Abstract
Background
Appropriate breastfeeding training for midwives is necessary to enhance their knowledge, attitude, and practice (KAP). However, evidence surrounding the effects of midwife breastfeeding training programmes is insufficient to draw a conclusion of its effectiveness on breastfeeding initiation, duration, and rates.
Objective
The aim of this systematic review was to identify, summarise, and critically analyse the available literature to evaluate the effects of midwife breastfeeding training programmes on the midwives’ KAP towards breastfeeding and breastfeeding initiation, duration and rates among postnatal mothers.
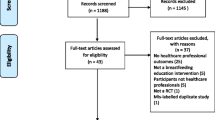
Methods
Nine English and six Chinese databases were searched with relevant key words. The methodological quality of the included studies were assessed by two reviewers independently using the Joanna Briggs Institute critical appraisal checklists.
Results
Nine English and one Chinese articles were included in this review. Five articles investigating midwives’ KAP towards breastfeeding reported positive results (p < 0.05). The meta-analysis revealed that breastfeeding training programmes significantly improved midwives’ breastfeeding-related knowledge and skills (standardised mean difference = 1.33; 95% confidence interval, 0.98 to 1.68; p < 0.01; I2 = 36%), as well as their attitude towards breastfeeding (p < 0.05). An additional five articles measured the effects of breastfeeding training programmes on the initiation, duration, and rates of breastfeeding among postnatal mothers. Following the implementation of a breastfeeding training programme for midwives, mothers had significantly longer durations of exclusive breastfeeding (p < 0.05), fewer breastfeeding challenges (p < 0.05) (e.g. breast milk insufficiency), and higher satisfaction with breastfeeding counselling (p < 0.01), and fewer infants received breast milk substitutes in their first week of life without medical reasons (p < 0.05) in the intervention group compared with the control group. However, no significant effects were seen on the initiation and rates of breastfeeding after implementation of the programmes.
Conclusions
This systematic review has demonstrated that midwife breastfeeding training programmes could improve midwives’ KAP towards breastfeeding. However, the breastfeeding training programmes had limited effects on breastfeeding initiation and rates. We suggest that future breastfeeding training programme should incorporate counselling skills alongside breastfeeding knowledge and skills training.
Review registration
This systematic review has been registered in the International prospective register of systematic reviews (PROSPERO) (ID: CRD42022260216).
Similar content being viewed by others
Introduction
Breastfeeding is a topic of global attention. It is considered as the best way to feed a baby and has been shown to have substantial short- and long-term benefits forboth mothers and infants [1,2,3,4,5,6]. In view of the beneficial effects of breastfeeding, the World Health Organisation (WHO)/ United Nations Children’s Fund (UNICEF) Global Strategy on Infant and Young Child Feeding specifically recommended that governments protect, promote, and support breastfeeding [7]. The World Health Assembly has also developed a ‘comprehensive plan for mother, infant and child nutrition’ with the goal of increasing the rate of exclusive breastfeeding during the first six months to at least 50% by 2025. In mainland China, the Chinese State Council stated in its Programme for the Development of Children in China (2011–2020) that the goal of having 50% of infants breastfeed exclusively during their first six months should be reached by year of 2020 [26,27,28,29]. Only one study measured the attitudes of midwives one year post training [25]. Moreover, factors such as policy changes and staff turnover may also affect long-term evaluation results. Therefore, to sustain the impact of such training programmes, regular in-service training is likely necessary.
The effects of breastfeeding training programmes on breastfeeding initiation, duration, and rates among postnatal mothers
The definition of exclusive breastfeeding varied in five studies in terms of how secondary outcomes were measured [30,31,32,33,34]. Two studies followed the WHO definition of breastfeeding: ‘exclusive breastfeeding means no other food or drink, not even water, except breastmilk (including milk expressed or from a wet nurse) for the first six months of life, with the exception of rehydration solution (ORS), drops and syrups (vitamins, minerals and medicines)’ [30, 34]. In contrast, three studies used the definition of breastfeeding provided by the National Board of Health and Welfare, which was revised to align with the WHO definition of breastfeeding: ‘exclusive breastfeeding is breastfeeding with occasional use of water, breast milk substitutes (not more than a few times), and/or solids (not more than one tablespoon per day)’ [31,32,33].
Additionally, the length of the follow-up period also varied among the studies. Three studies reassessed the outcomes at three days, three months, and nine months postpartum [31,32,33], while one study followedup at three, six, and 12 months postpartum, or until discontinued [30]. In contrast Shamim et al. was a pragmatic clustered RCT with repeated cross-sectional surveys conducted six months apart [34]. Therefore, meta-analysis of these studies was not possible, and the results should be interpreted with caution.
Three studies assessed breastfeeding initiation [30, 33, 34]. Shamim et al. and Zakarija-Grkovic et al. reported opposite results relating to breastfeeding initiation rate [30, 34]. In terms of the rate of exclusive breastfeeding, both Shamim et al. and Zakarija-Grkovic et al. reported that it was not statistically significantly different between the intervention and control groups [30, 34]. This suggests that the breastfeeding training programmes had limited effects on breastfeeding initiation and rates. In a systematic review by Balogun et al., among all six studies included, only one examined the effects of breastfeeding training programmes for healthcare professionals on secondary outcomes and reported that the rate of exclusive breastfeeding increased [18]. However, no statistically significant differences were found in breastfeeding initiation rates, which differed from the results of the current review.
For other secondary outcomes, longer breastfeeding durations [31, 33], less and later introduction of breast milk substitutes without medical reasons [31, 33, 34], fewer breastfeeding challenges [32, 33], and higher maternal satisfaction were reported [32, 33]. This suggests that breastfeeding training programmes for midwives were effective in improving some breastfeeding outcomes.
Breastfeeding training programme design
The results of this review suggest that the inclusion of counselling skills training, in addition to breastfeeding knowledge and skills training led to statistically significant positive effects on both primary and secondary outcomes. Besides, it was found that all training formats were effective in improving both primary and secondary outcomes.
Breastfeeding training programmes of different durations all resulted in increased KAP of midwives. Courses of longer duration correlated with more statistically significant effects on secondary outcomes [25, 31,32,33].
The course providers and teaching materials were often not reported. Despite this, the quality of the teachers and materials statistically significantly affected the effectiveness of the training programmes. More studies should be conducted to explore the effects of teachers’ characteristics (e.g. working years, experience, teaching ability) and teaching materials on breastfeeding training programme outcomes.
Limitations
Some limitations of this review should be noted. First, the literature in this field is limited and all of the included studies had some methodological weaknesses. Second, in this review, the breastfeeding training programmes varied widely in terms of target audience, duration, content, providers, materials, and teaching methods. Thus, subgroup analyses to compare the effects of training duration, course contents, teaching methods, and teacher characteristics were not feasible. In addition to the heterogeneity of the training programmes, the measurement tools, assessment strategies, and outcome definition also varied, making meta-analysis not feasible for many outcomes. Lastly, only studies published in Chinese or English were included in this review, and expanding the analysis to other languages may provide additional evidence to support our conclusions.
Conclusions
This systematic review has demonstrated that breastfeeding training programmes can improve midwives’ KAP towards breastfeeding. However, the breastfeeding training programmes had limited effects on breastfeeding initiation and rates.
More RCTs are required to explore the appropriate scientific content, methods, duration and provider of breastfeeding training for midwives, in addition to the effects of these variables on outcomes. Longitudinal studies are also warranted to examine the long-term effects of breastfeeding training programmes on midwives’ KAP, and breastfeeding initiation and rates towards breastfeeding. We suggest that future breastfeeding training programmes should incorporate counselling skills alongside breastfeeding knowledge and skills training.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Aguilar Cordero MJ, Madrid Banos N, Baena Garcia L, et al. Breastfeeding as a method to prevent cardiovascular diseases in the mother and the child. Nutricion Hospitalaria. 2015;31:1936–46. https://doi.org/10.3305/nh.2015.31.5.8810.
Amitay EL, Keinan-Boker L. Breastfeeding and childhood leukemia incidence: a meta-analysis and systematic review. JAMA Pediatr. 2015;169:e151025.
Chowdhury R, Sinha B, Sankar MJ, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatrica. 2015;104:96–113. https://doi.org/10.1111/apa.13102.
Debes AK, Kohli A, Walker N, et al. Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health. 2013;13(Suppl 3):19. https://doi.org/10.1186/1471-2458-13-s3-s19.
Qu G, Wang L, Tang X, et al. Association between duration of breastfeeding and maternal hypertension: A systematic review and meta-analysis. Breastfeed Med. 2018;13:318–26. https://doi.org/10.1089/bfm.2017.0180.
Rameez RM, Sadana D, Kaur S, et al. Association of maternal lactation with diabetes and hypertension: a systematic review and meta-analysis. JAMA Network Open. 2019;2:e1913401. https://doi.org/10.1001/jamanetworkopen.2019.13401.
WHO. Infant and young child nutrition: Global strategy on infant and young child feeding. 2020. https://apps.who.int/gb/archive/pdf_files/WHA55/ea5515.pdf?ua=1.
Chinese State Council. Development of Children in China (2011–2020). **nhua monthly report. 2011. p. 101–7.
UNICEF. From the first hour of life: A new report on infant and young child feeding. 2020. https://data.unicef.org/resources/first-hour-life-new-report-breastfeeding-practices/.
UNICEF. 2019 Global breastfeeding scorecard. 2020. http://www.fao.org/3/ca5162en/ca5162en.pdf.
UNICEF. Global breastfeeding scorecard. 2020. https://www.unicef.org/nutrition/index_100585.html.
Howe-Heyman A, Lutenbacher M. The Baby-Friendly Hospital Initiative as an intervention to improve breastfeeding rates: a review of the literature. J Midwifery Womens Health. 2016;61:77–102. https://doi.org/10.1111/jmwh.12376.
Kim SK, Park S, Oh J, et al. Interventions promoting exclusive breastfeeding up to six months after birth: A systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. 2018;80:94–105. https://doi.org/10.1016/j.ijnurstu.2018.01.004.
Perez-Escamilla R, Martinez JL, Segura-Perez S. Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Matern Child Nutr. 2016;12:402–17. https://doi.org/10.1111/mcn.12294.
de Almeida JM, de Araújo Barros Luz S, da Veiga Ued F. Support of breastfeeding by health professionals: integrative review of the literature. Revista Paulista de Pediatria (English Edition). 2015;33:355–62. https://doi.org/10.1016/j.rppede.2015.06.016.
Power ML, Locke E, Chapin J, et al. The effort to increase breast-feeding. J Reprod Med. 2003;48:72–8 2003/03/08.
Schanler RJ, O’Connor KG, Lawrence RA. Pediatricians’ practices and attitudes regarding breastfeeding promotion. Pediatrics. 1999;103:E35. https://doi.org/10.1542/peds.103.3.e35.
Balogun OO, Dagvadorj A, Yourkavitch J, et al. Health facility staff training for improving breastfeeding outcome: A systematic review for step 2 of the Baby-Friendly Hospital Initiative. Breastfeed Med. 2017;12:537–46. https://doi.org/10.1089/bfm.2017.0040.
de Jesus PC, de Oliveira MI, Fonseca SC. Impact of health professional training in breastfeeding on their knowledge, skills, and hospital practices: a systematic review. Jornal de Pediatria (Rio J). 2016;92:436–50. https://doi.org/10.1016/j.jped.2015.09.008.
Gavine A, MacGillivray S, Renfrew MJ, et al. Education and training of healthcare staff in the knowledge, attitudes and skills needed to work effectively with breastfeeding women: a systematic review. Int Breastfeed J. 2017;12. https://doi.org/10.1186/s13006-016-0097-2.
JBI. Critical appraisal tools. 2020. https://joannabriggs.org/critical-appraisal-tools.
Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted? Stat Med. 2002;21:1559–73. https://doi.org/10.1002/sim.1187.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. https://doi.org/10.1002/sim.1186.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. https://doi.org/10.1136/bmj.327.7414.557.
Ekström A, Widström AM, Nissen E. Process-oriented training in breastfeeding alters attitudes to breastfeeding in health professionals. Scand J Public Health. 2005;33(6):424–31. https://doi.org/10.1080/14034940510005923.
Moran VH, Bramwell R, Dykes F, et al. An evaluation of skills acquisition on the WHO/UNICEF Breastfeeding Management Course using the pre-validated Breastfeeding Support Skills Tool (BeSST). Midwifery. 2000;16:197–203. https://doi.org/10.1054/midw.2000.0214.
Law SM, Dunn OM, Wallace LM, Inch SA. Breastfeeding Best Start study: training midwives in a 'hands off' positioning and attachment intervention. Matern Child Nutr. 2007;3(3):194–205. https://doi.org/10.1111/j.1740-8709.2007.00083.x.
Wang H-H, Ku C-Y. Effectiveness of health education on nurses breastfeeding knowledge and attitude. J Health Manag. 2012;10:22–33.
Al-Nuaimi K, Ali R, Ali FH. The effect of a breastfeeding educational workshop on clinicans’ knowledge, attitudes and practices. Br J Midwifery. 2019;27:242–50.
Zakarija-Grkovic I, Šegvić O, Bozinovic T, et al. Hospital practices and breastfeeding rates before and after the UNICEF/WHO 20-hour course for maternity staff. J Hum Lact. 2012;28:389–99. https://doi.org/10.1177/0890334412447079.
Ekström A, Kylberg E, Nissen E. A process-oriented breastfeeding training program for healthcare professionals to promote breastfeeding: an intervention study. Breastfeed Med. 2012;7:85–92. https://doi.org/10.1089/bfm.2010.0084.
Blixt I, Martensson LB, Ekstrom AC. Process-oriented training in breastfeeding for health professionals decreases women’s experiences of breastfeeding challenges. Int Breastfeed J. 2014;9:15–15. https://doi.org/10.1186/1746-4358-9-15.
Ekström AC, Thorstensson S. Nurses and midwives professional support increases with improved attitudes - design and effects of a longitudinal randomized controlled process-oriented intervention. BMC pregnancy and childbirth. 2015;15:275. https://doi.org/10.1186/s12884-015-0712-z.
Shamim T, Dina F, Vitta B, et al. In a rural area of Bangladesh, traditional birth attendant training improved early infant feeding practices: a pragmatic cluster randomized trial. Matern Child Nutr. 2017;13:e12237. https://doi.org/10.1111/mcn.12237.
Moran VH, Dinwoodie K, Bramwell R, et al. The development andvalidation of the Breastfeeding Support Skills Tool (BeSST). Clin Effective Nurs. 1999;3:151–5.
Acknowledgements
The authors would like to acknowledge the support and contributions of the Liu Yuexin (Head nurse of the obstetric department, The First Affiliated Hospital of Sun Yat-sen University) to the review.
Funding
This systematic review was not funded by any institution, organisation or individual.
Author information
Authors and Affiliations
Contributions
Wang Tianci: conceptualisation (equal); data curation (lead); formal analysis (equal); methodology (equal); resources (equal); writing – original draft (equal); writing – review & editing (equal). Shang Meimei: formal analysis (equal); resources (equal). Chow Ka Ming: conceptualisation (equal); methodology (equal); project administration (lead); supervision (lead); writing – original draft (equal); writing – review & editing (equal). The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, T., Shang, M. & Chow, K.M. Effects of breastfeeding training programmes for midwives on breastfeeding outcomes: a systematic review and meta-analysis. BMC Pregnancy Childbirth 23, 262 (2023). https://doi.org/10.1186/s12884-023-05540-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05540-6