, Hopper JL, Dite GS, Apicella C, Southey MC, Schmidt MK, Broeks A, Cornelissen S, van Hien R, Sawyer E, Tomlinson I, Kerin M, Miller N, Milne RL, Zamora MP, Perez JI, Benitez J, Hamann U, Ko YD, Bruning T, GENICA Network, Chang-Claude J, Eilber U, Hein R, Nickels S, Flesch-Janys D, Wang-Gohrke S, John EM, Miron A, Winqvist R, Pylkas K, Jukkola-Vuorinen A, Grip M, Chenevix-Trench G, Beesley J, Chen X, Investigators kConFab, Australian Ovarian Cancer Study Group, Menegaux F, Cordina-Duverger E, Shen CY, Yu JC, Wu PE, Hou MF, Andrulis IL, Selander T, Glendon G, Mulligan AM, Anton-Culver H, Ziogas A, Muir KR, Lophatananon A, Rattanamongkongul S, Puttawibul P, Jones M, Orr N, Ashworth A, Swerdlow A, Severi G, Baglietto L, Giles G, Southey M, Marme F, Schneeweiss A, Sohn C, Burwinkel B, Yesilyurt BT, Neven P, Paridaens R, Wildiers H, Brenner H, Muller H, Arndt V, Stegmaier C, Meindl A, Schott S, Bartram CR, Schmutzler RK, Cox A, Brock IW, Elliott G, Cross SS, Fasching PA, Schulz-Wendtland R, Ekici AB, Beckmann MW, Fletcher O, Johnson N, Silva Idos S, Peto J, Nevanlinna H, Muranen TA, Aittomaki K, Blomqvist C, Dork T, Schurmann P, Bremer M, Hillemanns P, Bogdanova NV, Antonenkova NN, Rogov YI, Karstens JH, Khusnutdinova E, Bermisheva M, Prokofieva D, Gancev S, Jakubowska A, Lubinski J, Jaworska K, Durda K, Nordestgaard BG, Bojesen SE, Lanng C, Mannermaa A, Kataja V, Kosma VM, Hartikainen JM, Radice P, Peterlongo P, Manoukian S, Bernard L, Couch FJ, Olson JE, Wang X, Fredericksen Z, Alnaes GG, Kristensen V, Borresen-Dale AL, Devilee P, Tollenaar RA, Seynaeve CM, Hooning MJ, Garcia-Closas M, Chanock SJ, Lissowska J, Sherman ME, Hall P, Liu J, Czene K, Kang D, Yoo KY, Noh DY, Lindblom A, Margolin S, Dunning AM, Pharoah PD, Easton DF, Guenel P, Brauch H. 11q13 is a susceptibility locus for hormone receptor positive breast cancer. Hum Mutat. 2012;33(7):1123–32.
Chavali GB, Ekblad CM, Basu BP, Brissett NC, Veprintsev D, Hughes-Davies L, Kouzarides T, Itzhaki LS, Doherty AJ. Crystal structure of the ENT domain of human EMSY. J Mol Biol. 2005;350(5):964–73.
Raouf A, Brown L, Vrcelj N, To K, Kwok W, Huntsman D, Eaves CJ. Genomic instability of human mammary epithelial cells overexpressing a truncated form of EMSY. J Natl Cancer Inst. 2005;97(17):1302–6.
Garapaty S, Xu CF, Trojer P, Mahajan MA, Neubert TA, Samuels HH. Identification and characterization of a novel nuclear protein complex involved in nuclear hormone receptor-mediated gene regulation. J Biol Chem. 2009;284:7542–52.
Ezell SA, Polytarchou C, Hatziapostolou M, Guo A, Sanidas I, Bihani T, Comb MJ, Sourvinos G, Tsichlis PN. The protein kinase Akt1 regulates the interferon response through phosphorylation of the transcriptional repressor EMSY. Proc Natl Acad Sci U S A. 2012;109(10):E613–21.
Vire E, Curtis C, Davalos V, Git A, Robson S, Villanueva A, Vidal A, Barbieri I, Aparicio S, Esteller M, Caldas C, Kouzarides T. The breast cancer oncogene EMSY represses transcription of antimetastatic microRNA miR-31. Mol Cell. 2014;53(5):806–18.
Rodriguez C, Hughes-Davies L, Valles H, Orsetti B, Cuny M, Ursule L, Kouzarides T, Theillet C. Amplification of the BRCA2 pathway gene EMSY in sporadic breast cancer is related to negative outcome. Clin Cancer Res. 2004;10(17):5785–91.
Kirkegaard T, Nielsen KV, Jensen LB, Campbell FM, Muller S, Tovey SM, Brown S, Cooke TG, Bartlett JM. Genetic alterations of CCND1 and EMSY in breast cancers. Histopathology. 2008;52(6):698–705.
Brown LA, Johnson K, Leung S, Bismar TA, Benitez J, Foulkes WD, Huntsman DG. Co-amplification of CCND1 and EMSY is associated with an adverse outcome in ER-positive tamoxifen-treated breast cancers. Breast Cancer Res Treat. 2010;121(2):347–54.
Bane AL, Mulligan AM, Pinnaduwage D, O’Malley FP, Andrulis IL. EMSY and CCND1 amplification in familial breast cancer: from the Ontario site of the breast cancer family registry. Breast Cancer Res Treat. 2011;127(3):831–9.
Kornegoor R, Moelans CB, Verschuur-Maes AH, Hogenes MC, de Bruin PC, Oudejans JJ, Marchionni L, van Diest PJ. Oncogene amplification in male breast cancer: analysis by multiplex ligation-dependent probe amplification. Breast Cancer Res Treat. 2012;135:49–58.
Brown LA, Irving J, Parker R, Kim H, Press JZ, Longacre TA, Chia S, Magliocco A, Makretsov N, Gilks B, Pollack J, Huntsman D. Amplification of EMSY, a novel oncogene on 11q13, in high grade ovarian surface epithelial carcinomas. Gynecol Oncol. 2006;100(2):264–70.
Altinisik J, Karateke A, Coksuer H, Ulutin T, Buyru N. Expression of EMSY gene in sporadic ovarian cancer. Mol Biol Rep. 2011;38(1):359–63.
van Hattem WA, Carvalho R, Li A, Offerhaus GJ, Goggins M. Amplification of EMSY gene in a subset of sporadic pancreatic adenocarcinomas. Int J Clin Exp Pathol. 2008;1(4):343–51.
Nurminen R, Wahlfors T, Tammela TL, Schleutker J. Identification of an aggressive prostate cancer predisposing variant at 11q13. Int J Cancer. 2011;129(3):599–606.
Kuusisto KM, Bebel A, Vihinen M, Schleutker J, Sallinen SL. Screening for BRCA1, BRCA2, CHEK2, PALB2, BRIP1, RAD50, and CDH1 mutations in high-risk Finnish BRCA1/2-founder mutation-negative breast and/or ovarian cancer individuals. Breast Cancer Res. 2011;13(1):R20.
Kuusisto KM, Akinrinade O, Vihinen M, Kankuri-Tammilehto M, Laasanen S, Schleutker J. Copy number variation analysis in familial BRCA1/2-negative Finnish breast and ovarian cancer. PLoS One. 2013;8(8):e71802.
Syrjakoski K, Vahteristo P, Eerola H, Tamminen A, Kivinummi K, Sarantaus L, Holli K, Blomqvist C, Kallioniemi OP, Kainu T, Nevanlinna H. Population-based study of BRCA1 and BRCA2 mutations in 1035 unselected Finnish breast cancer patients. J Natl Cancer Inst. 2000;92(18):1529–31.
UCSC Genome Browser Home. [http://genome.ucsc.edu/]. Accessed 21 July 2017.
Kent WJ, Sugnet CW, Furey TS, Roskin KM, Pringle TH, Zahler AM, Haussler D. The human genome browser at UCSC. Genome Res. 2002;12(6):996–1006.
SNP Home. [http://www.ncbi.nlm.nih.gov/snp]. Accessed 21 July 2017.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81(3):559–75.
Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21(2):263–5.
Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, Higgins J, DeFelice M, Lochner A, Faggart M, Liu-Cordero SN, Rotimi C, Adeyemo A, Cooper R, Ward R, Lander ES, Daly MJ, Altshuler D. The structure of haplotype blocks in the human genome. Science. 2002;296(5576):2225–9.
PON-P2. [http://structure.bmc.lu.se/PON-P2/]. Accessed 21 July 2017.
Ward LD, Kellis M. HaploReg: a resource for exploring chromatin states, conservation, and regulatory motif alterations within sets of genetically linked variants. Nucleic Acids Res. 2012;40(Database issue):D930–4.
ENCODE Project Consortium, Bernstein BE, Birney E, Dunham I, Green ED, Gunter C, Snyder M. An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489(7414):57–74.
Boyle AP, Hong EL, Hariharan M, Cheng Y, Schaub MA, Kasowski M, Karczewski KJ, Park J, Hitz BC, Weng S, Cherry JM, Snyder M. Annotation of functional variation in personal genomes using RegulomeDB. Genome Res. 2012;22(9):1790–7.
Desmet FO, Hamroun D, Lalande M, Collod-Beroud G, Claustres M, Beroud C. Human splicing finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 2009;37(9):e67.
Benusiglio PR, Lesueur F, Luccarini C, McIntosh J, Luben RN, Smith P, Dunning A, Easton DF, Ponder BA, Pharoah PD. Common variation in EMSY and risk of breast and ovarian cancer: a case-control study using HapMap tagging SNPs. BMC Cancer. 2005;5:81.
Acknowledgements
The authors would like to thank Ms. Linda Enroth, Tiina Wahlfors, Ph.D., and Sanna-Kaisa Harjunen, M.Sc., for their assistance. The authors would also like to thank the cancer patients for their participation in this study and the personnel of the Tampere University Hospital Genetics Outpatient Clinic for assistance related to study material collection. The ENCODE data were obtained from the ENCODE consortium.
Funding
This work was financially supported by grants from the Competitive State Research Financing of the Expert Responsibility of Tampere University Hospital (#X51003), The Finnish Cancer Organisations, the Sigrid Juselius Foundation, and the Academy of Finland (#251074). The Funding body has no role in the design of the study or in collection, analysis, and interpretation of data or in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
KMM participated in patient collection, study design, performed laboratory analyses and drafted the manuscript. RN contributed to the study design, participated in laboratory analyses, performed statistical and bioinformatics analyses and drafted the manuscript. MKT and AK contributed study materials and critically reviewed the manuscript. S-LL and JS participated in the study design and coordination and critically reviewed the manuscript. S-LL also participated in patient collection and was responsible for the genetic counselling of patients. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients were informed of the analyses and provided written consent for the use of existing DNA samples in the present study. The Ethical Committees of Tampere and Turku University Hospitals and the National Authority for Medicolegal Affairs approved this research project.
Consent for publication
‘Not applicable’.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: Table S1.
Functional annotation of the location of the c.2709 + 122delT deletion. Table S2. The effect of the c.2709 + 122delT variant on splicing regulatory elements. (DOCX 16 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Määttä, K.M., Nurminen, R., Kankuri-Tammilehto, M. et al. Germline EMSY sequence alterations in hereditary breast cancer and ovarian cancer families. BMC Cancer 17, 496 (2017). https://doi.org/10.1186/s12885-017-3488-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-017-3488-x