Abstract
Background
KDIGO and pRIFLE classifications are commonly used in pediatric acute kidney injury (AKI). As a novel AKI definition, pROCK considered the high variability of serum creatinine in children. This study aimed to compare the above three definitions for AKI in infants undergoing cardiac surgery.
Methods
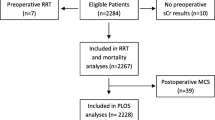
We analyzed a clinical cohort of 413 infants undergoing cardiac surgery. AKI was defined and staged according to pRIFLE, KDIGO, and pROCK, respectively. Incidence differences and diagnostic agreement across definitions were assessed. The association between postoperative outcomes and AKI by each definition was investigated.
Results
Postoperative AKI was identified in 185 (44.8%), 160 (38.7%), and 77 (18.6%) patients according to pRIFLE, KDIGO, and pROCK, respectively. The agreement between pRIFLE and KDIGO was almost perfect (κ = 0.88), while there was only a slight agreement between pROCK and them. AKI by pROCK was independently associated with adverse outcomes (p = 0.003) and prolonged mechanical ventilation (p = 0.002).
Conclusions
There were considerable differences in AKI incidence and staging among definitions. Compared with pRIFLE and KDIGO, AKI defined by pROCK was significantly reduced and better associated with postoperative adverse outcomes.
Similar content being viewed by others
Background
Acute kidney injury (AKI) is a common finding after pediatric cardiac surgery, especially in young infants [1, 2]. It is also associated with increased mortality and morbidity [1, 3]. There have been many AKI definitions, which has made it difficult to compare results across studies. In 2004, the Acute Dialysis Quality Initiative group proposed a definition for AKI: the Risk, Injury, Failure, Loss of Kidney Function, and End-stage Kidney Disease (RIFLE) definition, which was the first evidence-based consensus [4]. Since then, in 2007, RIFLE criteria were modified into pediatric RIFLE (pRIFLE) to adapt the application in children, and pRIFLE was suggested to characterize the pattern of AKI in children [5]. Later, a new classification was introduced by the Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group in 2012 [6]. This classification included three stages of AKI according to relative changes in serum creatinine (SCr) and urine output. The above definitions have been evaluated in many studies of pediatric patients with AKI and showed good predictive ability for adverse outcomes [7,
According to the three AKI definitions, patients were assigned into four groups to show baseline characteristics: non-AKI by the three definitions, AKI by pRIFLE, AKI by KDIGO, and AKI by pROCK (Table 1). The patients with AKI identified by all three criteria were younger and with lower baseline hemoglobin and creatinine (p < 0.05). AKI patients also had lower white blood cells and higher direct bilirubin (p < 0.05).
AKI incidence and agreement between definitions
In the study population of 413 patients, 185 (44.8%) had AKI according to pRIFLE, 160 (38.7%) according to KDIGO, and 77 (18.6%) according to pROCK (Table 2). The incidences of overall AKI were different between the three definitions (p < 0.001). The incidences of stage 1 AKI according to pRIFLE, KDIGO, and pROCK were 33.9%, 26.2%, and 17.9% respectively; and the incidences of stage 2 AKI were 10.9%, 10.2%, and 0.7%, respectively. 10 (2.4%) patients were identified as stage 3 AKI by KDIGO, and no patient was stage 3 AKI according to pRIFLE and pROCK criteria.
AKI overlap across the three definitions was shown in Fig. 2. AKI patients diagnosed by pRIFLE covered all patients with AKI identified by KDIGO and pROCK. A total of 25 (6.1%) patients were diagnosed with AKI only by pRIFLE. According to pROCK, 58.37% (108/185) of the pRIFLE-AKI patients were reclassify as non-AKI, and 51.87% (83/160) of the KDIGO-AKI patients were reclassify as non-AKI.
The three definitions did not lead to a similar diagnosis or staging of AKI. The agreement between pRIFLE and KDIGO was almost perfect, while there was only a slight agreement between pROCK and them. Regarding the diagnosis of AKI, pRIFLE agreed KDIGO with 93.9% (κ = 0.88) of the time, pRIFLE agreed pROCK with 73.8% (κ = 0.44) of the time, and KDIGO agreed pROCK with 79.9% (κ = 0.53) of the time. Additionally, patients with AKI were staged differently among the three definitions. pRIFLE and KDIGO agreed on AKI stage 89.8% (κ = 0.82) of the time, pRIFLE and pROCK agreed on AKI stage 65.1% (κ = 0.29) of the time, and KDIGO and pROCK agreed on AKI stage 69.5% (κ = 0.33) of the time.
Moreover, as shown in Supplementary table 2, in the 274 (66.3%) patients with baseline creatinine ≤ 30 umol/L, a higher percentage of AKI was identified by all three definitions (p < 0.001). And the incidence of AKI was significantly higher according to pRIFLE and KDIGO compared with pROCK (55.5% and 49.6% vs 23.7%, p < 0.001). The difference in AKI incidence between patients with baseline SCr ≤ 30 umol/L and > 30 umol/L was over 30% according to pRIFLE and KDIGO, while it was 15.1% for pROCK.
Comparison of clinical outcomes
Among the 413 patients included, postoperative composite morbidity was 7.5%. As shown in Table 3, the incidence of composite outcome was higher in patients with AKI according to pROCK classification (16.9% vs 5.4%, p = 0.001). However, there was no significant difference between patients with or without AKI according to the other two definitions (pRIFLE, 9.2% vs 6.1%, p = 0.242; KDIGO, 8.1% vs 7.1%, p = 0.704).
MV duration was longer in patients with AKI according to KDIGO and pROCK, but showed no significant difference in pRIFLE (pRIFLE, p = 0.071; KDIGO, p = 0.048, pROCK, p < 0.001). In AKI patients according to pROCK, the incidence of prolonged MV was higher (22.1% vs 7.1%, p < 0.001). There was no difference in prolonged MV among patients with AKI versus non-AKI according to pRIFLE and KDIGO classification (Table 3).
In terms of postoperative PICU stay, the median LOS was longer in AKI patients according to pROCK, but not significant for pRIFLE and KDIGO (pRIFLE, 3.5 days [IQR 2–5 days] vs 3 days [IQR 1–5 days], p = 0.70; KDIGO, 3 days [IQR 2–5 days] vs 3 days [IQR 2–5 days], p = 0.842; pROCK, 3 days [IQR 2–5 days] vs 5 days [IQR 3–8 days], p = 0.001). The incidence of prolonged PICU stay was higher in patients identified as AKI by pROCK, (18.2% vs 8.0%, p = 0.007), but this was not significant in pRIFLE and KDIGO (Table 3).
As shown in Fig. 3, pROCK criteria yielded a better separation (p < 0.001) between non-AKI and AKI patients on the Kaplan–Meier curves than pRIFLE and KDIGO in MV duration and PICU LOS. In multivariable logistic regression for adverse outcomes, after adjusting for age, weight, CPB duration, and RACHS category, AKI by pROCK was an independent risk factor for the composite outcome (OR 3.293, 95%CI 1.487–7.292, p = 0.003) and prolonged MV (OR 3.211, 95%CI 1.530–6.738, p = 0.002). Although AKI by pROCK was associated with prolonged PICU stay in univariable logistic regression, it was not significant in multivariate analysis (p = 0.118). Additionally, AKI by pRIFLE and KDIGO was not associated with in-hospital adverse outcomes (Table 4).
Discussion
In this study, we compared the incidence of postoperative AKI and the association with adverse outcomes, according to pRIFLE, KDIGO, and pROCK definitions. As far as we know, this was the first analysis using pROCK classification to investigate AKI after infant cardiac surgery. We found that there were considerable differences in AKI incidence and staging among definitions. Compared with pRIFLE and KDIGO, fewer patients were identified as AKI according to pROCK, especially for patients with low levels of baseline SCr. Moreover, AKI was independently associated with in-hospital adverse outcomes and prolonged MV, for the patients diagnosed by pROCK but not by RIFLE or KDIGO.
AKI was a common finding after pediatric cardiac surgery [1, 2]. Even mild AKI was associated with increased morbidity and mortality [14, 15]. Several criteria have been described to define AKI in children, among which pRIFLE and KDIGO were the most commonly used in current practice [16]. Estimated creatinine clearance was used to define AKI according to pRIFLE [5], while KDIGO classification was based on the relative changes in SCr [6]. According to different definitions, the incidence of AKI after pediatric cardiac surgery varied greatly, ranging from 15 to 64% [17, 18]. A Meta-analysis reported the pooled incidence rate of AKI after pediatric cardiac surgery was 38.4% (95% CI 32.0%-44.7%) [19]. In our data, the incidence was 38.7% according to KDIGO and 44.8% according to pRIFLE, which was comparable to previous reports [20, 21]. However, the association between postoperative outcomes and AKI defined by pRIFLE and KDIGO was not detected like that in previous studies.
Recently, as a novel SCr-based definition for pediatric AKI, pROCK was developed from a large cohort of hospitalized children [10]. In pROCK definition, the RCV of SCr was estimated based on age and baseline SCr level, and AKI was defined as SCr increase over RCV of SCr. Neither pRIFLE nor KDIGO took into account the high variability of changes in SCr, which did not reflect a real change in renal function [22]. Xu et al. [10] indicated that a greater increase in SCr than normal variability might better represent the true decrease in renal function in children. In their study, 5.3%, 10.2%, and 15.2% of patients were identified as AKI according to pROCK, KDIGO, and pRIFLE, respectively [10]. About 66% of AKI patients defined by pRIFLE and 51% of AKI patients defined by KDIGO were reclassified as non-AKI by pROCK, and mortality risk in these children was comparable with those without AKI. Therefore, the investigators of pROCK concluded it improved the detection of “true” AKI in children compared with earlier definitions that might lead to overdiagnosis of AKI. Our data also showed the incidence of AKI was 18.6% according to pROCK, which was significantly lower than that defined by pRIFLE (44.8%) and KDIGO (38.7%).
Both KDIGO and pRIFLE defined AKI by a fixed percentage increase in SCr (eGFR used in pRIFLE was calculated from SCr), which would lead to limited accuracy of AKI diagnosis in patients with lower levels of baseline SCr. The relative changes seemed less reliable when the baseline SCr was low [23]. However, relatively low SCr was a common characteristic of young children [10]. In our patients, the mean baseline SCr was 27.15 ± 8.10 umol/L, and a total of 274 (66.3%) patients had baseline SCr ≤ 30 umol/L. The incidence of AKI identified by KDIGO and pRIFLE was significantly higher (approximately 50%) in children with baseline SCr ≤ 30 μmol/L. Among these AKI patients defined by pRIFLE or KDIGO, more than one-half of the AKI cases were reclassified as non-AKI by pROCK. Clinically, a relative increase in SCr of > 50% was common in patients with low baseline SCr, while an absolute increase of > 20 μmol/L would be obviously less. Thus, pROCK might avoid overdiagnosis of AKI, particularly in children with lower baseline SCr, and help in detecting “true” AKI in children. Our results also demonstrated that AKI defined by pROCK was more strongly associated with adverse outcomes and MV duration than AKI defined by the other two definitions.
As a novel definition for pediatric AKI, there was limited evidence on the application of pROCK criteria in pediatric cardiac surgery at present. Nevertheless, the high specificity of pROCK criteria was determined in critically ill children [24]. Moreover, in terms of the association with risk of mortality, pROCK was slightly stronger than that of KDIGO [25]. There might be the risk of overdiagnosis in current AKI definitions [26], as our results showed no differences in postoperative adverse outcomes between AKI and non-AKI patients according to pRIFLE and KDIGO. In contrast, our results were not compatible with many reports, in which AKI was regarded as an important indicator of mortality and health care costs in cardiac surgery [27, 28]. In addition, as the creator of pRIFLE, Stuart L. Goldstein [29] indicated that the use of definition with high specificity could lead to less attention to AKI patients who were ruled out by pROCK. And pROCK was deficient in identifying patients at risk for renal dysfunction compared with pRIFLE. Despite this concern, pROCK consistently outperformed the creatinine criteria of KDIGO and pRIFLE in predicting both survival time and survival status [10]. Hopefully, as the further exploration of the correlation of AKI defined by pROCK with short- and long-term renal function and postoperative outcomes, pROCK would be adopted as a standard AKI definition in pediatric cardiac surgery.
The study had some limitations. Firstly, due to the limited sample size, severe AKI (stage 2–3) was rare. Therefore, we did not compare the differences of postoperative outcomes in each AKI stage. Moreover, since the study design of the original study, some relevant data was missed, such as vasopressor need, fluid balance the outcome follow-up. The application of pROCK in pediatric cardiac surgery needs to be further explored, and future research should include larger patient populations, such as neonates, as well as children with higher risk for postoperative AKI.
The association between long-term outcomes and AKI according to the three definitions remained to be explored.
Conclusions
There were considerable differences in AKI incidence and staging among definitions. Compared with pRIFLE and KDIGO, the incidence of AKI was significantly decreased according to pROCK based on the RCV of SCr. Postoperative AKI defined by pROCK was also better associated with adverse outcomes, suggesting that it might be the preferable method for diagnosing AKI in low-weight infants (≤ 10 kg) undergoing cardiac surgery. The application of pROCK might reduce overdiagnosis and thus provide promise to improve the diagnostic ability of AKI after pediatric cardiac surgery.