Abstract
Background
Serum uric acid (UA) and the neutrophil-to-lymphocyte ratio (NLR) have been reported to be associated with outcomes in acute ischemic stroke (AIS). However, whether UA is related to the prognosis of AIS patients undergoing intravenous thrombolysis (IVT) remains inconclusive. We sought to explore the combined effect of UA and NLR on the prognosis of AIS treated with IVT.
Methods
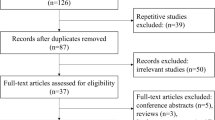
A total of 555 AIS patients receiving IVT treatment were enrolled. Patients were categorized into four groups according to the levels of UA and NLR: LNNU (low NLR and normal UA), LNHU (low NLR and high UA), HNNU (high NLR and normal UA), and HNHU (high NLR and high UA). Multivariable logistic regression analysis was used to evaluate the value of serum UA level and NLR in predicting prognosis. The primary outcomes were major disability (modified Rankin scale (mRS) score 3–5) and death within 3 months.
Results
After multivariate adjustment, a high NLR (≥ 3.94) increased the risk of 3-month death or major disability (OR, 2.23; 95% CI, 1.42 to 3.55, p < 0.001). However, there was no statistically significant association between a high UA level (≥ 313.00 µmol/L) and clinical outcome. HNHU was associated with a 5.09-fold increase in the risk of death (OR, 5.09; 95% CI, 1.31–19.83; P value = 0.019) and a 1.98-fold increase in the risk of major disability (OR, 1.98; 95% CI 1.07–3.68; P value = 0.030) in comparison to LNNU.
Conclusions
High serum UA levels combined with high NLR were independently associated with 3-month death and major disability in AIS patients after IVT.
Similar content being viewed by others
Introduction
Acute ischemic stroke (AIS) remains the second leading cause of both disability and death worldwide. Intravenous thrombolysis (IVT) with recombinant tissue plasminogen activator (rt-PA) is considered to be the most effective medical reperfusion treatment within 4.5 h of symptom onset in AIS patients. However, the prognosis of patients with AIS after IVT may be affected by modifiable factors such as C-reactive protein, white blood cell count and neutrophil-lymphocyte ratio (NLR) [1,2,3,4]. Hence, useful biomarker detection is essential for early risk assessment and effective treatment after IVT.
Uric acid (UA), the end product of purine metabolism in humans, is a major endogenous antioxidant with neuroprotective effect in the blood and an easily detectable and reliable biomarker in clinical practice [5]. However, it can also act as a pro-oxidant depending on the chemical microenvironment [6]. The role of UA in the prognosis of stroke is also conflicting [7]. With respect to preclinical studies, when serum UA levels were elevated, reduced brain damage and improved functional outcome were shown in a transgenic mouse (UOX+/-) model of focal ischemic stroke [8]. Moreover, a systematic review and meta-analysis of rodent data showed that UA significantly reduced infarct size and neurofunctional deficits [9]. With regard to AIS patients, the tertiary analysis of the URICO-ICTUS trial suggested that the combination of rt-PA and UA may prevent early ischemic deterioration [10]. In addition, a low serum UA level at Days 3 and 4 of onset was reported to be negatively associated with DWI volume at diagnosis [11]. Nevertheless, a retrospective study suggested that a high level of UA [≥ 340 µmol/L (5.712 mg/dl)] was related to stroke recurrence in older patients [12]. Furthermore, a U-shaped relationship between UA and functional outcomes in patients with AIS was found by Zhang and colleagues [13]. Patients with higher serum UA levels (> 380 µmol/L) or lower serum UA levels (≤ 250 µmol/L) were more likely to have a poor outcome compared to the baseline group (UA level 316–380 µmol/L). Some prospective cohort studies demonstrated that higher serum uric acid levels were associated with 3-month better functional outcome in AIS patients with IVT [14, 15]. Notably, a meta-analysis showed that there was no significant correlation between serum UA levels and the prognosis of AIS [16]. Thus, it is important to clarify the relationship between UA and the prognosis of AIS patients undergoing IVT [7, 26]. Our results showed that a high NLR level was an independent predictor for poor clinical outcome in AIS after IVT, and this is in line with our previous study [2].
The correlation between UA and NLR has gained substantial attention recently. One study showed that the NLR was positively correlated with UA in patients with chronic kidney disease [27]. However, in a study on multiple sclerosis, a negative correlation was observed between the NLR and UA [28]. The findings of the same study indicated that combined evaluation of NLR and UA may be a more effective approach in determining disability in patients with multiple sclerosis than assessing these parameters separately. These studies showed that there is a correlation between UA and the NLR, but this correlation may vary in different diseases. Previous studies have demonstrated that both UA and NLR are closely related to AIS, but few studies have examined UA, NLR, and AIS together. A recent study suggested that patients with high UA and high NLR levels are at greater risk for AIS recurrence [12]. Our study explored the combined effect of NLR and UA on the outcomes of AIS patients after IVT, and we found that high NLR and serum UA levels are associated with increased risks of 3-month major disability and death. The possible mechanisms are oxidation and inflammation.
In general, the reference interval of serum UA is 1.5 to 6.0 mg/dl in women and 2.5 to 7.0 mg/dl in men. Hyperuricemia is defined as a serum UA level greater than 6.0 mg/dL in women and 7.0 mg/dL in men [29]. Only suitable concentrations of serum UA may have a protective effect. In our study, the demarcation point of UA was 313 µmol/L (5.3 mg/dl). One dose‒response study showed a J-shaped trend between ascending UA levels and a higher risk of suffering from ischemic stroke. When the UA reached 5.25 mg/dl, it started to become statistically significant [30]. Therefore, it is reasonable to speculate that the high level of UA (> 5.3 mg/dl) acts as a pro-oxidant. A previous experimental study showed that increased UA (> 6 mg/dl) was associated with endothelial dysfunction and increased oxidative stress [31].
UA can also induce inflammation. A population study reported a positive relationship between serum UA and acute-phase reactants, such as C-reactive protein, fibrinogen and complement C3 [32]. The same study also examined the effect of UA on the expression of inflammatory biomarkers in vitro and found that hyperuricemia might induce inflammation by activating the proinflammatory NF-κB signaling cascade. Another study found that hyperuricemia (up to 50 mg/dL) can exacerbate chronic inflammation by altering the balance of interleukin-1β/interleukin-1Ra [33]. Moreover, elevated UA (9 mg/dl) was reported to induce vascular inflammation by upregulating the (pro) renin receptor in human umbilical vein endothelial cells [34]. Inflammatory biomarkers such as C-reactive protein and fibrinogen are upregulated following AIS [2]. The correlations of these biomarkers with increased mortality and poor functional outcome of stroke have been reported. Thus, we speculate that high UA may exacerbate poor prognosis in AIS patients with a high NLR through oxidation and inflammation.
UA and NLR were easily accessible biomarkers of oxidative stress and inflammation from daily blood examinations and can be easily translated into clinical practice. To date, no studies have investigated the relationship between the combined effect of UA and NLR and the outcomes of AIS patients after IVT. This is the innovative point and a major strength of this research. However, several limitations should also be noted. First, this study was a single-center study, and the population was relatively small, which may limit the generalization of our findings. Second, a subgroup analysis with stratification by sex was not performed to assess the effect of UA on the prognosis of AIS patients after IVT. Third, UA and NLR levels were only measured at admission. Without consecutive measurements, we have no data to examine the correlation between UA and NLR variations and stroke prognosis. Last, A clinical study showed that cerebral infarcts in the territory of the anterior cerebral artery have a better prognosis than infarcts in the territory of the middle cerebral artery [35]. It is reasonable to investigate the effect of the combination of uric acid and neutrophil-to-lymphocyte ratio on the different vascular cerebral topographies. Since cerebral infarcts in the ACA territory were infrequent, there was not a sufficient sample size in our study to conduct tratified analysis of different infarcted areas. Future studies are necessary to explore the effect of the combination of uric acid and neutrophil-to-lymphocyte ratio on the different vascular cerebral topographies.
Conclusion
There might be no significant association between UA and the prognosis of AIS patients with IVT. The combination of high UA and high NLR may be a predictor of 3-month death and major disability in AIS patients with IVT. This study suggests that strict control of UA and inflammatory parameters may help to improve outcomes for patients with ischemic stroke.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- UA:
-
Serum uric acid
- NLR:
-
Neutrophil-to-lymphocyte ratio
- AIS:
-
Acute ischemic stroke
- rt-PA:
-
Recombinant tissue plasminogen activator
- IVT:
-
Intravenous thrombolysis
- NIHSS:
-
National Institutes of Health Stroke Scale
- Mrs:
-
Modified Rankin Scale
- TOAST:
-
Trial of Org 10172 in the Acute Stroke Treatment
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- NRI:
-
Net reclassification index
- IDI:
-
Integrated discrimination improvement
References
Cheng Y, Luo J, Lin Y, Zeng Y, Yu J, Lin Y. Impact of hyperglycaemia on complications in patients who had a stroke after thrombolysis. Postgrad Med J. 2021;97 1154:792–7. https://doi.org/10.1136/postgradmedj-2020-138736.
Shi J, Peng H, You S, Liu Y, Xu J, Xu Y, et al. Increase in neutrophils after recombinant tissue plasminogen activator thrombolysis predicts poor functional outcome of ischaemic stroke: a longitudinal study. Eur J Neurol. 2018;25(4):687–e45. https://doi.org/10.1111/ene.13575.
Liu Y, Li G, Jia J, Liu X, Guo J, Zhao X. Clinical significance of neutrophil to lymphocyte ratio in ischemic stroke and transient ischemic attack in young adults. BMC Neurol. 2022;22(1:481). https://doi.org/10.1186/s12883-022-03011-7.
Wang C, Zhang Q, Ji M, Mang J, Xu Z. Prognostic value of the neutrophil-to-lymphocyte ratio in acute ischemic stroke patients treated with intravenous thrombolysis: a systematic review and meta-analysis. BMC Neurol. 2021;21(1:191). https://doi.org/10.1186/s12883-021-02222-8.
Campbell BC, Davis SM, Donnan GA. Uric acid for stroke: glimmer of hope or false dawn? Lancet Neurol. 2014;13 5:440–1. https://doi.org/10.1016/S1474-4422(14)70019-5.
Vassalle C, Mazzone A, Sabatino L, Carpeggiani C. Uric Acid for Cardiovascular Risk: Dr. Jekyll or Mr. Hide? Dis. 2016;4(1:12). https://doi.org/10.3390/diseases4010012.
Zhang Y, Churilov L, Meretoja A, Teo S, Davis SM, Yan B. Elevated urea level is associated with poor clinical outcome and increased mortality post intravenous tissue plasminogen activator in stroke patients. J Neurol Sci. 2013;332(1–2):110–5. https://doi.org/10.1016/j.jns.2013.06.030.
Cutler RG, Camandola S, Feldman NH, Yoon JS, Haran JB, Arguelles S, et al. Uric acid enhances longevity and endurance and protects the brain against ischemia. Neurobiol Aging. 2019;75:159–68. https://doi.org/10.1016/j.neurobiolaging.2018.10.031.
Aliena-Valero A, Baixauli-Martín J, Castelló-Ruiz M, Torregrosa G, Hervás D, Salom JB. Effect of uric acid in animal models of ischemic stroke: a systematic review and meta-analysis. J Cereb Blood Flow Metab. 2021;41(4):707–22. https://doi.org/10.1177/0271678x20967459.
Amaro S, Laredo C, Renú A, Llull L, Rudilosso S, Obach V, et al. Uric acid therapy prevents early ischemic stroke progression: a tertiary analysis of the URICO-ICTUS Trial (Efficacy Study of Combined Treatment with Uric Acid and r-tPA in Acute ischemic stroke). Stroke. 2016;47 11:2874–6. https://doi.org/10.1161/strokeaha.116.014672.
Fernández-Gajardo R, Matamala JM, Gutiérrez R, Lozano P, Cortés-Fuentes IA, Sotomayor CG. Relationship between infarct size and serum uric acid levels during the acute phase of stroke. PLoS ONE. 2019;14 7:e0219402. https://doi.org/10.1371/journal.pone.0219402.
Zhu HY, Zhao SZ, Zhang ML, Wang Y, Pan ZM, Cheng HR, et al. Elevated serum uric acid increases the risk of ischemic stroke recurrence and its inflammatory mechanism in older adults. Front Aging Neurosci. 2022;14:822350. https://doi.org/10.3389/fnagi.2022.822350.
Zhang X, Huang ZC, Lu TS, You SJ, Cao YJ, Liu CF. Prognostic significance of uric acid levels in ischemic stroke patients. Neurotox Res. 2016;29 1:10–20. https://doi.org/10.1007/s12640-015-9561-9.
Sun Z, Feng J, He M, Wang M, Zhang Y, Wang N, et al. Higher uric acid is associated with better discharge recovery and short-term outcome in stroke patients treated with thrombolysis. Neurol Sci. 2021;42 8:3225–31. https://doi.org/10.1007/s10072-020-04919-z.
Amaro S, Urra X, Gomez-Choco M, Obach V, Cervera A, Vargas M, et al. Uric acid levels are relevant in patients with stroke treated with thrombolysis. Stroke. 2011;42(1 Suppl):S28–32. https://doi.org/10.1161/STROKEAHA.110.596528.
Zhang M, Wang Y, Wang K, Yin R, Pan X, Ma A. Association between uric acid and the prognosis of acute ischemic stroke: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. 2021;31 11:3016–23. https://doi.org/10.1016/j.numecd.2021.07.031.
Cheng Z, Zhan Z, Fu Y, Zhang WY, **a L, Xu T, et al. U-Shaped Association between serum Uric Acid and Hemorrhagic Transformation after Intravenous Thrombolysis. Curr Neurovasc Res. 2022;19 2:150–9. https://doi.org/10.2174/1567202619666220707093427.
Liu YL, Wu ZQ, Qu JF, Qiu DH, Luo GP, Yin HP, et al. High neutrophil-to-lymphocyte ratio is a predictor of poor short-term outcome in patients with mild acute ischemic stroke receiving intravenous thrombolysis. Brain Behav. 2020;10 12:e01857. https://doi.org/10.1002/brb3.1857.
Chen S, Cheng J, Ye Q, Ye Z, Zhang Y, Liu Y, et al. Day 1 neutrophil-to-lymphocyte ratio (NLR) predicts stroke outcome after intravenous thrombolysis and mechanical thrombectomy. Front Neurol. 2022;13:941251. https://doi.org/10.3389/fneur.2022.941251.
Del Turco S, Bastiani L, Minichilli F, Landi P, Basta G, **itore A, et al. Interaction of Uric Acid and Neutrophil-to-lymphocyte ratio for cardiometabolic risk stratification and prognosis in coronary artery Disease patients. Antioxid (Basel). 2022;11 11:2163. https://doi.org/10.3390/antiox11112163.
Chamorro A, Obach V, Cervera A, Revilla M, Deulofeu R, Aponte JH. Prognostic significance of uric acid serum concentration in patients with acute ischemic stroke. Stroke. 2002;33 4:1048–52. https://doi.org/10.1161/hs0402.105927.
Romanos E, Planas AM, Amaro S, Chamorro A. Uric acid reduces brain damage and improves the benefits of rt-PA in a rat model of thromboembolic stroke. J Cereb Blood Flow Metab. 2007;27 1:14–20. https://doi.org/10.1038/sj.jcbfm.9600312.
Amaro S, Soy D, Obach V, Cervera A, Planas AM, Chamorro A. A pilot study of dual treatment with recombinant tissue plasminogen activator and uric acid in acute ischemic stroke. Stroke. 2007;38 7:2173–5. https://doi.org/10.1161/STROKEAHA.106.480699.
Chamorro A, Amaro S, Castellanos M, Segura T, Arenillas J, Martí-Fábregas J, et al. Safety and efficacy of uric acid in patients with acute stroke (URICO-ICTUS): a randomised, double-blind phase 2b/3 trial. Lancet Neurol. 2014;13 5:453–60. https://doi.org/10.1016/s1474-4422(14)70054-7.
Wang C, Cui T, Wang L, Zhu Q, Wang A, Yuan Y, et al. Prognostic significance of uric acid change in acute ischemic stroke patients with reperfusion therapy. Eur J Neurol. 2021;28 4:1218–24. https://doi.org/10.1111/ene.14643.
Song SY, Zhao XX, Rajah G, Hua C, Kang RJ, Han YP, et al. Clinical significance of baseline neutrophil-to-lymphocyte ratio in patients with ischemic stroke or hemorrhagic stroke: an updated Meta-analysis. Front Neurol. 2019;10:1032. https://doi.org/10.3389/fneur.2019.01032.
Yilmaz G, Sevinc C, Ustundag S, Yavuz YC, Hacıbekiroglu T, Hatipoglu E, et al. The relationship between mean platelet volume and neutrophil/lymphocyte ratio with inflammation and proteinuria in chronic kidney disease. Saudi journal of kidney diseases and transplantation : an official publication of the Saudi Center for Organ Transplantation. Saudi Arabia. 2017;28(1):90–4. https://doi.org/10.4103/1319-2442.198152.
Bolayir A, Cigdem B, Gokce SF, Yilmaz D. The relationship between neutrophil/lymphocyte ratio and uric acid levels in multiple sclerosis patients. Bratisl Lek Listy. 2021;122 5:357–61. https://doi.org/10.4149/bll_2021_060.
Maiuolo J, Oppedisano F, Gratteri S, Muscoli C, Mollace V. Regulation of uric acid metabolism and excretion. Int J Cardiol. 2016;213:8–14. https://doi.org/10.1016/j.ijcard.2015.08.109.
Qiao T, Wu H, Peng W. The relationship between elevated serum uric acid and risk of Stroke in Adult: an updated and dose-response Meta-analysis. Front Neurol. 2021;12:674398. https://doi.org/10.3389/fneur.2021.674398.
Li P, Zhang L, Zhang M, Zhou C, Lin N. Uric acid enhances PKC-dependent eNOS phosphorylation and mediates cellular ER stress: a mechanism for uric acid-induced endothelial dysfunction. Int J Mol Med. 2016;37 4:989–97. https://doi.org/10.3892/ijmm.2016.2491.
Spiga R, Marini MA, Mancuso E, Di Fatta C, Fuoco A, Perticone F, et al. Uric acid is Associated with inflammatory biomarkers and induces inflammation Via activating the NF-κB signaling pathway in HepG2 cells. Arterioscler Thromb Vasc Biol. 2017;37 6:1241–9. https://doi.org/10.1161/atvbaha.117.309128.
Crișan TO, Cleophas MC, Oosting M, Lemmers H, Toenhake-Dijkstra H, Netea MG, et al. Soluble uric acid primes TLR-induced proinflammatory cytokine production by human primary cells via inhibition of IL-1Ra. Ann Rheum Dis. 2016;75 4:755–62. https://doi.org/10.1136/annrheumdis-2014-206564.
Yang X, Gu J, Lv H, Li H, Cheng Y, Liu Y, et al. Uric acid induced inflammatory responses in endothelial cells via up-regulating(pro)renin receptor. Biomed Pharmacother. 2019;109:1163–70. https://doi.org/10.1016/j.biopha.2018.10.129.
Arboix A, García-Eroles L, Sellarés N, Raga A, Oliveres M, Massons J. Infarction in the territory of the anterior cerebral artery: clinical study of 51 patients. BMC Neurol. 2009;9:30. https://doi.org/10.1186/1471-2377-9-30.
Acknowledgements
Not applicable. We have no acknowledgments to disclose.
Funding
This work was supported by the National Natural Science Foundation of China (82171296), the Suzhou Science and Technology Development Plan Project (SKY2023180), the Scientific Research Foundation of the Second Affiliated Hospital of Soochow University (SDFEYGJ2009), the Clinical Research Center of Neurological Disease of The Second Affiliated Hospital of Soochow University (ND2023B06), the Scientific research project of **’an Health Commission (2024yb48), and the Jiangsu Provincial Medical Key Discipline (ZDXK202217).
Author information
Authors and Affiliations
Contributions
JJS, WNK and YJC: study concept and design. CTW, MLZ, TTK and SJY: Acquisition of data. CTW and JJS: statistical analysis and interpreted the data. JJS: study supervision. All authors approved the protocol.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University (JD-LK-2012-001-01) and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all participants or patient care providers.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, C., Zhou, M., Kang, T. et al. The prognostic value of combined uric acid and neutrophil-to-lymphocyte ratio in acute ischemic stroke patients treated with intravenous thrombolysis. BMC Neurol 24, 183 (2024). https://doi.org/10.1186/s12883-024-03628-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03628-w