Abstract
Background
Multisystem Inflammatory Syndrome in Children (MIS-C) is a life-threatening complication of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, which manifests as a hyper inflammatory process with multiorgan involvement in predominantly healthy children in the weeks following mild or asymptomatic coronavirus disease 2019 (COVID-19). However, host monogenic predisposing factors to MIS-C remain elusive.
Methods
Herein, we used whole exome sequencing (WES) on 16 MIS-C Brazilian patients to identify single nucleotide/InDels variants as predisposition factors associated with MIS-C.
Results
We identified ten very rare variants in eight genes (FREM1, MPO, POLG, C6, C9, ABCA4, ABCC6, and BSCL2) as the most promising candidates to be related to a higher risk of MIS-C development. These variants may propitiate a less effective immune response to infection or trigger the inflammatory response or yet a delayed hyperimmune response to SARS-CoV-2. Protein–Protein Interactions (PPIs) among the products of the mutated genes revealed an integrated network, enriched for immune and inflammatory response mechanisms with some of the direct partners representing gene products previously associated with MIS-C and Kawasaki disease (KD). In addition, the PPIs direct partners are also enriched for COVID-19-related gene sets. HLA alleles prediction from WES data allowed the identification of at least one risk allele in 100% of the MIS-C patients.
Conclusions
This study is the first to explore host MIS-C-associated variants in a Latin American admixed population. Besides expanding the spectrum of MIS-C-associated variants, our findings highlight the relevance of using WES for characterising the genetic interindividual variability associated with COVID-19 complications and ratify the presence of overlap**/convergent mechanisms among MIS-C, KD and COVID-19, crucial for future therapeutic management.
Similar content being viewed by others
Background
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is generally milder in children than in adults (Stokes et al. 2020; Götzinger et al. 2020). Nonetheless, in April 2020, a novel entity following SARS-CoV-2 primary infection has emerged in a small subset of children and adolescents and termed “Multisystem Inflammatory Syndrome in Children" (MIS-C) (Riphagen et al. 2020; Verdoni et al. 2020). The Centers for Disease Control definition for MIS-C includes an individual aged < 21 years with a minimum of 24-h of fever > 38.0 °C, severe illness requiring hospitalization with two or more organ systems affected (i.e., cardiac, renal, respiratory, hematologic, gastrointestinal, dermatological, neurological), laboratory evidence of inflammation, laboratory or epidemiological evidence of prior SARS-CoV-2 infection and no alternative diagnosis. The syndrome occurs about three to six weeks after mild or asymptomatic SARS-CoV-2 infection without detectable viral shedding in the respiratory tract (Consiglio et al. 2020; Belot et al. 2020), although SARS-CoV-2 mRNA is noticeable in more than 10% in faecal samples of MIS-C patients up to > 21 days from the presumed contact with the virus (Parodi et al. 2021). The main clinical features of MIS-C include persistent fever, gastrointestinal (GI) symptoms (diarrhea, emesis and abdominal pain), conjunctivitis, cardiac dysfunction, neurological symptoms (headache, confusion, lethargy), shock, rash, lymphopenia, neutrophilia, and hyperferritinemia (Syrimi et al. 2021; Jiang et al. 2022). Some of these features overlap to the symptoms present in the autoimmune Kawasaki disease, and other inflammatory paediatric conditions, such as toxic shock syndrome and hemophagocytic lymphohistiocytosis/macrophage activation syndrome, although the outcomes are distinct (Nakra et al. 2020; Sancho-Shimizu et al. 2021). The geographic distribution of MIS-C is not uniform worldwide, with higher numbers of cases reported in Europe, the Americas, Africa, South Asia, and the Middle East and an expressive scarcity of cases in countries of the East Asia, in which the number of COVID-19 cases was lower (Sancho-Shimizu et al. 2021).
During the past 2 years, some immunopathogenic mechanisms subjacent to MIS-C have begun to be elucidated, including a hyperinflammatory response with increased levels of serum cytokines and endothelial injury, immune dysfunction, a possible role for complement/coagulation, myeloid cell activation and autoimmune dysregulation (Sancho-Shimizu et al. 2021; Ramaswamy et al. 2021; Fraser et al. 2021; Porritt et al. 2021b). Besides, MIS-C patients display uncontrolled neutrophil activation and neutrophil extracellular trap release in the vasculature (Boribong et al. 2021). MIS-C transcriptional signature in blood also partially shares the transcriptional response to SARS-CoV-2 and the Kawasaki disease signature, with enrichment for exhausted CD8* T-cells and CD56dimCD57* natural killer cells, suggesting downregulation of natural killer cells and cytotoxic T cell exhaustion response to SARS-CoV-2 infection in MIS-C, with TBX21, TGFBR3, C1ORF21, S1PR5, PRF1, MYBL1, KLRD1, SH2D1B, and GZMA genes as the key drivers of MIS-C pathogenesis (Beckmann et al. 2021). Besides, immunosequencing of MIS-C blood samples revealed expansion of T cell receptor beta variable gene 11-2 (TRBBV11-2), which is correlated to severity and serum cytokine levels, consistent with superantigen triggered immune responses of SARS-CoV-2 and autoimmune signatures (Porritt et al. 2021a; 2021b). Moreover, patients with TRBV11-2 expansion shared human leukocyte antigen class I (HLA-I) alleles A*02, B*35, and C*04, suggesting that MHC class I may mediate TRBV11-2 expansion in a specific HLA-I allele combination (Porritt et al. 2021a). Recently, a multi-omics approach to assess changes of innate and adaptive immune responses between paediatric COVID-19 and MIS-C revealed distinct immunopathological signatures, with MIS-C patients exhibiting elevated levels of soluble biomarkers related to recruitment and activation of monocytes and neutrophils, matrisome activation, vascular endothelium injury, and increased levels of circulating spike protein with no correlation with SARS-CoV-2 PCR status (Sacco et al. 2022). Besides, structure-based computational models demonstrated that the SARS-CoV-2 spike (S) glycoprotein exhibits a high-affinity motif for binding T-cell receptors and may form a ternary complex with major histocompatibility complex class II (MHCII) molecules. Finally, the interaction between SARS-CoV-2 and T cells could be strengthened by the SARS-CoV-2 variant D839Y/N/E (Cheng et al. 2020), which could point to a viral genetics’ contribution to MIS-C development.
It remains elusive, however, why some children previously infected with different SARS-CoV-2 strains develop MIS-C and most do not, suggesting that rare single-gene host genetic variants may have an essential role in increasing the susceptibility to MIS-C. Few studies exploring potential monogenic causes of MIS-C were conducted so far and, although Latino individuals appear to be overrepresented in epidemiological data of MIS-C in the United States studies, in which ancestry was reported (reviewed in Sancho-Shimizu et al. 2021), no whole exome sequencing (WES) study in patients with MIS-C from admixed populations of Latin America has been already conducted.
Herein, we searched for very rare (< 1%) or unique monogenic variants (single nucleotide variants—SNVs or InDels) that could predispose to SARS-CoV-2-triggered hyperinflammation or post-infectious immune/autoimmune dysregulation in a cohort of healthy Brazilian patients with MIS-C. Elucidating the risk factors for MIS-C following SARS-CoV-2 infection is crucial for possible preventive measures and patients’ management and prognosis concerning SARS-CoV-2 and other emergent viruses.
Methods
Study participants
A series of 16 children with MIS-C, diagnosed according to the World Health Organization criteria (WHO 2020), was referred to the Paediatric Intensive care unit from Pedro Ernesto University Hospital at State University of Rio de Janeiro and to the Pediatric Rheumatology Service from Instituto de Puericultura e Pediatria Martagão Gesteira at Federal University of Rio de Janeiro, Brazil, from May 2020 to July 2021. All MIS-C patients tested positive for COVID-19 by anti-SARS-CoV-2 antibodies (rapid test or serology) or RT-PCR, with exception of patients EXOC3 and EXOC11, who were non-reagent on serology tests and EXOC17, who was not individually tested. However, the three patients had direct contact with their parents infected by SARS-CoV-2, contemplating the MIS-C WHO criteria (WHO 2020). Two additional patients with MIS-C (EXOC8 and EXOC9) were ruled out from the study, due to insufficient DNA quality. The Institutional Ethics Committees approved the research protocols (CAAE 0135320.0.0000.5259 and 33040420.3.0000.5264) and written informed consent was obtained from the participants and their parents.
DNA extraction and whole exome sequencing
Peripheral blood samples from MIS-C children were collected after recovery using Tempus™ Blood RNA Tube (Thermo Fisher Inc.) and DNA samples were extracted using Flexigene Kit or QIAamp DNA Blood mini kit (QIAGEN). Sequencing libraries were prepared using the QIAseq Human Exome Kit (Qiagen), according to the manufacturer's protocol. Sequencing was performed using Illumina NextSeq® 500/550 High Output Kit v2 (300 cycles), generating 2 × 149 bp paired-end reads with depth coverage of at least ×100. The short reads were mapped to the human reference genome (GRCh38/hg38) using Bowtie2 version 2.3.4.1 (Langmead and Salzberg 2012). SAM files were converted into BAM files, sorted and filtered by MAP** Quality (MAPQ > 30) using SAMtools version 1.3 (Li et al. 2009; Langmead and Salzberg 2012). MarkDuplicates from Picard tools version 2.18 (http://picard.sourceforge.net/) was applied to mark duplicate reads. SNVs/InDels variants calling was performed using the HaplotypeCaller tool from Genome Analysis Toolkit (GATK) version 4.1 (DePristo et al. 2011).
Variants prioritization
The prioritization of potentially pathogenic variants related to a high MIS-C risk was performed according to Vianna et al. (2020) with modifications. The filtered variants’ features included (a) sequencing and map** quality over 30 and read depth over 10; (b) non-synonymous or splice sites variants with moderate or high predicted functional impact according to Variant Effect Predictor (Ensembl) (McLaren et al. 2016); (c) SIFT and/or Polyphen values between 0–0.15 and 0.85–1.0, respectively for coding non-synonymous single nucleotide variants; (d) global minor allele frequency less than 0.01 in at least one populational database (1000 Genomes; ESP6500; Exome Aggregation Consortium—ExAC; The Genome Aggregation Database—GnomAD; and the Brazilian genomic variants database ABraOM).
For better exploring the pathogenic and conservation context of the filtered variants, Varsome (Kopanos et al. 2019) and Variant Effect Predictor (Ensembl) (McLaren et al. 2016) were used for accessing additional computational predictors, including Mutation Taster, Mutation Assessor, M-CAP, Revel, PROVEAN, MetaLR, MetaSVM, MetaRNN, CADD, LRP, GERP++, FATHMM, PhastCons, PhyloP, and Splice Al. OMIM (https://omim.org/), ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/), and Orphanet (https://www.orpha.net/consor/cgi-bin/index.php) were used to search for association with known diseases and inheritance patterns. Only variants with zygosity profiles consistent with the reported inheritance pattern of the related genes were selected. Gene Ontology and KEGG were used to provide functional or pathway annotation for the selected genes. Finally, filtered variants were classified according to the guidelines of the American College of Medical Genetics (ACMG) (Richards et al. 2015). Then, the filtered variants were validated by Sanger sequencing.
HLA prediction
The HLA alleles were predicted from WES samples with the HLAminer tool (Warren et al. 2012), using the genomic sequences of classes I and II HLA retrieved from the IMGT/HLA database in FASTA format. WES sequences in FASTQ format were mapped against chromosome 6 (GRCh38) using bowtie2 (Langmead and Salzberg 2012) to direct analysis to the chromosome of the HLA loci. The sequences recovered were assembled into 200 bp contigs using the TASR tool (Warren and Holt 2011) and aligned to HLA reference sequences using BLAST (Basic Local Alignment Tool). Aligned sequences were then used to predict HLA alleles, including HLA class I (HLA-A, HLA-B, HLA-C, HLA-G, HLA-E, HLA-F) and HLA class II [HLA-DP (DPA1, DPB1, DPB2), HLA-DQ (DQA1, DQA2, DQB1), HLA-DR (DRA, DRB1, 3, 4, 5)].
Integrative bioinformatic analysis
The context of the filtered variants was analyzed at the functional domain level. The annotation of functional domains was retrieved through the Pfam 32.0 platform (El-Gebali et al. 2019) and the protein architecture was represented with IBS (Liu et al. 2019). Particularly, ALDH7A1 was reported to attenuate reactive aldehyde and oxidative stress-induced cytotoxicity (Brocker et al. 2011). So, as oxidative stress is present in MIS-C patients, we cannot completely discard the involvement of a subclinical less effective ALDH7A1 enzyme over MIS-C risk, even that ALDH7A1 variants were only related to a clinical trait (OMIM 107323) in a homozygous or compound heterozygous status.
The variants identified in previous MIS-C studies were not detected in our cohort and there are no overlap** variants among previous studies. The absence of common variants in different studies could be mainly due to the rarity of the variants, the small number of studies focusing on host genetic susceptibility to MIS-C and discrepancies concerning patients’ selection and experimental design. However, in our study, there is clear a recurrence of variants in genes within the same family, such as ABCA4/ABCC6 and C6/C9.
We also examined the MIS-C samples for class I and II HLA alleles. Regarding class I alleles, three major genotypes A*02, B*35, and C*04, previously described to increase the risk of MIS-C (Kouo et al. 2021; Mazer et al. 2022; Sacco et al. 2022), were found in ten (62.5%) of our patients (Additional file 5: Table S5). Concerning the HLA class II, risk alleles DRB1*15:01 and DQB1*06:02, observed in children with SARS-CoV-2 infection (Valentini et al. 2021), were predicted in five (31.2%) and eight (50%) of our patients, respectively (Additional file 5: Table S5). So, altogether HLA alleles prediction from WES data of the MIS-C patients allowed the identification of at least one risk allele in 100% of the patients.
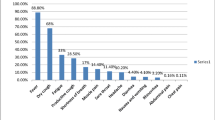
The frequencies of some clinical or laboratory findings in our cohort are quite different from what was reported in large non-genetic studies (Feldstein et al. 2020), including a higher proportion of coronary dilatations and thrombocytosis, as well as a lower prevalence of lymphocytopenia. We consider that these discrepancies could be a result of the small sample size or, alternatively, a feature of the Brazilian population. Indeed, the higher proportion of coronary dilatations is in accordance with a multicenter, prospective cohort study, conducted in 17 pediatric intensive care units in five states in Brazil, which revealed that 27% of 56 patients with MIS-C had signs of coronary dilatation (Lima-Setta et al. 2021). Besides, the patients with coronary alterations (all of them hospitalised in ICU) had thrombocytosis, which could be associated with the inflammatory involvement of the vascular endothelium. So, the inclusion of ICU children with a great severity may have caused an overestimation of thrombocytosis.
Conclusions
Host genetic predisposition knowledge on MIS-C risk remains limited and no study had been conducted in admixed populations of Latin America. We used WES to investigate very rare SNVs/InDels in MIS-C patients and identified ten very rare/unique variants in eight genes as the most promising candidates. Our findings highlight the relevance of using WES for identifying host genetic interindividual variability associated with COVID-19 complications and emphasize the need for COVID-19 prevention, even in children. Besides, characterization of host genetic factors predisposing to MIS-C may reveal biological mechanisms crucial for therapeutic management aiming to modify the worst outcomes.
Availability of data and materials
The variants herein described have been submitted to the National Center for Biotechnology Information (NCBI, BioProject ID: PRJNA848757).
References
Abolhassani H, Landegren N, Bastard P, Materna M, Modaresi M, Du L, et al. Inherited IFNAR1 deficiency in a child with both critical COVID-19 pneumonia and multisystem inflammatory syndrome. J Clin Immunol. 2022;42:471–83.
Ahmed M, Advani S, Moreira A, Zoretic S, Martinez J, Chorath K, et al. Multisystem inflammatory syndrome in children: a systematic review. EClinicalMedicine. 2020;26: 100527.
Bazewicz CG, Dinavahi SS, Schell TD, Robertson GP. Aldehyde dehydrogenase in regulatory T-cell development, immunity and cancer. Immunology. 2019;156:47–55.
Beckmann ND, Comella PH, Cheng E, Lepow L, Beckmann AG, Tyler SR, et al. Downregulation of exhausted cytotoxic T cells in gene expression networks of multisystem inflammatory syndrome in children. Nat Commun. 2021;12:4854.
Belot A, Antona D, Renolleau S, Javouhey E, Hentgen V, Angoulvant F, et al. SARS-CoV-2-related paediatric inflammatory multisystem syndrome, an epidemiological study, France, 1 March to 17 May 2020. Euro Surveill. 2020;25:2001010.
Boribong BP, LaSalle TJ, Bartsch YC, Ellett F, Loiselle ME, Davis JP, et al. Neutrophil Profiles of Pediatric COVID-19 and Multisystem Inflammatory Syndrome in Children. bioRxiv [Preprint]. 2021:2021.12.18.473308.
Brocker C, Cantore M, Failli P, Vasiliou V. Aldehyde dehydrogenase 7A1 (ALDH7A1) attenuates reactive aldehyde and oxidative stress induced cytotoxicity. Chem Biol Interact. 2011;191:269–77.
Cheng MH, Zhang S, Porritt RA, Noval Rivas M, Paschold L, Willscher E, et al. Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation. Proc Natl Acad Sci U S A. 2020;117:25254–62.
Chou J, Platt CD, Habiballah S, Nguyen AA, Elkins M, Weeks S, et al. Mechanisms underlying genetic susceptibility to multisystem inflammatory syndrome in children (MIS-C). J Allergy Clin Immunol. 2021;148:732-738.e1.
Consiglio CR, Cotugno N, Sardh F, Pou C, Amodio D, Rodriguez L, et al. The immunology of multisystem inflammatory syndrome in children with COVID-19. Cell. 2020;183(4):968-981.e7.
COVID-19 Host Genetics Initiative. Map** the human genetic architecture of COVID-19. Nature. 2021;600:472–7.
Dean M, Moitra K, Allikmets R. The human ATP-Binding Cassette (ABC) transporter superfamily. Hum Mutat. 2022;43:1162–82.
DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C, et al. A framework for variation discovery and genoty** using next-generation DNA sequencing data. Nat Genet. 2011;43:491–8.
El-Gebali S, Mistry J, Bateman A, Eddy SR, Luciani A, Potter SC, et al. The Pfam protein families database in 2019. Nucleic Acids Res. 2019;47:D427–32.
Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, et al. multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020;383:334–46.
Francisco Junior RDS, Lamarca AP, de Almeida LGP, Cavalcante L, Machado DT, Martins Y, et al. Turnover of SARS-CoV-2 lineages shaped the pandemic and enabled the emergence of new variants in the State of Rio de Janeiro, Brazil. Viruses. 2021;13:2013.
Fraser DD, Patterson EK, Daley M, Cepinskas G. Case report: inflammation and endothelial injury profiling of COVID-19 pediatric multisystem inflammatory syndrome (MIS-C). Front Pediatr. 2021;9: 597926.
Fuke S, Kametani M, Yamada K, Kasahara T, Kubota-Sakashita M, Kujoth GC, et al. Heterozygous Polg mutation causes motor dysfunction due to mtDNA deletions. Ann Clin Transl Neurol. 2014;1:909–20.
Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653–61.
Holter JC, Pischke SE, de Boer E, Lind A, Jenum S, Holten AR, et al. Systemic complement activation is associated with respiratory failure in COVID-19 hospitalized patients. Proc Natl Acad Sci U S A. 2020;117:25018–25.
Horiuchi T, Nishizaka H, Kojima T, Sawabe T, Niho Y, Schneider PM, et al. A non-sense mutation at Arg95 is predominant in complement 9 deficiency in Japanese. J Immunol. 1998;160:1509–13.
Jiang L, Tang K, Irfan O, Li X, Zhang E, Bhutta Z. Epidemiology, clinical features, and outcomes of multisystem inflammatory syndrome in children (MIS-C) and adolescents-a live systematic review and meta-analysis. Curr Pediatr Rep. 2022;10:19–30.
Jost PJ, Vucic D. Regulation of Cell Death and Immunity by XIAP. Cold Spring Harb Perspect Biol. 2020;12: a036426.
Kashem MA, Li H, Liu LR, Liang B, Omange RW, Plummer FA, Luo M. The potential role of FREM1 and its isoform TILRR in HIV-1 acquisition through mediating inflammation. Int J Mol Sci. 2021a;22:7825.
Kashem MA, Yuan XY, Li L, Kimani J, Plummer F, Luo M. TILRR (toll-like interleukin-1 receptor regulator), an important modulator of inflammatory responsive genes, is circulating in the blood. J Inflamm Res. 2021b;14:4927–43.
Kopanos C, Tsiolkas V, Kouris A, Chapple CE, Albarca Aguilera M, Meyer R, Massouras A. VarSome: the human genomic variant search engine. Bioinformatics. 2019;35:1978–80.
Kouo T, Chaisawangwong W. SARS-CoV-2 as a superantigen in multisystem inflammatory syndrome in children. J Clin Invest. 2021;131: e149327.
Langmead B, Salzberg SL. Fast gapped-read alignment with Bowtie 2. Nat Methods. 2012;9:357–9.
Lee PY, Day-Lewis M, Henderson LA, Friedman KG, Lo J, Roberts JE, et al. Distinct clinical and immunological features of SARS-CoV-2-induced multisystem inflammatory syndrome in children. J Clin Invest. 2020;130:5942–50.
Lei Y, Guerra Martinez C, Torres-Odio S, Bell SL, Birdwell CE, Bryant JD, et al. Elevated type I interferon responses potentiate metabolic dysfunction, inflammation, and accelerated aging in mtDNA mutator mice. Sci Adv. 2021;7:eabe7548.
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The sequence alignment/map format and SAMtools. Bioinformatics. 2009;25:2078–9.
Lima-Setta F, Magalhães-Barbosa MC, Rodrigues-Santos G, Figueiredo EADN, Jacques ML, Zeitel RS, et al. Multisystem inflammatory syndrome in children (MIS-C) during SARS-CoV-2 pandemic in Brazil: a multicenter, prospective cohort study. J Pediatr. 2021;97:354–61.
Liu W, **e Y, Ma J, Luo X, Nie P, Zuo Z, et al. IBS: an illustrator for the presentation and visualization of biological sequences. Bioinformatics. 2015;31:3359–61.
Marsh RA, Madden L, Kitchen BJ, Mody R, McClimon B, Jordan MB, et al. XIAP deficiency: a unique primary immunodeficiency best classified as X-linked familial hemophagocytic lymphohistiocytosis and not as X-linked lymphoproliferative disease. Blood. 2010;116:1079–82.
Mazer MB, Bulut Y, Brodsky NN, Lam FW, Sturgill JL, Miles SM, et al. Multisystem inflammatory syndrome in children: host immunologic responses. Pediatr Crit Care Med. 2022;23:315–20.
McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GR, Thormann A, et al. The Ensembl variant effect predictor. Genome Biol. 2016;17:122.
Mehta P, Fajgenbaum DC. Is severe COVID-19 a cytokine storm syndrome: a hyperinflammatory debate. Curr Opin Rheumatol. 2021;33:419–30.
Melo RC, Dvorak AM. Lipid body-phagosome interaction in macrophages during infectious diseases: host defense or pathogen survival strategy? PLoS Pathog. 2012;8: e1002729.
Nakra NA, Blumberg DA, Herrera-Guerra A, Lakshminrusimha S. Multi-system inflammatory syndrome in children (MIS-C) following SARS-CoV-2 infection: review of clinical presentation, hypothetical pathogenesis, and proposed management. Children (basel). 2020;7:69.
Noval Rivas M, Porritt RA, Cheng MH, Bahar I, Arditi M. COVID-19-associated multisystem inflammatory syndrome in children (MIS-C): a novel disease that mimics toxic shock syndrome-the superantigen hypothesis. J Allergy Clin Immunol. 2021;147:57–9.
Odobasic D, Kitching AR, Holdsworth SR. Neutrophil-mediated regulation of innate and adaptive immunity: the role of myeloperoxidase. J Immunol Res. 2016;2016:2349817.
Parodi E, Carpino A, Franchitti E, Pruccoli G, Denina M, Pagliero F, et al. Detection of faecal SARS-CoV-2 RNA in a prospective cohort of children with multisystem inflammatory syndrome (MIS-C). Epidemiol Prev. 2021;45:522–7.
Porritt RA, Paschold L, Rivas MN, Cheng MH, Yonker LM, Chandnani H, et al. HLA class I-associated expansion of TRBV11-2 T cells in multisystem inflammatory syndrome in children. J Clin Invest. 2021a;131:e146614.
Porritt RA, Binek A, Paschold L, Rivas MN, McArdle A, Yonker LM, et al. The autoimmune signature of hyperinflammatory multisystem inflammatory syndrome in children. J Clin Invest. 2021b;131:e151520.
Ramaswamy A, Brodsky NN, Sumida TS, Comi M, Asashima H, Hoehn KB, et al. Immune dysregulation and autoreactivity correlate with disease severity in SARS-CoV-2-associated multisystem inflammatory syndrome in children. Immunity. 2021;54:1083-1095.e7.
Reis ES, Mastellos DC, Hajishengallis G, Lambris JD. New insights into the immune functions of complement. Nat Rev Immunol. 2019;19:503–16.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607–8.
Sacco K, Castagnoli R, Vakkilainen S, Liu C, Delmonte OM, Oguz C, et al. Immunopathological signatures in multisystem inflammatory syndrome in children and pediatric COVID-19. Nat Med. 2022;28:1050–62.
Sancho-Shimizu V, Brodin P, Cobat A, Biggs CM, Toubiana J, Lucas CL, et al. SARS-CoV-2-related MIS-C: a key to the viral and genetic causes of Kawasaki disease? J Exp Med. 2021;218: e20210446.
Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–504.
Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, El Burai FS, et al. Coronavirus Disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759–65.
Strzepa A, Pritchard KA, Dittel BN. Myeloperoxidase: a new player in autoimmunity. Cell Immunol. 2017;317:1–8.
Syrimi E, Fennell E, Richter A, Vrljicak P, Stark R, Ott S, et al. The immune landscape of SARS-CoV-2-associated Multisystem Inflammatory Syndrome in Children (MIS-C) from acute disease to recovery. iScience. 2021;24:103215.
Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588:315–20.
Tang S, Wang J, Lee NC, Milone M, Halberg MC, Schmitt ES, et al. Mitochondrial DNA polymerase gamma mutations: an ever expanding molecular and clinical spectrum. J Med Genet. 2011;48:669–81.
Vagrecha A, Zhang M, Acharya S, Lozinsky S, Singer A, Levine C, et al. Hemophagocytic lymphohistiocytosis gene variants in multisystem inflammatory syndrome in children. Biology (basel). 2022;11:417.
Valentini P, Sodero G, Buonsenso D. The relationship between COVID-19 and innate immunity in children: a review. Children (basel). 2021;8:266.
Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, Bonanomi E, D’Antiga L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395:1771–8.
Vianna EQ, Piergiorge RM, Gonçalves AP, Dos Santos JM, Calassara V, Rosenberg C, et al. Understanding the landscape of X-linked variants causing intellectual disability in females through extreme X chromosome inactivation skewing. Mol Neurobiol. 2020;57:3671–84.
Warren RL, Choe G, Freeman DJ, Castellarin M, Munro S, Moore R, Holt RA. Derivation of HLA types from shotgun sequence datasets. Genome Med. 2012;4:95.
Warren RL, Holt RA. Targeted assembly of short sequence reads. PLoS ONE. 2011;6: e19816.
Würzner R, Hobart MJ, Fernie BA, Mewar D, Potter PC, Orren A, Lachmann PJ. Molecular basis of subtotal complement C6 deficiency. A carboxy-terminally truncated but functionally active C6. J Clin Invest. 1995;95:1877–83.
Zhang X, Shephard F, Kim HB, Palmer IR, McHarg S, Fowler GJ, et al. TILRR, a novel IL-1RI co-receptor, potentiates MyD88 recruitment to control Ras-dependent amplification of NF-kappaB. J Biol Chem. 2010;285:7222–32.
Zhang AQ, Liu YX, ** JY, Wang CY, Fan LL, Xu DB. Identification of a novel mutation in the C6 gene of a Han Chinese C6SD child with meningococcal disease. Exp Ther Med. 2021;21:510.
Zhou H, Li J, Su H, Li J, Lydic TA, Young ME, Chen W. BSCL2/Seipin deficiency in hearts causes cardiac energy deficit and dysfunction via inducing excessive lipid catabolism. Clin Transl Med. 2022;12: e736.
Web resources
1000 Genomes, 2022, https://www.internationalgenome.org/
Brazilian genomic variants—AbraOM, 2022, https://abraom.ib.usp.br/
Brazilian Initiative on Precision Medicine—BIPMed, 2022, https://bipmed.org/
ClinVar, 2022, https://www.ncbi.nlm.nih.gov/clinvar/
EnrichR, 2022, https://maayanlab.cloud/Enrichr/
ExAC Browser, 2022, http://exac.broadinstitute.org/
Exome Variant Server—ESP6500, 2022, https://evs.gs.washington.edu/EVS/
Human Base, 2022, https://hb.flatironinstitute.org/
Online Mendelian Inheritance in Man—OMIM, 2022, http://www.omim.org/
Orphanet, 2022, https://www.orpha.net/consor/cgi-bin/index.php
Pfam platform, 2022, http://pfam.sanger.ac.uk/
The Genome Aggregation Database—GnomAD, 2022, https://gnomad.broadinstitute.org/
The Human Protein Atlas, 2022, https://www.proteinatlas.org/
Variant Effect Predictor, Ensembl Genome Browser, 2022, https://www.ensembl.org/info/docs/tools/vep/index.html
Varsome, 2022, https://varsome.com/
WHO, World Health Organization. Multisystem inflammatory syndrome in children and adolescents with COVID-19: Scientific Brief. 2020. https://www.who.int/publications-detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19. Accessed 27 May 27 2022.
Acknowledgements
We thank Dr. Orlando da Costa Ferreira Júnior and Dr Amilcar Tanuri for his advice and critical reading of this manuscript. This work was developed in the frameworks of Corona-ômica-RJ (FAPERJ E-26/210.179/2020 and E-26/211.107/2021). We also acknowledge the support from the Rede Corona-ômica BR MCTI/FINEP affiliated to RedeVírus/MCTI (FINEP 01.20.0029.000462/20, CNPq 404096/2020-4) and BRICS - CNPq (440931/2020-7). C.B.S.R. is supported by CNPq (302263/2019-5) and FAPERJ (E-26/210.179/2020). A.T.R.V. is supported by CNPq (307145/2021-2) and FAPERJ (E-26/201.046/2022). The authors declare that’s the subheadings were also described along the manuscript.
The URLs for data presented herein are given in web resources.
Funding
This work was developed in the frameworks of Corona-ômica-RJ (FAPERJ E-26/210.179/2020 and E-26/211.107/2021). It was also supported by the Rede Corona-ômica BR MCTI/FINEP affiliated to RedeVírus/MCTI (FINEP 01.20.0029.000462/20, CNPq 404096/2020-4) and BRICS - CNPq (440931/2020-7). C.B.S.R. is supported by CNPq (302263/2019-5) and FAPERJ (E-26/210.179/2020). A.T.R.V. is supported by CNPq (307145/2021-2) and FAPERJ (E-26/201.046/2022).
Author information
Authors and Affiliations
Contributions
Conception and design: CBSR, CCC, ATRV. Clinical evaluation: RSZ, RMS, ARF, MCFR, ATAMS. Acquisition of data: ALG, APCG, RCS, ADR, LCMSP. Analysis and interpretation: CBSR, CCC, RMP, CSF. Manuscript drafting: CBSR, CCC, RMP, CSF, ATRV. Obtained funding: CBSR, CCC, ATRV. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Ethics Committees approved the research protocols (CAAE 0135320.0.0000.5259 and 33040420.3.0000.5264) and written informed consent was obtained from the participants and their parents.
Consent for publication
Not applicable. There are no patients’ images and all individuals were anonymized by code numbers.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Genes in which sequence variants or abnormal mRNA expression were previously associated with MIS-C (Lee et al. 2020; Chou et al. 2021; Beckmann et al. 2021; Abolhassani et al. 2022; Vagrecha et al. 2022) and genes for which genome-wide studies found association with Kawasaki disease (Sancho-Shimizu et al. 2021).
Additional file 2: Table S2.
Overview of WES data quality.
Additional file 3: Table S3.
Sequencing metrics to support the call quality of each potentially causative variant.
Additional file 4: Table S4.
Additional very rare variants (MAF < 0.01) found in MIS-C patients. No relevant variants were found in patient EXOC17.
Additional file 5: Table S5.
Prediction of class I and II HLA alleles from WES data.
Additional file 6: Table S6.
Previous host genetic variants described in patients with MIS-C by whole exome sequencing or immune-gene-panel.
Additional file 7: Figure S1.
Workflow of the methodology used. Figure S2. Electropherograms obtained by Sanger sequencing, confirming the WES results. Figure S3. Location of the potentially causative variants in the canonical protein forms obtained from the UniProt Platform. The proteins, proportional to size, the positions of the mutations (lollipops), and the coordinates of the domains annotated in Pfam are represented. Variants identified in FREM1, C6, C9, ABCC6, and BSCL2 are contained in the functional domains of their proteins, whereas for the ABCA4 variant, two variants are outside functional domains and one is within it. For POLG, the variant is located outside functional domains. MPO variant was not illustrated, since it is intronic. Figure S4. Highly reliable protein–protein interactions network retrieved from the products of the eight genes studied. The red hexagons represent the genes carrying the variants. The circles represent the interactions obtained through the STRING plugin, with the green circles representing genes already related to the MIS-C phenotype and blue circles representing genes already related to Kawasaki disease. Figure S5. Enrichment analysis through EnrichR tool of the proteins verified in the PPIs network (FDR < 0.05) against the following gene-set libraries: KEGG 2021 (a); Gene Ontology 2021—biological processes (b), molecular function (c), and cellular component (d); Jensen tissues (e); the scRNA-seq database PanglaoDB Augmented 2021 (f); COVID-19-related gene sets 2021 (g). Top ten elements were sorted by adjusted p-value ranking.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Santos-Rebouças, C.B., Piergiorge, R.M., dos Santos Ferreira, C. et al. Host genetic susceptibility underlying SARS-CoV-2-associated Multisystem Inflammatory Syndrome in Brazilian Children. Mol Med 28, 153 (2022). https://doi.org/10.1186/s10020-022-00583-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10020-022-00583-5