Abstract
Background
Hypertension has been known to increase the risk of obstetric complications. Recently, the American College of Cardiology endorsed lower thresholds for hypertension as systolic blood pressure of 130-139 mmHg or diastolic blood pressure 80-89 mmHg. However, there is a paucity of information regarding the impact of pre-pregnancy blood pressure on pregnancy outcomes. We aimed to evaluate the effect of pre-pregnancy blood pressure on maternal and neonatal complications.
Methods
In this nationwide, population based study, pregnant women without history of hypertension and pre-pregnancy blood pressure < 140/90 mmHg were enrolled. The primary outcome of composite morbidity was defined as any of the followings: preeclampsia, placental abruption, stillbirth, preterm birth, or low birth weight.
Results
A total of 375,305 pregnant women were included. After adjusting for covariates, the risk of composite morbidity was greater in those with stage I hypertension in comparison with the normotensive group (systolic blood pressure, odds ratio = 1.68, 95% CI: 1.59 – 1.78; diastolic blood pressure, odds ratio = 1.56, 95% CI: 1.42 – 1.72). There was a linear association between pre-pregnancy blood pressure and the primary outcome, with risk maximizing at newly defined stage I hypertension and with risk decreasing at lower blood pressure ranges.
Conclusions
‘The lower, the better’ phenomenon was still valid for both maternal and neonatal outcomes. Our results suggest that the recent changes in diagnostic thresholds for hypertension may also apply to pregnant women. Therefore, women with stage I hypertension prior to pregnancy should be carefully observed for adverse outcomes.
Similar content being viewed by others
Background
Hypertension (HTN) is defined as an elevated blood pressure (BP) state, which can cause adverse effects if left untreated. Traditionally, guidelines have defined HTN as BP ≥ 140/90 mmHg, based on evidence from randomized clinical trials that treatment-induced BP reductions were beneficial at this threshold [1]. However, epidemiologic data have shown that the risk of cardiovascular disease already begins to rise above 120/80 mmHg [2]. Moreover, the SPRINT trial showed that even patients who were clinically believed to have prehypertension had increased risks of cardiovascular events [3]. These findings led to the lowering of BP thresholds for HTN diagnosis and treatment [2].
In the normal BP range, data regarding the impact of BP on cardiovascular risk have been inconsistent. Some studies have reported a linear relationship between BP and cardiovascular risk, showing progressive reductions in cardiovascular risk with decreasing BP [4, 5]. Others have proposed that a J-curve association exists between BP and cardiovascular risk specifically in those with coronary artery disease, suggesting that not only high, but low BP can also increase the risk of cardiovascular disease [6, 7].
In the case of pregnant women, HTN before pregnancy is a well-known risk factor for increased obstetric complications [8,9,10]. And blood pressure patterns in early pregnancy have been studied to be associated with an increased risk of hypertensive disorders during pregnancy which is common cause of maternal death [11, 12]. Having a persistently elevated diastolic BP (DBP ≥ 110 mmHg) despite therapy is a severe risk factor for pregnant women that affects pregnancy outcomes [13]. And whether lower thresholds for hypertension endorsed by the American College of Cardiology (ACC) can be applied to women has not yet been determined. Few studies have studied the impact of lower thresholds during pregnant period on diagnosis of preeclampsia and other pregnancy outcomes [14,15,16].
However, there is a paucity of information regarding the impact of pre-pregnancy BP on pregnancy outcomes. Moreover, the potential risk of stage I HTN before pregnancy has not been well examined. The current study was designed (1) to evaluate the effect of pre-pregnancy blood pressure on maternal and neonatal complications and (2) to determine whether there is a linear association between pre-pregnancy blood pressure and obstetric outcomes using a nationwide, population-based cohort.
Methods
Study population
Data on the study population was acquired from the Korean Health Insurance Review and Assessment (HIRA) service database. The Korean healthcare system is a single-payer system. Most of the population (97%) are registered with the National Health Insurance Service (NHIS), and all claims data are collected at HIRA. The database contains demographic, socioeconomic, diagnostic, procedural, and prescription information for its 50 million beneficiaries. Additionally, data from the bi-annual National Health Screening Examination (NHSE) provided by the NHIS, and the National Health Screening Program for Infants and Children (NHSP-IC) were used to assess pre-pregnancy BP and neonatal outcomes. The NHSP-IC, initiated in 2007, includes data on physical examination, anthropometric values, and results from developmental screening. All databases are open to researchers upon approval of their study protocols. The study was also approved by the Institutional Review Board of the Korean University Guro Hospital (No. 2020GR0105).
Study design
The study population consisted of pregnant Korean women who met the following criteria: (1) singleton pregnancy; (2) delivery between 2007 and 2015; (3) participation in the NHSE within 6 months prior to pregnancy; and (4) pre-pregnancy BP < 140/90 mmHg. Women with multifetal pregnancies, pre-pregnant HTN, and those who lacked detailed clinical information were excluded from the study. Pre-pregnancy HTN was defined as having systolic BP (SBP) ≥ 140 mmHg, DBP ≥ 90 mmHg, or an International Classification of Diseases-10th Revision (ICD-10) code for HTN (I10 – I15). Stage I HTN was defined as having an SBP 130 – 139 mmHg or DBP 80 – 89 mmHg, according to the ACC guidelines [2]. Women were excluded from analysis for neonatal outcome if their offspring had not undergone at least one of the seven consecutive NHSP-IC health examinations.
National health screening examination before pregnancy
Pre-pregnancy factors were collected using the NHSE database. The NHSE database is comprised of two components (health interview and health examination). The health interview questions contain information on demographics, socioeconomic status, and lifestyle. The smoking status before pregnancy was self-reported. The health examination includes physical examination and laboratory tests. Blood pressure was measured in the seated position using semi-automated sphygmomanometers, after at least 5 minutes of rest. Mean arterial pressure was calculated as 1/3(SBP) + 2/3(DBP). Blood samples were collected after at least 8 hours fasting, and aspartate aminotransferase (AST), alanine aminotransferase (ALT), and cholesterol levels were used for the analysis. The cohort profile and accuracy of the NHSE database have been described previously [17].
Pregnancy and neonatal outcomes
Using the HIRA database, women with preeclampsia, placenta abruptio, or stillbirth during their pregnancy were identified by ICD-10 diagnostic codes. Data on neonatal outcomes, such as preterm birth and birth weight, were acquired from the NHSP-IC database. The primary outcome, which was composite morbidity, included preeclampsia, placenta abruptio, stillbirth, preterm birth, and low birth weight, [8, 18, 19] which have been reported to be increased in hypertensive pregnant women. Additional maternal outcomes, such as cesarean section, gestational diabetes mellitus (GDM), postpartum hemorrhage, and placenta previa, were also assessed. Finally, neonatal sex and birth weight were also included as neonatal outcomes.
Statistical analysis
Shapiro-Wilk test was performed to assess normality distribution. The continuous variables are described as mean and standard deviation (SD), and compared by Student’s t-test or ANOVA for multiple group comparisons. The categorical variables are given as numbers and percentages and compared using the chi-square test. The study subjects were categorized into six groups by SBP, DBP, and me, and the risk of the outcomes was estimated for each group using an SBP of 110 – 119 mmHg, a DBP of 75 –59 mmHg, and a mean arterial pressure of 90 – 94 mmHg as references. Multivariate logistic regression analysis was used to estimate the adjusted odds ratios (OR) and 95% confidence intervals (CI). We included age, parity, obesity, high liver function test, high cholesterol, smoking, overt DM which are known predictors of preeclampsia and obstetrical complications as covariates [20,21,22,23] and that are differed when univariate analysis according to BP. Previous studies have demonstrated that the risk of develo** HTN was higher in obese people, and that adiposity was related to the development of HTN. To evaluate this hypothesis, subgroup analysis was performed for different BMI values to adjust for the effect of obesity. The subjects were divided into three groups according to the Asian-Pacific cutoff points for BMI from the World Health Organization (WHO) [24]. For exploratory purposes, the relationships between BP and obstetric outcomes were also assessed by a restricted cubic splines [25]. The analyses were performed using SPSS version 23.0 (IBM Inc., Armonk, NY, USA), and a P-value of < 0.05 was considered statistically significant.
Results
Baseline characteristics
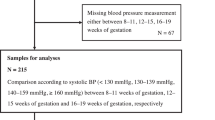
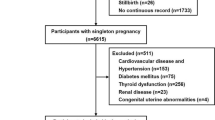
A total of 398,199 pregnant women who delivered between 2007 and 2015, and those who also underwent health examinations within 6 months prior to pregnancy were screened. Among the subjects screened, subjects with multi-fetal pregnancies (n = 5920), pre-existing HTN (n = 16,472), and those with missing data (n = 502) were excluded. The final cohort comprised of 375,305 subjects, as shown in Fig. 1. Women were excluded from the neonatal outcome analysis if their offspring had not undergone at least one of the seven consecutive NHSP-IC health examinations.
Table 1 describes the baseline characteristics of the study population. The mean pre-pregnancy SBP was 109.7 ± 10.4 mmHg and the DBP was 68.9 ± 7.7 mmHg. As expected, the study population was healthy young subjects with a low prevalence of comorbidities (diabetes, 4.03%; dyslipidemia, 2.52%; and current smoker, 2.87%). The baseline characteristics were compared between women with stage I HTN (SBP 130 – 139 mmHg or DBP 80 – 89 mmHg) and those with not (SBP < 130 mmHg and DBP < 80 mmHg). Women with stage I HTN had a higher body mass index (BMI), a higher frequency of comorbidities, and increased levels of AST, ALT, and total cholesterol compared to normotensive women (Tables 2, 3).
Pregnancy outcomes
Pregnancy and neonatal outcomes were assessed according to the pre-pregnancy BP categories. Having a pre-pregnancy SBP ≥ 130 mmHg significantly increased the risk for composite morbidity compared to an SBP of 110 – 119 mmHg (OR = 1.681, 95% CI: 1.586 – 1.783). Having a pre-pregnancy DBP (≥ 85 mmHg) also increased the risk of the primary outcome compared to a DBP of 75 – 79 mmHg (OR = 1.560, 95% CI: 1.420 – 1.715). Even at normal and elevated BP (< 130/80 mmHg), lower BP was associated with a significantly lower risk of the primary outcome. This linear relationship between BP and composite morbidity was consistent in the SBP, DBP, and mean arterial pressure categories, and also after adjusting for covariates (Tables 4, 5 and 6). The relationship between the risk of the composite morbidity and BP values is visualized in Fig. 2 using restricted cubic splines.
Subgroup analysis
Subgroup analysis was performed using pre-pregnancy BMIs. The subjects were categorized into three groups: underweight (< 18.5 kg/m2), normal (18.5 – 22.9 kg/m2), and overweight/obese (≥ 23 kg/m2). The linear relationship between pre-pregnancy BP and composite morbidity was consistent across all BMI subgroups and BP components, but the rate of increase was greater in overweight or obese women (pre-pregnancy BMI ≥ 23 kg/m2) (Fig. 3).
Pregnancy and neonatal outcomes according to pre-pregnancy BP
The incidence rates of the primary outcome and its components, and additional maternal outcomes according to BP values are shown in Tables 7, 8 and 9. Higher SBP was associated with increased rates of cesarean sections, preeclampsia, and GDM, whereas no significant differences were observed for postpartum hemorrhage, placental abruption, or placenta previa. For neonatal outcomes, significant increases in preterm birth, and low birth weight were observed in patients with higher SBP. The association between BP and outcomes was also consistent for the DBP and mean arterial pressure, except for postpartum hemorrhage, showing significantly increased events at higher DBP and mean arterial pressure. Figure 4 shows the incidence of the primary outcome and preeclampsia according to baseline systolic and diastolic BPs. Both systolic and diastolic BP was associated with the incidence of preeclampsia, with the highest incidence observed at SBPs of 130 – 139 mmHg and DBPs of 85 – 89 mmHg.
Discussion
Principle Findings
The current analysis of a large number of pregnant women found that (1) women with pre-pregnancy stage I HTN (SBP ≥ 130 mmHg or DBP ≥ 85 mmHg) had a significantly increased risk of composite morbidity; (2) there was a linear relationship between BP and risk of composite morbidity, with a progressive decrease in risk at lower BP observed even in women with normal BP; (3) the relationship between pre-pregnancy BP and composite morbidity was consistent across various BMI subgroups, with the steepest slope observed in overweight/obese women; and (4) both SBP and DBP were associated with increased risks for preeclampsia and composite morbidity.
Results
The risk of cardiovascular disease is known to increase with increases in BP, and lowering BP reduces this risk in hypertensive patients [26, 27]. Traditionally, the threshold at which BP interventions have been beneficial has been 140/90 mmHg. Those with prehypertension or elevated BP, are at an increased risk of develo** HTN, but no benefit has been observed with treatment. However, recent ACC/AHA guidelines changed the HTN threshold to ≥130/80 mmHg as a result of the SPRINT trial [2]. It is still debatable whether subjects with borderline BP will benefit from intensive treatment, and whether this threshold can also be applied to younger, healthier subjects. Using a large, nationwide database, we were able to analyze the effect of stage I hypertension on maternal and neonatal outcomes in young, healthy women.
The obstetric risk of stage I HTN was also reported in a study by Reddy et al. In this study, stage I HTN during pregnancy was associated with an increased risk of preeclampsia, preterm birth and adverse perinatal outcomes, showing the clinical risk of stage I HTN during pregnancy [16]. And other studies showed that use of newly endorsed lower BP thresholds has been shown to better identify the risk of preeclampsia [14, 15], gestational diabetes and preterm birth [28]. In the current study, we evaluated the significance of pre-pregnancy stage I HTN and demonstrated that having elevated BP prior to pregnancy significantly affected maternal and neonatal outcomes and that the risk of preeclampsia also increased.
Until now, the clinical significance of stage I HTN in the pre-pregnancy period has not been well studied. In the current study, pre-pregnancy stage I HTN significantly increased the composite morbidity of the mother and fetus, increasing the risk of outcomes, such as preeclampsia, placental abruption, stillbirth, preterm birth, and low birth weight. The incidence of composite morbidity and preeclampsia was high, at 12 and 7%, respectively, in women with stage I HTN. As the current guidelines have yet to identify this group as having increased risk, we believe that these women should be intensively monitored during pregnancy and that they may be candidates for prevention treatment, such as aspirin prophylaxis.
As pregnancy is the window period used to assess future ardiovascular risk [29], we tried to evaluate the occurrence of pregnancy complications in women with BP < 140/90 mmHg. In pregnant women, the lowest obstetric risk was observed in the lowest BP category, showing a ‘the lower, the better’ association.
Clinical and Research implications
In this study, we defined composite morbidity as outcomes including preeclampsia, placental abruption, stillbirth, preterm birth, and low birth weight. These maternal and neonatal outcomes are well-known adverse events associated with chronic HTN [8, 18, 19]. Theoretically, elevated BP during pregnancy is a risk factor for adverse pregnancy outcomes because several conditions, such as preterm birth, small-for-gestational age, uteroplacental insufficiency, and gestational HTN or preeclampsia, are related to elevated BP. Our results suggest that the recent changes in diagnostic thresholds for HTN may also apply to pregnant women. Although the newly endorsed stage I HTN before pregnancy showed a worsening of pregnancy outcome, in the current study we did not confirm that the use of antihypertensive drugs in stage I HTN improved the prognosis. On this basis, there is a need for future prospective clinical trials to evaluate the benefits of intensive preventive treatment.
Another issue to consider is whether different BP components, systolic, diastolic or mean arterial pressure, correlate better with adverse outcomes. In non-pregnant adults, systolic BP is the main component in diagnosing and treating HTN. However, in pregnant women, DBP has also been considered to be important in diagnosing and initiating treatment [30]. In our analysis, all systolic, diastolic, and mean arterial pressures were significantly associated with composite morbidity.
In a subgroup analysis according to pre-pregnancy BMI, the linear relationship between BP and composite morbidity was consistent across the various BMI groups. Previous studies have demonstrated that the risk of develo** HTN was higher in obese people, and BMI itself can affect pregnancy outcomes [31,32,33,34]. In the overweight/obese group, defined as a pre-pregnancy BMI of ≥23 kg/m2, a steep slope was observed between pre-pregnancy BP and composite morbidity. This finding suggests the increased effects of BP changes on outcomes in obese, pregnant women. Therefore, overweight women with stage I HTN prior to pregnancy should be carefully observed for adverse outcomes.
Strengths and Limitations
Our study had several strengths and limitations. This is a large-scale study that systematically evaluated the obstetrical outcome after pregnancy according to the pre-pregnancy BP category. Women of childbearing age are usually healthy and young, and it is rare to check their BP or undergo health check-ups. Therefore, it is difficult to conduct a study to confirm the outcome of BP before pregnancy. However, due to a government-paid, bi-annual health screening examination, we were able to acquire data on pre-pregnancy BP and assess its correlation with composite morbidity in a large cohort. In addition, systolic, diastolic, and mean arterial pressure were separately analyzed to examine the effect each BP component had on the outcome. The study also has a limitation in its retrospective design. As it is not mandatory to undergo health examinations, we cannot exclude the possibility of selection bias. Furthermore, incorrect or failure to input appropriate diagnostic codes might have led to an underestimation of events. And we could not handle all the predisposing conditions to preeclampsia and adverse pregnancy outcomes, medication history and social economic status that may affect results. A well-designed prospective study is needed to better assess the relationship between pre-pregnancy BP and outcomes. Pre-pregnancy stage I HTN was associated with an increased risk of maternal and neonatal adverse outcomes. ‘The lower, the better’ phenomenon was still valid for both maternal and neonatal outcomes.
Conclusions
There was a linear association between pre-pregnancy blood pressure and the maternal and neonatal outcomes, with risk maximizing at newly defined stage I hypertension and with risk decreasing at lower blood pressure ranges. Our results suggest that the recent changes in diagnostic thresholds for HTN may also apply to pregnant women. Therefore, women with stage I HTN prior to pregnancy should be carefully observed for adverse outcomes.
Availability of data and materials
The data that support the findings of this study are available from the National Health Insurance Service (NHIS), but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are however available from the author (Geum Joon Cho) upon reasonable request and with permission of the NHIS. The results do not necessarily represent the opinion of the National Health Insurance Corporation.
Abbreviations
- HTN:
-
Hypertension
- BP:
-
Blood pressure
- DBP:
-
Diastolic blood pressure
- HIRA:
-
Health Insurance Review and Assessment
- NHIS:
-
National Health Insurance Service
- NHSE:
-
National Health Screening Examination
- NHSP-IC:
-
National Health Screening Program for Infants and Children
- ICD-10:
-
International Classification of Diseases-10th Revision
- SBP:
-
Systolic blood pressure
- ACC:
-
Amerian College of Cardiology
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- GDM:
-
Gestational diabetes mellitus
- SD:
-
Standard deviation
- OR:
-
Odds ratio
- CI:
-
Confidence intervals
- WHO:
-
World Health Organization
- BMI:
-
Body mass index
References
Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019;25(1):20.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–248.
Group SR, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373(22):2103–16.
Rutan GH, McDonald RH, Kuller LH. A historical perspective of elevated systolic vs diastolic blood pressure from an epidemiological and clinical trial viewpoint. J Clin Epidemiol. 1989;42(7):663–73.
Turnbull F, Kengne AP, MacMahon S. Blood pressure and cardiovascular disease: tracing the steps from Framingham. Prog Cardiovasc Dis. 2010;53(1):39–44.
Bangalore S, Messerli FH, Wun CC, Zuckerman AL, DeMicco D, Kostis JB, et al. Treating to New Targets Steering C, Investigators: J-curve revisited: An analysis of blood pressure and cardiovascular events in the Treating to New Targets (TNT) Trial. Eur Heart J. 2010;31(23):2897–908.
Messerli FH, Panjrath GS. The J-curve between blood pressure and coronary artery disease or essential hypertension: exactly how essential? J Am Coll Cardiol. 2009;54(20):1827–34.
Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301.
Nzelu D, Dumitrascu-Biris D, Nicolaides KH, Kametas NA. Chronic hypertension: first-trimester blood pressure control and likelihood of severe hypertension, preeclampsia, and small for gestational age. Am J Obstet Gynecol. 2018;218(3):337.e331–7.
Wadhwani P, Saha PK, Kalra JK, Gainder S, Sundaram V. A study to compare maternal and perinatal outcome in early vs. late onset preeclampsia. Obstet Gynecol Sci. 2020;63(3):270–7.
Gunderson EP, Greenberg M, Nguyen-Huynh MN, Tierney C, Roberts JM, Go AS, et al. Early Pregnancy Blood Pressure Patterns Identify Risk of Hypertensive Disorders of Pregnancy Among Racial and Ethnic Groups. Hypertension. 2021; Hypertensionaha12118568.
Lee KJ, Sohn S, Hong K, Kim J, Kim R, Lee S, et al. Maternal, infant, and perinatal mortality statistics and trends in Korea between 2009 and 2017. Obstet Gynecol Sci. 2020;63(5):623–30.
Cunningham FG, Leveno KJ, Bloom SL, Dashe JS, Spong CY, Hoffman BL, et al. Williams obstetrics. 25th ed. New York, New York, N.Y: McGraw Hill Medical; 2018.
Hu J, Li Y, Zhang B, Zheng T, Li J, Peng Y, et al. Impact of the 2017 ACC/AHA Guideline for High Blood Pressure on Evaluating Gestational Hypertension-Associated Risks for Newborns and Mothers. Circ Res. 2019;125(2):184–94.
Hauspurg A, Parry S, Mercer BM, Grobman W, Hatfield T, Silver RM, et al. Blood pressure trajectory and category and risk of hypertensive disorders of pregnancy in nulliparous women. Am J Obstet Gynecol. 2019;221(3):277.e271–8.
Reddy M, Rolnik DL, Harris K, Li W, Mol BW, Da Silva CF, et al. Challenging the definition of hypertension in pregnancy: a retrospective cohort study. Am J Obstet Gynecol. 2020;222(6):606 e601–21.
Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017;7(9):e016640.
Sibai BM, Lindheimer M, Hauth J, Caritis S, VanDorsten P, Klebanoff M, et al. Risk factors for preeclampsia, abruptio placentae, and adverse neonatal outcomes among women with chronic hypertension. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;339(10):667–71.
Ananth CV, Basso O. Impact of pregnancy-induced hypertension on stillbirth and neonatal mortality. Epidemiology. 2010;21(1):118–23.
Wright D, Syngelaki A, Akolekar R, Poon LC, Nicolaides KH. Competing risks model in screening for preeclampsia by maternal characteristics and medical history. Am J Obstet Gynecol. 2015;213(1):62.e61–10.
Bdolah Y, Elchalal U, Natanson-Yaron S, Yechiam H, Bdolah-Abram T, Greenfield C, et al. Relationship between nulliparity and preeclampsia may be explained by altered circulating soluble fms-like tyrosine kinase 1. Hypertens Pregnancy. 2014;33(2):250–9.
Kozic JR, Benton SJ, Hutcheon JA, Payne BA, Magee LA, von Dadelszen P. Abnormal liver function tests as predictors of adverse maternal outcomes in women with preeclampsia. J Obstet Gynaecol Can. 2011;33(10):995–1004.
Spracklen CN, Saftlas AF, Triche EW, Bjonnes A, Keating B, Saxena R, et al. Genetic Predisposition to Dyslipidemia and Risk of Preeclampsia. Am J Hypertens. 2015;28(7):915–23.
Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29(9):1037–57.
Heerspink HJ, Ninomiya T, Zoungas S, de Zeeuw D, Grobbee DE, Jardine MJ, et al. Effect of lowering blood pressure on cardiovascular events and mortality in patients on dialysis: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2009;373(9668):1009–15.
Weber MA, Lackland DT. Hypertension: Cardiovascular benefits of lowering blood pressure. Nat Rev Nephrol. 2016;12(4):202–4.
Sutton EF, Hauspurg A, Caritis SN, Powers RW, Catov JM. Maternal Outcomes Associated With Lower Range Stage 1 Hypertension. Obstet Gynecol. 2018;132(4):843–9.
Paauw ND, van Rijn BB, Lely AT, Joles JA. Pregnancy as a critical window for blood pressure regulation in mother and child: programming and reprogramming. Acta Physiol (Oxford). 2017;219(1):241–59.
Higgins JR, de Swiet M. Blood-pressure measurement and classification in pregnancy. Lancet. 2001;357(9250):131–5.
Stamler J. Epidemiologic findings on body mass and blood pressure in adults. Ann Epidemiol. 1991;1(4):347–62.
Kannel WB, Brand N, Skinner JJ Jr, Dawber TR, McNamara PM. The relation of adiposity to blood pressure and development of hypertension. The Framingham study. Ann Intern Med. 1967;67(1):48–59.
Jeffreys M, Lawlor DA, Galobardes B, McCarron P, Kinra S, Ebrahim S, et al. Lifecourse weight patterns and adult-onset diabetes: the Glasgow Alumni and British Women's Heart and Health studies. Int J Obes. 2006;30(3):507–12.
Salihu HM, Garcia BY, Dongarwar D, Maiyegun SO, Yusuf KK, Agili DEA. Maternal pre-pregnancy underweight and the risk of small-for-gestational-age in Asian-American ethnic groups. Obstet Gynecol Sci. 2021;64(6):496–505.
Acknowledgements
Not applicable.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0502) and a grant (0320210230) from the Seoul National University Hospital research fund.
Author information
Authors and Affiliations
Contributions
YMJ, GCO, EN, HYL, MJO, JSP, JKJ, SML and GJC conceived the study and designed the experiment. YMJ, GCO, EN, HYL, MJO, JSP, JKJ, SML and GJC contributed the collection of data and performed the experiment. YMJ, GCO, EN, SML and GJC analyzed the data and contributed to the statistical analysis. YMJ, GCO, SML and GJC wrote the article. All authors critically revised the article and gave approval of the version to be published.
Corresponding authors
Ethics declarations
Ehics approval and consent to participate
The study was also approved by the Institutional Review Board of the Korean University Guro Hospital (No. 2020GR0105). All methods were performed according to the Declaration of Helsinki. Anonymized and deidentified information for participants was used for analysis, so the requirement for informed consent or parental permission was waived by the Institutional Review Board of the Korean University Guro Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jung, Y.M., Oh, G.C., Noh, E. et al. Pre-pregnancy blood pressure and pregnancy outcomes: a nationwide population-based study. BMC Pregnancy Childbirth 22, 226 (2022). https://doi.org/10.1186/s12884-022-04573-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04573-7