Abstract
Background
Increasing macrolide resistance makes treatment of Mycoplasma genitalium infections challenging. The second-line treatment is moxifloxacin, an antibiotic drug best avoided due to the potential of severe side effects and interactions. This study evaluates the effects of treatment with doxycycline 100 mg twice daily for 2 weeks as an alternative to moxifloxacin.
Methods
This retrospective observational study examined the medical records of patients testing positive for macrolide resistant Mycoplasma genitalium from January 1st, 2016 to September 1st, 2019 in Trondheim, Norway. Information regarding symptoms as well as clinical and microbiological cure was collected.
Results
263 infections from 259 patients (161 females/98 males) were examined. 155 (58.9%) had a negative test of cure following treatment. 34.7% of symptomatic patients not achieving microbiological cure experienced symptom relief or clearance. There was no statistical difference between bacterial loads in symptomatic versus asymptomatic patients. The mean difference was 1.6 × 105 copies/ml (95% CI − 1.4 × 105–4.8 × 105, p = 0.30) for women and 1.4 × 106 copies/ml (95% CI -4.0 × 105–3.2 × 106, p = 0.12) for men.
Conclusions
The cure rate of doxycycline in this study is higher than previously reported. This adds support to doxycycline’s role in treatment before initiating treatment with less favorable drugs such as moxifloxacin.
Similar content being viewed by others
Background
Mycoplasma genitalium is a sexually transmitted pathogen that can cause acute urethritis in men. It is associated with cervicitis and pelvic inflammatory disease (PID) in women, although less is known about its role in female reproductive tract syndromes[1, 2]. It has been associated with an increased risk of PID, infertility and adverse pregnancy outcomes [2, 3]. However, due to variable diagnostic criteria and the need for invasive diagnostic sampling the evidence to support these associations are weak.
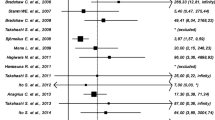
Treatment of M. genitalium has become increasingly difficult. First-line treatment for M. genitalium in Europe was until recently the macrolide antibiotic azithromycin, either as a 1 g single-dose or as a 5-day regimen with 500 mg on day 1 and 250 mg on days 2–5[4]. The latter regimen has been recommended to avoid selection of macrolide resistance [5, 6]. Over the last few years, studies indicating high rates of treatment failure and increasing macrolide resistance has emerged all over the world. A meta-analysis evaluating the efficacy of 1 g azithromycin showed a pooled efficacy of 85.3% in studies performed prior to 2009 and 67.0% in studies performed between 2009 and 2013, indicating that azithromycin has become less effective over time [7]. In Trondheim, Norway, the number of macrolide resistant strains in clinical samples in 2017 was 73% (unpublished data). The implementation of a macrolide resistance test before treatment has been strongly advised in order to avoid unnecessary use of azithromycin where this is futile [8].
The current recommended treatment for macrolide resistant M. genitalium in Europe is moxifloxacin 400 mg daily for 7–10 days [4]. Moxifloxacin is a fluoroquinolone, an antibiotic drug that targets DNA gyrase and topoisomerase IV in bacterial DNA, inhibiting replication [9]. Adverse events described for this drug includes reduction of seizure threshold, QT prolongation, tendinopathy, arthropathy, neuropathies, liver toxicity, psychosis, and photosensitivity [10]. Several cases of fluoroquinolone resistance have been described, especially in Australia and Asia [8, 11, 12]. A review of antimicrobial resistance in Europe based on literature published between 2012 and 2018 report fluoroquinolone resistance-associated mutations in the parC gene with an estimated prevalence of 5% [13]. In Scandinavia, a study from 2017 reported a prevalence of fluoroquinolone resistance-associated mutations of 5.1% in Denmark, 4.1% in Norway and 10.2% in Sweden [14].
A meta-analysis evaluating treatment efficacy of moxifloxacin on M. genitalium infections showed a decrease in elimination rate from 100% on participants enrolled in studies prior to 2010 to 89% in participants enrolled in studies between 2010 and 2016[15]. The 2016 European Mycoplasma Guidelines suggest two third-line treatment options in cases of macrolide and fluoroquinolone treatment failures [4]. The first is pristinamycin, a streptogramin inhibiting protein synthesis, with a prescribed regime of 1 g four times daily for 10 days. The alternative third-line treatment is doxycycline 100 mg twice daily for 14 days. Doxycycline is a second-generation tetracycline, a bacteriostatic antibiotic acting on the ribosomal protein synthesis unit [16]. Benefits include good availability worldwide, affordability and good tolerability by most patients. Randomized controlled trials have found an efficacy of doxycycline of 30–45% for treatment of M.genitalium [17,18,19,20]. Thus far, no mutations associated with tetracycline resistance has been identified for M. genitalium and the reason for the low efficacy of tetracyclines is unknown.
Recently, Read et al. found a ≥ 92% cure rate of M. genitalium infections after conducting sequential antimicrobial therapy [21]. Patients presenting with nongonococcal urethritis, cervicitis or proctitis were initially treated with doxycycline 100 mg twice daily for 7 days followed by M. genitalium macrolide resistance testing, and subsequent resistance-guided therapy with either azithromycin 2.5 g (1 g on day 1 and 500 mg on days 2–4) if resistance negative or sitafloxacin 100 mg twice daily for 7 days if resistance positive. The pre-treatment therapy with doxycycline was assumed to lower bacterial load and thus likely contributed to the high cure rate. The sequential therapy was later evaluated with the more commonly used second-line drug moxifloxacin instead of sitafloxacin, with equal results [22]. The updated guidelines for management of M. genitalium in Britain, Australia and New Zealand now recommend a sequential therapy model for uncomplicated infection [23, 24].
Aims
Following the implementation of macrolide resistance testing at St. Olav’s Hospital in Trondheim, Norway, in 2016, patients with macrolide resistant strains were treated with doxycycline 100 mg twice daily for 14 days to limit the use of moxifloxacin. This study aimed to evaluate the treatment efficiency of doxycycline on macrolide resistant M. genitalium infections. In extension, the study aimed to contribute to reducing unnecessary use of fluoroquinolones.
Materials and methods
Data collection
A list of patients testing positive for macrolide resistant M. genitalium from January 1st, 2016 to September 1st, 2019, was acquired. The samples originated primarily from the Department of Venereology at St. Olav’s Hospital, Trondheim, Norway. Additional samples originated from the Student Sexual Health Clinic at Gløshaugen Campus at the Norwegian University of Science and Technology, the Gynecology Department at St. Olav’s Hospital and the Youth Health Care Centre in Trondheim. The medical records for each of these patients were then accessed and information about treatment regime, control test results and symptom reports were gathered in a pre-defined spreadsheet. Only patients 16 years or above at the time of treatment, who received doxycycline 100 mg twice daily for 14 days, were included. All patients who had made a reservation from biological research were excluded. Other exclusion criteria included lack of test of cure (TOC) or a TOC taken > 3 months after the pre-treatment test. Once the list was complete, patients were de-identified. The final list of included patients consisted of 259 patients. Age, sex and symptom status are shown in Table 1.
Laboratory methods
Before inclusion in the study, all samples had undergone routine microbiological testing for sexually transmitted infections at the Department of Medical Microbiology at St. Olav’s Hospital. Swab samples were collected with flocked swabs in 2.0 ml UTM medium (Copan, Brescia, Italy). 1 mL of urine and 200 µL of transport medium from swab samples were extracted using the NucliSens EasyMag system (bioMerieux SA, Marcy l’Etoile, France), yielding 55 µl of DNA eluate. Polymerase chain reaction was performed using a CFX96 Real-Time PCR instrument (Bio-Rad Laboratories Inc., Hercules, CA, USA). The commercially available screening kit FTD Urethritis basic (Fast-track diagnostics Ltd, Esch-sur-Alzette, Luxembourg) was used for the simultaneous testing of Neisseria gonorrhoeae, Chlamydia trachomatis and M. genitalium. Any M. genitalium positive sample succeedingly underwent macrolide resistance testing using an in-house SimpleProbe PCR Assay [25]. The SimpleProbe assay was introduced as part of routine diagnostics at the laboratory in 2016 and has proven to be a reliable test, with a sensitivity of 95.2% in 2019 (unpublished data). In addition, quantification of all specimens positive for M. genitalium was performed in accordance with instructions from the manufacturer.
Statistics
The sample size was calculated as follows: to obtain a 95% Wilson Score confidence interval with width 0.1 we required a sample size between 320 and 381 for a proportion between 0.3 and 0.5. Expanding the width to 0.2 lowered the required sample size to between 78 and 93 for a proportion between 0.3 and 0.5. The sample size calculation was carried out in the software PASS 2019, v19.0.2. The t-test was used to calculate differences in bacterial load. The analyses were performed using SPSS (IBM SPSS Statistics Version 26, International Business Machines Corporation). The remaining statistical analyses were performed using Microsoft Excel (Microsoft Corporation).
Results
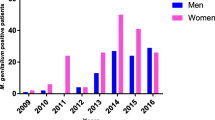
259 patients were included in the study, four of whom had two separate M. genitalium infections during the inclusion time period. Figure 1 shows the distribution of the patient samples. Of the 263 infections evaluated, 155 (58.9%) had a negative TOC after two weeks of treatment with doxycycline 100 mg twice daily. Median time to TOC from the initial positive test based on available dates was 34 days (range 15–92 days). 229 patients from the original list of patients with macrolide resistant samples did not meet the inclusion criteria and were excluded from the study. The mean bacterial load for the 263 included infections was 8.4 x 105 copies/ml (SD 2.7 x 106 copies/ml). The mean difference in bacterial load between asymptomatic and symptomatic patients, as well as the mean difference in bacterial load between patients with a negative TOC and those with a positive TOC, are shown in Table 2.
Table 3 shows the distribution of symptoms stratified by sex. 54.0% of the infections studied were asymptomatic and 4.9% had unknown symptom status. Of the 58.9% with a negative TOC, 57.4% were asymptomatic. Of the 49 patients who reported symptoms at inclusion that had not achieved microbiological cure at TOC, 17 (34.7%) had records of symptom improvement or clearance at the follow-up visit. 16 (32.7%) had no relief of symptoms and 16 (32.7%) had no information on changes in symptom status in their medical records.
Discussion
Increasing macrolide resistance has enforced alternative treatments for M. genitalium infections. Macrolide resistance testing before treatment allows for more appropriate management and contributes to reducing unnecessary use of macrolides where this is futile. Moxifloxacin, as the current recommended second-line treatment option in case of macrolide resistance, belongs to a class of antibiotics shown to be among the worst environmental contaminators [26]. Due to the long list of interactions, precautions and contra-indications of moxifloxacin it would be beneficial to limit its use. In this study, we report a 58.9% cure rate after a two-week course of doxycycline on macrolide resistant infections of M. genitalium. Although low relative to the effects shown for moxifloxacin, this longer course of doxycycline showed a higher efficacy than previously reported.
Symptoms and bacterial load
Several patients in this study experienced a relief of symptoms or symptom clearance despite bacterial persistence. Doxycycline is thought to reduce bacterial load, and several studies have shown that M. genitalium infections with low bacterial loads are more likely to be eliminated [27, 28]. It is therefore possible that the included patients with low bacterial load were more likely to be cured. In our material, the pre-treatment bacterial load for patients with a negative TOC did not differ statistically from those with a positive TOC, although for men the difference was close to significant with a p-value of 0.07. We had no information on the duration of symptoms before the initial testing, a factor that is likely to influence the bacterial load. Without this information further analysis on differences in bacterial load between asymptomatic and symptomatic patients with or without a negative TOC becomes speculative. Available dates for TOC showed a median time of 34 days, with a range from 15 to 92 days. Due to the retrospective study design, there was a lack of standardization which makes exact time of treatment start impossible to assess. TOC was thus recorded as time from the initial pre-treatment test and not the day of treatment start. Even if PCR is a very sensitive test, detecting bacterial loads below 400 copies/ml, the early negative TOCs might represent false negative tests with bacterial loads below the detection limit, and thus overestimate the cure rate. This risk declines if TOC is taken at a later time, and many recommend performing TOC no earlier than 3weeks after treatment. However, the risk of reinfection increases with time. A study comparing one and two weeks of doxycycline with a standardized time to TOC would be beneficial.
Many patients had to be excluded from the study due to a lack of TOC. Whether these patients obtained a TOC or not is unknown. It is plausible that patients not experiencing symptoms at all or patients who experienced a relief of symptoms following treatment were less likely to return for TOC than those with persistent symptoms. Data regarding TOC were inconsistent in the journal notes and advise not to return for a control test when asymptomatic increased from 2019. In addition, advice not to test asymptomatic individuals has increased over the last years, as research has failed to provide clear evidence of severe outcome if M. genitalium is left untreated [2, 29, 30].
Strengths and limitations
Evaluations of new treatments are ideally performed as randomized controlled trials (RCTs) to minimize risk of bias and to control variables. A retrospective observational study like ours has limitations but provides insight into clinical management and adherence of local guidelines with valuable data to support the design of possible prospective studies. 259 patients were included in our study. The sample size was initially estimated to obtain a 95% confidence interval with a width of 0.1. Estimated treatment effect was 30–50%, based on previous studies [17, 19, 31] and preliminary estimates from clinical practice. Although slightly lower than we aimed for, the total amount of included infections is high, providing an acceptable external validity. The main limitation to a retrospective study design is the inability to control which information is available in the medical records and the inability to control for appropriate follow-up. In our study, this resulted in a very high number of patients not meeting inclusion criteria due to lack of TOC within reasonable time. For study purposes a TOC within three months was regarded appropriate. Many had control tests taken later than this and were thus excluded because the risk of re-infection could not be ruled out. Also, spontaneous microbiological clearance is thought to happen, and the likelihood increases with time [32]. Negative control tests taken later than 3 months after treatment can thus be the result of spontaneous clearance rather than the treatment. Many of the TOCs were self-tests and thus the records contained no information of symptoms. As a consequence of the retrospective study design, no instructions were given to health care professionals in advance, and medical notes and patient guidance varied both between and within study sites. It would have been relevant to include all positive M. genitalium samples from the laboratory for the evaluation. However, the ethical approval obtained gave permission to use the macrolide resistant samples only.
Conclusions
Microbiological cure following treatment with doxycycline 100 mg twice daily for two weeks was found in 58.9% of 263 M. genitalium infections in a Norwegian population between January 2016 and September 2019. This is higher than previously reported. Despite several limitations to the study design, our study adds support to doxycycline’s role in treatment of macrolide-resistant M. genitalium before initiating treatment with less favorable drugs like fluoroquinolones.
Availability of data and materials
The data sets used and analyzed during the current study are not publicly available due to privacy of the included patients but are available from the corresponding author on reasonable request.
Abbreviations
- FVU:
-
First-void urine
- M. genitalium:
-
Mycoplasma genitalium
- RCT:
-
Randomized controlled trial
- TOC:
-
Test of cure
References
Gnanadurai R, Fifer H. Mycoplasma genitalium: a review. Microbiology. 2019. https://doi.org/10.1099/mic.0.000830.
Wiesenfeld HC, Manhart LE. Mycoplasma genitalium in women: current knowledge and research priorities for this recently emerged pathogen. J Infect Dis. 2017;216(suppl_2):389–95.
Lis R, Rowhani-Rahbar A, Manhart LE. Mycoplasma genitalium infection and female reproductive tract disease: a meta-analysis. Clin Infect Dis. 2015;61(3):418–26.
2016 European guideline on Mycoplasma genitalium infections. https://iusti.org/wp-content/uploads/2019/12/Jensen_et_al-2016-Journal_of_the_European_Academy_of_Dermatology_and_Venereology.pdf.
Jensen JS, Bradshaw CS, Tabrizi SN, Fairley CK, Hamasuna R. Azithromycin treatment failure in Mycoplasma genitalium-positive patients with nongonococcal urethritis is associated with induced macrolide resistance. Clin Infect. 2008;47(12):1546–53.
Horner P, Ingle SM, Garrett F, Blee K, Kong F, Muir P, Moi H. Which azithromycin regimen should be used for treating Mycoplasma genitalium? A meta-analysis. Sex Transm Infect. 2018;94(1):14–20.
Lau A, Bradshaw CS, Lewis D, Fairley CK, Chen MY, Kong FY, Hocking JS. The efficacy of azithromycin for the treatment of genital Mycoplasma genitalium: a systematic review and meta-analysis. Clin Infect Dis. 2015;61(9):1389–99.
Murray GL, Bradshaw CS, Bissessor M, Danielewski J, Garland SM, Jensen JS, Fairley CK, Tabrizi SN. Increasing macrolide and fluoroquinolone resistance in Mycoplasma genitalium. Emerg Infect Dis. 2017;23(5):809–12.
Hooper DC, Jacoby GA. Topoisomerase inhibitors: fluoroquinolone mechanisms of action and resistance. Cold Spring Harb Perspect Med. 2016. https://doi.org/10.1101/cshperspect.a025320.
Moxifloxacin (systemic): Drug information. https://www.uptodate.com/contents/moxifloxacin-systemic-drug-information?search=moxifloxacin&source=search_result&selectedTitle=1~93&usage_type=default&display_rank=1#F9347994.
Tagg KA, Jeoffreys NJ, Couldwell DL, Donald JA, Gilbert GL. Fluoroquinolone and macrolide resistance-associated mutations in Mycoplasma genitalium. J Clin Microbiol. 2013;51(7):2245–9.
Kikuchi M, Ito S, Yasuda M, Tsuchiya T, Hatazaki K, Takanashi M, Ezaki T, Deguchi T. Remarkable increase in fluoroquinolone-resistant Mycoplasma genitalium in Japan. J Antimicrob Chemother. 2014;69(9):2376–82.
Fernandez-Huerta M, Barbera MJ, Serra-Pladevall J, Esperalba J, Martinez-Gomez X, Centeno C, Pich OQ, Pumarola T, Espasa M. Mycoplasma genitalium and antimicrobial resistance in Europe: a comprehensive review. Int J STD AIDS. 2020;31(3):190–7.
Unemo M, Salado-Rasmussen K, Hansen M, Olsen AO, Falk M, Golparian D, Aasterod M, Ringlander J, Nilsson CS, Sundqvist M, et al. Clinical and analytical evaluation of the new Aptima Mycoplasma genitalium assay, with data on M. genitalium prevalence and antimicrobial resistance in M. genitalium in Denmark, Norway and Sweden in 2016. Clin Microbiol Infect. 2018;24(5):533–9.
Li Y, Le WJ, Li S, Cao YP, Su XH. Meta-analysis of the efficacy of moxifloxacin in treating Mycoplasma genitalium infection. Int J STD AIDS. 2017;28(11):1106–14.
Peyriere H, Makinson A, Marchandin H, Reynes J. Doxycycline in the management of sexually transmitted infections. J Antimicrob Chemother. 2018;73(3):553–63.
Mena LA, Mroczkowski TF, Nsuami M, Martin DH. A randomized comparison of azithromycin and doxycycline for the treatment of Mycoplasma genitalium-positive urethritis in men. Clin Infect. 2009;48(12):1649–54.
Manhart LE, Gillespie CW, Lowens MS, Khosropour CM, Colombara DV, Golden MR, Hakhu NR, Thomas KK, Hughes JP, Jensen NL, et al. Standard treatment regimens for nongonococcal urethritis have similar but declining cure rates: a randomized controlled trial. Clin Infect. 2013;56(7):934–42.
Schwebke JR, Rompalo A, Taylor S, Sena AC, Martin DH, Lopez LM, Lensing S, Lee JY. Re-evaluating the treatment of nongonococcal urethritis: emphasizing emerging pathogens—a randomized clinical trial. Clin Infect Dis. 2011;52(2):163–70.
Anagrius C, Lore B, Jensen JS. Treatment of Mycoplasma genitalium. Observations from a Swedish STD clinic. PLoS ONE. 2013;8(4): e61481.
Read TRH, Fairley CK, Murray GL, Jensen JS, Danielewski J, Worthington K, Doyle M, Mokany E, Tan L, Chow EPF, et al. Outcomes of resistance-guided sequential treatment of Mycoplasma genitalium infections: a prospective evaluation. Clin Infect Dis. 2019;68(4):554–60.
Durukan D, Read TRH, Murray G, Doyle M, Chow EPF, Vodstrcil LA, Fairley CK, Aguirre I, Mokany E, Tan LY, et al. Resistance-guided antimicrobial therapy using doxycycline-moxifloxacin and doxycycline-2.5g azithromycin for the treatment of Mycoplasma genitalium infection: efficacy and tolerability. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciz1031.
Soni S, Horner P, Rayment M, Pinto-Sander N, Naous N, Parkhouse A, Bancroft D, Patterson C, Fifer H. British Association for Sexual Health and HIV national guideline for the management of infection with Mycoplasma genitalium (2018). Int J STD AIDS. 2019. https://doi.org/10.1177/0956462419825948.
Australian STI management guidelines for use in primary care: Mycoplasma genitalium. http://www.sti.guidelines.org.au/sexually-transmissible-infections/mycoplasma-genitalium#management.
Gosse M, Lysvand H, Pukstad B, Nordbo SA. A novel simpleprobe PCR assay for detection of mutations in the 23S rRNA gene associated with macrolide resistance in Mycoplasma genitalium in clinical samples. J Clin Microbiol. 2016;54(10):2563–7.
Van Doorslaer X, Dewulf J, Van Langenhove H, Demeestere K. Fluoroquinolone antibiotics: an emerging class of environmental micropollutants. Sci Total Environ. 2014;500–501:250–69.
Read TRH, Jensen JS, Fairley CK, Grant M, Danielewski JA, Su J, Murray GL, Chow EPF, Worthington K, Garland SM, et al. Use of Pristinamycin for macrolide-resistant Mycoplasma genitalium infection. Emerg Infect Dis. 2018;24(2):328–35.
Guschin A, Ryzhikh P, Rumyantseva T, Gomberg M, Unemo M. Treatment efficacy, treatment failures and selection of macrolide resistance in patients with high load of Mycoplasma genitalium during treatment of male urethritis with josamycin. BMC Infect Dis. 2015;15:40.
Huang C, Zhu HL, Xu KR, Wang SY, Fan LQ, Zhu WB. Mycoplasma and ureaplasma infection and male infertility: a systematic review and meta-analysis. Andrology. 2015;3(5):809–16.
Alfarraj DA, Somily AM. Isolation of Mycoplasma genitalium from endocervical swabs of infertile women. Saudi Med J. 2017;38(5):549–52.
Bjornelius E, Anagrius C, Bojs G, Carlberg H, Johannisson G, Johansson E, Moi H, Jensen JS, Lidbrink P. Antibiotic treatment of symptomatic Mycoplasma genitalium infection in Scandinavia: a controlled clinical trial. Sex Transm Infect. 2008;84(1):72–6.
Vandepitte J, Weiss HA, Kyakuwa N, Nakubulwa S, Muller E, Buve A, Van der Stuyft P, Hayes R, Grosskurth H. Natural history of Mycoplasma genitalium infection in a cohort of female sex workers in Kampala, Uganda. Sex Transm Dis. 2013;40(5):422–7.
Acknowledgements
We would like to thank Professor of Medical Statistics Stian Lydersen for statistical advice and for help estimating sample size.
Funding
The PhD program in Medicine and Health Sciences at the Norwegian University of Technology and Science funded the study. The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Author information
Authors and Affiliations
Contributions
MG was involved in the planning of the study. She collected and analyzed all the data and drafted the manuscript. She created all tables and figures. BP was involved with the planning of the study. She drafted the ethics application and applied for approval. She revised the manuscript draft. SAN was involved with planning of the study. He revised the manuscript draft and provided the microbiological test results. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Regional Ethics Committee (REK midt 2018/928) June 2018. An extended approval to include patients under the age of eighteen at the Youth Health Care Center was sought. Approval was granted in November 2019 and allowed the inclusion of patients sixteen years or above.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gossé, M., Nordbø, S.A. & Pukstad, B. Evaluation of treatment with two weeks of doxycycline on macrolide-resistant strains of Mycoplasma genitalium: a retrospective observational study. BMC Infect Dis 21, 1225 (2021). https://doi.org/10.1186/s12879-021-06910-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06910-1