Abstract
Background
Community health workers (CHWs) have demonstrated capability to improve various health indicators, however, many programmes require support in meeting their objectives due to subpar performance and a high rate of CHW attrition. This systematic review investigated the types of CHWs, their workloads, and supervision practices that contribute to their performance in different countries.
Methods
The search was carried out in November 2022 in Medline, Embase, and Neliti for studies published in Indonesian or English between 1986 and 2022 that reported public health services delivered by CHWs who live and serve the community where they live but are not considered health professionals. The findings were synthesised using a thematic analysis to assess key factors influencing the performance of CHWs.
Results
Sixty eligible articles were included in this review. CHWs were responsible for more than two diseases (n = 35) and up to fifteen, with more than eighteen activities. Their roles covered the human life cycle, from preparation for pregnancy, care for newborns, health for children, adolescents, and productive age to elderly individuals. They were also involved in improving environmental health, community empowerment, and other social issues hindering access to health services. They carried out promotive, preventive, and curative interventions. The CHW-population ratio varied from eight to tens of thousands of people. Some CHWs did not have a clear supervision system. Challenges that were often faced by CHWs included inappropriate incentives, inadequate facilities, insufficient mentoring, and supervision, many roles, and a broad catchment area. Many studies revealed that CHWs felt overburdened and stressed. They needed help to balance their significant work and domestic tasks.
Conclusions
Effective planning that considered the scope of work of CHWs in proportion to their responsibilities and the provision of necessary facilities were crucial factors in improving the performance of CHWs. Supportive supervision and peer-supervision methods are promising, however, any CHW supervision required a detailed protocol. This systematic review emphasised the opportunity for CHW management system improvement in Indonesia.
Similar content being viewed by others
Background
The roots of Community Health Worker (CHW) programmes trace back to the 1930s in China, where the first CHWs, known as "Farmer Scholars," were trained. They laid the groundwork for the Barefoot Doctors, a movement that saw over a million trained individuals from the 1950s to the 1970s. During the 1960s and 1970s, smaller CHW initiatives began to emerge in various countries, especially in Latin America. These early CHW programmes served as prototypes and inspiration for larger-scale initiatives in many low-income countries during the 1980s. Despite initial enthusiasm, many CHW programmes faced challenges and failures in the 1980s and 1990s [1].
After decades, CHWs have gained significant recognition as a critical resource in achieving national and global health goals [2]. CHWs’ role in addressing the shortage of healthcare workers has become increasingly vital due to their effectiveness and practical deployment [3], making them not only an essential bridge for communities to access health services in many countries [4], but also an actor to enhance equitable access to primary healthcare (PHC) across diverse populations [5]. CHWs have demonstrated their ability to reach marginalised groups [6], resulting in positive impacts that include improvements in clinical disease indicators, screening rates, health behavioural change [7], and maternal and child health [8]. In many low- and middle-income nations, including Indonesia, CHWs deliver health services to the community and serve as the first point of contact for health-related issues as part of primary healthcare approaches [6].
In Indonesia, CHWs originated from the national women's Family Welfare Movement (PKK) in the 1970s, with trained volunteers called kader conducting health and nutrition activities. This evolved into the Pos Pelayanan Terpadu (Posyandu) in the mid-1980s, formally recognised by the Ministry of Health [9]. In response to the escalating health issues, the government established Posyandu and additional CHWs to address a broader range of concerns, including non-communicable diseases, elderly health, and adolescent health. This is deemed necessary as the existing Posyandu primarily focuses on maternal and child health services. However, the segmented nature of health services proven ineffective due to the cross-cutting nature of many health targets.
In 2022, the Ministry of Health initiated a comprehensive approach to integrate and revitalise primary health services, including the Posyandu strengthening. The transformed Posyandu aims to provide services across the entire life cycle, catering to pregnant women, the elderly, and others in an integrated manner. This approach is reinforced by regular and planned home visits conducted by CHW to ensure a holistic and cohesive healthcare strategy [10]. Yet, it is imperative for the government to glean insights from past experiences and proactively anticipate potential challenges that might impede the success of the programme. This is particularly crucial since initiatives involving CHWs often encounter obstacles, and the reliability of CHWs can be undermined by various factors.
Despite their valuable contributions, CHWs often face burnout due to overwhelming workloads [11]. This can lead to demotivation and decreased performance, ultimately impeding the achievement of programme objectives [12]. Numerous studies have highlighted that CHWs frequently receive additional assignments beyond their primary responsibilities [13]. Their small numbers are often tasked with serving disproportionately large populations, making it challenging to provide adequate care to all in need [14]. One crucial question that arises is determining the ideal ratio of CHWs to population or identifying the maximum population size that can be effectively handled by a single CHW. The circumstances under which specialist or generalist CHWs are more suitable to be deployed are also essential to explore. This is closely related to the multifaceted responsibility imposed on CHWs. To address these challenges, understanding the supervisory mechanisms implemented in various countries is key. Effective supervision plays a significant role in optimising the performance of CHWs and can help regulate their workload to become more manageable [15, 16]. By providing appropriate support and guidance, supervisors can empower CHWs to work more efficiently and sustainably [16, 17].
We used a systematic review method to gain evidence of the type, workload, and supervision mechanism of CHWs from various studies conducted in various countries. The analysis of this study was tailored to the local context of Indonesia to inform policymakers in improving the existing CHW programme.
Methods
Search strategy and procedure
The systematic review search was performed on three databases on different dates: Medline and Embase (November 18th, 2022) and Neliti (November 21st, 2022). We included Neliti to obtain more articles from the Indonesian context. All studies identified are written in Indonesian or English, published in a peer-reviewed journal, and a primary research. Articles reported as a secondary study (opinion pieces, editorials, conference abstracts, letters, and advocacy materials were excluded. The articles included in this study were only those with Open Access. Multiple keywords and alternative terms were compiled as prompts to find relevant articles for this systematic review (see Table S1 for detailed search strategy). Five sets of search terms were used:
-
1.
“community health worker community health worker or village health worker or community health aide or cadre or family planning personnel or kader kesehatan or kader posyandu”, AND
-
2.
“supervision terms, or charge or monitoring or evaluation or coordination or superintendent or control or assessing or administrative or management or overseeing or direction or directive or governance or regulation or operation”, OR
-
3.
“workload or prevent or screening or surveillance or detecting or counselling or educate or promote or task or employment or function or role or capacity or skill or communicate”, OR
-
4.
“expertise or generalization or ability or specialization or arrangement or types of CHW or types of cadre”, AND
-
5.
“performance or effectiveness or quality or improvement”.
Eligibility criteria
The inclusion and exclusion criteria to obtain eligible articles were structured according to the standard population, intervention, comparison, and outcome (PICO) approach (see Table 1).
Study screening
All database search results were uploaded to Covidence, a systematic review platform [18]. Then, articles that met the inclusion and exclusion criteria of the study based on keyword searches were exported. The screening process was carried out in three stages. First, articles were filtered to remove any duplicates. Then, two independent reviewers screened the titles and abstracts of the included studies against the PICOS criteria. After that, the full texts of the remaining articles were reviewed by two independent reviewers. In case disagreement arose between the reviewers, a third reviewer would assist in resolution.
Data extraction
Following the screening, eight reviewers extracted ten categories of information from the article: title, author, year of publication, population, study location (country), health programme or intervention, CHW duties, supervision mechanisms, types of CHW, and intervention results (programme output or outcome). One independent reviewer checked the accuracy of at least 30% random sample from the extraction. The effect measures extracted were any type of outcomes that assess the efficiency or efficacy of the health programme, for example, health-related outcomes (e.g., mortality rate), service delivery outcomes (e.g., number of people being treated), and CHW-related outcomes (e.g., CHW depression or satisfaction).
Quality appraisal
The quality of the selected studies was assessed by one reviewer and re-examined by another reviewer for at least 10% of the total studies using the Mixed Method Appraisal Tool (MMAT) version 2018 [19], a critical assessment tool designed for the assessment phase of systematic mixed study reviews. The MMAT consists of two screening questions and five criteria (questions), where each study for each criterion will be graded 1 (one) if it satisfies the requested criterion, 0 (zero) if it fails to satisfy the criteriona, and "not available" if it is not reported in the article. If the screening questions are marked 1 or "not available", it indicates that there is potential weakness in the study design and does not necessarily conclude that the research is not empirical. All eligible studies were included in the analysis.
Data synthesis
Once all studies had been extracted using a standardised form, studies with similar outcomes were grouped into specific categories, such as CHW workload per population, and presented in a tabular format. Frequency calculations for studies within the same category were performed to identify trends on the workload and supervision of CHWs. The findings were synthesised using a thematic analysis. Despite the inclusion of various quantitative studies, a meta-analysis was not conducted due to the notable heterogeneity in methods and interventions across included articles.
Results
General descriptions
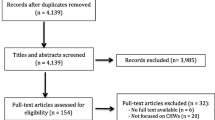
After duplicate articles were removed, we included 7,565 articles, of which; 286 articles were obtained in the title and abstract screening, manual search, and further assessment of full-texts yielded a total of 60 articles. A summary of the screening process is presented in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram (Fig. 1). Of the included articles, 53 discussed CHW workload and 50 examined CHW supervision mechanisms (see Table S3). Most studies were undertaken in East Africa (n = 25), South Asia (n = 12), and West Africa (n = 8), and the rest were in various regions, including South and Central Africa, Southeast Asia, the US, and Australia. In other words, most of the studies focused on low-middle-income countries (n = 51), with the remainder on upper-middle-income countries.
Quality assessment
The articles quality assessment (see Table S2) shows that the majority of articles (n = 27) employed qualitative research methods, while others used non-randomised quantitative (n = 14), mixed methods (n = 14), and a randomised controlled trial (RCT) design (n = 5). The quality appraisals used the full sets of MMAT criteria (see Additional file); where a higher score indicates a better study quality. The results showed that, from 60 articles, 47 articles met 4–5 MMAT criteria, 7 articles met 3 criteria, and 6 articles met 1–2 criteria (see Table S2).
Types of CHWs
Our findings showed that CHWs can be categorised based on the number of disease prevention programmes assigned to them or the population groups (see Table S3), namely, specialist and generalist CHWs, which is in line with WHO (2007) and Koon (2013) [20, 21]. A specialist CHW would provide a narrower range of services, responsible for no more than three disease prevention programmes that target the same population group. Meanwhile, generalist CHWs would be responsible for more than three programmes with multiple tasks and serve all age groups. We found only 53 articles reported CHWs’ workload, including 19 (34.5%) that highlighted specialist CHWs focusing on one to two diseases within the same population group and 36 (65.5%) discussing generalists CHWs responsible for managing various diseases across all age groups. Specialist CHWs typically addressed diseases necessitating specialised care and prompt treatment, including HIV, tuberculosis, malaria, diabetes mellitus, and paediatric conditions such as diarrhoea and pneumonia. They offered comprehensive health services, including curative treatments, with a narrower focus and specific outcome targets such as patient recovery and controlled blood pressure or blood sugar levels.
The workload of CHWs
-
a)
Roles of CHWs
Most of the articles indicated that CHWs felt burdened by unrealistic workloads (n = 15) due to disproportionate population and task assignment, compounded by inappropriate incentives or benefits made available to them. Tasks assigned to CHWs, especially generalists, varied from country to country. In Brazil, one CHW could bear the responsibilities for 15 diseases and more than 18 programme activities, including pregnancy preparation and care for the newborns, health for children, adolescents, productive age, and elderly, all of which received community satisfaction with CHW performance [17]. In other countries, CHWs were also involved in efforts to improve environmental health [11, 17, 22,23,24,25], community empowerment, and other social issues [26,27,28,29,30] that hinder access to health services. These studies have made it evident that CHWs carry out promotive, preventive, and curative actions. Table 2 presents the roles of CHWs based on these three classifications.
We found that most CHWs (n = 24) conducted their roles, such as health screening, monitoring child growth, health promotion, and health promotion, through monthly home visits. Kawasaki (2015) found that CHWs were expected by the community to assist in monitoring their health status through routine home visits, rather than provide strong medicine.
-
b)
Catchment Area
The catchment area refers to the number of target populations assigned to each CHW. Table 3 shows that the catchment areas of CHWs were quite variable and distinguished by the number of patients, households, or population. Most papers identified that one CHW was responsible for 100–250 households (n = 11) [22, 26, 31,32,33] and fewer CHWs (n = 2) were in charge of more than 10,000 people (n = 3) [14, 34, 35]. CHWs who felt burnout were more likely overtasked in a catchment area with low CHW to population ratio [36]. However, those with higher ratios still experienced burnout despite having fewer tasks [14, 35]. CHWs handling 100 households showed many positive outcomes because their work was mostly supported by strong supervision, monthly remuneration, and adequate equipment [15, 17, 25, 27, 29, 35,36,37,38,39,40,41].
-
c)
Time commitment and remuneration of CHWs
We found that among 53 studies, 15 discussed CHW work durations and 13 addressed the provision of incentives. From 15 studies, CHW working hours spanned from 2 to 40 h per week, where three studies [32, 33, 53] reported that CHWs working for 2–4 hours received incentives [37], and one reported no incentives for CHWs. Aridi (2014) highlighted dissatisfaction among incentive recipients as they received incentives to compensate for additional tasks [32]. This emphasises the need for incentives based on working hours and targets. Gadsden’s research (2022) in Malang Regency, Indonesia, supported the idea that CHWs desired compensation proportional to their specific working hours [53]. Other studies indicated varying CHW working hours, ranging from 5–10 hours [48] to 10–20 hours per week [44, 54, 55], over 20 hours per week [46, 51] and even 40 or over weekly hours [14, 26, 43, 56]. In the latter case, some CHWs faced difficulties despite receiving incentives, with one study revealing that 14% of CHWs contemplated quitting.
Only one study by LeFevre analysed [48] the load and time commitment of CHWs, reporting that on average (median, 228 CHWs), each CHW only reached 25% of target households per year (around 120 home visits) despite earning monthly remuneration (USD 15.00). This means that one CHW reached only 10 households per month, while Ngugi (2018) mentioned 20 households per month [22].
Supervision mechanism
There are four commonly discussed aspects or factors in the included studies that may impact the assessment of CHWs performance or productivity: supervisor position, supervision frequency, supervision method, and the number of supervisees.
-
a)
Supervisor Position
On the position of CHWs supervisor, many articles (n = 27) [11, 16, 17, 24, 26,27,28, 32,33,34, 42, 45,46,47,48, 50, 56,57,58,59,60,61,62,63,64,65] reported that CHWs supervision activities were mandated to health workers, all of whom worked at either the primary care or the lowest level of the health care facility. Seven articles [22, 29, 40, 44, 49, 55, 66] mentioned that supervision was conducted by a position that was working closely with CHWs, but they were not health workers or completing formal education. The nature of supervisors resembled that of a peer supervisor. Another type of supervisor was collaborative supervision by two or more people. Kenya had their CHWs supervised by the Community Health Committee (CHC) through monthly supervision to validate CHW reports before turning them further to the Community Health Extension Workers (CHEWs) [22, 32]. CHWs in Malawi worked in a household model, where CHWs were part of a three-tier structure locally called the Health Surveillance Assistants (HSAs), Senior CHW (SCHW), and Site Supervisor (SS). They worked together under the national CHW structure to assess clients’ identification and to coordinate activities, where each position had a clear job description [40] (see Table 4).
-
b)
Supervision Frequency
Seven articles [16, 17, 22, 31, 40, 69] mentioned supervision frequency, ranging from once a month to weekly sessions with varied results in CHWs’ performance or responses (see Table 5). While more frequent supervision sessions implied a more positive outcome, the method and quality of supervision played a large role in the successful performance of CHWs. Most government-led health programmes had supervision sessions more than once a month.
Positive outputs were noted in a health project in Brazil [17, 19] where CHWs were supervised by health professionals (unspecified types). The article mentioned that the supervision method created a partnership and collaboration process between health workers and CHWs. Some examples of negative output were evident in Kenya [22] which measured the incidence of CHW attrition and reported higher attrition in the group that received more frequent supervision because supervision “aimed at fault-finding rather than being supportive.”
-
c)
Supervision Method
There were multiple methods of CHW supervision reported, both in the mechanisms and the instruments employed. Most health programmes used combined methods to monitor CHW reports and their day-to-day activities or tasks. The former typically involved supervisors checking reports, registering quality assurance, or validating data (see Table 6).
The supportive supervision method was mentioned several times in articles [24, 33, 36, 38, 40, 48, 49, 52, 57, 62, 64, 66, 71,72,73] with promising results. Supportive supervision is an accommodative and facilitative process where supervisors facilitate solutions for problems not only those related to medicine or public health, but also any social and psychological issues.
-
d)
Supervision Group Scale
Many articles did not mention how many CHWs were supervised by one assigned supervisor. While fourteen articles mentioned the number of supervised CHWs, the range was enormous, from three people in a cluster RCT in India [44] to more than 50 people in a pilot project evaluation in Uganda [68].
Health programmes engaging larger groups (more than twenty CHWs per supervisory group) usually utilised peer-supervisory mechanisms, such as in India and Pakistan [31, 49, 66]. Meanwhile, health programmes in South Africa had professional nurses supervising approximately 21 CHWs [56], and Kenya combined health professionals and community health committees supervising approximately 25 CHWs [32].
Discussion
Types of CHWs
Our findings revealed a correlation between the CHW types, generalist and specialist, and the target population size as well as the programme workload. Ensuring the appropriate workload for CHWs may minimise potential burnout and hinder target achievement. Based on our systematic review, generalist CHWs were responsible for addressing various types of diseases and they could work effectively when they received a manageable workload, with an estimated coverage of under 100 households per CHW. Adequate support in the form of appropriate facilities such as fair remuneration, transportation, and necessary equipment was essential. These CHWs are best suited to concentrate on conducting home visits to oversee community health, which is in alignment with the preferences of the community [17].
In the Indonesian context, an integrated primary health service programme must be implemented [74] by engaging generalist CHWs to devise strategies to prevent the inefficiency of health services programmes for all age groups. When planning the tasks and scope of work of CHWs, relevant policymakers and decision-makers should consider lessons learned from other countries synthesised in this review. For example, inspiration can be drawn from Brazil's successful CHW programs that receive support in the form of regulations to ensure CHW welfare and accessible community facilities, thus contributing to CHWs’ achievements in improving public health outcomes. Brazil's experience offers valuable insights into Indonesian contexts that share common characteristics, such as a large population and vast geographical area [17].
Identifying the optimum workload
Balancing the workload of CHWs is pivotal for programme success and community well-being. Workload should be customised according to their capabilities, available time (or working hours), and community accessibility. Addressing these concerns is vital to enhance CHWs’ effectiveness and job satisfaction.
We found that the ratio of CHW to population varied widely, with most areas having more than 100 households per CHW. The ideal ratio of CHWs to the population remains unclear, and, to our knowledge, no research with a robust method has addressed this issue. While some advocate for a 1:1000 ratio [75], others argue that this ratio, when applied to the population as a whole or to households, falls short of achieving desired outcomes [76]. Instead, more targeted ratios as potentially more effective alternatives are proposed, such as 1:600 population or 1:150 households [76]. The choice between these ratios depends on specific circumstances, resource availability, and the goals of the allocation.
We found one article that explained how programme makers determined the targets for CHWs [48]. It involves a calculation of the potential number of cases per year in a CHW work area and then distributed it over time to establish monthly or even daily targets. However, the evaluation results demonstrated that, on average, CHWs were only able to achieve 25% (120 households per CHW) of the set targets [48]. Therefore, determining CHWs' workload solely based on case estimates may not always be appropriate. This is especially true for programmes with voluntary participation schemes or limited incentives. Further research needs to focus on identifying relevant variables, particularly those related to the local context, to calculate the ideal workload for the CHWs.
Peer vs supportive supervisions
Supervision mechanisms are highly contextual and dependent on various factors, including the clarity and division of roles between supervisors and CHWs, positive outcomes of supportive and peer supervisions, specific instruments, and the number of supervised CHWs in a single group. Implementing appropriate and well-thought-out supervision mechanisms based on the existing needs and available resources has proven to be effective in enhancing the quality of service delivery and performance of CHWs. On the other hand, evidence has shown that unclear, complex, and low-capacity supervision mechanisms can be frustating for CHWs [11, 47, 65].
Intuitively, more frequent and face-to-face sessions of supervision would have a more positive impact on CHW performance. However, the frequency of supervision alone is not the main factor in improving CHW performance. This review shows that the success of a supervision relies on the combination of both its frequency and methods. Studies also provide evidence of the success and good practices of peer and supportive supervisions.
Peer supervision can be a feasible and affordable option in areas with substantial catchment areas and a large number of CHWs. However, it is important to note that financial and time constraints can pose a challenge [68, 77, 78]. This is a promising method to adopt in Indonesia, where resources are limited. The recommended approach for peer supervision is to appoint high-performing CHWs as peer supervisors and provide them with additional training and support materials, for example, assessment tools on peer-supervisor selection and guidance for conducting supervision sessions. A set of predefined key performance indicators (KPIs) or checklists is a viable option for instruments as feedback references [29, 68]. The peer supervision mechanism provides a good opportunity for skill development between peers and improves the motivation of workers [79]. A similar approach has proven effective when applied to healthcare workers; nurses and midwives who gave routine peer review to each other had better service outcomes [80], and on-the-job peer training in vaccination for nurses had improved coverage [77].
Supportive supervision is a collaborative partnership where supervisors act as facilitators instead of inspectors. A facilitative or supportive supervision provides constructive feedback and facilitates supervisees in searching for solutions [24]. While several studies collectively recommended this method, it requires supporting factors. Complex methodology, in some articles, is the presumable aspect of supportive supervision that may hinder wide-range replications [57, 67]. The main characteristics of supervisors in the facilitative or supportive mechanism, according to Brown (2020), are being present to CHWs while providing safe space, constructive and constant monitoring, and coaching for CHWs.
Although repeatedly pictured as the most ideal form of supervision in the studies, supervision sessions needed some prerequisites prior to implementation. For example, supportive supervisors must have a certain depth of expertise and skills [81], commission additional external assistance (for the first initial sessions, training, and monitoring) [31], and dedicate abundant time allocation that also applies to CHWs. Therefore, supportive supervision should be considered in areas and conditions where prerequisite requirements are sufficient.
Policy implication
The policy implications derived from our findings present a comprehensive framework for the advancement of CHW-based health programmes in Indonesia. First, the allocation of CHWs is not determined through workload calculations. For instance, in the case of maternal and child health CHWs (kader posyandu), the Ministry of Health determines the required number of CHWs based on five-stage services. Five CHWs are responsible for providing maternal and child services in a designated work area called a hamlet (RW or dusun) [82]. The number of households within an RW varies highly between districts; for example, the average household in one RW in North Jakarta (2019) is 116, while in Blitar City (2020), it is 60 [83]. Nonetheless, our findings suggest that this ratio remains balanced even when extending services to monitoring the health of all age groups (Posyandu PRIMA) through home visits, contingent on the government's resolute commitment to the programme. Essential to its success are comprehensive training for CHWs, clearly defined roles and working hours, fair compensation, adequate supervision, and supportive infrastructure. Our review provides learning that several programmes set ambitious targets without specifically addressing the corresponding commitment, leading to inadequate planning, funding, and essential resources for CHWs and supervisors. Vital resources such as transportation, appropriate remuneration, and clear programme guidelines are often lacking in most of our systematic reviews [11, 13, 14, 22, 24, 32, 34, 43, 45, 47, 48, 54, 58, 59, 61, 62, 64, 65, 71, 84].
Second, in Indonesia, CHWs receive substantial guidance from health workers at the Community Health Center (Puskesmas) in the form of relevant training to carry out their duties. However, the supervision to monitor CHW performance has not been fulfilled due to the overload duties of health workers. Therefore, we recommend that there should be regulations, prepared in the form of formal documents, to guarantee the availability of CHW supervisors and their supervision mechanisms. In the setting of organisation-based intervention, a protocol for operating procedure can be established [38], whereas in a larger sub-national or national context, a higher-functioned document or legal product such as Mayor Regulations or Ministry of Health and Ministry of Internal Affair Regulations [14, 85]. A formalised supervision mechanism is a good practice that contributes to a clear coordination of supervision sessions and positive outputs in our studies. These regulations may specify the personnel responsible for the supervision, the method, and the sought outputs or objectives.
Our findings underscore the importance of a well-defined workload distribution, effective supervision, and ample financial support for CHW operations. Consequently, the recommended policy action is to augment the budget allocated to the CHW programme and transfer budget authority to the Ministry of Health for increased flexibility in programme development. The current practice of CHW selection by village heads [86] or under the Ministry of Home Affairs presents several challenges in programme advancement, such as disparate CHW incentives, less robust supervision, and CHW turnovers with changes in the village leadership.
Strengthening the role of CHWs faces challenges without clear and detailed regulations delineating their rights and obligations. Implementation of minimum service standards by CHWs is crucial for enhancing service quality. Moreover, there is a need for the government to prepare CHWs as professionals rather than volunteers to amplify the impact of health service transformation.
Strengths and limitation
The strengths of this systematic review lie in its comprehensive exploration of CHW workload, focusing on catchment areas and working hours. It also provides valuable insights into diverse supervision models used globally, an under researched area in systematic reviews. Furthermore, it aims to be applicable in the Indonesian context, serving as a practical resource for policymakers.
However, this study is limited by its reliance on a limited number of databases, potentially missing relevant research with diverse outcomes. The scarcity of published articles about CHWs in Indonesia limits a comprehensive understanding from the local perspective, despite efforts that have been made to include articles in Indonesia.
Conclusions
The implementation of generalist CHWs may be suitable for Indonesia, especially alongside the rollout of the integrated primary health services. CHWs will be concentrated on health promotion and prevention of health concerns across all age groups. Despite the limited research on the optimal CHW-to-population or CHW-to-household ratio, successful examples from various nations demonstrate that CHWs overseeing fewer than 100 households showcase strong performance, even while managing diverse responsibilities. Clear guidelines from the central government are essential for CHWs, including qualifications, roles, workload, and reporting mechanisms. The recommended measures include establishing a supervision procedure to monitor and support CHW performance; regulating supervision methods to avoid overlap** roles; managing CHWs' workload; and accounting for population, accessibility challenges, as well as resources.
Availability of data materials
Data is provided within the manuscript or supplementary information files (Table S3 Findings).
Abbreviations
- CHW:
-
Community Health Worker
- MMAT:
-
Mixed Methods Appraisal Tools
- PICO:
-
Population, intervention, comparison, and outcome
- PRISMA:
-
The Preferred Reporting Items for Systematic Reviews and Meta-analyses
- RCT:
-
Randomised controlled trial
- WHO:
-
World Health Organization
- HIV:
-
Human immunodeficiency virus
- iCCM:
-
Integrated community case management
- TB:
-
Tuberculosis
- CHC:
-
Community health committee
- CHEW:
-
Community health extension worker
- HSA:
-
Health surveillance assistant
- SCHW:
-
Senior community health worker
- SS:
-
Site supervisor
- LHS:
-
Lady health supervisor
- LHW:
-
Lady health worker
- KPI:
-
Key performance indicator
References
Perry H. A Brief History of Community Health Worker Programs. 2013.
Perry HB. Health for the People: National Community Health Worker Programs from Afghanistan to Zimbabwe. 2021.
Masis L, Gichaga A, Zerayacob T, Lu C, Perry HB. Community health workers at the dawn of a new era: 4 Programme financing. Health Res Policy Syst. 2021;19:107.
Jeet G, Thakur JS, Prinja S, Singh M. Community health workers for non-communicable diseases prevention and control in develo** countries: Evidence and implications. PLoS ONE. 2017;12:e0180640.
Javanparast S, Windle A, Freeman T, Baum F. Community health worker programs to improve healthcare access and equity: are they only relevant to low- and middle-income countries? Int J Health Policy Manag. 2018;7:943–54.
Ahmed S, Chase LE, Wagnild J, Akhter N, Sturridge S, Clarke A, et al. Community health workers and health equity in low- and middle-income countries: systematic review and recommendations for policy and practice. Int J Equity Health. 2022;21:49.
Sharma N, Harris E, Lloyd J, Mistry SK, Harris M. Community health workers involvement in preventative care in primary healthcare: a systematic sco** review. BMJ Open. 2019;9:e031666.
Blanchard AK, Prost A, Houweling TAJ. Effects of community health worker interventions on socioeconomic inequities in maternal and newborn health in low-income and middle-income countries: a mixed-methods systematic review. BMJ Glob Health. 2019;4:e001308.
Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health. 2014;35:399–421.
Kemenkes Integrasikan dan Revitalisasi Pelayanan Kesehatan Primer. Sehat Negeriku. 2022.https://sehatnegeriku.kemkes.go.id/baca/rilis-media/20220610/2440110/kemenkes-integrasikan-dan-revitalisasi-pelayanan-kesehatan-primer/. Accessed 4 Feb 2024.
Rodriguez DC, Banda H, Namakhoma I. Integrated community case management in Malawi: an analysis of innovation and institutional characteristics for policy adoption. Health Policy Plan. 2015;30(Suppl 2):ii74–83.
Sarma H, Jabeen I, Luies SK, Uddin MDF, Ahmed T, Bossert TJ, et al. Performance of volunteer community health workers in implementing home-fortification interventions in Bangladesh: a qualitative investigation. PLOS ONE. 2020;15:e0230709.
Chin-Quee DS, Ridgeway K, Onadja Y, Guiella G, Bai GM, Brennan C, et al. Evaluation of a pilot program for task sharing short and long-acting contraceptive methods in Burkina Faso. Gates Open Res. 2019;3:1499.
Roy S, Pandya S, Hossain MI, Abuya T, Warren CE, Mitra P, et al. beyond institutionalization: planning for sustained investments in training, supervision, and support of community health worker programs in Bangladesh. Glob Health Sci Pract. 2021;9:765–76.
Glenton C, Javadi D, Perry HB. Community health workers at the dawn of a new era: 5. Roles and tasks. Health Res Policy Syst. 2021;19:128.
Hennein R, Ggita JM, Turimumahoro P, Ochom E, Gupta AJ, Katamba A, et al. Core components of a Community of Practice to improve community health worker performance: a qualitative study. Implement Sci Commun. 2022;3:27.
Kawasaki R, Sadamori T, Ferreira de Almeida T, Akiyoshi M, Nishihara M, Yoshimura T, et al. Reactions of community members regarding community health workers’ activities as a measure of the impact of a training program in Amazonas Brazil. J Rural Med. 2015;10:7–19.
Kellermeyer L, Harnke B, Knight S. Covidence and Rayyan. J Med Libr Assoc JMLA. 2018;106:580–3.
Hong QN, Pluye P, Fabregues S, Bartlett G, Boardman S, Cargo M. Mixed Methods Appraisal Tool (MMAT) Version 2018 User Guide | NCCMT. https://www.nccmt.ca/knowledge-repositories/search/232. Accessed 2 May 2023.
WHO. What do we know about community health workers? A systematic review of existing reviews. 2007.https://www.who.int/publications-detail-redirect/what-do-we-know-about-community-health-workers-a-systematic-review-of-existing-reviews. Accessed 7 Sept 2023.
Koon AD, Goudge J, Norris SA. A review of generalist and specialist community health workers for delivering adolescent health services in sub-Saharan Africa. Hum Resour Health. 2013;11:54.
Ngugi AK, Nyaga LW, Lakhani A, Agoi F, Hanselman M, Lugogo G, et al. Prevalence, incidence and predictors of volunteer community health worker attrition in Kwale County. Kenya BMJ Glob Health. 2018;3:e000750.
Greenspan JA, McMahon SA, Chebet JJ, Mpunga M, Urassa DP, Winch PJ. Sources of community health worker motivation: a qualitative study in Morogoro Region. Tanzania Hum Resour Health. 2013;11:52.
Ludwick T, Turyakira E, Kyomuhangi T, Manalili K, Robinson S, Brenner JL. Supportive supervision and constructive relationships with healthcare workers support CHW performance: use of a qualitative framework to evaluate CHW programming in Uganda. Hum Resour Health. 2018;16:11.
Kok M, Abdella D, Mwangi R, Ntinginya M, Rood E, Gassner J, et al. Getting more than ‘claps’: incentive preferences of voluntary community-based mobilizers in Tanzania. Hum Resour Health. 2019;17:101.
Munshi S, Christofides NJ, Eyles J. Sub-national perspectives on the implementation of a national community health worker programme in Gauteng Province. South Africa BMJ Glob Health. 2019;4:e001564.
Collinsworth AW, Vulimiri M, Schmidt KL, Snead CA. Effectiveness of a community health worker-led diabetes self-management education program and implications for CHW Involvement in care coordination strategies. Diabetes Educ. 2013;39:792–9.
Kowitt SD, Emmerling D, Fisher EB, Tanasugarn C. Community health workers as agents of health promotion: analyzing thailand’s village health volunteer program. J Community Health. 2015;40:780–8.
Wroe EB, Nhlema B, Dunbar EL, Kulinkina AV, Kachimanga C, Aron M, et al. A household-based community health worker programme for non-communicable disease, malnutrition, tuberculosis, HIV and maternal health: a stepped-wedge cluster randomised controlled trial in Neno District. Malawi BMJ Glob Health. 2021;6:e006535.
Shelley KD, Frumence G, Mpembeni R, George AS, Stuart EA, Killewo J, et al. Can volunteer community health workers manage multiple roles? An interrupted time-series analysis of combined HIV and maternal and child health promotion in Iringa. Tanzania Health Policy Plan. 2018;33:1096–106.
Aftab W, Rabbani F, Sangrasi K, Perveen S, Zahidie A, Qazi SA. Improving community health worker performance through supportive supervision: a randomised controlled implementation trial in Pakistan. Acta Paediatr Oslo Nor 1992. 2018;107(Suppl 471):63–71.
Aridi JO, Chapman SA, Wagah MA, Negin J. A comparative study of an NGO-sponsored CHW programme versus a ministry of health sponsored CHW programme in rural Kenya: a process evaluation. Hum Resour Health. 2014;12:64.
Kambarami R.A., Mbuya M.N., Pelletier D., Fundira D., Tavengwa N.V., Stoltzfus R.J. Factors Associated With Community Health Worker Performance Differ by Task in a Multi-Tasked Setting in Rural Zimbabwe. Glob Health Sci Pract 2016; 4: 238–250.
Chipukuma HM, Halwiindi H, Zulu JM, Azizi SC, Jacobs C. Evaluating fidelity of community health worker roles in malaria prevention and control programs in Livingstone District, Zambia-A bottleneck analysis. BMC Health Serv Res. 2020;20:612.
Musoke D, Ssemugabo C, Ndejjo R, Atusingwize E, Mukama T, Gibson L. Strengthening the community health worker programme for health improvement through enhancing training, supervision and motivation in Wakiso district. Uganda BMC Res Notes. 2019;12:812.
John A, Nisbett N, Barnett I, Avula R, Menon P. Factors influencing the performance of community health workers: a qualitative study of Anganwadi Workers from Bihar. India PLoS ONE. 2020;15:e0242460.
Maravilla JC, Betts KS, Abajobir AA, Coutocruz C, Alati R. The role of community health workers in preventing adolescent repeat pregnancies and births. J Adolesc Health. 2016;59:378–90.
Kaphle S, Matheke-Fischer M, Lesh N. Effect of performance feedback on community health workers’ motivation and performance in Madhya Pradesh, India: a randomized controlled trial. JMIR Public Health Surveill. 2016;2:e169.
Van Boetzelaer E, Zhou A, Tesfai C, Kozuki N. Performance of low-literate community health workers treating severe acute malnutrition in South Sudan. Matern Child Nutr. 2019;15:e12716.
Ndambo MK, Munyaneza F, Aron MB, Nhlema B, Connolly E. Qualitative assessment of community health workers’ perspective on their motivation in community-based primary health care in rural Malawi. BMC Health Serv Res. 2022;22:179.
O’Donovan J, Saul NA, Hamala R. Exploring supervision for volunteer community health workers in Mukono District, Uganda: an exploratory mixed-methods study. Glob Public Health. 2022;17:1958–72.
Brenner JL, Kabakyenga J, Kyomuhangi T, Wotton KA, Pim C, Ntaro M, et al. Can volunteer community health workers decrease child morbidity and mortality in southwestern Uganda? An impact evaluation PloS One. 2011;6:e27997.
Jerome G, Ivers LC. Community health workers in health systems strengthening: A qualitative evaluation from rural Haiti. AIDS. 2010;24:S67–72.
Khetan AK, Zullo MZ, Gupta RG, Agarwal SA, Mohan SM, Josephson RJ. Effect of a community health worker based approach to integrated cardiovascular risk factor control in India: A cluster randomized, controlled, parallel-group trial (SEHAT). Eur Heart J. 2018;39:646–7.
Pandya S, Hamal M, Abuya T, Kintu R, Mwanga D, Warren CE, et al. Understanding factors that support community health worker motivation, job satisfaction, and performance in three Ugandan districts: opportunities for strengthening uganda’s community health worker program. Int J Health Policy Manag. 2022. https://doi.org/10.34172/ijhpm.2022.6219.
Bhattacharji S, Abraham S, Muliyil JP. Evaluating community health worker performance in India. Health Policy Plan. 1986;1:232–9.
Smith S, Deveridge A, Berman J, Negin J, Mwambene N, Chingaipe E, et al. Task-shifting and prioritization: a situational analysis examining the role and experiences of community health workers in Malawi. Hum Resour Health. 2014;12:24.
LeFevre AE, Mpembeni R, Chitama D, George AS, Mohan D, Urassa DP, et al. Profile, knowledge, and work patterns of a cadre of maternal, newborn, and child health CHWs focusing on preventive and promotive services in Morogoro Region. Tanzania Hum Resour Health. 2015;13:98.
Rabbani F, Shipton L, Aftab W, Sangrasi K, Perveen S, Zahidie A. Inspiring health worker motivation with supportive supervision: a survey of lady health supervisor motivating factors in rural Pakistan. BMC Health Serv Res. 2016;16:397.
Goudge J, De Kadt J, Babalola O, Muteba M, Tseng Y-H, Malatji H, et al. Household coverage, quality and costs of care provided by community health worker teams and the determining factors: findings from a mixed methods study in South Africa. BMJ Open. 2020;10:e035578.
Kawade A, Gore M, Lele P, Chavan U, Pinnock H, Smith P, et al. Interplaying role of healthcare activist and homemaker: a mixed-methods exploration of the workload of community health workers (Accredited Social Health Activists) in India. Hum Resour Health. 2021;19:7.
Kawakatsu Y, Sugishita T, Aiga H, Oruenjo K, Wakhule S, Honda S. Effectiveness of four interventions in improving community health workers’ performance in western Kenya: a quasi-experimental difference-in-differences study using a longitudinal data. Prim Health Care Res Dev. 2022;23:e20.
Gadsden T, Sujarwoto S, Purwaningtyas N, Maharani A, Tampubolon G, Oceandy D, et al. Understanding community health worker employment preferences in Malang district, Indonesia, using a discrete choice experiment. BMJ Glob Health. 2022;7:e008936.
Chin-Quee D, Mugeni C, Nkunda D, Uwizeye MR, Stockton LL, Wesson J. Balancing workload, motivation and job satisfaction in Rwanda: assessing the effect of adding family planning service provision to community health worker duties. Reprod Health. 2016;13:2.
Whidden C, Kayentao K, Liu JX, Lee S, Keita Y, Diakite D, et al. Improving Community Health Worker performance by using a personalised feedback dashboard for supervision: a randomised controlled trial. J Glob Health. 2018;8:020418.
Assegaai T, Schneider H. The supervisory relationships of community health workers in primary health care: social network analysis of ward-based outreach teams in Ngaka Modiri Molema District. South Africa BMJ Glob Health. 2019;4:e001839.
Kok MC, Vallieres F, Tulloch O, Kumar MB, Kea AZ, Karuga R, et al. Does supportive supervision enhance community health worker motivation? A mixed-methods study in four African countries. Health Policy Plan. 2018;33:988–98.
Assegaai T, Schneider H. National guidance and district-level practices in the supervision of community health workers in South Africa: a qualitative study. Hum Resour Health. 2019;17:25.
Oluwole A, Dean L, Lar L, Salami K, Okoko O, Isiyaku S, et al. Optimising the performance of frontline implementers engaged in the NTD programme in Nigeria: lessons for strengthening community health systems for universal health coverage. Hum Resour Health. 2019;17:79.
Strodel RJ, Perry HB. The National Village Health Guide Scheme in India: lessons four decades later for community health worker programs today and tomorrow. Hum Resour Health. 2019;17:76.
Raven J, Wurie H, Idriss A, Bah AJ, Baba A, Nallo G, et al. How should community health workers in fragile contexts be supported: qualitative evidence from Sierra Leone, Liberia and Democratic Republic of Congo. Hum Resour Health. 2020;18:58.
Ashebir F, Medhanyie AA, Mulugeta A, Persson LÅ, Berhanu D. Exploring women’s development group leaders’ support to maternal, neonatal and child health care: A qualitative study in Tigray region. Ethiopia PLOS ONE. 2021;16:e0257602.
Olaniran A, Madaj B, Bar-Zeev S, Banke-Thomas A, van den Broek N. Factors influencing motivation and job satisfaction of community health workers in Africa and Asia-A multi-country study. Int J Health Plann Manage. 2022;37:112–32.
Roy S., Kennedy S., Hossain S., Warren C.E., Sripad P. Examining Roles, Support, and Experiences of Community Health Workers During the COVID-19 Pandemic in Bangladesh: A Mixed Methods Study. Glob Health Sci Pract 2022; 10. https://doi.org/10.9745/GHSP-D-21-00761.
Kelly JM, Osamba B, Garg RM, Hamel MJ, Lewis JJ, Rowe SY, et al. Community health worker performance in the management of multiple childhood illnesses: Siaya District, Kenya, 1997–2001. Am J Public Health. 2001;91:1617–24.
Revadi G., Joshi A., Pakhare A.P. A mixed method study on supportive supervision of Community Health Workers from Central India. medRxiv 2022. https://doi.org/10.1101/2022.01.18.22269339.
Karuga RN, Mireku M, Muturi N, McCollum R, Vallieres F, Kumar M, et al. Supportive supervision of close-to-community providers of health care: Findings from action research conducted in two counties in Kenya. PLoS ONE. 2019;14:e0216444.
Nakibaala G, Watsemba A, Ssali B, Namugera F, Katushabe P, Carleen M, et al. An evaluation of a peer supervision pilot project among community health workers in rural Uganda. Afr Health Sci. 2022;22:647–56.
Datiko DG, Yassin MA, Tulloch O, Asnake G, Tesema T, Jamal H, et al. Exploring providers’ perspectives of a community based TB approach in Southern Ethiopia: implication for community based approaches. BMC Health Serv Res. 2015;15:501.
Phiri SC, Prust ML, Chibawe CP, Misapa R, van den Broek JW, Wilmink N. An exploration of facilitators and challenges in the scale-up of a national, public sector community health worker cadre in Zambia: a qualitative study. Hum Resour Health. 2017;15:40.
Toney AM, Martin T, Sanchez S, Kelley MS, Palmer-Wackerly AL, Chaidez V. Examining the Macrosystem level of influence on community health worker effectiveness in the State of Nebraska: a qualitative approach. J Community Health. 2022;47:510–8.
Hill Z, Dumbaugh M, Benton L, Kallander K, Strachan D, ten Asbroek A, et al. Supervising community health workers in low-income countries–a review of impact and implementation issues. Glob Health Action. 2014;7:24085.
Dam TA, Forse RJ, Tran PMT, Vo LNQ, Codlin AJ, Nguyen LP, et al. What makes community health worker models for tuberculosis active case finding work? A cross-sectional study of TB REACH projects to identify success factors for increasing case notifications. Hum Resour Health. 2022;20:25.
UU No. 17 Tahun 2023. Database Peratur. JDIH BPK. http://peraturan.bpk.go.id/Details/258028/uu-no-17-tahun-2023. Accessed 12 Oct 2023.
Indicator Metadata Registry Details. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/85. Accessed 27 Sept 2023.
Spotlight. 5: How many CHWs do we need? Spotlight. 2015.https://www.spotlightnsp.co.za/2015/11/30/5-many-chws-need/. Accessed 27 Sept 2023.
Robinson JS, Burkhalter BR, Rasmussen B, Sugiono R. Low-cost on-the-job peer training of nurses improved immunization coverage in Indonesia. Bull World Health Organ. 2001;79:150–8.
Campbell C, Scott K. Retreat from Alma Ata? The WHO’s report on task shifting to community health workers for AIDS care in poor countries. Glob Public Health. 2011;6:125–38.
Strachan DL, Källander K, ten Asbroek AHA, Kirkwood B, Meek SR, Benton L, et al. Interventions to improve motivation and retention of community health workers delivering integrated community case management (iCCM): Stakeholder Perceptions and Priorities. Am J Trop Med Hyg. 2012;87:111–9.
Kim YM, Putjuk F, Basuki E, Kols A. Self-Assessment and peer review: improving indonesian service providers’ communication with clients. Int Fam Plan Perspect. 2000;26:4–12.
Brown O, Kangovi S, Wiggins N, Alvarado and CS. Supervision Strategies and Community Health Worker Effectiveness in Health Care Settings. NAM Perspect 2020. https://doi.org/10.31478/202003c.
Kementerian Kesehatan RI. Pedoman Umum Pengelolaan Posyandu. Kementerian Kesehatan RI: Jakarta, 2011https://ayosehat.kemkes.go.id/pub/files/files72087Pedoman_Umum_Pengelolaan_Posyandu.pdf.
SIMPEDAK | Sistem Informasi Penyajian Data Kependudukan. https://simpedak.blitarkota.go.id/buku_data/jumlah_penduduk_per_rt_rw_kelurahan/1005-tanggung. Accessed 13 Oct 2023.
Gottert A, McClair TL, Hossain S, Dakouo SP, Abuya T, Kirk K, et al. Development and validation of a multi-dimensional scale to assess community health worker motivation. J Glob Health. 2021;11:07008.
Ministry of Health and Family Welfare. Bangladesh National Strategy for Community Health Workers. 2019.http://www.communityclinic.gov.bd/admin/content_uploads/CHW%20strategy.pdf.
Permenkes No. 8 Tahun 2019. Database Peratur. JDIH BPK. http://peraturan.bpk.go.id/Details/111722/permenkes-no-8-tahun-2019. Accessed 8 Feb 2024.
Acknowledgements
We thank the Covidence team, who facilitated us with a free subscription. The authors also thank Yudhi Prayudha Ishak Djuarsa, Yurdhina Meilissa, and Olivia Herlinda for their critical feedback.
Funding
None declared.
Author information
Authors and Affiliations
Contributions
S.N., A.S.A.T., A.E., and N.E.P conceptualised the study. S.N., A.S.A.T., and A.E. developed the methods. S.N. wrote the main manuscript text (abstract, introduction, methodology, and conclusion). S.N. and A.S.A.T. analysed data and wrote the finding. A.L. made Fig. 1 and wrote the methods. S.N. and N.E.P made table S3. S.N., A.S.A.T., and AE. wrote the discussion. A.E. reviewed and edited the main manuscript text. S.N., A.S.A.T., A.E., N.E.P, A.L., A.A.W., R.S., and S.L. screened and extracted the data. S.N and A.S.A.T conducted a data curation.
Corresponding author
Ethics declarations
Ethics approval and consent to participants
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nida, S., Tyas, A.S.A., Putri, N.E. et al. A systematic review of the types, workload, and supervision mechanism of community health workers: lessons learned for Indonesia. BMC Prim. Care 25, 82 (2024). https://doi.org/10.1186/s12875-024-02319-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02319-2