Abstract
Multidrug-resistant enterococcal pathogens, especially vancomycin-resistant enterococci (VRE), are among the pathogens that require new antibiotic innovation. The colonization of the gut represents a major pathway by which VRE can cause infection and spread to other patients. In the current study, auranofin (FDA-approved rheumatoid arthritis drug) is evaluated for its potential use as a decolonizing agent for VRE. Auranofin was found to exert potent antimicrobial activity against a wide range of enterococcal clinical isolates with a minimum inhibitory concentration of 1 μg/mL. No resistant mutants could be developed against auranofin over the course of 14 passages. Auranofin was also found to exert potent anti-biofilm activity against VRE. Auranofin was superior to linezolid, the drug of choice for VRE infection treatment, in the in vivo mouse model. Auranofin significantly reduced the VRE burden in feces, cecum, and ileum contents after 8 days of treatment. Accordingly, this study provides valuable evidence that auranofin has significant promise as a novel gastrointestinal decolonizing agent for VRE.
Similar content being viewed by others
Introduction
Enterococcal species are one of the major pathogens of healthcare settings1. Two strains, Enterococcus faecium and Enterococcus faecalis, are of major concern. Both strains can lead to bloodstream infection, endocarditis, meningitis, urinary tract infection, and other infections2. Enterococci, especially E. faecium, exhibits intrinsic resistance against several classes of antibiotics and can also develop resistance via mutation or exogenous gene transfer, which resulted in the emergence of multi-drug resistant enterococcal strains. The most pronounced resistance is against vancomycin. Vancomycin-resistant enterococcal (VRE) infections comprise most Enterococcus faecium infections as well as a significant proportion of Enterococcus faecalis infections1.
The widespread use of broad-spectrum antibacterial agents has contributed to the elevated prevalence of these opportunistic pathogens and the reduction of their antibiotic susceptibility2. Enterococci are normal inhabitants of several tissues of the human body, particularly the gastrointestinal tract (GIT). In the GIT Enterococci remain under the control of other intestinal commensals and gut cell receptors. The administration of high antibiotic concentrations, like in hospital settings, leads to reduced populations of susceptible gut commensals, which allows Enterococci to overgrow3,4. The VRE domination of the gut’s microbial consortium can persist even after the cessation of antibiotic treatment, and is usually followed by the translocation of the antibiotic-resistant bacteria across the mucosal barrier, which causes systemic infections4.
An effective decolonizing agent is required to prevent systemic VRE infections and limit the VRE endemicity in healthcare settings5. Unfortunately, no drugs are approved by the Food and Drug Administration (FDA) to decolonize VRE from the intestine. The clinical molecule, ramoplanin, was evaluated in Phase II of clinical trials and was able to temporarily suppress VRE colonization and was not tested further in Phase III6,7.
Repurposing FDA-approved drugs for which human safety, bioavailability, and efficacy have already been proven is an efficient approach to drug discovery8,9,10. Auranofin is an FDA-approved drug for the treatment of rheumatoid arthritis, it has a well-studied safety profile11. Adverse effects associated with auranofin administration are rare and mostly associated with long-term use. These adverse reactions include diarrhea (2–5% of the patients), skin rash, and extremely rare thrombocytopenia. In most cases, these adverse effects were all mild and usually self-limiting12. We recently showed that auranofin exerts broad-spectrum antibacterial and antifungal activities13,14. Auranofin was also shown to possess antiprotozoal activity, and is currently in Phase II studies for the treatment of amoebic dysentery and giardiasis15,16. Even though auranofin is oral bioavailable FDA-approved drug, only 20–30% of the oral dose is being absorbed17. These characteristics make auranofin a potential candidate to decolonize VRE in the GI tract. In the current study, auranofin is being evaluated for its ability to decolonize VRE in the GI tract.
Results
Susceptibility of enterococcal isolates to auranofin
We tested the activity of auranofin against a wide panel of enterococcal isolates and compared auranofin to the control antibiotics. Using the standard microdilution assay, auranofin was found to exhibit potent activity against the 27 tested isolates with an MIC range of 0.5 to 1 µg/ml (Table 1). Linezolid showed an MIC range of 0.5 to 16 µg/ml, ramoplanin showed an MIC range of 0.25 to 4 µg/ml, and vancomycin showed an MIC range of 0.5 to >128. The MIC90 (the minimum inhibitory concentration that inhabited 90% of the strains) of auranofin was found to be 1 µg/ml. The MIC90 for linezolid and ramoplanin was 2 and 4 µg/ml, respectively.
Killing kinetics of auranofin
After confirming the potent activity of auranofin against VRE, we next assessed the growth kinetics of VRE strain E. faecium HM 952 when exposed to auranofin at two different concentrations: 3X and 6X the MIC. As depicted in Fig. 1, auranofin at 3X and 6X reduced VRE by 2.57 and 2.72 after 72 hours, respectively. Linezolid, a known bacteriostatic against VRE, as expected did not reduce CFU after 72 hours of exposure. Ramoplanin, a known rapid bactericidal18,19, demonstrated rapid bactericidal activity against VRE and cleared the VRE within 4 hours.
In vitro multistep resistance development of VRE against auranofin
In order to test the likelihood of enterococci to develop resistance against auranofin, we serially passaged VRE isolate E. faecium HM 952 daily in the presence of a subinhibitory concentration of auranofin and control antibiotics for 14 days20. A four-fold shift in the MIC was considered resistance21. As presented in Fig. 2, the MIC of auranofin did not change over 14 passages, which indicates that VRE did not develop resistance to auranofin. There was a one-fold increase in the linezolid’s MIC observed over 14 passages. There was a rapid shift and increase to a 7-fold MIC after the second passage for gentamicin. VRE developed a 32-fold increase in MIC to gentamicin after 14 passages with the drug.
Multi-step resistance selection of auranofin, gentamicin, linezolid, and ramoplanin against VRE strain E. faecium HM 952. VRE was serially passaged with drugs for 14 days and the broth microdilution assay was used to determine the minimum inhibitory concentration of each drug against VRE after each successive passage. A 4-fold increase in the MIC is considered resistance.
Activity of auranofin against VRE biofilm
To examine whether the potential therapeutic application of auranofin could be expanded beyond the inhibition of planktonic VRE, we tested the ability of auranofin to inhibit biofilm formation in VRE and remove established biofilm. As presented in Fig. 3, auranofin at subinhibitory concentrations (0.0625X and 0.125X MIC) resulted in a significant reduction (~50%) of the VRE’s biofilm-forming ability. Linezolid did not inhibit the biofilm formation in VRE, and ramoplanin exhibited a 30% VRE reduction at 0.125X MIC.
The anti-biofilm activity of auranofin against E. faecalis NR 31972. (A) Biofilm inhibition activity of auranofin; Sub-inhibitory concentrations of the drugs were added at the same time with the bacteria in TSB + 1% glucose and incubated for 24 hours at 37 °C, then the biofilm density was measured using crystal violet. (B) Biofilm eradication activity of auranofin; The bacteria were incubated for 24 hours in TSB + 1% glucose to allow for the formation of mature biofilm. Drugs were then added and incubated with the bacterial biofilm for additional 24 hours before the biofilm density was measured. (*) Denotes significant difference from the DMSO treated control, while (‡) denotes a significant difference from the linezolid treated wells at equal concentration.
Next, we tested auranofin activity against established VRE biofilm. Auranofin at concentrations of 4, 8, and 16X MIC significantly reduced the established VRE biofilm by 50, 60 and 95%, respectively. Linezolid at 4, 8, and 16X MIC reduced the established VRE biofilm by 30, 40 and 50%, respectively. Ramoplanin concentrations of at 4, 8, and 16X MIC reduced the established VRE biofilm by 55, 55, and 65%, respectively.
Activity of auranofin against enterococci in an in vivo model of intestinal VRE colonization
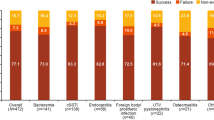
In order to validate our in vitro results, the VRE-colonization model3,22,23 was utilized to assess the ability of auranofin to reduce the shedding and burden of VRE in the gastrointestinal tract of mice. As presented in Fig. 4, auranofin and ramoplanin were superior to linezolid in decreasing the burden of VRE in fecal samples collected from mice. After three days of treatment, auranofin significantly reduced the burden of VRE in fecal samples by more than 97.79%, a rate similar to ramoplanin (99.5%). Linezolid, in contrast, was unable to reduce the burden of VRE after three days of treatment. The presence of VRE in the fecal samples of mice treated with auranofin diminished to a remarkable 99.12% reduction after five days of treatment. Linezolid generated a 52.18% reduction in the VRE CFU count of fecal samples after five days of treatment. Mice treated with ramoplanin exhibited a 99.99% reduction of VRE in the fecal samples after five days for treatment. The burden of VRE (~107 CFU/gram feces) remained consistent in the control group (untreated mice) throughout the course of even days, which suggests that the decrease in VRE burden observed in mice receiving auranofin, ramoplanin, or linezolid was primarily due to the treatment received (rather than the excretion elimination of bacteria from the intestinal tract), data are shown in Fig. 5.
Bacterial counts of E. faecium HM-952 in the fecal samples of the mice. Infected mice were orally treated with auranofin (0.5 mg/kg), linezolid (10 mg/kg) and ramoplanin (10 mg/kg) daily for 8 days, one group was left untreated. Fecal samples were freshly collected from each group in days 0, 3, 5 and 7 post treatment. (*) Denotes significant difference from the untreated group (P < 0.05).
Bacterial counts of E. faecium HM 952 in (A) cecum and (B) ileum contents of the mice. Infected mice (5/group) were orally treated with auranofin (0.5 mg/kg), linezolid (10 mg/kg) and ramoplanin (10 mg/kg) daily for 8 days, one group was left untreated. Cecum and ileum contents were collected on day 9. (*) Denotes significant difference from the untreated group (P < 0.05) (#) denotes significant difference from the Linezolid-treated group (P < 0.05).
A similar pattern was observed in the cecum and ileum contents. Linezolid did not reduce the cecum and ileum bacterial counts. Auranofin and ramoplanin significantly reduced the VRE load in the cecum and ileum. Auranofin decreased the burden of VRE in the cecal content by 1.4-log10 and in the ileal content by 1.3-log10, relative to the untreated mice. Ramoplanin decreased the burden of VRE in the cecal content by 2.3-log10 and in the ileal content by 1.8-log10, relative to untreated mice.
Discussion
Enterococci are normal inhabitants of several human body niches, especially the GIT. Enterococci have the capacity to overgrow other normal flora and colonize the gut, particularly after the administration of broad spectrum antibiotics. Heavy VRE gut colonization usually precedes infections and is considered the initial source of bacteremia-induced endocarditis2,3,24,25. Moreover, the increased number of colonized patients increases the colonization pressure and the enterococcal acquisition by other patients26. Enterococci are naturally resistant to several antibiotics and can rapidly develop resistance to antibiotics via several mechanisms27,28. Vancomycin resistance is one of the most remarkable resistances developed by enterococci. More than one third of enterococcal infections in the U.S. are caused by VRE, and the percentage is higher for infections caused by E. faecium (almost 80%)29. Furthermore, VRE also displays resistance to the other clinically important antibiotics like ampicillin and aminoglycosides2,28,30. Enterococci are capable of forming biofilm, a feature that not only facilitates infections but also helps to colonize the GIT31,32.
Despite the significance of enterococcal colonization of the gut, the FDA has yet to approve a drug that can be used for VRE decolonization2,25. Also, the current control methods, including contact precautions and isolation of the patient are costly, have negative psychological impact on the patients and were not proven to have positive clinical outcomes33. Overall, there is an unmet and urgent need for a potent decolonizing agent against VRE.
Auranofin is an FDA-approved drug for the treatment of rheumatoid arthritis. It has a well-defined toxicity profile and an acceptable safety for human use34,35. Auranofin was reported to have a potent inhibitory activity against Gram-positive bacteria, including enterococci, fungi and parasites12,36,37. Due to its poor intestinal absorption auranofin has been granted orphan-drug status from the FDA for treatment of intestinal amebiasis, and is currently in a Phase II clinical trial for treatment of intestinal giardiasis16,34,36.
In the current study we showed the superior in vitro activity of auranofin against a broad panel of enterococcus isolates compared to linezolid (the drug of choice for the treatment of VRE infections) and ramoplanin (clinical molecule currently in clinical trials for VRE decolonization). It is worth mentioning that the activity of auranofin did not change between vancomycin-resistant and vancomycin-sensitive strains. Auranofin was also consistent against both E. faecium and E. faecalis, a property that is lacking in some current antibacterial agents, for example quinupristin-dalfopristin27.
A time-kill assay was utilized to ascertain whether auranofin is bacteriostatic or bactericidal. Auranofin exerted a bacteriostatic effect against the tested VRE isolate, a result that concurs with the previous report against staphylococcus aureus at equal concentration38. Although the bacterial count was reduced after 24 hours, it did not reach to the 3-log10 cutoff value that distinguishes bacteriostatics from bactericidals. The bacteriostatic activity of auranofin should not be discouraging, especially in the GIT environment of numerous competing microorganisms.
In previous studies, auranofin exhibited a complex mechanism of action against methicillin-resistant staphylococcus aureus (MRSA), a possible reason for MRSA’s inability to develop resistance against auranofin36. These results were encouraging for our test of VRE’s ability to develop resistance against auranofin. As reported earlier, the MIC of auranofin against the tested isolate did not change during the 14-day experiment and even up to 25 days (data not shown). This is in agreement with the previous reports of failure to generate auranofin-resistant MRSA36,39.
As discussed earlier, biofilm is a virulence factor that helps enterococci to establish colonization. Biofilm-positive enterococcal phenotypes are associated with GI colonization. Auranofin is known to inhibit the enterococcal biofilm through the inhibition of selenium metabolism and selenoenzymes, given that biofilm formation is reported to enhance gut colonization of enterococci31,40. We sought to test the biofilm inhibition activity of auranofin as well as the ability of auranofin to eradicate established biofilms. As was expected, when auranofin was incubated with the bacteria, auranofin significantly inhibited the biofilm formation at sub-MIC concentrations (Fig. 3A). While linezolid and ramoplanin had no effect at all or a minimal effect, auranofin inhibited about 50% of the biofilm formation when compared to the untreated control. Additionally, auranofin treatment to the already formed biofilm drastically reduced the biofilm intensity at supra-MIC concentration. This effect was superior to those of linezolid and ramoplanin (Fig. 3B). Biofilm enhances enterococcal colonization capacity, and the antibiofilm activity is particularly important in evaluating the decolonization efficiency of auranofin31.
Auranofin’s potent in vitro activity against numerous multi drug-resistant enterococcus strains and the inhibition of VRE biofilm (combined with the low intestinal absorption of auranofin and the inability of VRE to develop resistance against auranofin in vitro) prompted us to investigate the efficacy of auranofin in vivo in the VRE colonization mouse model. We were interested in evaluating the ability of auranofin to reduce the VRE shedding in fecal samples as well as reduce the VRE burden in the mice guts. The ampicillin-primed mice were infected with a VRE strain, and treatment began after the VRE colonization was established. At a concentration of 0.5 mg/kg, auranofin significantly reduced the bacterial shedding in fecal samples after only three days of treatment. By the seventh day of treatment, the bacterial shedding was reduced by about 99% compared to the untreated control (Fig. 4). Auranofin (at the same concentration, 0.5 mg/kg) reduced the bacterial load in cecum and ileum contents (Fig. 5) by more than 99.9%. This effect was superior to linezolid at a concentration of 10 mg/kg, which had a minimal effect in fecal samples and no significant effect in cecum and ileum contents. Although both auranofin and linezolid are bacteriostatic, linezolid’s lack of activity is possibly due to its complete absorption from the GI tract41. The auranofin dose used in this study is lower than the published toxic dose (TDLo) in humans (0.54 mg/kg)42, and is far less than the oral LD50 in mice, 84.94 mg/kg43. Although auranofin was not as effective as ramoplanin in reducing the VRE burden in the mouse model, auranofin is FDA-approved and ramoplanin—a Phase II clinical molecule—is not. Further investigations are needed to test whether VRE recurrence observed with ramoplanin treatment is also encountered with auranofin treatment7 as well as the effect of auranofin on the normal bacterial population of the gut. Overall, the current study suggests that auranofin is a good candidate for further investigation as a decolonizing agent of VRE.
Materials and Methods
Bacterial strains and chemicals
Vancomycin-resistant Enterococci (VRE) strains (Table 1) were obtained from the American type culture collection (ATCC) and Biodefense and Emerging Infections Research Resources Repository (BEI Resources). All experiments were carried out in accordance with relevant guidelines and regulations and were approved by the Institutional Biosafety Committee of Purdue University. All chemicals and reagents were purchased from commercial vendors. Auranofin, linezolid (Chem-impex International, Wood Dale, IL), ampicillin (Peosta, IA), vancomycin hydrochloride (Gold Biotechnology, St. Louis, MO), gentamicin sulfate (Fisher Bioreagents, Fairlawn, NJ), and ramoplanin (Sigma-Aldrich, St. Louis, MO) were purchased commercially. Brain heart infusion (BHI), tryptic soya broth (TSB), tryptic soya agar (TSA) and enterococcosel broth were purchased from BD (Becton, Dickinson and Company, Cockeysville, MD) and Phosphate buffered saline (PBS) was purchased from corning (Corning, NY).
In vitro antibacterial assay
The standard broth microdilution assay was utilized to assess the minimum inhibitory concentration (MIC) of auranofin and the control antibiotics following the guidelines of the Clinical and Laboratory Standards Institute (CLSI)44. The minimum inhibitory concentrations (MICs) reported are the lowest concentration of each drug that could inhibit the visual turbidity due to bacterial growth. MIC90 is the drug concentration that can inhibit the growth of 90% of the tested isolates.
Killing kinetics of auranofin and control drugs
A time-kill assay was performed as described previously45,46,47,48. Briefly, an overnight culture of E. faecium HM-952 was diluted to approximately 106 CFU/ml. Three- and six-fold MIC of auranofin and the control drugs, in triplicates, were incubated with the bacterial suspension for 24 hours. At the indicated time intervals, samples were taken, diluted, and cultured on BHI agar to detect the bacterial counts at each time point.
In vitro development of resistant mutants
To assess the propensity of VRE to develop resistance against auranofin, E. faecium strain HM-952 was serially passaged with sub inhibitory concentrations of auranofin and control drugs (linezolid, ramoplanin, and gentamicin) in 14 passages over a period of two weeks. Resistance was defined as a 4-fold shift in the MIC20,21,23.
Auranofin activity against VRE biofilm
A Biofilm Inhibition assay was utilized to examine the effect of sub-inhibitory concentrations of auranofin on the ability of VRE to form biofilm as described before49,50. Briefly, an overnight culture of E. faecalis NR 31972 was diluted 1:100 in TSB +1% glucose and seeded in 96-well plates. Different sub-inhibitory concentrations of auranofin and control antibiotics (linezolid and ramoplanin) were added, and the plates were incubated for 24 hours at 37 °C. After incubation, the medium containing drugs and planktonic bacteria was discarded, and the adherent biofilms were washed twice with Phosphate buffered saline (PBS). The plates were then stained with 0.1% crystal violet for 30 minutes and washed again to remove the non-adherent stain. The remaining stain was solubilized using 95% ethanol for 45 minutes. Then the OD595 was measured using a kinetic microplate reader (SpectraMax i3x, Molecular Devices LLC, Sunnyvale, CA).
The auranofin activity was assessed against the mature biofilms using the aforementioned protocol. The drugs were added at concentrations higher than the MIC to allow for the effective eradication of the mature biofilm. All experiments were carried out in quadruplicates and repeated at least twice.
Decolonization of VRE from the gastro-intestinal tract of mice
The study was reviewed, approved, and performed under the guidelines of the Purdue University Animal Care and Use Committee (PACUC) and carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. To assess the efficiency of auranofin in decolonizing VRE from the gut in an animal model, the VRE mice decolonization model was followed3,23. Briefly, 6-week-old female C57BL/6 mice (Envigo, Indianapolis, IN) were sensitized by ampicillin (0.5 gm/ml in drinking water) for seven days. One day later mice were orally infected with 3 × 108 CFU/mL of VRE strain E. faecium HM-952. Seven days post infection, the mice were divided into groups and treated orally with either auranofin (0.5 mg/kg), linezolid (10 mg/kg), ramoplanin (10 mg/kg), or PBS. Treatments were continued for eight days before the mice were humanely euthanized on day 9 via CO2 asphyxiation. Fecal samples were taken freshly from the mice on days 0, 3, 5 and 7 post treatment. The cecum and ileum contents were collected following euthanasia. The contents of the cecum and ileum as well as the fecal sample were weighed, diluted with PBS, plated on enterococcosel agar (supplemented with vancomycin, 8 µg/mL), and incubated for 48 hours at 37 °C to determine the bacterial count in each sample.
Statistical analysis
GraphPad Prism version 7.00 for Windows (GraphPad Software, La Jolla CA) was utilized in performing the statistical analysis. Two-way ANOVA followed by Dunnett’s multiple comparisons test was performed to analyze biofilm inhibition and eradication data and the data from fecal samples. For the data generated from cecum and ileum content, one-way ANOVA was used and was followed by t test for the post hoc pairwise comparison.
Data availabilit
All data generated or analyzed in this study are available from the corresponding author on reasonable request.
References
Rice, L. B. Antimicrobial resistance in gram-positive bacteria. Am J Infect Control 34, S11–19; discussion S64–73, https://doi.org/10.1016/j.ajic.2006.05.220 (2006).
Agudelo Higuita, N. I. & Huycke, M. M. In Enterococci: From Commensals to Leading Causes of Drug Resistant Infection (eds M. S. Gilmore, D. B. Clewell, Y. Ike, & N. Shankar) (2014).
Ubeda, C. et al. Vancomycin-resistant Enterococcus domination of intestinal microbiota is enabled by antibiotic treatment in mice and precedes bloodstream invasion in humans. J Clin Invest 120, 4332–4341, https://doi.org/10.1172/JCI43918 (2010).
Lebreton, F., Willems, R. J. L. & Gilmore, M. S. In Enterococci: From Commensals to Leading Causes of Drug Resistant Infection (eds M. S. Gilmore, D. B. Clewell, Y. Ike, & N. Shankar) (2014).
Cheng, V. C. et al. Decolonization of gastrointestinal carriage of vancomycin-resistant Enterococcus faecium: case series and review of literature. BMC Infect Dis 14, 514, https://doi.org/10.1186/1471-2334-14-514 (2014).
Wong, M. T. et al. Effective suppression of vancomycin-resistant Enterococcus species in asymptomatic gastrointestinal carriers by a novel glycolipodepsipeptide, ramoplanin. Clin Infect Dis 33, 1476–1482, https://doi.org/10.1086/322687 (2001).
Montecalvo, M. A. Ramoplanin: a novel antimicrobial agent with the potential to prevent vancomycin-resistant enterococcal infection in high-risk patients. J Antimicrob Chemother 51(Suppl 3), iii31–35, https://doi.org/10.1093/jac/dkg274 (2003).
Younis, W., AbdelKhalek, A., Mayhoub, A. S. & Seleem, M. N. In Vitro Screening of an FDA-Approved Library Against ESKAPE Pathogens. Curr Pharm Des 23, 2147–2157, https://doi.org/10.2174/1381612823666170209154745 (2017).
Thangamani, S. et al. Ebselen exerts antifungal activity by regulating glutathione (GSH) and reactive oxygen species (ROS) production in fungal cells. Biochim Biophys Acta 1861, 3002–3010, https://doi.org/10.1016/j.bbagen.2016.09.029 (2017).
Younis, W., Thangamani, S. & Seleem, M. N. Repurposing Non-Antimicrobial Drugs and Clinical Molecules to Treat Bacterial Infections. Curr Pharm Des 21, 4106–4111 (2015).
Thangamani, S., Mohammad, H., Younis, W. & Seleem, M. N. Drug repurposing for the treatment of staphylococcal infections. Curr Pharm Des 21, 2089–2100 (2015).
Roder, C. & Thomson, M. J. Auranofin: repurposing an old drug for a golden new age. Drugs in R&D 15, 13–20, https://doi.org/10.1007/s40268-015-0083-y (2015).
Thangamani, S., Mohammad, H., Abushahba, M. F., Sobreira, T. J. & Seleem, M. N. Repurposing auranofin for the treatment of cutaneous staphylococcal infections. Int J Antimicrob Agents 47, 195–201, https://doi.org/10.1016/j.ijantimicag.2015.12.016 (2016).
Thangamani, S. et al. Repurposing Approach Identifies Auranofin with Broad Spectrum Antifungal Activity That Targets Mia40-Erv1 Pathway. Front Cell Infect Microbiol 7, 4, https://doi.org/10.3389/fcimb.2017.00004 (2017).
Parsonage, D. et al. X-ray structures of thioredoxin and thioredoxin reductase from Entamoeba histolytica and prevailing hypothesis of the mechanism of Auranofin action. J Struct Biol 194, 180–190, https://doi.org/10.1016/j.jsb.2016.02.015 (2016).
Tejman-Yarden, N. et al. A reprofiled drug, auranofin, is effective against metronidazole-resistant Giardia lamblia. Antimicrob Agents Chemother 57, 2029–2035, https://doi.org/10.1128/AAC.01675-12 (2013).
Blocka, K. L., Paulus, H. E. & Furst, D. E. Clinical pharmacokinetics of oral and injectable gold compounds. Clin Pharmacokinet 11, 133–143, https://doi.org/10.2165/00003088-198611020-00003 (1986).
Johnson, C. C., Taylor, S., Pitsakis, P., May, P. & Levison, M. E. Bactericidal activity of ramoplanin against antibiotic-resistant enterococci. Antimicrob Agents Chemother 36, 2342–2345 (1992).
Cheng, M., Huang, J. X., Ramu, S., Butler, M. S. & Cooper, M. A. Ramoplanin at bactericidal concentrations induces bacterial membrane depolarization in Staphylococcus aureus. Antimicrob Agents Chemother 58, 6819–6827, https://doi.org/10.1128/AAC.00061-14 (2014).
Mohammad, H. et al. Phenylthiazole Antibacterial Agents Targeting Cell Wall Synthesis Exhibit Potent Activity in Vitro and in Vivo against Vancomycin-Resistant Enterococci. J Med Chem 60, 2425–2438, https://doi.org/10.1021/acs.jmedchem.6b01780 (2017).
Garcia, L. S. & Isenberg, H. D. Clinical microbiology procedures handbook. 3rd edn, (ASM Press, 2010).
Seiler, P. et al. Cadazolid Does Not Promote Intestinal Colonization of Vancomycin-Resistant Enterococci in Mice. Antimicrob Agents Chemother 60, 628–631, https://doi.org/10.1128/AAC.01923-15 (2015).
Mohammad, H., AbdelKhalek, A., Abutaleb, N. S. & Seleem, M. N. Repurposing niclosamide for intestinal decolonization of vancomycin-resistant enterococci. Int J Antimicrob Agents, https://doi.org/10.1016/j.ijantimicag.2018.02.003 (2018).
Cattoir, V. & Leclercq, R. Twenty-five years of shared life with vancomycin-resistant enterococci: is it time to divorce? J Antimicrob Chemother 68, 731–742, https://doi.org/10.1093/jac/dks469 (2013).
Arias, C. A. & Murray, B. E. The rise of the Enterococcus: beyond vancomycin resistance. Nat Rev Microbiol 10, 266–278, https://doi.org/10.1038/nrmicro2761 (2012).
Bonten, M. J. et al. The role of “colonization pressure” in the spread of vancomycin-resistant enterococci: an important infection control variable. Archives of internal medicine 158, 1127–1132 (1998).
Hollenbeck, B. L. & Rice, L. B. Intrinsic and acquired resistance mechanisms in enterococcus. Virulence 3, 421–433, https://doi.org/10.4161/viru.21282 (2012).
Miller, W. R., Munita, J. M. & Arias, C. A. Mechanisms of antibiotic resistance in enterococci. Expert review of anti-infective therapy 12, 1221–1236, https://doi.org/10.1586/14787210.2014.956092 (2014).
O’Driscoll, T. & Crank, C. W. Vancomycin-resistant enterococcal infections: epidemiology, clinical manifestations, and optimal management. Infect Drug Resist 8, 217–230, https://doi.org/10.2147/IDR.S54125 (2015).
Beier, R. C. et al. Antibiotic and disinfectant susceptibility profiles of vancomycin-resistant Enterococcus faecium (VRE) isolated from community wastewater in Texas. Bull Environ Contam Toxicol 80, 188–194, https://doi.org/10.1007/s00128-007-9342-0 (2008).
Creti, R., Koch, S., Fabretti, F., Baldassarri, L. & Huebner, J. Enterococcal colonization of the gastro-intestinal tract: role of biofilm and environmental oligosaccharides. BMC Microbiol 6, 60, https://doi.org/10.1186/1471-2180-6-60 (2006).
Mohamed, J. A. & Huang, D. B. Biofilm formation by enterococci. J Med Microbiol 56, 1581–1588, https://doi.org/10.1099/jmm.0.47331-0 (2007).
Ho, C., Lau, A., Cimon, K., Farrah, K. & Gardam, M. In Screening, Isolation, and Decolonization Strategies for Vancomycin-Resistant Enterococci or Extended Spectrum Beta-Lactamase Producing Organisms: A Systematic Review of the Clinical Evidence and Health Services Impact CADTH Rapid Response Reports (2012).
Kean, W. F., Hart, L. & Buchanan, W. W. Auranofin. Br J Rheumatol 36, 560–572 (1997).
Glennas, A. et al. Auranofin is safe and superior to placebo in elderly-onset rheumatoid arthritis. Br J Rheumatol 36, 870–877 (1997).
Thangamani, S. et al. Antibacterial activity and mechanism of action of auranofin against multi-drug resistant bacterial pathogens. Sci Rep 6, 22571, https://doi.org/10.1038/srep22571 (2016).
Fuchs, B. B. et al. Inhibition of bacterial and fungal pathogens by the orphaned drug auranofin. Future Med Chem 8, 117–132, https://doi.org/10.4155/fmc.15.182 (2016).
Cassetta, M. I., Marzo, T., Fallani, S., Novelli, A. & Messori, L. Drug repositioning: auranofin as a prospective antimicrobial agent for the treatment of severe staphylococcal infections. Biometals 27, 787–791, https://doi.org/10.1007/s10534-014-9743-6 (2014).
Harbut, M. B. et al. Auranofin exerts broad-spectrum bactericidal activities by targeting thiol-redox homeostasis. Proc Natl Acad Sci USA 112, 4453–4458, https://doi.org/10.1073/pnas.1504022112 (2015).
Srivastava, M., Mallard, C., Barke, T., Hancock, L. E. & Self, W. T. A selenium-dependent xanthine dehydrogenase triggers biofilm proliferation in Enterococcus faecalis through oxidant production. J Bacteriol 193, 1643–1652, https://doi.org/10.1128/JB.01063-10 (2011).
Dryden, M. S. Linezolid pharmacokinetics and pharmacodynamics in clinical treatment. J Antimicrob Chemother 66(Suppl 4), iv7–iv15, https://doi.org/10.1093/jac/dkr072 (2011).
Gambari, P., Ostuni, P., Lazzarin, P., Tavolato, B. & Todesco, S. Neurotoxicity following a very high dose of oral gold (auranofin). Arthritis Rheum 27, 1316–1317 (1984).
Coppi, G., Borella, F., Gatti, M. T., Comini, A. & Dall’Asta, L. Synthesis, antiinflammatory and antiarthritic properties of a new tiopronine gold derivative. Boll Chim Farm 128, 22–24 (1989).
(CLSI), C. a. L. S. I. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard—Ninth Edition M07-A9. 32 No. 2 (January 2012).
Thangamani, S., Younis, W. & Seleem, M. N. Repurposing celecoxib as a topical antimicrobial agent. Front Microbiol 6, 750, https://doi.org/10.3389/fmicb.2015.00750 (2015).
Mohamed, M. F., Brezden, A., Mohammad, H., Chmielewski, J. & Seleem, M. N. Targeting biofilms and persisters of ESKAPE pathogens with P14KanS, a kanamycin peptide conjugate. Biochim Biophys Acta 1861, 848–859, https://doi.org/10.1016/j.bbagen.2017.01.029 (2017).
Mohamed, M. F., Brezden, A., Mohammad, H., Chmielewski, J. & Seleem, M. N. A short D-enantiomeric antimicrobial peptide with potent immunomodulatory and antibiofilm activity against multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Sci Rep 7, 6953, https://doi.org/10.1038/s41598-017-07440-0 (2017).
Mohammad, H. et al. Bacteriological profiling of diphenylureas as a novel class of antibiotics against methicillin-resistant Staphylococcus aureus. PLoS One 12, e0182821, https://doi.org/10.1371/journal.pone.0182821 (2017).
Mohammad, H., Mayhoub, A. S., Cushman, M. & Seleem, M. N. Anti-biofilm activity and synergism of novel thiazole compounds with glycopeptide antibiotics against multidrug-resistant staphylococci. J Antibiot (Tokyo) 68, 259–266, https://doi.org/10.1038/ja.2014.142 (2015).
Thangamani, S. et al. Exploring simvastatin, an antihyperlipidemic drug, as a potential topical antibacterial agent. Sci Rep 5, 16407, https://doi.org/10.1038/srep16407 (2015).
Acknowledgements
This work was supported by the National Institutes of Health [grant number R01AI130186].
Author information
Authors and Affiliations
Contributions
A.A. designed and performed the M.I.C. and M.B.C. experiments, multi-step resistance selection assay, biofilm assays, animal infection experiment, and wrote the manuscript; N.S.A. and K.A.E. assisted with the M.I.C. and M.B.C. experiments, time-kill assay, and multi-step resistance selection experiment. M.N.S. interpreted the results and wrote the manuscript. All authors contributed to analyze and interpret the results.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
AbdelKhalek, A., Abutaleb, N.S., Elmagarmid, K.A. et al. Repurposing auranofin as an intestinal decolonizing agent for vancomycin-resistant enterococci. Sci Rep 8, 8353 (2018). https://doi.org/10.1038/s41598-018-26674-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-26674-0
- Springer Nature Limited