Abstract
Background
A higher Life's Essential 8 (LE8)-based cardiovascular health (CVH) has been reported to be associated with a lower risk of both all-cause mortality and cardio-cerebrovascular diseases (CCVDs) related mortality in adults in the United States. At the same time, multiple studies have shown a significant negative association of CVH with the risk of stroke and CCVDs. Since no research has investigated the applicability of the LE8 in stroke patients, this study aimed to explore the association of LE8 with all-cause mortality and cardio-cerebrovascular mortality in stroke patients.
Methods
Data of patients were extracted from the National Health and Nutrition Examination Surveys (NHANES) database in 2007–2018 in this retrospective cohort study. Weighted univariate and multivariate COX regression analyses were utilized to investigate the associations of LE8 with all-cause mortality and cardio-cerebrovascular mortality. We further explored these relationships in subgroups of age, gender, body mass index (BMI), cancer, congestive heart failure (CHF), and coronary heart disease (CHD). The evaluation indexes were hazard ratios (HRs) and 95% confidence intervals (CIs).
Results
Among the eligible patients, 278 died from all-cause and 89 (8.38%) of them died due to CCVDs. After adjusting for covariates, patients with LE8 score ≥ 58.75 seemed to have both lower risk of all-cause mortality (HR = 0.46, 95%CI: 0.31–0.69) and cardio-cerebrovascular mortality (HR = 0.51, 95%CI: 0.26–0.98), comparing to those with LE8 score < 48.123. Higher LE8 scores were associated with lower risk of all-cause mortality in patients aged < 65 years old, without cancer, and whatever the gender, BMI, CHF or CHD conditions (all P < 0.05). The relationships between high LE8 scores and low cardio-cerebrovascular mortality risk were only found in age < 65 years old and non-cancer subgroups (all P < 0.05).
Conclusion
A higher LE8 score was associated with lower risk of both all-cause mortality and cardio-cerebrovascular mortality in patients with stroke, which may provide some reference for risk management and prognosis improvement in stoke. However, more evidences are needed to verify this beneficial role of high LE8 score in stroke prognosis.
Similar content being viewed by others
Background
Stroke is one of the most well-known and extensively studied cardio-cerebrovascular diseases (CCVDs), which is the second cause of mortality and the third cause of disability worldwide [1, 2]. In 2019, there were 12.2 million new stroke cases and the dead cases up to 6.55 million, contributing to a significant global disease burden [3]. Therefore, prevention and management of stroke has become a major public health challenge in the world today.
In recent years, influencing factors associated with prognoses in patients with stroke have been explored widely. The main contributors to CCVDs include smoking, alcohol intake, hypertension, diabetes mellitus (DM), dyslipidaemia and atrial fibrillation, and the most prevalent risk factors among stroke survivors were hypertension and smoking [4]. Also, physical activity as well as diet quality could significantly modified the negative impact of comorbidity on disability in stroke patients [5]. In 2010, a composite indicator basing on seven healthy behaviors and health factors was constructed by the American Heart Association (AHA), namely the Life's Simple 7 (LS7), to represent cardiovascular health (CVH) conditions [6]. The LS7 aims to facilitate a shift from focusing solely on the treatment of disease to actively promoting and maintaining health throughout the life course of populations and individuals [6]. The AHA updated this definition according to experience and evidences in 2022, adding sleep to construct the Life's Essential 8 (LE8), which includes diet quality, physical activity, tobacco exposure, sleep health, body mass index (BMI), lipids, blood sugar and blood pressure [7]. Population-based evidences have suggested a higher LE8-based CVH is linked to lower risk of both all-cause mortality and CCVD-related mortality in the United States adults [8,9,10]. Besides, multiple prospective cohort studies have shown a significant negative association of LE8 with the risk of stroke and cardiovascular diseases [11, 12]. However, since no research has investigated the applicability of the LE8 in outcomes of stroke patients, it is necessary to clarify whether LE8 could be beneficial for prognoses management in stroke survivors, or bring about extraneous earnings.
Herein, the current study aims to explore the associations of the LE8 with all-cause mortality and cardio-cerebrovascular mortality in patients with stroke, with the hope of providing some references for health management and the reduction of disease burden in stroke.
Methods
Study design and participants
This was a retrospective cohort study, and data of patients with stroke were extracted from the National Health and Nutrition Examination Surveys (NHANES) database in 2007–2018. The NHANES is conducted jointly by the National Center for Health Statistics (NCHS) and the Centers for Disease Control and Prevention (CDC) that aims to assess nutritional and health status of noninstitutionalized population in the United States. It includes a complex, multistage stratified probability sample on the basis of selected counties, blocks, households, and persons within households. Information was collected through interviews in participants’ homes that conducted by the NCHS well trained professionals, and extensive physical examinations conducted at mobile exam centers (MECs). For details please visit: https://www.cdc.gov/nchs/nhanes/index.htm.
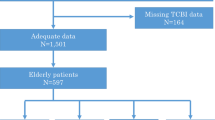
There were 1,398 individuals diagnosed as stroke in the database. The exclusion criteria were (1) aged < 20 years old, (2) missing information on LE8 assessment, (3) missing survival data, and (4) missing information on study variables including education level, sedentary time, cancer, congestive heart failure (CHF), coronary heart disease (CHD), time course of stroke and cotinine. Finally, 865 patients were eligible. The NHANES survey has been approved by the institutional review board (IRB) of the NCHS, and all the participants have provided informed consent. The requirement of ethical approval for this study was waived by the IRB of **ling Hospital, Medical School of Nan**g University, because this database was publicly available. In addition, all study methods were performed in accordance with the relevant guidelines and regulations.
Measurement of LE8
The LE8 score is composed of four health behaviors (including diet quality, physical activity, tobacco exposure and sleep duration) as well as four health factors (BMI, non-high-density-lipoprotein cholesterol [non-HDL-C], blood glucose and blood pressure). Detailed algorithms for calculation of the LE8 scores for each of the metrics to NHANES data have been shown elsewhere [13]. Briefly, each of the eight factors was scored ranging from 0 to 100 points, and the unweighted average of these factors were used to calculate the overall LE8 score. Therefore, a higher LE8 score represents a better health condition. In the current study, we categorized the LE8 score (< 48.13, 48.13–58.75 and ≥ 58.75), health behaviors (< 43.75, 43.75–61.25 and ≥ 61.25), and health factors (< 47.50, 47.50–62.50 and ≥ 62.50) into three levels according to their tertiles respectively [7].
In addition, we calculated the contribution of each component in LE8 to reflect importance rank of these variables. To be specific, random forest models were established to analyses associations of each component in LE8 with all-cause mortality and cardio-cerebrovascular mortality respectively, and using variable importance (VIMP) method to rank the importance of these components. The VIMP calculated the difference value of error rate in models before and after inclusion of the variables. If a variable had a VIMP value < 0 represents it reduced the accuracy prediction of the model. Also, the larger the VIMP value, the greater the impact of this variable on the accuracy of the model, and the greater the importance of this variable.
Variables selection
We also extracted variables from the database as potential covariates, including age, gender, race, education level, marital status, poverty income ratio (PIR), heavy alcohol drinking, sedentary time, hypertension, dyslipidemia, DM, depression, cancer, CHF, CHD, anticoagulants, antiplatelet agents, sleep duration, time course of stroke, height, weight, BMI, waist circumference, systolic blood pressure (SBP), diastolic blood pressure (DBP), total cholesterol (TC), low-density-lipoprotein cholesterol (LDL-C), HDL-C, non-HDL-C, triglyceride (TG), fasting glucose, glycosylated hemoglobin (HbAlc), creatinine (Cr), estimated glomerular filtration rate (eGFR) and the Healthy Eating Index (HEI)-2015.
In the LE8 scoring algorithm, diet quality was evaluated using the HEI-2015. The NHANES collected dietary intakes of participants via two 24-h dietary recalls, and was combined with the United States Department of Agriculture (USDA) food patterns equivalents data to construct and calculate the HEI-2015 scores [14]. Information on heavy alcohol drinking (≥ 8 drinks/week) was collected by self-report questionnaires [15]. DM, dyslipidemia, and hypertension were estimated through laboratory examination, self-report, or medication history: participants with fasting blood glucose ≥ 7.0 mmol/L or HbAlc ≥ 6.5% or self-reported DM or receiving hypoglycemic therapy were considered as DM patients; dyslipidemia referred to TC ≥ 200 mg/dL (5.2 mmol/L) or TG ≥ 150 mg/dL (1.7 mmol/L) or LDL-C ≥ 130 mg/dL (3.4 mmol/L) or HDL-C ≤ 40 mg/dL (1.0 mmol/L) or self-reported hypercholesterolemia or lipid-lowering therapy; hypertension was defined as self-reported high blood pressure or SBP ≥ 130 mmHg or DBP ≥ 80 mmHg or taking hypotensive drugs [16]. In addition, cancer, stroke, depression were also assessed via the NHANES questionnaires [17].
Height, and weights were measured during the physical examination in MECs. The BMI was calculated as the weight in kilograms (kg) divided by the height in meters squared (m2). According to the World Health Organization (WHO) standard, we divided BMI into underweight (< 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 25 kg/m2), overweight (25 kg/m2 ≤ BMI < 30 kg/m2), and obesity (BMI ≥ 30 kg/m2). Besides, the cut-off value for high waist circumference was 88 cm for females and 102 cm for males [18]. Also, the blood samples were collected and sent to central laboratories for the determination of hematological indexes in the NHANES.
Study outcomes and follow-up duration
The study outcomes were all-cause mortality and cardio-cerebrovascular mortality. The NHANES public-use linked mortality file as of December 31, 2019, which was correlated with the NCHS with the National Death Index (NDI) through a probability matching algorithm was used to determine the mortality status of the participants (https://ftp.cdc.gov/pub/health_statistics/NCHS/datalinkage/linked_mortality/). Of which, dying from arbitrary cause was recognized as all-cause mortality, whereas dying due to “disease of heart” (I00-I09, I11, I13, I20-I51) or “cerebrovascular diseases” (I60-I69) was considered as cardio-cerebrovascular mortality. Moreover, the follow-up ended when participants died or at December 31, 2019.
Statistical analysis
Normally distributed continuous data were described using mean ± standard error (mean ± SE), and t test was used for comparation between survival group and all-cause mortality group. Categorical data were expressed as frequency and constituent ratio [N (%)], and chi-square test (χ2) was used for comparison. Due to we included information collected from two 24-h dietary recalls, special weights “dietary two-day sample weight (WTDR2D)” should be used according to the NHANES guideline. The WTDR2D weights were constructed by taking the MEC two-year cycle sample weights (WTMEC2YR), and further adjusting for (a) the additional non-response and (b) the differential allocation by day of the week for the dietary intake data collection.
Weighted univariate COX regression analyses were used to screen the covariates associated with all-cause mortality and cardio-cerebrovascular mortality respectively. Weighted univariate and multivariate COX regression analyses were employed to investigate the association of LE8 with all-cause mortality and cardio-cerebrovascular mortality in patients with stroke. Also, these relationships were assessed in subgroups of age, gender, BMI, cancer, and CHD. Model 1 was unadjusted model. Model 2 adjusted for demographic and socioeconomic factors, including age, gender, race, educational level, marital status and PIR. Model 3 additionally adjusted for selected covariates on the basis of Model 2. The evaluation indexes were hazard ratios (HRs) and 95% confidence intervals (CIs). Two-sided P < 0.05 was considered significant. Statistical analyses were performed by SAS 9.4 (SAS Institute, Cary, NC, USA) and R version 4.2.3 (Institute for Statistics and Mathematics, Vienna, Austria).
Results
Characteristics of participants
The procedure of study participants screening was shown in the Fig. 1. We initially included 1,398 patients with stroke in the NHANES. Then, those who missing information on LE8 assessment (n = 496), education level (n = 1), sedentary time (n = 8), cancer (n = 1), CHF (n = 9), CHD (n = 6), time course of stroke (n = 10) or Cr (n = 2) were excluded. Finally, 865 were eligible.
The median follow-up duration was 64 months, and a total of 278 patients died from all cause. The comparation on characteristics of patients between survival group and all-cause mortality group was shown in the Table 1. Average age of the study population was 63.66 years old, and 451 (57.45%) were female. In survival group, most patients had LE8 score ≥ 58.75 [210 (42.68%)], followed by that < 48.13 [206 (31.13%)], whereas in all-cause mortality group, most patients had LE8 score < 48.13 [95 (33.81%)], and followed by that ≥ 58.75 [91 (33.44%)]. However, between survival group and all-cause mortality group, no significant difference was found in LE8 score, health behaviors score or health factors score (all P > 0.05). In addition, list of the score of each component in LE8 was shown in the Table S1.
Associations of LE8 with all-cause mortality and cardio-cerebrovascular mortality in patients with stroke
Table S2 showed characteristics respectively linked to all-cause mortality and cardio-cerebrovascular mortality. Age, race, cancer, CHF, CHD, anticoagulants, antiplatelet agents, waist circumference, and eGFR were significantly associated with all-cause mortality, whereas that age, race, sedentary time, cancer, CHF, CHD, anticoagulants, antiplatelet agents, and eGFR were associated with cardio-cerebrovascular mortality (all P < 0.05). Then, we constructed multivariate models on the basis of these variables, and screen the covariates through stepwise regression.
We investigated the association of LE8 with all-cause mortality in patients with stroke (Table 2). After adjusting for all covariates, including age, gender, race, education level, marital status, PIR, CHF, CHD and eGFR, patients with LE8 score ≥ 58.75 seemed to have lower risk of all-cause mortality compared to those with LE8 score < 48.13 (HR = 0.46, 95%CI: 0.31–0.69). Besides, health behaviors scores ≥ 61.25 (HR = 0.51, 95%CI: 0.32–0.81) and health factors scores of 47.50–62.50 (HR = 0.63, 95%CI: 0.40–1.00) were also associated with lower risk of all-cause mortality in patients with stroke.
In addition, the Table 3 showed association of LE8 with cardio-cerebrovascular mortality in patients with stroke. Similarly, we found the highest tertile of LE8 score was linked to a lower risk of cardio-cerebrovascular mortality (HR = 0.51, 95%CI: 0.26–0.98) after adjusting for age, gender, race, education level, marital status, PIR, CHF, anticoagulants and eGFR. Also, health factors scores of 47.50–62.50 was associated with lower risk of cardio-cerebrovascular mortality (HR = 0.45, 95%CI: 0.22–0.92) compared to those < 47.50. Unfortunately, no significant association between health behaviors score and cardio-cerebrovascular mortality was observed (P > 0.05).
Associations of LE8 with all-cause mortality and cardio-cerebrovascular mortality in subgroups
These associations were further explored in age, gender, BMI, cancer, CHF, and CHD subgroups. It’s easy to see in the Fig. 2, higher LE8 scores were associated with lower risk of all-cause mortality in patients aged < 65 years old (HR = 0.26, 95%CI: 0.10–0.66), without cancer (HR = 0.42, 95%CI: 0.24–0.73), and whatever the gender (female: HR = 0.44, 95%CI: 0.26–0.74; male: HR = 0.43, 95%CI: 0.24–0.75), BMI (underweight/normal: HR = 0.28, 95%CI: 0.10–0.81; overweight/obesity: HR = 0.52, 95%CI: 0.31–0.88), CHF (non-CHF: HR = 0.45, 95%CI: 0.27–0.74; CHF: HR = 0.32, 95%CI: 0.13–0.78) or CHD (non-CHD: HR = 0.55, 95%CI: 0.34–0.90; CHD: HR = 0.34, 95%CI: 0.13–0.88) conditions. Differently, the negative relationship between LE8 scores and cardio-cerebrovascular mortality were found in age < 65 years old (HR = 0.28, 95%CI: 0.09–0.90) and non-cancer (HR = 0.45, 95%CI: 0.21–0.97) subgroups (Fig. 3).
Discussion
In the current study, we investigated the associations of LE8 with all-cause mortality and cardio-cerebrovascular mortality in patients with stroke respectively. The study results suggested that a higher LE8 score was linked to both lower risk of all-cause mortality and cardio-cerebrovascular mortality. The negative association between LE8 and all-cause mortality was found in patients aged < 65 years old, without cancer, and whatever the gender, BMI, CHF or CHD conditions. In addition, the relationship between a higher LE8 score and low cardio-cerebrovascular mortality risk was only observed in aged < 65 years old and non-cancer subgroups.
The LE8 metric was introduced on the basis of LS7, adding sleep metrics and revisions of the previous 7 domains, and has been reported to be associated with incident CCVDs as well as mortality [9, 19]. Due to the severe disease burden of stroke globally, we thought it is necessary to clarify the association of LE8 with mortality risk in patients with stroke in order to provide some references for relatively comprehensive methods on stroke prevention and management. Studies have investigated the role of LE8 in all-cause and cardio-cerebrovascular mortality in different populations. Hernández-Martínez et al. [20] assessed the association of LE8 with mortality in the Spanish adult population, and found that a higher LE8 score was associated with lower all-cause and CVD related mortality. Isiozor et al. [21] examined the association between LE8 and the risk of cardiovascular and all-cause mortality in Finnish men, and showed that high level of CVH, which was defined by LE8, was linked to significantly lower risks of CHD, stroke, as well as CVD. Different to these previous studies, our study population was adult patients with stroke in the United States, which relatively supplemented the literature blank in this population.
The LE8-related CVH score can significantly predict future stroke risk [11]. Smoking, non-HDL-C, blood pressure, BMI, HbA1c, physical activity, diet quality, and sleep duration were used to create a modified version of the LE8 score. Among the above 8 factors, we found physical activity, BMI, and blood pressure had the highest contribution to the predictive value of LE8 on all-cause mortality in patients with stroke (Figure S1), whereas physical activity, sleep duration, and diet quality had the highest contribution to that on cardio-cerebrovascular mortality (Figure S2). A prospective cohort study has shown that objectively measured physical activity was linked to lower risk of stroke or all-cause mortality in 70-year-old individuals [22]. Also, physical activity was strongly associated with lower risk of CVD-, CHD-, and stroke-related mortality among people with a history of these specific diseases [23]. Therefore, advocating appropriate physical activity in stroke patients is an effective measure to reduce the risk of poor prognosis. In adults, a higher BMI is linked with a higher chance of hypertension, CVD, stroke, heart disease, and mortality [24,25,26]. It seemed that the predictive value of cardiovascular-related factors for all-cause mortality in stroke patients was relatively higher, but the specific mechanisms need further clarification. In addition to physical activity, sleep duration and diet quality also played important roles in the association between IE8 and cardio-cerebrovascular mortality in stroke patients. In fact, sleep was a new metric added into LE8 [7]. A prospective magnetic resonance neuroimaging study in middle-aged individuals without stroke or dementia enrolled in the UK Biobank showed that suboptimal sleep duration is associated with poorer neuroimaging brain health profiles in middle-aged adults without stroke or dementia [27]. Similarly, a high diet quality, especially adherence to the Mediterranean (Med) diet pattern, can effectively reduce cardiovascular mortality [28]. Livingstone et al. [29] considered a better quality of diet predicted lower risk of all-cause and CVD related mortality in Australian adults, while a more inflammatory diet predicted higher mortality risk.
The LE8 provides a simple and effective tool for assessing individual’s CVH and promoting healthy lifestyle behaviors. The LE8 metrics would not only benefit individuals to specifically identify modifiable risk factors but would highlight LE8 factors that can be directly changed for better and improved LE8 scores and better CVH [30]. However, the underlying mechanisms that a higher LE8 linked to a better prognosis of stroke are still unclear. Previous studies have concluded several hypothetical mechanisms. Hypertension may be indirectly related to white matter hyperintensities (WMH) progression via arterial compliance, and the underlying pathophysiological process between hypertension and mortality in stroke may be associated with cognitive impairment associated with stroke [31]. In parallel, hyperlipidaemia results in microvascular haemodynamic regulation disorder, and increases viscosity and resistance of blood flow, for the progression of WMH [32]. Besides, visceral obesity contributed to deep WMH through increases in proinflammatory cytokines [33]. The healthy dietary patterns can improve endothelial function, adiposity and lower levels of inflammatory markers [34]. Meanwhile, poor sleep efficiency was independently associated with basal ganglia according to altering waste clearance mechanisms, and sleep may be associated with relieving inflammation [35]. Healthcare providers could use LE8 to educate stroke patients on the importance of maintaining a healthy lifestyle and managing risk factors such as blood pressure, physical activity levels, and sleep duration. However, as the current study did not find significant associations between health behaviors and cardio-cerebrovascular mortality, indicating that stroke patients are recommend to focus on improving the overall LE8 score rather than emphasizing only one component.
Furthermore, subgroup analyses showed associations of LE8 with all-cause mortality and cardio-cerebrovascular mortality had differences in gender and cancer subgroups. In general population in the United States, no gender difference has been observed according to previous researches on association between LE8 and mortality risk [8, 36]. In 2019, stroke was the 3rd leading cause of mortality in female adults, compared with 5th in males in the United States [37]. Also, elevated BMI, clinical obesity, and higher waist circumference are linked to higher risk of total and ischemic stroke in both sexes, with a stronger association in women than men [38]. Female-specific risk factors such as use of oral contraceptive pills, menopausal hormone therapy, and adverse pregnancy outcomes, may also increase the possibility of adverse prognoses in stroke [39]. Therefore, our findings indicated that targeted health promotion strategies and lifestyle changes should be used in women with stroke to reduce the risk of mortality. Additionally, compared with patients with cancer, higher LE8 scores in those who without cancer were significantly associated with lower risk of both all-cause mortality and cardio-cerebrovascular mortality. It may because these populations may be particularly concerned about intervening with lifestyle-related factors or following medical advice for specific treatments in clinical practice.
This was the first research investigated the associations of LE8 with all-cause mortality and cardio-cerebrovascular mortality in patients with stroke on the basis of the NHANES database, which includes large samples with good representativeness. Our results may provide some references for further comprehensive health management in stroke survivors to reduce the disease burdens. Nevertheless, there are some limitations in this study. Although we have taken possible confounding factors into consideration, due to some of the data were self-reported, and unavailable follow-up duration data, information bias is unavoidable. In addition, the study populations were only from the United States that the applicability of LE8 in stroke populations of other races still needs to be further validated.
Conclusion
A high LE8 score was associated with lower risk of mortality in stroke patients, which may provide some information on prognosis management in stroke. However, the causal association between LE8 and stroke prognosis needs further clarification.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available in the NHANES database, https://ftp.cdc.gov/pub/health_statistics/NCHS/datalinkage/linked_mortality.
Abbreviations
- CCVDs:
-
Cardio-cerebrovascular diseases
- DM:
-
Diabetes mellitus
- AHA:
-
American Heart Association
- LS7:
-
Life’s Simple 7
- CVH:
-
Cardiovascular health
- LE8:
-
Life’s Essential 8
- BMI:
-
Body mass index
- NHANES:
-
National Health and Nutrition Examination Surveys
- NCHS:
-
National Center for Health Statistics
- CDC:
-
Centers for Disease Control and Prevention
- MECs:
-
Mobile exam centers
- CHF:
-
Congestive heart failure
- CHD:
-
Coronary heart disease
- IRB:
-
Institutional review board
- PIR:
-
Poverty income ratio
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density-lipoprotein cholesterol
- TG:
-
Triglyceride
- HbAlc:
-
Glycosylated hemoglobin
- Cr:
-
Creatinine
- eGFR:
-
Estimated glomerular filtration rate
- HEI:
-
Healthy Eating Index
- USDA:
-
United States Department of Agriculture
- WHO:
-
World Health Organization
- NDI:
-
National Death Index
- HRs:
-
Hazard ratios
- CIs:
-
Confidence intervals
References
Wu H, Chiou J. Potential benefits of probiotics and prebiotics for coronary heart disease and stroke. Nutrients. 2021;13:2878.
Xu S, Huang P, Yang J, Du H, Wan H, He Y. Calycosin alleviates cerebral ischemia/reperfusion injury by repressing autophagy via STAT3/FOXO3a signaling pathway. Phytomedicine. 2023;115: 154845.
Collaborators GBDS. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820.
Wang YJ, Li ZX, Gu HQ, Zhai Y, Jiang Y, Zhao XQ, et al. China Stroke Statistics 2019: A report from the National center for healthcare quality management in neurological diseases, China national clinical research center for neurological diseases, the chinese stroke association, national center for chronic and non-communicable disease control and prevention, chinese center for disease control and prevention and institute for global neuroscience and stroke Collaborations. Stroke Vasc Neurol. 2020;5:211–39.
Nguyen LTK, Do BN, Vu DN, Pham KM, Vu MT, Nguyen HC, et al. Physical activity and diet quality modify the association between comorbidity and disability among stroke patients. Nutrients. 2021;13:1641.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613.
Lloyd-Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, et al. Life’s essential 8: updating and enhancing the american heart association’s construct of cardiovascular health: a presidential advisory from the american heart association. Circulation. 2022;146:e18–43.
Yi J, Wang L, Guo X, Ren X. Association of Life’s Essential 8 with all-cause and cardiovascular mortality among US adults: A prospective cohort study from the NHANES 2005–2014. Nutr Metab Cardiovasc Dis. 2023;33:1134–43.
Sun J, Li Y, Zhao M, Yu X, Zhang C, Magnussen CG, et al. Association of the American Heart Association’s new “Life’s Essential 8” with all-cause and cardiovascular disease-specific mortality: prospective cohort study. BMC Med. 2023;21:116.
Sun Y, Yu Y, Zhang K, Yu B, Yu Y, Wang Y, et al. Association between Life’s Essential 8 score and risk of premature mortality in people with and without type 2 diabetes: A prospective cohort study. Diabetes Metab Res Rev. 2023;39: e3636.
Wu S, Wu Z, Yu D, Chen S, Wang A, Wang A, et al. Life’s essential 8 and risk of stroke: a prospective community-based study. Stroke. 2023;54:2369–79.
Zhang J, Chen G, Habudele Z, Wang X, Cai M, Li H, et al. Relation of Life’s Essential 8 to the genetic predisposition for cardiovascular outcomes and all-cause mortality: results from a national prospective cohort. Eur J Prev Cardiol. 2023;30:1676–85.
Wang L, Yi J, Guo X, Ren X. Associations between life’s essential 8 and non-alcoholic fatty liver disease among US adults. J Transl Med. 2022;20:616.
Vilar-Gomez E, Nephew LD, Vuppalanchi R, Gawrieh S, Mladenovic A, Pike F, et al. High-quality diet, physical activity, and college education are associated with low risk of NAFLD among the US population. Hepatology. 2022;75:1491–506.
Gay IC, Tran DT, Paquette DW. Alcohol intake and periodontitis in adults aged >/=30 years: NHANES 2009–2012. J Periodontol. 2018;89:625–34.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation. 2018;138:e426–83.
Patel JS, Oh Y, Rand KL, Wu W, Cyders MA, Kroenke K, et al. Measurement invariance of the patient health questionnaire-9 (PHQ-9) depression screener in U.S. adults across sex, race/ethnicity, and education level: NHANES 2005–2016. Depress Anxiety. 2019;36:813–23.
You Y, Luo J, Elstgeest LEM, Zhang Y, Tan SS, Raat H. Associations between health indicators and sleep duration of American adults: NHANES 2011–16. Eur J Public Health. 2021;31:1204–10.
Howard G, Cushman M, Blair J, Wilson NR, Yuan Y, Safford MM, et al. Comparative discrimination of life's simple 7 and life's essential 8 to stratify cardiovascular risk: is the added complexity worth it? Circulation. 2023;149:905–13.
Hernandez-Martinez A, Duarte-Junior MA, Sotos-Prieto M, Ortola R, Banegas JR, Rodriguez-Artalejo F, et al. Cardiovascular health in Spain based on the life's essential 8 and its association with all-cause and cardiovascular mortality: the ENRICA cohort. Rev Esp Cardiol (Engl Ed). 2023;77:372–80.
Isiozor NM, Kunutsor SK, Voutilainen A, Laukkanen JA. Life’s Essential 8 and the risk of cardiovascular disease death and all-cause mortality in Finnish men. Eur J Prev Cardiol. 2023;30:658–67.
Ballin M, Nordstrom P, Niklasson J, Nordstrom A. Associations of objectively measured physical activity and sedentary time with the risk of stroke, myocardial infarction or all-cause mortality in 70-year-old men and women: a prospective cohort study. Sports Med. 2021;51:339–49.
Cabanas-Sanchez V, Duarte Junior MA, Lavie CJ, Celis-Morales C, Rodriguez-Artalejo F, Martinez-Gomez D. Physical activity and cause-specific cardiovascular mortality among people with and without cardiovascular disease: a cohort study of 0.6 million US adults. Mayo Clin Proc. 2023;99:564–77.
Stamler J. Epidemiologic findings on body mass and blood pressure in adults. Ann Epidemiol. 1991;1:347–62.
Kee CC, Sumarni MG, Lim KH, Selvarajah S, Haniff J, Tee GHH, et al. Association of BMI with risk of CVD mortality and all-cause mortality. Public Health Nutr. 2017;20:1226–34.
Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7.
Clocchiatti-Tuozzo S, Rivier CA, Renedo D, Torres Lopez VM, Geer JH, Miner B, et al. Suboptimal sleep duration is associated with poorer neuroimaging brain health profiles in middle-aged individuals without stroke or dementia. J Am Heart Assoc. 2024;13: e031514.
Rees K, Takeda A, Martin N, Ellis L, Wijesekara D, Vepa A, et al. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2019;3:CD009825.
Livingstone KM, Milte CM, Torres SJ, Hart MJ, Dingle SE, Shaw JE, et al. Nineteen-year associations between three diet quality indices and all-cause and cardiovascular disease mortality: the Australian diabetes, obesity, and lifestyle study. J Nutr. 2022;152:805–15.
Isiozor NM, Laukkanen JA, Voutilainen A, Bensenor IM, Kunutsor SK. Life’s Essential 8 is associated with atherosclerotic cardiovascular disease but not venous thromboembolism in men: a prospective cohort study. Ann Med. 2023;55:2233894.
Tanabe J. White matter hyperintensities are associated with an increased risk of stroke, dementia and mortality. Evid Based Ment Health. 2011;14:1.
Shu Z, Xu Y, Shao Y, Pang P, Gong X. Radiomics from magnetic resonance imaging may be used to predict the progression of white matter hyperintensities and identify associated risk factors. Eur Radiol. 2020;30:3046–58.
Lampe L, Zhang R, Beyer F, Huhn S, Kharabian Masouleh S, Preusser S, et al. Visceral obesity relates to deep white matter hyperintensities via inflammation. Ann Neurol. 2019;85:194–203.
Si XL, Gu LY, Song Z, Zhou C, Fang Y, ** CY, et al. Different perivascular space burdens in idiopathic rapid eye movement sleep behavior disorder and parkinson’s disease. Front Aging Neurosci. 2020;12: 580853.
Zhang DD, Cao Y, Mu JY, Liu YM, Gao F, Han F, et al. Inflammatory biomarkers and cerebral small vessel disease: a community-based cohort study. Stroke Vasc Neurol. 2022;7:302–9.
Ma H, Wang X, Xue Q, Li X, Liang Z, Heianza Y, et al. Cardiovascular health and life expectancy among adults in the United States. Circulation. 2023;147:1137–46.
Heron M. Deaths: leading causes for 2019. Natl Vital Stat Rep. 2021;70:1–114.
Peters SAE, Carcel C, Millett ERC, Woodward M. Sex differences in the association between major risk factors and the risk of stroke in the UK Biobank cohort study. Neurology. 2020;95:e2715–26.
Rexrode KM, Madsen TE, Yu AYX, Carcel C, Lichtman JH, Miller EC. The impact of sex and gender on stroke. Circ Res. 2022;130:512–28.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Bin Yan and Yugang Yin designed the study. Bin Yan wrote the manuscript. Yan ** and Song Mao collected, analyzed, and interpreted the data. Yugang Yin critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The requirement of ethical approval for this was waived by the IRB of **ling Hospital, Medical School of Nan**g University, because the data was accessed from NHANES (a publicly available database). The need for written informed consent was waived by the IRB of **ling Hospital, Medical School of Nan**g University due to retrospective nature of the study. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12872_2024_3947_MOESM2_ESM.tiff
Supplementary Material 2: Figure S1. Contributions of each component in the association between LE8 and all-cause mortality.
12872_2024_3947_MOESM3_ESM.tiff
Supplementary Material 3: Figure S2. Contributions of each component in the association between LE8 and cardio-cerebrovascular mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, B., **, Y., Mao, S. et al. Association of Life’s essential 8 score with the risk of all-cause mortality and cardio-cerebrovascular mortality in patients with stroke. BMC Cardiovasc Disord 24, 320 (2024). https://doi.org/10.1186/s12872-024-03947-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03947-3