Abstract
Background
Conventional, non-specific preventive migraine treatments often demonstrate low rates of treatment persistence due to poor efficacy or tolerability. Effective, well-tolerated preventive treatments are needed to reduce migraine symptoms, improve function, and enhance quality of life. Atogepant is a migraine-specific oral calcitonin gene–related peptide receptor antagonist that is indicated for the preventive treatment of migraine in adults. This analysis evaluated the safety and tolerability profile of atogepant for the preventive treatment of migraine, including adverse events (AEs) of interest, such as constipation, nausea, hepatic safety, weight changes, and cardiac disorders.
Methods
This post hoc analysis was performed using data pooled from 2 (12-week) randomized, double-blind, placebo-controlled trials (RCTs) and 2 (40- and 52-week) open-label long-term safety (LTS) trials of oral atogepant for episodic migraine (EM).
Results
The safety population included 1550 participants from the pooled RCTs (atogepant, n = 1142; placebo, n = 408) and 1424 participants from the pooled LTS trials (atogepant, n = 1228; standard care [SC], n = 196). In total, 643/1142 (56.3%) atogepant participants and 218/408 (53.4%) placebo participants experienced ≥ 1 treatment-emergent AEs (TEAEs) in the RCTs. In the LTS trials, 792/1228 (64.5%) of atogepant participants and 154/196 (78.6%) of SC participants experienced ≥ 1 TEAEs. The most commonly reported TEAEs (≥ 5%) in participants who received atogepant once daily were upper respiratory tract infection (5.3% in RCTs, 7.7% in LTS trials), constipation (6.1% in RCTs, 5.0% in LTS trials), nausea (6.6% in RCTs, 4.6% in LTS trials), and urinary tract infection (3.4% in RCTs, 5.2% in LTS trials). Additionally, weight loss appeared to be dose- and duration-dependent. Most TEAEs were considered unrelated to study drug and few led to discontinuation.
Conclusions
Overall, atogepant is safe and well tolerated in pooled RCTs and LTS trials for the preventive treatment of EM in adults.
Trial registration
ClinicalTrials.gov identifiers: NCT02848326 (MD-01), NCT03777059 (ADVANCE), NCT03700320 (study 302), NCT03939312 (study 309).
Graphical Abstract

Similar content being viewed by others
Introduction
Migraine, a leading cause of disability worldwide, is a highly prevalent neurologic disease defined by recurrent attacks of headache pain and associated symptoms (eg, photophobia, nausea, allodynia) [1]. According to the American Headache Society Consensus Statement, preventive treatment should be considered for individuals with migraine who experience ≥ 3 monthly headache days (MHDs) with severe disability, ≥ 4 MHDs with some disability, or ≥ 6 MHDs regardless of the level of disability [2]. Conventional non-specific preventive migraine treatments often demonstrate low rates of treatment persistence, primarily due to inadequate efficacy or poor tolerability [3]. Effective, well-tolerated, migraine-specific preventive treatments are needed to reduce migraine symptoms, improve function, and enhance quality of life [3, 4].
Atogepant, a migraine-specific oral CGRP receptor antagonist administered once daily, is indicated for the preventive treatment of migraine in adults [5]. Multiple clinical trials have confirmed its efficacy, safety, and tolerability [6,7,8]. In the phase 2b/3 (MD-01) and phase 3 (ADVANCE) trials, all studied doses of atogepant significantly reduced mean monthly migraine days across 12 weeks of treatment compared with placebo; the proportions of atogepant participants with ≥ 50% reduction in monthly migraine days across 12 weeks of treatment ranged from 52 to 62% [6, 7]. Moreover, in an open-label trial, 84% of atogepant participants achieved ≥ 50% reduction in monthly migraine days across 52 weeks of treatment [8]. This post hoc analysis using pooled data across four phase 3 clinical trials evaluated the overall safety and tolerability profile of atogepant for the preventive treatment of episodic migraine (EM) in adults, including the occurrence of adverse events (AEs) of interest. Based on the potential hepatotoxicity of first-generation gepants, treatment-emergent elevations in liver enzymes were evaluated as prespecified AEs of interest throughout the phase 3 clinical program of atogepant, a second-generation gepant [9, 10]. Given the potential effect on inhibition of vasodilation through the anti-CGRP mechanism of action, cardiac disorders, including hypertension, were also deemed AEs of interest [11, 12]. Identifying treatments that do not result in weight gain is important, as obesity is a common comorbidity and risk factor for disease progression in people with migraine [13]. Therefore, a change in body weight of ≥ 7% from baseline was determined as potentially clinically significant during the clinical trials and also an AE of interest.
Methods
Study design
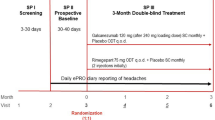
This original research is a pooled analysis that assessed the safety and tolerability of atogepant in adults with EM using data from 2 randomized, double-blind, placebo-controlled trials (RCTs; phase 2b/3 [MD-01], NCT02848326; phase 3 [ADVANCE], NCT03777059) and 2 open-label long-term safety (LTS) trials (52 weeks, NCT03700320; 40 weeks, NCT03939312) (Table 1). The phase 2b/3 trial evaluated atogepant 10, 30, and 60 mg once daily and 30 and 60 mg twice daily versus placebo [6]. The ADVANCE trial evaluated the efficacy and safety of once-daily atogepant 10, 30, and 60 mg versus placebo [7]. Participants who completed one of these trials were eligible to participate in the LTS trials (phase 2b/3 and ADVANCE trial participants were eligible to enroll in the 52-week and 40-week LTS trials, respectively). Both LTS trials assessed the safety and tolerability of once-daily atogepant 60 mg [8, 14]. In the 52-week LTS trial, a standard care (SC) arm was included to contextualize long-term safety data [8]. Participants in the SC group could have been prescribed an alternative medication, not prescribed any migraine preventive medication, or discontinued migraine preventive medication as often as needed throughout the study. These results focused on the US-approved atogepant doses for EM of 10, 30, and 60 mg once daily, as twice-daily dosing is not approved [5].
All trials were performed in compliance with the International Conference on Harmonisation E6 Guideline for Good Clinical Practice and the principles of the Declaration of Helsinki. Each investigator obtained approval from an independent ethics committee or a local institutional review board. Before administration of any study procedures, participants provided written informed consent.
Participants
Inclusion and exclusion criteria for each study were published previously [6,7,8, 14]. Eligible participants were adults with 4–14 migraine days per month in the 3 months before visit 1 and 4–14 migraine days in the 28-day baseline period. Participants were diagnosed with migraine with or without aura according to the International Classification of Headache Disorders, 3rd edition [15], > 1 year before screening, with diagnosis made before the age of 50 years.
Safety parameters
Safety assessments were reported by participants throughout the trials and included evaluation of treatment-emergent AEs (TEAEs) for seriousness and relationship to study medication (as determined by the investigator), TEAEs leading to discontinuation, lab monitoring, electrocardiograms, and the Columbia Suicide Severity Rating Scale questionnaire. The intensity of each TEAE was assessed as mild (does not generally interfere with usual activities of daily living), moderate (interferes with usual activities of daily living), or severe (interrupts usual activities of daily living). Notably, TEAEs were not treatment related. Serious AEs (SAEs) were defined based on investigator judgement as those that were life-threatening or resulted in hospitalization, disability, or death, or events that may require medical or surgical intervention to prevent hospitalization, disability, or death. The following events were also highlighted due to clinical interest: alanine aminotransferase (ALT) or aspartate aminotransferase (AST) concentration ≥ 3 times the upper limit of normal (3 × ULN) and potential Hy’s law cases (defined as concurrent ALT or AST elevation ≥ 3 × ULN, bilirubin elevation ≥ 2 × ULN, and alkaline phosphatase value < 2 × ULN, in any of the clinical trials), weight changes, and cardiac disorders (including hypertension). Potentially clinically significant weight loss was defined as ≥ 7% reduction of body weight at any time postbaseline.
Statistical analyses
Safety assessments were performed on the pooled safety population, which included participants who received ≥ 1 dose of study medication. AE data were collected through the last visit and are reported as number (percentage) of the pooled safety population (pooled RCTs and pooled LTS trials). AEs were classified by investigators by severity, potential relationship to study medication, start and stop dates, and seriousness. Demographics and baseline characteristics were summarized for the safety population. Descriptive statistics (n, mean, standard deviation [SD], median, minimum, and maximum) were presented for continuous variables. Frequency distributions (numbers and percentages) were reported for categorical variables.
Results
Participants
A total of 1550 participants were analyzed across the 2 pooled RCTs (Supplemental Fig. 1A; Table 1) and 1424 participants in the pooled LTS trials (Supplemental Fig. 1B; Table 1). Of the LTS trial participants, 792 were previously enrolled in an RCT (MD-01: 107; ADVANCE: 685). Demographic and baseline characteristics are summarized in Table 2.
Treatment-emergent adverse events
TEAEs for the pooled safety population are summarized in Table 3. In the RCTs, 643/1142 (56.3%) atogepant participants and 218/408 (53.4%) placebo participants experienced ≥ 1 TEAEs. In the LTS trials, 792/1228 (64.5%) atogepant participants and 154/196 (78.6%) SC participants experienced ≥ 1 TEAEs.
The most commonly reported TEAEs (≥ 5%) with once-daily atogepant were upper respiratory tract infection (5.3% in RCTs, 7.7% in LTS trials), constipation (6.1% in RCTs, 5.0% in LTS trials), nausea (6.6% in RCTs, 4.6% in LTS trials), and urinary tract infection (3.4% in RCTs, 5.2% in LTS trials). The majority of the TEAEs were mild or moderate in severity (Table 4).
Treatment-related TEAEs and serious TEAEs
Most TEAEs were considered not related to the study drug by the investigator in the RCTs and LTS trials. In the RCTs, 228/1142 (20.0%) atogepant participants and 50/408 (12.3%) placebo participants experienced ≥ 1 treatment-related TEAEs (TR-TEAEs). In the LTS trials, 158/1228 (12.9%) atogepant participants experienced ≥ 1 TR-TEAEs. The most commonly reported TR-TEAEs (> 2%) in atogepant participants were constipation (RCTs: 4.7% [54/1142]; LTS trials: 3.0% [37/1228]), nausea (RCTs: 4.0% [46/1142]; LTS trials: 2.0% [24/1228]), and fatigue (RCTs: 1.7% [19/1142]; LTS trials: 1.1% [14/1228]) (Table 5).
Serious TEAEs in the RCTs were reported in 7 (0.6%) atogepant participants compared with 4 (1.0%) in the pooled placebo group. In the LTS trials, 47 (3.8%) atogepant participants and 7 (3.6%) SC participants reported any serious TEAE (Table 3). With the exception of 1 case of optic neuritis, all serious TEAEs were considered by the investigator to be unrelated to study treatment. The case of optic neuritis occurred in a 23-year-old woman who received atogepant 10 mg once daily; magnetic resonance imaging of the brain and orbits, and visual-evoked potential results were normal, and the optic neuritis resolved without any sequela. Serious TEAEs are summarized in Table 6. In the LTS trials, 2 deaths were reported, 1 due to homicide and 1 due to beta-hemolytic streptococcal infection (toxic shock syndrome), both of which were deemed unrelated to atogepant per the investigator.
Treatment discontinuations
In the pooled RCTs, the proportions of participants with TEAEs leading to discontinuation were 3.5% (40/1142) with atogepant and 2.7% (11/408) with placebo. In the pooled LTS trials, 4.3% (53/1228) of atogepant participants and 2.6% (5/196) of SC participants discontinued due to TEAEs (Table 3). No dose–response relationship was observed for TEAEs leading to discontinuation. The AEs that most led to discontinuation in RCTs were constipation (0.5%), nausea (0.5%), and fatigue/somnolence (0.5%). The AEs that most led to discontinuation in the LTS trials were nausea (0.5%) and dizziness (0.3%).
AEs of interest
AEs of interest included AEs commonly reported with atogepant and ones that are of interest to health care professionals (Table 4).
Constipation
Constipation was reported in 6.1% (70/1142) of atogepant participants in the RCTs and in 5.0% (62/1228) of atogepant participants in the LTS trials. Most cases of constipation were mild or moderate in severity and there was no clear dose dependency. There were no SAEs of constipation, including no constipation-related complications (eg, hospitalization, ileus). Few TEAEs of constipation resulted in discontinuation (RCTs: 0.5% [6/1142], LTS trials: 0.2% [2/1228]). Most cases (RCTs: 71.4% [50/70], LTS trials: 45.2% [28/62]) occurred within the first 2 weeks after treatment initiation, and the majority (RCTs: 64.3% [45/70], LTS trials: 87.1% [54/62]) resolved by the end of the study, either spontaneously or with over-the-counter treatment.
Nausea
Nausea was reported at rates of 6.6% (75/1142) in the RCTs and 4.6% (57/1228) in the LTS trials. The majority of cases were mild in severity. No SAEs of nausea occurred. Few instances of nausea led to discontinuation (RCTs: 0.4% [5/1142], LTS trials: 0.5% [6/1228]). Most cases (RCTs: 54.7% [41/75], LTS trials: 36.8% [21/57]) occurred within the first 2 weeks after treatment initiation, and the majority (RCTs: 94.7% [71/75], LTS trials: 96.5% [55/57]) of cases resolved by the end of the study.
Hepatic safety
Hepatic safety was evaluated thoroughly in all clinical trials through AE reporting and lab monitoring. An external clinical adjudication committee provided a blinded review and adjudication of all post-treatment elevations of ALT or AST ≥ 3 × ULN to assess their causal relationship to atogepant. In the RCTs, 1.3% (15/1142) and 1.1% (12/1142) of atogepant participants experienced a TEAE of increased ALT or AST, respectively (placebo: ALT, 2.2% [9/408]; AST, 2.0% [8/408]). In the LTS trials, 1.3% (16/1228) and 1.6% (20/1228) experienced a TEAE of increased ALT or AST, respectively (SC: ALT, 2.0% [4/196]; AST, 2.6% [5/196]) (Table 4).
There were no potential Hy’s law cases. In the RCTs, the rates of ALT or AST elevation ≥ 3 × ULN were similar between those who received atogepant (1.0% [11/1126]) and those who received placebo (1.8% [7/399]). In the LTS trials, ALT or AST elevation ≥ 3 × ULN was observed in 1.4% (17/1214) with atogepant and 3.2% (6/190) with SC. The adjudication committee determined most cases to be unlikely related to atogepant and a few to be probably or possibly (8 cases in RCTs and LTS trials) related to atogepant. Among the possible/probable cases, confounding factors were also identified in all but 1 case.
Weight changes
In the RCTs, the percentages of participants with a weight decrease of a clinically significant weight loss of ≥ 7% at any time point during the 12 weeks were 3.8% for atogepant 10 mg, 3.2% for atogepant 30 mg, and 4.9% for atogepant 60 mg, compared with 2.8% for placebo. At week 12, the percentage changes from baseline for atogepant 10 mg, 30 mg, and 60 mg were 0.12, − 0.51, and − 1.02. In the LTS trials, the percentages of clinically significant weight loss were 14.7% for those treated with SC and 24.1% for those treated with atogepant 60 mg once daily. At week 4 and week 40, the percentage changes from baseline for atogepant 60 mg were − 0.42 and − 2.38, respectively, in the 52-week LTS trial, and − 0.76 and − 2.09, respectively, in the 40-week LTS trial. Weight loss appeared to be dose- and duration-dependent.
The percentages of atogepant participants who reported a TEAE of decreased weight were 0.4% in the RCTs and 2.6% in the LTS trials (Table 4). Discontinuation due to weight loss as a TEAE was rare (0 in the RCTs and 2 participants in the LTS trials). An exploratory analysis revealed no clear relationship between weight change and nausea or vomiting, but a slightly higher incidence of decreased appetite was observed in weight-loss responders.
Cardiac Disorders and Hypertension
In the RCTs and LTS trials, cardiac disorders were uncommon TEAEs. Hypertension was reported by 0.4% (5/1142) of atogepant participants and 0% of placebo participants in the RCTs, and by 1.9% (23/1228) of atogepant participants and 1.0% (2/196) of SC participants in the LTS trials (Table 4). There were no serious cases of hypertension in any of the clinical trials. One participant in each of the pooled RCTs and pooled LTS trials discontinued due to hypertension. No cases in the RCTs were considered treatment related. One nonserious case of mild hypertension in the LTS trials was considered related to atogepant treatment by the investigator. Blood pressure was measured at each participant visit, and the data collected across RCTs and LTS trials did not reveal any clinically relevant changes in blood pressure. Other cardiac disorders (including atrioventricular block first degree, atrioventricular block second degree, left bundle branch block, left atrial enlargement, palpitations, postural orthostatic tachycardia syndrome, and supraventricular extrasystoles) were experienced by 1.4% (16/1142) of atogepant participants and 1.0% (4/408) of placebo participants in the RCTs and by 1.3% (16/1228) of atogepant participants and 2.6% (5/196) of SC participants in the LTS trials.
Discussion
Preventive migraine therapies have been underutilized at least in part due to limited efficacy and poor tolerability of the oral nonspecific generic treatments [3]. Atogepant is a migraine-specific preventive treatment that has demonstrated rapid and continuous reductions in mean monthly migraine days among adults with episodic and chronic migraine [6, 7, 16, 17]. Analyses of pooled data from 4 phase 3 clinical studies [2, 6, 8, 14] indicate that once-daily atogepant may offer a more favorable safety and tolerability profile for the preventive treatment of EM in adults. Most TEAEs in the 4 clinical studies were mild to moderate in severity and considered unrelated to the study drug. The proportions of serious TEAEs were similar in the atogepant and placebo groups.
Among frequently reported TEAEs were constipation, nausea, and fatigue/somnolence, with most cases mild or moderate in severity and managed through standard clinical practice or resolving spontaneously. As atogepant can be administered with or without food [5], the incidence of nausea might be reduced by taking it with food.
In all four clinical trials, no potential Hy’s law cases were reported. A few cases of ALT/AST elevations ≥ 3 × ULN were temporally associated with atogepant, but all were nonserious, mild to moderate in severity, without concurrent bilirubin elevations, and resolved with or without atogepant discontinuation. No dose adjustments are required for mild or moderate hepatic impairment [5]. However, atogepant is not recommended in individuals with known severe hepatic impairment.
The administration of atogepant was associated with modest dose- and duration-dependent weight loss, without a significant clinical impact, as reflected by the low adverse event reporting rates and study drug discontinuation. The underlying mechanism for this observation remains unknown.
This analysis showed a low incidence of cardiovascular AEs associated with atogepant, which is consistent with the published literature for other anti-CGRP therapies [18, 19]. However, as CGRP is a potent vasodilator [20], concerns exist regarding the use of therapies that target the CGRP pathway and blood pressure regulation. In a prospective follow-up study of anti-CGRP mAbs, increased mean systolic and diastolic blood pressure was observed after 3 months of treatment and continued throughout 12 months [11]. Although our findings show that 5 participants treated with atogepant experienced a TEAE of hypertension in the RCTs, none of the cases were deemed to be treatment related. In a post hoc analysis of participants with cardiovascular risk factors, without significant cardiovascular diseases, a low incidence of overall cardiovascular TEAEs was observed, and none were serious [21]. These results suggest the safety of atogepant in those with cardiovascular risk factors. Additionally, AEs of atogepant tend to resolve rapidly upon its discontinuation due to its half-life of approximately 11 h and elimination within approximately 2 days [5].
Pooled analyses increase the power to detect potentially rare events that may have been missed in single studies, but they have limitations [22]. This pooled analysis included participants with 4–14 migraine days per month and hence excluded participants with chronic migraine, limiting generalizability. However, a separate clinical trial of atogepant for the preventive treatment of chronic migraine has demonstrated positive efficacy results and a similar safety and tolerability profile [16]. Moreover, participants demonstrating greater tolerability in the RCTs were more prone to enroll in the LTS trials. Furthermore, the LTS trials were open-label trials that may have had potential inherent biases. Lastly, we acknowledge that additional studies are warranted to further evaluate the safety of atogepant in a more diverse patient population.
Conclusion
In summary, atogepant showed a favorable safety and tolerability profile in adults with EM. The most common TEAEs associated with atogepant were mild to moderate constipation, nausea, fatigue, and somnolence that did not lead to discontinuation. Taken together with existing data on the efficacy and safety of atogepant, this analysis further supports the safety and tolerability of atogepant for the preventive treatment of EM.
Availability of data and materials
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This includes access to anonymized, individual, and trial-level data (analysis data sets), as well as other information (eg, protocols, clinical study reports, or analysis plans), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications.
These clinical trial data can be requested by any qualified researchers who engage in rigorous, independent, scientific research, and will be provided following review and approval of a research proposal, Statistical Analysis Plan, and execution of a Data Sharing Agreement. Data requests can be submitted at any time after approval in the US and Europe and after acceptance of this manuscript for publication. The data will be accessible for 12 months, with possible extensions considered. For more information on the process or to submit a request, visit the following link: https://vivli.org/ourmember/abbvie/ then select “Home.”
Abbreviations
- AE:
-
Adverse event
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CGRP:
-
Calcitonin gene–related peptide
- EM:
-
Episodic migraine
- LTS:
-
Long-term safety
- RCT:
-
Randomized, double-blind, placebo-controlled trial
- SC:
-
Standard care
- TEAE:
-
Treatment-emergent adverse event
- TR-TEAE:
-
Treatment-related treatment-emergent adverse event
- ULN:
-
Upper limit of normal
References
Ashina M (2020) Migraine. N Engl J Med 383:1866–1876
Ailani J, Burch RC, Robbins MS (2021) The American Headache Society consensus statement: update on integrating new migraine treatments into clinical practice. Headache 61:1021–1039
American Headache Society (2019) The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache 59:1–18
Eigenbrodt AK, Ashina H, Khan S, Diener HC, Mitsikostas DD, Sinclair AJ et al (2021) Diagnosis and management of migraine in ten steps. Nat Rev Neurol 17:501–514
Qulipta (2023) AbbVie
Goadsby PJ, Dodick DW, Ailani J, Trugman JM, Finnegan M, Lu K et al (2020) Safety, tolerability, and efficacy of orally administered atogepant for the prevention of episodic migraine in adults: a double-blind, randomised phase 2b/3 trial. Lancet Neurol 19:727–737
Ailani J, Lipton RB, Goadsby PJ, Guo H, Miceli R, Severt L et al (2021) Atogepant for the preventive treatment of migraine. N Engl J Med 385:695–706
Ashina M, Tepper SJ, Reuter U, Blumenfeld AM, Hutchinson S, **a J et al (2023) Once-daily oral atogepant for the long-term preventive treatment of migraine: findings from a multicenter, randomized, open-label, phase 3 trial. Headache 63:79–88
Messina R, Goadsby PJ (2019) CGRP—a target for acute therapy in migraine: clinical data. Cephalalgia 39:420–427
Negro A, Lionetto L, Simmaco M, Martelletti P (2012) CGRP receptor antagonists: an expanding drug class for acute migraine? Expert Opin Investig Drugs 21:807–818
de Vries LS, van der Arend BWH, Maassen VanDenBrink A, Terwindt GM (2022) Blood pressure in patients with migraine treated with monoclonal anti-CGRP (receptor) antibodies: a prospective follow-up study. Neurology 99:e1897–e1904
Robblee J, Harvey LK (2022) Cardiovascular disease and migraine: are the new treatments safe? Curr Pain Headache Rep 26:647–655
Kristoffersen ES, Børte S, Hagen K, Zwart JA, Winsvold BS (2020) Migraine, obesity and body fat distribution—a population-based study. J Headache Pain 21:97
Klein BC, Miceli R, Severt L, McAllister P, Mechtler L, McVige J et al (2023) Safety and tolerability results of atogepant for the preventive treatment of episodic migraine from a 40-week, open-label multicenter extension of the phase 3 ADVANCE trial. Cephalalgia 43:3331024221128250
Headache Classification Committee of the International Headache Society (2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38:1–211
Pozo-Rosich P, Ailani J, Ashina M, Goadsby PJ, Lipton RB, Reuter U et al (2023) Atogepant for the preventive treatment of chronic migraine (PROGRESS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 402:775–785
Schwedt TJ, Lipton RB, Ailani J, Silberstein SD, Tassorelli C, Guo H et al (2022) Time course of efficacy of atogepant for the preventive treatment of migraine: results from the randomized, double-blind ADVANCE trial. Cephalalgia 42:3–11
Smith TR, Spierings ELH, Cady R, Hirman J, Schaeffler B, Shen V et al (2021) Safety and tolerability of eptinezumab in patients with migraine: a pooled analysis of 5 clinical trials. J Headache Pain 22:16
Lampl C, Kraus V, Lehner K, Loop B, Chehrenama M, Maczynska Z et al (2022) Safety and tolerability of erenumab in individuals with episodic or chronic migraine across age groups: a pooled analysis of placebo-controlled trials. J Headache Pain 23:104
Edvinsson L, Haanes KA, Warfvinge K, Krause DN (2018) CGRP as the target of new migraine therapies - successful translation from bench to clinic. Nat Rev Neurol 14:338–350
Blumenfeld AM, Pavlovic JM, Harriott A, Best PJ, Monteith T, Ferreira R et al (2022) Post-hoc analysis evaluating safety of atogepant in ADVANCE & open-label extension participants with cardiovascular risk factors [abstract P-137]. Headache 62(suppl 1):119
Ashina M, Kudrow D, Reuter U, Dolezil D, Silberstein S, Tepper SJ et al (2019) Long-term tolerability and nonvascular safety of erenumab, a novel calcitonin gene-related peptide receptor antagonist for prevention of migraine: a pooled analysis of four placebo-controlled trials with long-term extensions. Cephalalgia 39:1798–1808
Acknowledgements
Medical writing support was provided by Anny Wu, PhD, of Peloton Advantage, LLC, an OPEN Health company, and was funded by AbbVie.
Funding
AbbVie funded this trial and contributed to the study design, the collection, analysis, and interpretation of data, and the review and approval of the final version for publication. All authors had access to relevant data and participated in the drafting, review, and approval of this publication. No honoraria or payments were made for authorship.
Author information
Authors and Affiliations
Contributions
BD contributed to the study design. JA was the study investigator and enrolled patients. JM and BD collected and assembled study data. JM, BD, RDF, and JHS performed data analysis. All authors contributed to data interpretation, manuscript preparation, review, revision, and approval of the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All trials were performed in compliance with the International Conference on Harmonisation E6 Guideline for Good Clinical Practice and the principles of the Declaration of Helsinki. Each investigator obtained approval from an independent ethics committee or a local institutional review board. Before administration of any study procedures, participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
PR reports no relevant disclosures. MJM within the past 24 months, has received compensation for consultation from Alder/Lundbeck, Axsome, Satsuma, Supernus, and Theranica; has participated in speaker bureaus for Amgen/Novartis and Eli Lilly; has received institutional support for serving as principal investigator for Allergan/AbbVie, and Teva; and has received payments for authorship or royalties from Cambridge University Press, Demos Medical, and MedLink. JR has received grant support from Barrow Neurological Foundation and investigator support from AbbVie and Eli Lilly; has served as a speaker for Impel; has a paid editorial relationship with MedLink Neurological and Neurodiem; and discloses that a family member has partial ownership of Scottsdale Providence Recovery Center. JM has served as a speaker and/or received research support from Alder, Allergan (now AbbVie), Amgen/Novartis, Avanir, Biohaven, Eli Lilly, Lundbeck, and Teva. SS has participated in advisory boards and/or is a speaker for Allergan (now AbbVie), Amgen, BDSI, Biohaven, Eli Lilly, Impel NeuroPharma, and Teva. SJN has received honoraria for consulting from Alder/Lundbeck, Allergan/AbbVie, Axsome (ended January 2022), BioDelivery Sciences (ended February 2022), Biohaven (ended November 2021), Eli Lilly, Teva (ended October 2021), Theranica (ended September 2022); has received honoraria for speaking from Eli Lilly (ended September 2021); has received honoraria for work in education or publishing from American Academy of Neurology, American Headache Society, Evolve Med Ed, Massachusetts Medical Society, MedLink Neurology, MJH Life Sciences, NACCME, Neurology Learning Network, Pennsylvania Neurologic Society, Springer, WebMD/Medscape, Wolters-Kluwer; has received legal fees for serving as a medical expert to Jackson & Campbell. JA has served as a consultant for AbbVie, Aeon, Amgen, Biohaven, Eli Lilly, GlaxoSmithKline, Gore, Impel, Linpharma, Lundbeck, Miravo, Nesos, Neurolief, Pfizer, Satsuma, Teva, and Theranica; received stock options from Ctrl M; provided editorial services to Current Pain and Headache Reports, SELF, and Medscape; and received clinical trial support from AbbVie, Biohaven, Eli Lilly, Rehaler, Satsuma, and Zosano. RDF, JM, JHS, and BD are employees of AbbVie and may hold AbbVie stock. MA has received personal fees from AbbVie, Amgen, Eli Lilly, GlaxoSmithKline, Lundbeck, Novartis, Pfizer and Teva; has participated in clinical trials as the principal investigator for AbbVie, Amgen, Eli Lilly, Lundbeck, Novartis, Pfizer and Teva; has received research grants from Lundbeck Foundation, Novo Nordisk Foundation, and Novartis; serves as associate editor of Cephalalgia, associate editor of The Journal of Headache and Pain, and associate editor of Brain; and has no ownership interest and does not own stocks of any pharmaceutical company.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Figure 1.
Participant disposition in the randomized, placebo-controlled (A) and long-term safety (B) trials.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rizzoli, P., Marmura, M.J., Robblee, J. et al. Safety and tolerability of atogepant for the preventive treatment of migraine: a post hoc analysis of pooled data from four clinical trials. J Headache Pain 25, 35 (2024). https://doi.org/10.1186/s10194-024-01736-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-024-01736-z