Abstract
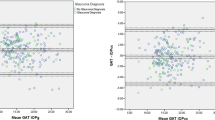
This study assesses the agreement between intraocular pressure (IOP) measurements taken with the Goldmann applanation tonometer (GAT) and a new experimental applanation tonometer with a convexly shaped apex (CT) after laser myopic refractive surgery. Two different CT radii (CT1 and CT2) were designed with a finite element analyser, and a prospective double masked study on 102 eyes from 102 patients was carried out. A Bland-Altman plot and intra-class correlation coefficient (ICC) were calculated to assess the agreement between GAT measurements and the measurements of both CT1 and CT2 before and after myopic laser assisted in situ keratomileusis (LASIK; n = 73) and photorefractive keratectomy (PRK; n = 29). We evaluated a subset of two subgroups (n = 36 each) for intra and inter-observer (IA/IE) error. From the whole cohort, the best IOP agreement was observed between GATpre and CT1post surgery: 16.09 ± 2.92 vs 16.42 ± 2.87 (p < 0.001); ICC = 0.675 (95% CI: 0.554–0.768). In the analysis of LASIK vs PRK, GATpre and CT1post showed the highest agreement, although LASIK measurements were more accurate than PRK, as the ICC = 0.718 (95% CI: 0.594–0.812) and ICC = 0.578 (95% CI: 0.182–0.795) respectively. Excellent agreement was observed for IA/IE, and there was an ICC > 0.8 (95% CI) in all cases. CT1 proved more accurate in the LASIK subgroup. In conclusion, our new version of GAT could be used with post-surgery LASIK patients as a more accurate measurement device compared to the current reference tonometer.
Similar content being viewed by others
Introduction
The Goldmann applanation tonometer (GAT; Haag-Streit, Switzerland) is the current reference tonometer for measuring intraocular pressure (IOP) in daily clinical practice due to its acceptably accurate measurements, reproducibility and reliability1,2,3,4. However, GAT readings are influenced by corneal central thickness (CCT) and corneal biomechanics (CB), which vary widely among normal individuals1,5,6. In myopic laser refractive surgery (LRS) patients, variations induced in both CCT and CB lead to differences in GAT readings. This change in IOP has been inconsistent in previous studies regardless of the type of surgery: Mardelli et al.7 found a significant reduction of 1 ± 2.8 mmHg in IOP measurements after ablating 23 μm in photorefractive keratectomy (PRK) patients; while Duch et al.8 found an underestimation of about 2.9 mmHg per 70 μm ablation in CCT after laser assisted in situ keratomileusis (LASIK). These IOP underestimations affect the reliability of GAT as gold standard after LASIK and PRK procedures9,10,11.
LASIK is one of the most frequent types of eye surgery and a total of 40 million people had this operation worldwide between 1991 and 201612. Moreover, the prevalence of glaucoma is 2 to 4 times higher among the myopic population13. Thus, it is very important to obtain an accurate and real estimation of IOP in order not to miss ocular hypertension after myopic LRS.
The aim of our study is to describe a new modified GAT as well as its translational application and clinical outcomes by evaluating IOP measurements before and after myopic LRS. We also evaluate the reliability of the intra and inter-observer agreement.
Methods
New device description
How corneal tissue will react in real life to external elements can be estimated with finite element analysis (FEA). Three-dimensional (3D) modelling is more accurate than two-dimensional (2D) modelling for predicting what could occur to tissue in vivo14. In our study, we used 2D (Fig. 1) and 3D (Fig. S1, supplementary data) FEA to simulate the biomechanical responses of a normal cornea and a laser operated cornea (OC) to the contact of two external forces: a plane surface (corresponding to GAT) and a convex surface (corresponding to the new CT device). Various simulations were carried out with different corneal thicknesses and elastic behaviours of the cornea (Figs. S2–S4).
FEA simulation of corneal antero-posterior displacement in response to GAT (A,B) and CT (C) contact. The graphics below correspond to force applied from the centre to the periphery of the cornea within the anterior tonometer contact surface, and the colour scale indicates the maximum corneal deformation (MCD = N/m2). A corresponds to CC. B and C correspond to OC with a 100 μm ablation of CCT. A similar arc length and a wider contact pressure profile graphic are observed when GAT contact is compared with normal corneas (A), and CT contact is compared with operated corneas (C). However, when GAT is used on an OC (B), a confluence of forces is observed at the same point (asterisk, *) from the beginning, and the arc length contact is narrower. Young’s Modulus (Y) = 0.5 MPa. CC, calibrated cornea. OC, operated cornea.
Two different individual corneas were designed. First, a regular or “calibration cornea” (CC), as described in the Orssengo-Pye algorithm6, with CCT = 520 μm, an anterior corneal curvature of 7.8 mm, and assuming radial symmetry for a cornea-GAT contact of 3.06 mm (Fig. 1A). The second FEA consisted in a “LRS OC”, whose CCT and anterior radial symmetry could be ablated as in LRS up to 420 µm and 8.43 mm for different simulations (Figs. 1B,C and 2).
In all cases, a nonlinearity material model with Mooney-Rivlin parameters39 due to its invasive nature. Second, the sequence in which we measured IOP could imply certain bias in the second and third IOP measurements: repeated tonometry may induce changes in the anterior chamber volume and thus, in the registered pressure. AlMubrad et al.40 found a statistically significant IOP reduction (1.5 ± 1.2 mmHg; p < 0.05) on subsequent measurements performed with a non-contact tonometer (Topcon CT80) after GAT in 65 patients. Gaton et al.41 recorded a significant IOP decrease between first and second successive measurements with GAT (15.94 mmHg vs 14.9 mmHg, p < 0.0001) in 70 glaucomatous eyes. We believe that repeated contact of any external force with the eye may produce occasional IOP fluctuations. This would lead to significant underestimations that could be transcendent regarding glaucoma diagnosis. However, other considerations should be taken into account, such as IOP levels beyond the normal range or CB. A third source of bias in our study could be related to IOP diurnal fluctuation in time. Baseline IOP could be unbalanced across measurements after 3 months even if measurements are taken at the exact same time42. Further research could determine whether CT performs accurately.
Regarding variables that could influence our measurements, CRF showed a significant correlation for all the tonometers pre- and post-surgery. As in other reported studies33,43, CRF decreased after both procedures but mainly in LASIK as opposed to PRK. It is evident that PRK is less invasive than LASIK, which implies that CB properties are better conserved. We believe this could be the reason why CT overestimates IOP before surgery and performs less accurately in PRK corneas. This would coincide with our clinical findings for CT1 and CT2pre, which were not useful in non-operated corneas since they overestimated IOP measurements.
The posterior corneal shift after LRS procedures has been widely evaluated to detect possible ectasia44,45,46. However, no previous studies have specifically addressed how PCC changes could influence GAT IOP readings after LRS procedures. In 50 normal subjects, Firat et al.47 found that anterior and posterior curvature values and corneal volume do not influence IOP readings made with GAT. These results coincide with our pre-surgery results in which no IOP reading of any tonometer was correlated with PCC, simK or VOL in 102 normal patients. In the post operated subgroups, PCC and VOL also did not seem to influence IOP readings. We believe this could be related to posterior corneal curvature changes recovering three months after surgery46, which was the time our measurements were taken. On the other hand, CCT, Max. abl, and PTA could explain the differences among GATpre, CT1 and CT2post in the LASIK group. As more corneal tissue is removed in high myopia in the anterior stroma, it is expected that CB is more altered. Therefore, a bias could be expected for all the tonometers, which would have a significant impact on GAT readings, compared to the PRK group.
Both pre- and post-surgery tissue characteristics should be taken into account when IOP measurements are considered in post LRS corneas. Although we could expect post-surgery measurements to be close to those prior to surgery, a range of known variability (as we find in GAT with normal corneas) can be expected because tonometry is not personalized. In addition, the most accurate options for measuring IOP in LRS patients are not usually available or accessible to all ophthalmologists. This new simple and affordable option could solve a problem that has not yet been solved and make it available for universal use. Notwithstanding, new studies will be necessary to confirm the data analysis, make comparisons with other tonometers, and verify whether CT could also be used in patients with hypermetropic LRS, keratoconus, or after corneal transplantation.
Nevertheless, our device has demonstrated good agreement between GAT and CT1post in the LASIK subgroup, and thus minimizes the effect of the loss of central tissue in this type of surgery. The IA/IE results also indicate that there were no significant differences between observers, and therefore it could be a reproducible and convenient alternative for any ophthalmologist, and suitable for a currently very frequent and specific patient profile10,11. In conclusion, we have designed a new version of the applanation tonometer that could be used after LASIK instead of the current tonometer reference. This provides a new applanation tonometry option that is appropriate for supporting the diagnosis of ocular hypertension in this subgroup of patients.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to exclusive rights to intellectual property of the new “CT” convex tonometer secured by a Spanish patent filed P201631280, but are available from the corresponding author upon reasonable request.
References
Pfeiffer, N. et al. Central corneal thickness in the European Glaucoma Prevention Study. Ophthalmology 114, 454–459 (2007).
Moses, R. A. The Goldmann applanation tonometer. Am. J. Ophthalmol. 46, 865–869 (1958).
De Moraes, C. G. V., Prata, T. S. & Liebmann, J. R. R. Modalities of Tonometry and their Accuracy with Respect to Corneal Thickness and Irregularities. J. Optom. 1(2), 43–49 (2008).
Society, E. G. Terminology Guidelines. European Glaucoma Society Foundation (2017).
Liu, J. & Roberts, C. J. Influence of corneal biomechanical properties on intraocular pressure measurement: Quantitative analysis. J. Cataract Refract. Surg. 31, 146–155 (2005).
Hamilton, K. E. & Pye, D. C. Young’s modulus in normal corneas and the effect on applanation tonometry. Optom. Vis. Sci. 85, 445–450 (2008).
Mardelli, P. G., Piebenga, L. W., Whitacre, M. M., Siegmund, K. D. & Argus, W. A. The effect of excimer laser photorefractive keratectomy on intraocular pressure measurements using the Goldmann applanation tonometer. Ophthalmology 104, 945–949 (1997).
Duch, S., Serra, a, Castanera, J., Abos, R. & Quintana, M. Tonometry after laser in situ keratomileusis treatment. J. Glaucoma 10, 261–5 (2001).
Yang, E. & Roberts, C. J. A Review of Corneal Biomechanics after LASIK and SMILE and the Current Methods of Corneal Biomechanical Analysis. J. Clin. Exp. Ophthalmol. 06, (2015).
Sánchez-Navés J, Furfaro L, Piro O, B. S. Impact and permanence of LASIK-induced structural changes in the cornea on pneumotonometric measurements: contributions of flap cutting and stromal ablation. J Glaucoma Dec;17(8) (2008).
Knorz, M. C., Liesenhoff, H. & Liewnann, A. Laser In Situ Keratomileusis for Moderate and High Myopia and Myopic Astigmatism. Ophthalmology 105, 932–940 (1998).
Cummings, A. et al. LASIK Volume Around the Globe. April 2016. (2018).
Rochtchina, E., Mitchell, P. & Wang, J. J. Relationship between age and intraocular pressure: The Blue Mountains Eye Study. Clin. Exp. Ophthalmol. 30, 173–175 (2002).
Kling, S. & Hafezi, F. Corneal biomechanics – a review. Ophthalmic Physiol. Opt. 37, 240–252 (2017).
Su, P., Yang, Y., **ao, J. & Song, Y. Corneal hyper-viscoelastic model: Derivations, experiments, and simulations. Acta Bioeng. Biomech. 17, 73–84 (2015).
Pinsky, P. M., Van Der Heide, D. & Chernyak, D. Computational modeling of mechanical anisotropy in the cornea and sclera. J. Cataract Refract. Surg. 31, 136–145 (2005).
Recep, Ö. F., Hasiripi, H., Vayisoǧlu, E., Kalayci, D. & Sankatipoǧlu, H. Accurate time interval in repeated tonometry. Acta Ophthalmol. Scand. 76, 603–605 (1998).
Shen, M. et al. Diurnal variation of ocular hysteresis, corneal thickness, and intraocular pressure. Optom. Vis. Sci. 85, 1185–1192 (2008).
Fernández, J., Rodríguez-Vallejo, M., Martínez, J., Tauste, A. & Piñero, D. P. Corneal biomechanics after laser refractive surgery: Unmasking differences between techniques. J. Cataract Refract. Surg. 390–398, (2018).
Landis, J. R. & Koch, G. G. The Measurement of Observer Agreement for Categorical Data Data for Categorical of Observer Agreement The Measurement. 33, 159–174 (2012).
Alonso-Muñoz, L. et al. Assessment of appla- nation tonometry after hyperopic laser in situ keratomileusis. Cornea. 21, 156–160 (2002).
Agudelo LM, Molina CA, A. D. Changes in intraocular pressure after laser in situ keratomileusis for myopia, hyperopia, and astigmatism. J Refract Surg. Jul-Aug;18 (2002).
Shih, P., Wang, I., Cai, W. & Yen, J. Biomechanical Simulation of Stress Concentration and Intraocular Pressure in Corneas Subjected to Myopic Refractive Surgical Procedures. Sci. Rep. 1–15, (2017).
Shimmyo, M., Ross, A. J., Moy, A. & Mostafavi, R. Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am. J. Ophthalmol. 136, 603–613 (2003).
Yen, J.-Y., Wang, I.-J. & Shih, P.-J. On the in Vivo Estimation of the Corneal Young’s Modulus. JOJ Ophthalmol. 5, 1–8 (2017).
Sinha Roy, A., Dupps, W. J. & Roberts, C. J. Comparison of biomechanical effects of small-incision lenticule extraction and laser in situ keratomileusis: Finite-element analysis. J. Cataract Refract. Surg. 40, 971–980 (2014).
Roberts, C. J. Concepts and misconceptions in corneal biomechanics. J. Cataract Refract. Surg. 40, 862–869 (2014).
Chang, D. H. & Stulting, R. D. Change in intraocular pressure measurements after LASIK: The effect of the refractive correction and the lamellar flap. Ophthalmology 112, 1009–1016 (2005).
Brandt, J. D. et al. Adjusting intraocular pressure for central corneal thickness does not improve prediction models for primary open-angle glaucoma. Ophthalmology 119, 437–42 (2012).
Mccafferty, S., Lim, G., Duncan, W., Enikov, E. & Schwiegerling, J. Goldmann Tonometer Prism with an Optimized Error Correcting Applanation Surface. 5, (2016).
Mccafferty, S. et al. Goldmann tonometer error correcting prism: clinical evaluation. 835–840 (2017).
Mccafferty, S., Tetrault, K., Mccolgin, A., Levine, J. & Muller, M. Intraocular pressure measurement accuracy and repeatability of a modified Goldmann prism: Multi-center randomized clinical trial. Am. J. Ophthalmol. 196, 145–153 (2018).
Pepose, J. A. Y. S., Feigenbaum, S. K., Qazi, M. A., Sanderson, J. P. & Roberts, C. J. Changes in Corneal Biomechanics and Intraocular Pressure Following LASIK Using Static, Dynamic, and Noncontact Tonometry. 39–48, (2007).
Sales-Sanz, M. et al. Effect of Laser in Situ Keratomileusis on Schiøtz, Goldmann, and Dynamic Contour Tonometric Measurements. J. Glaucoma 25, e419–23 (2016).
Lam, A. K. C. et al. Effect of laser in situ keratomileusis on rebound tonometry and Goldmann applanation tonometry. J. Cataract Refract. Surg. 36, 631–636 (2010).
Hong, J. et al. A new tonometer-the corvis ST tonometer: Clinical comparison with noncontact and goldmann applanation tonometers. Investig. Ophthalmol. Vis. Sci. 54, 659–665 (2013).
Busool, Y. et al. Risk factors predicting steroid-induced ocular hypertension after photorefractive keratectomy. J. Cataract Refract. Surg. 43, 389–393 (2017).
Shokoohi-Rad, S., Daneshvar, R., Jafarian-Shahri, M. & Rajaee, P. Comparison between Betamethasone, Fluorometholone and Loteprednol Etabonate on intraocular pressure in patients after keratorefractive surgery. J. Curr. Ophthalmol. 30, 130–135 (2018).
Feltgen, N., Leifert, D. & Funk, J. Correlation between central corneal thickness, applanation tonometry, and direct intracameral iop readings. Br. J. Ophthalmol. 85, 85–87 (2001).
Almubrad, T. M. & Ogbuehi, K. C. The effect of repeated applanation on subsequent IOP measurements. Clin. Exp. Optom. 91, 524–529 (2008).
Gaton, D. D. et al. Effect of repeated applanation tonometry on the accuracy of intraocular pressure measurements. Curr. Eye Res. 35, 475–479 (2010).
Kim, S. H. et al. The effect of diurnal fluctuation in intraocular pressure on the evaluation of risk factors of progression in normal tension glaucoma. PLoS One 11, 1–14 (2016).
Kamiya, K., Shimizu, K. & Ohmoto, F. Comparison of the changes in corneal biomechanical properties after photorefractive keratectomy and laser in situ keratomileusis. Cornea 28, 765–9 (2009).
Ciolino, J. B. & Belin, M. W. Changes in the posterior cornea after laser in situ keratomileusis and photorefractive keratectomy. J. Cataract Refract. Surg. 32, 1426–1431 (2006).
Wang, L., Guo, H.-K., Zeng, J., **, H.-Y. & Meng, Q.-L. Stability of the posterior corneal surface after laser in situ keratomileusis for myopia. Int. J. Ophthalmol. 12, 52–54 (2012).
Roberts, C. J. & Dupps, W. J. Paired versus unpaired significance testing: How improper statistical analysis altered interpretation of posterior surface changes after LASIK. J. Cataract Refract. Surg. 40, 858–861 (2014).
Firat, P. G., Orman, G., Doganay, S. & Demirel, S. Influence of corneal parameters in keratoconus on IOP readings obtained with different tonometers. Clin. Exp. Optom. 96, 233–237 (2013).
Acknowledgements
The authors would like to thank Emilio Iglesias Touriño MD, PhD, an ophthalmologist whose extraordinary knowledge and advice was indispensable in the development of the new CT device. GRANT INFORMATION: MI received a personal research grant from the Catalonian Ophthalmology Society 2016–2018 Barcelona, Spain. This society played no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
M.I. collected, analysed and interpreted the sample data and was a major contributor in writing the original manuscript. F.Y. analysed and interpreted the physics analysis. B.K. analysed and interpreted the clinical results. C.S. interpreted the statistical analysis. L.A. and B.K. contributed to collecting double-masked inter-observer data. R.P.C.M., J.N. and R.B. reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Each of the co-authors has seen and agrees with the competing interests statement presented by M. Iglesias, MD (as corresponding author) on behalf of all the authors of the paper. Financial competing interests: M. Iglesias, MD has personal financial interests, being the inventor of the new “CT” applanation tonometer. M. Iglesias, MD has exclusive personal rights to the intellectual property of this invention secured by a Spanish patent filed P201631280 (awarded patent), and an international patent PCT/ES2017/070626 application (patent pending). M. Iglesias, MD declares no other financial competing interests. The rest of the co-authors declare no financial competing interests. Non-financial competing interests: M. Iglesias, MD and the rest of the co-authors declare they do not have non-financial competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iglesias, M., Yebra, F., Kudsieh, B. et al. New applanation tonometer for myopic patients after laser refractive surgery. Sci Rep 10, 7053 (2020). https://doi.org/10.1038/s41598-020-64013-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64013-4
- Springer Nature Limited