Abstract
Vaccination with inactivated SARS-CoV-2 virus produces suboptimal immune responses among kidney transplant (KT), peritoneal dialyzed (PD), and hemodialyzed (HD) patients. Participants were vaccinated with two-dose inactivated SARS-CoV-2 vaccine (V2) and a third dose of ChAdOx1 nCoV-19 vaccine (V3) at 1–2 months after V2. We enrolled 106 participants: 31 KT, 28 PD, and 31 HD patients and 16 controls. Among KT, PD, and HD groups, median (IQR) of anti-receptor binding domain antibody levels were 1.0 (0.4–26.8), 1092.5 (606.9–1927.2), and 1740.9 (1106–3762.3) BAU/mL, and percent neutralization was 0.9 (0–9.9), 98.8 (95.9–99.5), and 99.4 (98.8–99.7), respectively, at two weeks after V3. Both parameters were significantly increased from V2 across all groups (p < 0.05). Seroconversion and neutralization positivity rates in PD, HD, and control groups were 100% but were impaired in KT patients (39% and 16%, respectively). S1-specific T-cell counts were increased in PD and HD groups (p < 0.05) but not in KT patients. The positive S1-specific T-cell responder rate was > 90% in PD, HD, and control groups, which was higher than that in KT recipients (74%, p < 0.05). The heterologous inactivated virus/ChAdOx1 nCoV-19 vaccination strategy elicited greater immunogenicity among dialysis patients; however, inadequate responses remained among KT recipients (TCTR20210226002).
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease that has caused a worldwide pandemic. Clinical presentation ranges from asymptomatic or mild upper respiratory tract disease to pneumonia and respiratory failure1. Patients who have comorbidities or are taking immunosuppressive drugs are likely to develop severe disease and complications2. Patients with end-stage kidney disease (ESKD) requiring dialysis often have compromised humoral immunity (HMI) because of uremic toxins, inflammation, and malnutrition. Furthermore, kidney transplant (KT) recipients have impaired cell-mediated immunity (CMI) from taking immunosuppressants to maintain their allografts3,4. Therefore, a preventive strategy is recommended to prepare for potentially aggressive disease. Immunogenicity of vaccine platforms and individual immune status are variable5. When whole, inactivated SARS-CoV-2 virus was utilized as a vaccine nationwide, optimal immune responses were observed among immunocompetent individuals6. However, the CVIM1 and ICON1 studies were prospective studies that investigated SARS-CoV-2-specific HMI and CMI responses after vaccination with two doses of inactivated SARS-CoV-2 vaccine in KT and ESKD patients who underwent hemodialysis (HD) and peritoneal dialysis (PD), respectively. SARS-CoV-2-specific HMI responses were suboptimal in dialysis patients and substantially impaired in KT patients compared with the CMI response7,8.
The WHO released interim recommendations for a third COVID-19 vaccine dose for immunocompromised individuals9. Investigations of third doses have primarily used homologous vaccine platforms and evaluated mRNA- and adenoviral vector-based vaccines. A heterologous vaccine platform with two doses of inactivated SARS-CoV-2 vaccine and a third dose of ChAdOx1 nCoV-19 vaccine was proposed to enhance immune responsiveness among immunocompromised populations such as patients receiving active treatment for hematologic malignancies or patients with advanced HIV infection. However, the immunogenicity and safety studies among KT and dialysis patients vaccinated with the third dose of ChAdOx1 nCoV-19 vaccine have recently received attention. Thus, we evaluated the immunogenicity and safety profiles of this new vaccination regimen among these vulnerable individuals.
Materials and methods
Study design
A single-arm clinical trial (CVIM2/ICON2 study) was performed between July 2021 and September 2021 at Ramathibodi Hospital, Mahidol University, Bangkok, Thailand. Participants who were vaccinated with two doses (V2) of the inactivated SARS-CoV-2 (CoronaVac, 3 μg of inactivated whole-virus SARS-CoV-2 in 0.5 ml) vaccine (Sinovac Biotech Ltd., China), were offered a third dose (V3) of the ChAdOx1 nCoV-19 (AZD1222, ChAdOx1-S of at least 2.5 × 108 infectious units in 0.5 ml) vaccine (Oxford University-AstraZeneca) at 1 to 2 months after V2 (Supplementary Fig. 1). We assessed both HMI and CMI responses and monitored for adverse events (AEs) following the third dose of the ChAdOx1 nCoV-19 vaccine.
The Institutional Review Board of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, approved the study protocol (approval number: MURA2021/523). The study was conducted following the principles laid out in the Declaration of Helsinki and was registered with the Thai Clinical Trials Registry (TCTR202110524002). All participants provided written informed consent. The approval from the Faculty of Medicine Ramathibodi Hospital was applied with acknowledgment of the medical director of Banphaeo General Hospital (Charoenkrung branch) due to unavailability of the local ethic committee of this facility. Furthermore, the patients from Banphaeo General Hospital (Charoenkrung branch) agreed to the participation, the referral, and providing information about their medical condition.
The eligibility criterion for participation (Supplementary Fig. 5) was adults aged 18 to 59 years old. Those with suspected respiratory tract infections within the past three days, ongoing infections, and previous history of COVID-19 were excluded. Screening questions were used to assess concurrent respiratory tract infection and potential exposure to COVID-19. Nasopharyngeal and oropharyngeal swabs were not collected for SARS-CoV-2 reverse transcription polymerase chain reaction (RT-PCR) tests before vaccination. Dialysis patients were those who were stable on their dialysis prescriptions for at least one month. KT recipients were at least 1-month post-transplant with stable allograft function and immunosuppressive regimens and without recent allograft rejections or intensive immunosuppressant therapy. Intense immunosuppressant regimens included methylprednisolone pulse therapy (500 mg/day for three days), antithymocyte globulin therapy, rituximab therapy within six months, or ≥ 15 mg/day prednisolone. A low C0 trough level of calcineurin inhibitor (CNI) was defined as ≤ 5 ng/mL tacrolimus or ≤ 150 ng/mL cyclosporine10. A low dose of mycophenolic acid (MPA) was defined as ≤ 1 g/day mycophenolate mofetil (MMF) or ≤ 720 mg/day mycophenolate sodium (MPS)11.
HMI and CMI responses were assessed two weeks after V2 and V3. HMI was measured using a SARS-CoV-2 immunoglobulin G (IgG) assay, which tests for antibodies against the S1 receptor-binding domain (RBD) of the SARS-CoV-2 spike protein, and SARS-CoV-2 surrogate virus neutralization test (sVNT). CMI was measured using an enzyme-linked immunospot assay for interferon-γ (IFN-γ).
SARS-CoV-2 anti-RBD IgG assay
SARS-CoV-2 anti-RBD IgG antibodies were measured using the Abbott SARS-CoV-2 IgG II Quantification assay (Abbott Diagnostics, USA). Plasma samples were run on the Abbott Alinity instrument following the manufacturer’s instructions. The assay is a chemiluminescent microparticle immunoassay for the quantitative detection of IgG against the RBD of the SARS-CoV-2 spike protein in human serum. The sequence of the RBD was derived from the WH-Human 1 coronavirus. The quantitative results for anti-RBD IgG were reported in binding antibody units (BAU)/mL. A cut-off value of ≥ 7.1 BAU/mL was considered seroconversion12. This value provided a diagnostic sensitivity and specificity of 91.6% and 99.4%, respectively12,13.
SARS-CoV-2 sVNT
The function of anti-SARS-CoV-2 S1/RBD antibodies was determined using a SARS-CoV-2 NeutraLISA surrogate neutralization assay (Euroimmun, Germany). The neutralizing antibodies in plasma inhibit binding between the RBD and angiotensin-converting enzyme 2 receptor. The sequence of the RBD was also derived from the WH-Human 1 coronavirus. The neutralizing antibody was measured and reported as a percentage; those participants with > 35% inhibition were considered positive14. This value provided a sensitivity and specificity of 95.9% and 99.7%, respectively15.
SARS-CoV-2 ELISpot assay
SARS-CoV-2–specific CMI responses were measured using the SARS-CoV-2 ELISpot assay as previously described7. The SARS-CoV-2 S1 scanning peptide pool (Mabtech, Inc.) and the SARS-CoV-2 spike protein, nucleoprotein, membrane protein, open reading frame (ORF)-3a, and ORF-7a proteins (SNMO) peptide pool (Mabtech, Inc.) were derived from the WH-Human 1 coronavirus and used as stimulants. Anti-CD3 antibody was a positive control. Results were reported as IFN-γ-producing spot forming units (SFUs) per 106 peripheral blood mononuclear cells (PBMCs) for each peptide pool16. Participants with ≥ 6 SFUs/106 PBMCs were considered responders17,18.
Adverse events
All participants were monitored for solicited AEs within 30 min after vaccination (Supplementary Fig. 2) and on days 3 and 7 by telephone (Supplementary Fig. 3). In addition, unsolicited AEs were documented by participants in the provided diaries (Supplementary Fig. 4). The occurrence of adverse events following vaccination was collected and compared.
Statistical analyses
Categorical and continuous variables were reported as absolute numbers, frequencies, or medians with interquartile range (IQR). The chi-square test and Fisher’s exact test were performed to compare categorical variables as appropriate. The Mann–Whitney U test and Wilcoxon signed-rank test were performed to compare continuous variables between and within the groups, respectively. Analysis of variance was used to compare variables across all groups. Statistical analyses were performed with Stata statistical software, version 15 (StataCorp, LLC; College Station, TX, USA). P values < 0.05 were considered significant. The prevalence of anti-RBD IgG, percent neutralization, and S1- or SNMO-specific T-cell SFUs/106 PBMCs were presented as dot plots or bar graphs generated with GraphPad Prism 6.0 (GraphPad Software, Inc.; San Diego, CA, USA).
Results
Clinical characteristics of participants
We enrolled 106 participants (Supplementary Fig. 6): 31 KT, 28 PD, and 31 HD patients and 16 healthy controls. Clinical characteristics of all participants are presented in Table 1. Age; sex; Charlson comorbidity index; comorbidities; absolute lymphocyte counts; and blood levels of albumin, calcium, and phosphorus were variable across all groups (p < 0.05). KT recipients were slightly older and received immunosuppressants. Two KT recipients (6.5%) received the ChAdOx1 nCoV-19 vaccine within the first year after transplant.
SARS-CoV-2 specific HMI responses
At two weeks after V3, the median anti-RBD antibody levels among KT, PD, HD, and controls were greater after V3 in all groups compared with those after V2 (p < 0.05) (Table 2, Fig. 1a,b). Anti- RBD antibody levels after V3 in HD patients were comparable with controls but significantly impaired in PD (p < 0.05) and KT (p < 0.05) patients. The seroconversion rates were 39% for KT patients and 100% for PD, HD, and control groups. For ESKD patients receiving dialysis, the seroconversion rate improved from 88% after V2 to 100% after V3 (p < 0.01). Among KT patients, the seroconversion rate increased significantly from 10% after V2 to 39% after V3 (p < 0.01).
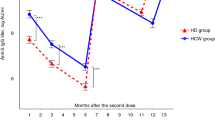
Humoral and cell-mediated immune responses in kidney transplant (KT), peritoneal dialyzed (PD), and hemodialyzed (HD) patients and healthy individuals (controls) who received two doses of inactivated vaccine (V2) compared with those receiving a third dose of ChAdOx1 nCoV-19 vaccine (V3). (a) Anti-receptor-binding domain (RBD) antibody levels at two weeks after V2 and V3 are presented in log10 binding antibody units (BAU)/mL using scatter dot plots. Each dot represents an individual participant, and horizontal lines indicate the median and interquartile range. The dotted line indicates the threshold value of 7.1 BAU/mL. (n = 106) (b) Anti-RBD antibody levels at two weeks after V2 and V3 within individuals are shown. (n = 106) (c) The percent neutralization inhibition at two weeks after V2 and V3 are presented. The dotted line indicates the 35% threshold for neutralization positivity. (n = 106) (d) SARS-CoV-2–specific, IFN-γ-producing T-cell responses to the S1 protein at two weeks after V2 and V3 are presented in the scatter dot plots. (n = 106) Horizontal lines indicate the median and interquartile range. The dotted line indicates the threshold value of 6 SFUs/106 PBMCs. *P-value < 0.05. IFN-γ, interferon-γ; SFU, spot forming unit; NS, non-significant; PBMCs, peripheral blood mononuclear cells; S, spike glycoprotein; S1, S1 domain of spike protein.
The median % inhibition by neutralizing antibodies among the KT, PD, HD, and control, as measured by the neutralization (NT) test was greater at two weeks after V3 than two weeks after V2 in all groups (p < 0.05) (Table 2, Fig. 1c). The % NT in the PD, HD, and control groups was comparable but significantly lower in KT patients (p < 0.05). The rate of NT positivity was 100% in PD, HD, and control groups and 16% in the KT group. After V3, the seropositivity rate for neutralizing antibodies increased in ESKD patients (58% for V2 vs. 100% for V3, p < 0.01); all twenty-four ESKD patients with % NT below 35 after V2 became seropositive after V3. Similarly, KT recipients achieved a higher seropositive rate after V3 (16%) compared with 0% after V2 (p = 0.05).
The seroconversion rate for anti-RBD antibodies was higher in KT recipients who were maintained on a low therapeutic dose of MPA or MPA-sparing regimen compared with those who were maintained on a high mycophenolic acid dose (75% vs. 16%; odds ratio [OR], 10.7; 95% confidence interval [CI], 1.9–59.6; p < 0.01) (Supplementary Table 1). This association was significant for KT recipients who were NT positive (100% vs. 31%; OR, 23.9; 95% CI, 1.2–484.2; p < 0.05). Time after transplant, age < 50 years, lymphopenia (< 1.5 × 103/μL), and low C0 level for CNI or CNI-sparing regimen were not significantly different between KT recipients with and without seroconversion and NT positivity.
SARS-CoV-2 specific CMI responses
The median SFUs for S1-specific T-cell responses were significantly increased after V3 in PD and HD patients (242 [71–473] and 188 [32–480] T-cells/106 PBMCs, respectively; p < 0.05) compared with those after V2. However, SFUs after V2 and V3 were not significantly different in the KT and control groups (p > 0.05) (Fig. 1d). The rates of S1-specific T-cell responders were 58%, 96%, 90%, 100% in KT, PD, HD, and controls, respectively.
After V3, the median SFUs for SNMO-specific T cell responses were significantly increased in HD patients compared with those after V2 (p < 0.05) but were not significantly different in the KT, PD, and control groups (12 [0–60], 240 [56–467], and 70 [16–184] T-cells/106 PBMCs, p > 0.05). The rates of SNMO-specific T cell responders were 74%, 96%, 90%, and 100% in the KT, PD, HD, and control groups, respectively, after V3. The responder rate in the control group was higher than that in the KT group (p < 0.05).
No significant differences were observed for low therapeutic doses of mycophenolic acid or mycophenolic acid-sparing regimen, time after transplant, age < 50 years, lymphopenia (< 1.5 × 103/μL), low C0 level of calcineurin inhibitors, or CNI-sparing regimen between KT recipients with and without S1-specific T-cell responses.
Adverse events
There were no serious local or systemic AEs within 30 min after V3. Solicited AEs within 3 and 7 days after V3 are presented and compared with those after V27,8 in Fig. 2 and Supplementary Table 2. AEs were reported in the KT (82%), PD (96%), HD (97%), and control (100%) groups within 3 days after V3. The numbers of AEs were significantly greater after V3 compared with those after V2 across all groups (p < 0.05). The most common AEs included pain at the injection site (9–39%), muscle aches (9–32%), fever (3–19%), and sleepiness (0–6%). On day 7, the AEs were almost entirely resolved. All AEs were graded as mild. No acute rejection episodes occurred in vaccinated KT recipients. No unsolicited AEs were reported.
Discussion
This study evaluated immune responses in dialysis and KT patients following a third dose of ChAdOx1 nCoV-19 vaccine, administered 4–8-weeks after two doses of an inactivated SARS-CoV-2 vaccine. This regimen induced robust SARS-CoV-2–specific HMI responses, as determined by measuring the levels of anti-RBD IgG and % NT, and achieved the same rate of seroconversion and NT positivity among ESKD patients as immunocompetent individuals. Although the magnitude of HMI and response rates were improved with this heterologous vaccination strategy, HMI remained suboptimal in KT recipients. A similar result was observed for SARS-CoV-2-specific CMI, which was assessed by IFN-γ ELISpot responses against SARS-CoV-2 S1 protein. Furthermore, most patients only experienced mild and spontaneously resolved AEs with this new vaccine strategy.
Few studies have reported HMI responses after three doses of COVID-19 vaccine among ESKD patients, and these studies focused on the same vaccine platform19,20,21,22. We demonstrated that the addition of ChAdOx1 nCoV-19 vaccines enabled ESKD patients to produce remarkably higher antibody levels which could potentially act against the variants. This heterologous inactivated virus/ChAdOx1 nCoV-19 vaccination regimen generated an excellent level of seroconversion in non-responders after V2, which was comparable to the efficacy of three doses of the BNT162b2 mRNA vaccine19,20,21,22. The magnitude of anti-RBD antibody production and the % NT in ESKD patients were comparable to the control group. However, there was a lower trend of production in the PD subgroup. This relationship was observed for NT positivity and T-cell immune responses. A significant proportion of T-cell responders (> 90%) were observed in the PD, HD, and control groups. The inactivated virus/ChAdOx1 nCoV-19 vaccination regimen enhanced the % NT in all dialysis patients who had previously produced a % NT below the cut-off level, and these patients became seropositive after the additional dose. Furthermore, the addition of the ChAdOx1 nCoV-19 vaccine after inactivated vaccine improved the % NT in ESKD patients to a level comparable to that of healthy controls. This effect concurs with the efficacy of two doses of BNT162b2 reported by Carr et al.23. Although direct comparisons between studies are limited due to different assays, timepoints and patient populations, the rate of NT seropositivity with the inactivated virus/ChAdOx1 nCoV-19 regimen was equal to or higher than that observed for two doses of the BNT162b2 vaccine23,24. Feng et al. reported that the anti-RBD antibody levels above 506 BAU/mL correlated with 80% vaccine efficacy against symptomatic COVID-19 infection from the Alpha (B.1.1.7) variant. Although we could potentially use this cut-off value to extrapolate the efficacy of new vaccine regimens, variability of ongoing spreading variant and individual immune status could limit interpretation. Nevertheless, most participants could achieve anti-RBD antibody levels more remarkable than this number, excluding KT recipients25. Thus, ESKD patients who received a two-dose regimen of inactivated vaccine may benefit from this heterologous combination.
Among several COVID-19 vaccines available, a third dose of an mRNA-based vaccine appeared to substantially improve the prevalence of anti–SARS-CoV-2 antibodies from 40 to 68% after a regular 2-dose course in solid organ transplant (SOT) recipients26,27,28,29. KT recipients who received an adenovirus-vectored vaccine revealed a significantly impaired immune response rate of 44% after a full course30. Data regarding an additional dose after an entire course of the adenovirus-vectored vaccine in SOT recipients remains limited. Among KT recipients in this study, the seroconversion rate after the heterologous vaccine regimen was 39% compared with 49% and 26% in KT recipients fully vaccinated with mRNA-1273 and BNT162b2, respectively30. Although no threshold has been established for protective immunity, antibody levels and their neutralization properties were lower in KT transplant recipients than in the control group who received the same vaccine regimen. Two doses of inactivated vaccine resulted in low immune responses among KT recipients as has been previously reported7,31. A supplemental dose of the adenovirus-vectored vaccine in these immunosuppressed patients successfully increased the seroconversion rate from 10% to approximately 40% and NT positivity in up to one out of six patients, which has not been reported. Therefore, our study supported the WHO interim recommendation for an additional vaccine in patients who are immunocompromised9. We propose that the accumulation of data after switching between vaccine platforms may be valuable for designing optimal vaccine regimens for patients with comorbidities and those receiving immunosuppressants.
Since measurement of cell-mediated immune response may not be widely available due to lacking the commercialized assay, we explored whether the association between vaccine-elicited humoral and cellular immune response exists in all participants, using Spearman’s correlation analysis. There was a weak positive correlation (r = 0.23, p = 0.02) between the anti-RBD antibody levels and the S1-specific T-cell responses after the second dose of inactivated SARS-CoV-2 vaccine and a moderate positive correlation (r = 0.39, p < 0.001) between those two parameters after the additional dose of ChAdOx1 nCoV-19 vaccine (Supplementary Fig. 7).
Several factors may lead to a failure in seroconversion after vaccination in transplant recipients, including higher numbers of immunosuppressive drugs29 and a dose of mycophenolate mofetil > 1 g/day7,32. In our study, KT patients with HMI responses received ≤ 1 g/day MMF, ≤ 720 mg/day MPS, or were on a treatment regimen without MPA, which reaffirmed the impact of MPA on seroconversion observed in a previous study6. Although immunosuppressive agents may have significantly blunted HMI in our KT patients, this effect was not demonstrated for CMI. A similar phenomenon was observed after a single dose of BNT162b2 in KT recipients11. A recommendation for withholding MPA after COVID vaccination exists for patients with autoimmune diseases33, and a strategy regarding MPA dose reduction among SOT recipients is undergoing investigation34.
The present study evaluated AEs after this new heterologous vaccine regimen in immunocompromised individuals. This specific vaccination strategy appeared to be tolerable and relatively safe. Although a substantial proportion of our participants experienced at least one AE after an additional dose of vaccine, the AEs were graded as non-severe. Pain at the injection site was frequently reported after the ChAdOx1 nCoV-19 vaccination in a phase 3 trial35.
Our study had limitations, including a relatively small number of patients and unmatched controls36. The sVNT is a surrogate test for neutralizing antibodies, which is not as standardized as the plaque reduction neutralization test, and the assumption of protective immunity against infection from this vaccine regimen cannot be concluded. Moreover, immune escape from vaccine-elicited immunity by the variant of concerns in circulation has been reported37. Studies using the live virus-based neutralization assay against variants of concerns are required to inform vaccine efficacy36. Additionally, the effectiveness may be variable based on local virus transmission rates and different COVID-19 variants. Furthermore, a direct comparison of immunogenicity may not be possible because of different vaccine platforms, variable definitions of immune responses, and intra- and inter-individual differences. Therefore, clinicians should interpret and apply these pieces of information with caution. Lastly, since we only screened SARS-CoV-2 infection by medical history, there is a possibility that our participants had been infected before receiving a third ChAdOx1 nCoV-19 dose. However, our findings provide additional information on SARS-CoV-2–specific immune responses following this unique regimen and the potential utilization of this strategy when mRNA-based vaccines are inaccessible. Our study assessed CMI, which is believed to boost a prolonged protective memory response, especially T-cell-dependent B-cell activation, which should be further explored24. Furthermore, although information regarding short-term AEs was collected, long-term safety and potential indirect AEs warrant further studies.
With acceptable short-term AEs, the heterologous 3-dose SARS-CoV-2 vaccination regimen elicited greater immunogenicity among dialyzed patients; however, inadequate responses remained in the KT recipients. Therefore, we conclude that an additional vaccine dose should be considered to a primary series to produce greater immune responsiveness among ESKD and KT patients, who remain vulnerable to COVID-19-related disease and mortality.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available because of privacy and ethical restrictions, but anonymized data are available from the corresponding author on reasonable request.
References
Bruminhent, J., Ruangsubvilai, N., Nabhindhakara, J., Ingsathit, A. & Kiertiburanakul, S. Clinical characteristics and risk factors for coronavirus disease 2019 (COVID-19) among patients under investigation in Thailand. PLoS ONE 15, e0239250 (2020).
Fung, M. & Babik, J. M. COVID-19 in immunocompromised hosts: What we know so far. Clin. Infect. Dis. 72, 340–350 (2021).
Sakulkonkij, P., Bruminhent, J., Pankongngam, C. & Chalermphunchai, N. A family cluster of diagnosed coronavirus disease 2019 (COVID-19) kidney transplant recipient in Thailand. Immun. Inflamm. Dis. 8, 534–543 (2020).
Thammathiwat, T. et al. A case of successful treatment of severe COVID-19 pneumonia with favipiravir and tocilizumab in post-kidney transplant recipient. Transpl Infect. Dis. 23, e13388 (2021).
Khan, W. H. et al. COVID-19 pandemic and vaccines update on challenges and resolutions. Front. Cell. Infect. Microbiol. 11, 690621 (2021).
Jantarabenjakul, W., Chantasrisawad, N., Puthanakit, T., et al. Short-term immune response after inactivated SARS-CoV-2 (CoronaVac, Sinovac) and ChAdOx1 nCoV-19 (Vaxzevria, Oxford-AstraZeneca) vaccinations in health care workers. Asian Pacific J. Allergy Immunol. (2021).
Bruminhent, J., Setthaudom, C., Chaumdee, P., et al. SARS-CoV-2-specific humoral and cell-mediated immune responses after immunization with inactivated COVID-19 vaccine in kidney transplant recipients (CVIM 1 Study). Am. J. Transpl. (2021).
Boongird, S. et al. Short-term immunogenicity profiles and predictors for suboptimal immune responses in patients with end-stage kidney disease immunized with inactivated SARS-CoV-2 vaccine. Infect. Dis. Ther. 3, 1–15 (2021).
World Health Organization. Interim recommendations for an extended primary series with an additional vaccine dose for COVID-19 vaccination in immunocompromised persons 2021 (accessed 26 October 2021); https://apps.who.int/iris/bitstream/handle/10665/347079/WHO-2019-nCoV-Vaccination-SAGE-recommendation-Immunocompromised-persons-2021.1-eng.pdf?sequence=2
Schiff, J., Cole, E. & Cantarovich, M. Therapeutic monitoring of calcineurin inhibitors for the nephrologist. Clin. J. Am. Soc. Nephrol. 2, 374–384 (2007).
Azzi, Y. et al. Risk factors associated with poor response to COVID-19 vaccination in kidney transplant recipients. Kidney Int. 100, 1127–1128 (2021).
Chew, K. L. et al. Clinical evaluation of serological IgG antibody response on the Abbott Architect for established SARS-CoV-2 infection. Clin. Microbiol. Infect. 26(1256), e9-1256.e11 (2020).
Abbott Core Laboratory. Abbott Alinity i SARS-CoV-2 IgG II Quant Reagent Instructions for Use (accessed 2 November 2021); https://www.corelaboratory.abbott/int/en/offerings/segments/infectious-disease/sars-cov-2
Available at: https://www.coronavirus-diagnostics.com/documents/Indications/Infections/Coronavirus/EI_2606_D_UK_F.pdf
Coronavirus diagnostics by Euroimmun. SARS-CoV-2 NeutraLISA (accessed 2 November 2021); https://www.coronavirus-diagnostics.com/documents/Indications/Infections/Coronavirus/EI_2606_D_UK_F.pdf (2021).
Zuo, J. et al. Robust SARS-CoV-2-specific T cell immunity is maintained at 6 months following primary infection. Nat. Immunol. 22, 620–626 (2021).
Package insert. T-SPOT. COVID. Available at: https://www.tspotcovid.com/wp-content/uploads/sites/5/2021/03/PI-T-SPOT.COVID-IVD-UK-v3.pdf
Schwarzkopf, S. et al. Cellular immunity in COVID-19 convalescents with PCR-confirmed infection but with undetectable SARS-CoV-2-specific IgG. Emerg. Infect. Dis. 27, 122 (2021).
Frantzen, L. et al. COVID-19 vaccination in haemodialysis patients: Good things come in threes. Nephrol. Dial. Transplant. 36, 1947–1949 (2021).
Bensouna, I. et al. SARS-CoV-2 antibody response after a third dose of the BNT162b2 vaccine in patients receiving maintenance hemodialysis or peritoneal dialysis. Am. J. Kidney Dis. 79, 185–192 (2021).
Ducloux, D., Colladant, M., Chabannes, M., Yannaraki, M. & Courivaud, C. Humoral response after 3 doses of the BNT162b2 mRNA COVID-19 vaccine in patients on hemodialysis. Kidney Int. 100, 702–704 (2021).
Dekervel, M. et al. Humoral response to a third injection of BNT162b2 vaccine in patients on maintenance haemodialysis. Clin. Kidney J. 14, 2349–2355 (2021).
Carr, E. J. et al. Neutralising antibodies after COVID-19 vaccination in UK haemodialysis patients. Lancet 398, 1038–1041 (2021).
Speer, C. et al. Longitudinal humoral responses after COVID-19 vaccination in peritoneal and hemodialysis patients over twelve weeks. Vaccines 9, 1130 (2021).
Feng, S. et al. Correlates of protection against symptomatic and asymptomatic SARS-CoV-2 infection. Nat. Med. 27(11), 2032–2040 (2021).
Marion, O. et al. Safety and immunogenicity of anti-SARS-CoV-2 messenger RNA vaccines in recipients of solid organ transplants. Ann. Intern. Med. 174, 1336–1338 (2021).
Boyarsky, B. J. et al. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. JAMA 325, 2204–2206 (2021).
Boyarsky, B. J. et al. Immunogenicity of a single dose of SARS-CoV-2 messenger RNA vaccine in solid organ transplant recipients. JAMA 325, 1784–1786 (2021).
Kamar, N. et al. Three doses of an mRNA Covid-19 vaccine in solid-organ transplant recipients. N. Engl. J. Med. 385, 661–662 (2021).
Prendecki, M. et al. Immunological responses to SARS-CoV-2 vaccines in kidney transplant recipients. Lancet 398, 1482–1484 (2021).
Eren Sadioğlu, R. et al. Antibody response to two doses of inactivated SARS-CoV-2 vaccine (CoronaVac) in kidney transplant recipients. Transpl. Infect. Dis. 23, e13740 (2021).
Kantauskaite, M. et al. Intensity of mycophenolate mofetil treatment is associated with an impaired immune response to SARS-CoV-2 vaccination in kidney transplant recipients. Am. J. Transpl. 22, 634–639 (2021).
American College of Rheumatology. COVID-19 vaccine clinical guidance summary for patients with rheumatic and musculoskeletal diseases developed by the ACR COVID-19 Vaccine Clinical Guidance Task Force (accessed 2 November 2021); https://www.rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf
Caillard, S. & Thaunat, O. COVID-19 vaccination in kidney transplant recipients. Nat. Rev. Nephrol. 17, 1–3 (2021).
Ramasamy, M. N. et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): A single-blind, randomised, controlled, phase 2/3 trial. Lancet 396, 1979–1993 (2021).
Khoury, D. S. et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 27, 1205–1211 (2021).
Zhou, D. et al. Evidence of escape of SARS-CoV-2 variant B.1.351 from natural and vaccine-induced sera. Cell 184(9), 2348-2361.e6 (2021).
Acknowledgements
We offer our gratitude to Pongsan Chatsangjaroen and Parnwas Pinnobphun, MS, for their laboratory support. We are also grateful for infectious diseases nurses and supportive staff at the Division of Infectious Diseases, Division of Nephrology, Department of Medicine, and Clinical Research Center, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
Funding
This work was supported by a grant from the National Research Council of Thailand (102912) and the Ramathibodi Foundation, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand (31010055).
Author information
Authors and Affiliations
Contributions
J.B., S.K., K.M., S.B. participated in conceptualization (create ideas and overarching research goals) and methodology. J.B., C.S., R.K., A.P., P.C., C.J., S.T., S.B. gathered data, J.B., S.B. analyzed data, J.B., S. K., M.A., A.N., S.B. drafted manuscript. All authors read and approved a final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bruminhent, J., Setthaudom, C., Kitpermkiat, R. et al. Immunogenicity of ChAdOx1 nCoV-19 vaccine after a two-dose inactivated SARS-CoV-2 vaccination of dialysis patients and kidney transplant recipients. Sci Rep 12, 3587 (2022). https://doi.org/10.1038/s41598-022-07574-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07574-w
- Springer Nature Limited