Abstract
Background
A national, lung cancer screening programme is under consideration in Australia, and we assessed cost-effectiveness using updated data and assumptions.
Methods
We estimated the cost-effectiveness of lung screening by applying screening parameters and outcomes from either the National Lung Screening Trial (NLST) or the NEderlands–Leuvens Longkanker Screenings ONderzoek (NELSON) to Australian data on lung cancer risk, mortality, health-system costs, and smoking trends using a deterministic, multi-cohort model. Incremental cost-effectiveness ratios (ICERs) were calculated for a lifetime horizon.
Results
The ICER for lung screening compared to usual care in the NELSON-based scenario was AU$39,250 (95% CI $18,150–108,300) per quality-adjusted life year (QALY); lower than the NLST-based estimate (ICER = $76,300, 95% CI $41,750–236,500). In probabilistic sensitivity analyses, lung screening was cost-effective in 15%/60% of NELSON-like simulations, assuming a willingness-to-pay threshold of $30,000/$50,000 per QALY, respectively, compared to 0.5%/6.7% for the NLST. ICERs were most sensitive to assumptions regarding the screening-related lung cancer mortality benefit and duration of benefit over time. The cost of screening had a larger impact on ICERs than the cost of treatment, even after quadrupling the 2006–2016 healthcare costs of stage IV lung cancer.
Discussion
Lung screening could be cost-effective in Australia, contingent on translating trial-like lung cancer mortality benefits to the clinic.
Similar content being viewed by others
Introduction
Lung cancer is the leading cause of cancer-related death, both in Australia and worldwide [1]. Poor prognosis, poor quality of life and substantial healthcare resource requirements mean there is a continuing need for effective and cost-effective lung cancer control interventions. Primary prevention through tobacco control is likely to remain the most effective, equitable, and cost-effective long-term strategy for reducing the burden of lung cancer. However, given the 20–30 year lag between population-level tobacco exposure and lung cancer incidence, the full benefits of these interventions will not be realised for many years to come [2]. A population-based lung cancer screening programme has the potential to mitigate the adverse impact of historical smoking trends on health, and save many lives by detecting lung cancer at an early stage.
Two randomised controlled trials have demonstrated a significant lung cancer mortality reduction among individuals with a history of heavy tobacco exposure screened with low-dose computed tomography (LDCT). The U.S. National Lung Screening Trial (NLST) in 2011 [3] found a 20% (95% confidence interval; CI 6.8%–26.7%) lung cancer mortality reduction and more recently, the NEderlands–Leuvens Longkanker Screenings ONderzoek (NELSON) [4] demonstrated a 24% (cumulative rate ratio 0.76, 95% CI 0.61–0.94) reduction for men (33% for women; cumulative rate ratio 0.67, 95% CI 0.38–1.14). These trials resulted in several agencies recommending lung cancer screening for people at high risk, including the U.S. Preventative Services Task Force (USPSTF [5, 6]), and health economic evaluations of lung screening have demonstrated favourable cost-effectiveness estimates in many settings [7,8,9,10,11].
In 2021, an Australian Government-led enquiry recommended the implementation of a population-wide, risk-based lung screening programme [12]. Previous published health economic evaluations of lung cancer screening in the Australian setting found that LDCT screening was not likely to be cost-effective [13, 14], however, the evidence on lung screening has advanced since those reports, including the results of the NELSON trial. We provide an updated cost-effectiveness estimate for the Australian healthcare system by using new modelled data on Australian rates of smoking initiation and cessation, Australian lung cancer mortality and survival, as well as updated Australian health services costs, to assess the economic impact given the lung cancer screening outcomes observed in the NELSON and NLST trials.
Methods
A cumulative lifetime risk model was implemented in R [15, 16], where Australian rates of all-cause and lung cancer (LC) mortality by sex, age and smoking status were used to estimate the number of LC cases and life-years/quality-adjusted life-years (LYs/QALYs) gained in a hypothetical scenario comparing a screened (applying NLST or NELSON trial parameters) versus unscreened population. That is, we modelled the direct impact of the screening-related lung cancer mortality benefit observed in the trials on population-level lung cancer mortality rates. Incremental costs, incremental benefits and the incremental cost-effectiveness ratio (ICER) of each trial setting in the Australian population compared to usual care were estimated. A probabilistic sensitivity analysis was used to determine the 95% confidence intervals for incremental costs, benefits, and ICERs for our base case (see Fig. 1a). A universal public payer perspective was taken. Detailed information on the model, data inputs, parameters and assumptions are provided in the Supplementary Appendix.
a Scatter plot of incremental costs (in AU$/person) vs incremental QALYs/person obtained from the PSA for the NELSON and NLST settings. b Corresponding estimated cost-effectiveness curve given the ICER distributions obtained from the PSA. c, d Histograms showing the ICER distributions obtained from the PSA for the NLST and NELSON settings, respectively. ICER Incremental cost-effectiveness ratio, QALY quality-adjusted life-year, NELSON Nederlands–Leuvens Longkanker Screenings Onderzoek, NLST National Lung Screen Trial, PSA probabilistic sensitivity analysis.
Data inputs
Screening parameters
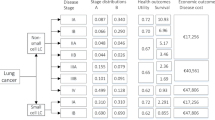
Data on the eligible age range, the number of screens, screening-related LC stage shift, follow-up CT rate, false-positive rate, overdiagnosis, and LC mortality benefit were ascertained from the NLST and the NELSON trial and modelled separately according to each trial (Table 1) [3, 4, 17]. For the NLST, false positive scans were partitioned into those requiring a follow-up CT scan (~15% of scans) and those requiring other diagnostic work-up (~8.5%) [3].
Screening-eligible population
A compartmental model of smoking prevalence, detailed in Wade et al. [18], calibrated to the observed distribution of smoking status (current daily/never/former) among individuals aged 20–99 years from 1962–2016 by sex and birth year (1910–1996) [19], was used to estimate the prevalence of current and former smoking in Australia, 2020–2066. Estimates were simulated using 50-year population projections [20] and accounted for all-cause mortality rates stratified by smoking status [18]. In the base case, we applied the estimated background all-cause mortality rate of individuals whose smoking status was “current” to those with both “current” and “former” smoking status.
The proportion of Australians eligible for screening was estimated by applying the NLST and NELSON selection criteria to a population-based Australian cohort study, the Sax Institute’s 45 and Up Study [21]. Detailed methods for ascertaining the proportion of screening-eligible participants in the cohort were published previously [22] and are described in the Supplementary Appendix. Ethical approval for the 45 and Up Study was provided by the University of NSW Human Research Ethics Committee and specific approval for this analysis was provided by the NSW Population and Health Services Research Ethics Committee. Informed consent was obtained from all participants.
Lung cancer incidence, mortality and stage distribution
The total number of LC cases diagnosed (excluding over-diagnosed cases) was assumed to be equal in the screening and no-screening scenarios and was obtained by dividing the number of LC deaths by the conditional probability of LC death given a LC diagnosis (which was approximated as one minus the 5-year relative LC survival by age and sex observed in Australia in 2011 [23]). For the screening scenario, the number of diagnosed cases was multiplied by a constant factor to account for overdiagnosis (5.3% of all LC cases in the screening arm for NELSON and 1.9% for NLST, see Supplementary Appendix).
Hazard ratios of LC mortality according to the NLST and NELSON eligibility criteria compared to ‘never-smoking’ status were derived from the 45 and Up Study, using previously published methods [22, 24] and were used to estimate the number of LC deaths in each eligible sub-population by age, sex and smoking status (see Supplementary Appendix). The background LC mortality rate of ‘never-smoking’ status was calculated from LC mortality rates observed in Australia [23, 24] and the smoking prevalence obtained from our modelled estimates [18].
The Australian, age- and sex-specific distribution of LC cases by stage of disease at diagnosis was applied to cases in both scenarios, and then adjusted in the screening scenario by applying the stage shift observed in the trials; however, LC is often reported as “unknown stage” in Australia, thus these cases were re-classified as Stages I–IV based on observed survival rates (see Supplementary Appendix). Stage-specific LC relative survival was ascertained from the national database for cancers diagnosed 2012–2016 [23].
Costs
The average excess health-system costs of LC (compared to cancer-free controls) were estimated previously using the 45 and Up Study for the years 2006–2016 [25]. Costs in the year prior to diagnosis and an initial treatment cost were applied to all cases. For cases who survived, an additional cost for the continuing care phase was applied, while for cases who died, a fraction of the continuing care cost (depending on the mean survival time by stage) and a terminal care phase cost were applied.
The calculated “average case” costs to 3 years by phase, were obtained by applying 1, 2 and 3-year survival data by stage of disease (see Supplementary Appendix). For the base case, the average costs were extended to 5 years (see Table 1). Note that in the screening scenario, the excess costs in the year prior to diagnosis were expected to be lower than usual care [25], given that screening eliminates the costs of diagnosing symptoms. Regardless, our base case assumed the same average pre-diagnosis costs in both scenarios.
The base-case cost of a LDCT scan was the price listed in the Medicare Benefits Schedule (AU$302 undiscounted in 2021), and the average cost of a follow-up CT and non-CT false-positive work-up were estimated from the Queensland Lung Cancer Screening Study [26]. All costs were presented in 2021 Australian dollars (1 AUD–0.72 USD) (Table 1). A constant discount rate of 5% was applied annually to all future costs and benefits from the beginning of the screening phase.
Utility weights
SF-6D utility values were derived from sources using the SF-12. Baseline utilities for screening-eligible men and women were derived from the 45 and Up Study [27] (Table 1). A drop in utility of 0.01 was applied at age 70–79, and 0.04 at age 80+ years [28].
Evidence of a measurable effect on quality of life following a positive or negative screening result is inconclusive [29,30,31,32,33]. Nevertheless, we conservatively applied a small, temporary disutility for LC screening itself (0.02 for 2 weeks). The same disutility was applied for 3 months to those that required follow-up CT. False-positive results requiring diagnostic work-up were assumed to incur the same utility as Stage I LC for 3 months.
Previously published LC utility weights [34] applied across the entire survival period, and decreased with age in the same way as individuals without LC (Table 1).
Sensitivity analyses
One-way sensitivity analyses were undertaken to assess the single parameter uncertainty (see Supplementary Appendix), in which we varied assumptions regarding, the (1) screening mortality benefit observed in the trials; (2) relative risk of LC and all-cause mortality for individuals who were currently smoking or had quit smoking compared to those who never smoked; (3) costs of screening, LC diagnosis and treatment, and false positives, including a doubling and quadrupling of Stage IV total healthcare costs; (4) rate of false positives, follow-up CT scans, and overdiagnosis; (5) time horizon; (6) stage shift; (7) 5-year survival; (8) utility weights. Note that the mortality benefit is assumed to be an independent parameter in our model. Variations in the stage shift and 5-year survival had no influence on the mortality benefit (and thus on the LYs). The results of these variations should be interpreted as the effect that they have on the incremental cost and disutilities. The effect of stage shift on the LYs gained is indirectly captured by variations in the mortality benefit.
We also evaluated the effect of changing the eligibility criteria (i.e., changing the risk profile of the participants along with their LC mortality risk). We compared trial eligibility with selection criteria defined by the PLCOm2012 risk calculator [35] (PLCOm2012 ≥ 0.0151), and the USPSTF-2021 selection criteria [6]. The proportion eligible by age, sex, and smoking status was estimated from the 45 and Up Study cohort [22], and the LC death hazard ratio was estimated for sub-groups whose smoking status was ‘current’/‘former’- compared to ‘never’ for each selection criteria.
The combined parameter uncertainty throughout the model was evaluated with probabilistic sensitivity analysis (PSA) which simulated 10,000 possible ICER estimates by taking random values of all the model parameters (each independently) listed in Table 1 from each of the parameter distributions (except the time horizon and discount rate given that these are likely to be fixed, and the selection criteria) (see Supplementary Appendix).
We included an exploratory analysis investigating the effect of higher smoking cessation rates (by a factor of 1.2, 1.5 and 2) at every screening point among the participants in the screening scenario [36, 37], assuming a LC mortality benefit of 3% for each year since quitting [38, 39]. The last assumption underestimated the benefit of quitting since the all-cause mortality reduction was not included in this analysis. To maintain our conservative approach (i.e., less favourable for screening), we assumed the same (low) LC mortality benefit from quitting for both scenarios. The baseline cessation rates by age, sex and birth cohort were estimated using the Australian smoking behaviour model [18].
A threshold analysis on the cost of a LDCT screening scan was conducted using indicative willingness-to-pay thresholds of ~$30,000–$50,000 per QALY gained.
Results
In the base case, the incremental number of LYs/QALYs per person, over a lifetime, was 0.038 (95% CI, 0.018–0.049)/0.019 (95% CI, 0.006–0.030) given the NLST trial and 0.067 (95% CI, 0.028–0.096)/0.041 (95% CI, 0.016–0.063) for the NELSON trial. The average incremental cost per person was $1434 (95% CI, $903–2097) for the NLST and $1606 (95% CI, $802–2762) for the NELSON trial, resulting in ICERs of $38,250 (95% CI, $24,400–83,550; NLST) and $24,050 (95% CI, $ 11,900–64,500; NELSON) per LY gained or $76,300 (95% CI, $41,750–236,500; NLST) and $39,250 (95% CI, $18,150–108,300; NELSON) per QALY gained.
The results of the PSA are presented in Fig. 1. The probability that the NELSON setting was cost-effective, assuming a willingness-to-pay threshold of $30,000 or $50,000/QALY gained was 15% and 60%, respectively, while the probability for the NLST was 0.5% and 6.7%.
Of all the model parameters, variations in the screening-related LC mortality benefit observed in the trials had the largest effect on the ICER. ICERs ranged from $37,850–$277,950/QALY gained in the NLST-like simulation and $21,500–$104,350/QALY gained in the NELSON-like simulation when the LC mortality benefit approached the upper and lower 95% CI values, and when the benefit was assumed to decrease or continue after the trial (Fig. 2; incremental costs/LY Supplementary Fig. s4).
Variation in all other base-case parameters resulted in ICERs ranging from $53,350 to $115,500/QALY gained given the NLST trial and $30,300 to $51,650/QALY given the NELSON trial (see Table 2 and Fig. 3). Apart from the mortality benefit, among the parameters assessed, the LC mortality hazard ratio applied to eligible participants, disutilities related to screening, indeterminate and false-positive results, the cost per LDCT scan and the selection criteria had the greatest impact on the ICER (Fig. 3). The PLCOm2012 selection criteria was more cost-effective than both the base case and the USPSTF-2021 criteria (Table 2 and Fig. 3).
The incremental costs in both trial settings were largely dominated by the cost per screen (accounting for ~74% of the incremental cost). Varying the cost of a LDCT scan from $200 to $400, resulted in a ~±20% change in the ICER (NELSON: $30,300–$47,850; NLST: $60,300–$91,650/QALY gained). Assuming a willingness-to-pay threshold of $30,000-$50,000/QALY gained, screening was cost-effective in the base-case scenario when the cost of a LDCT scan was $7–$135 given the NLST trial and $196–$424 given the NELSON trial.
The total cost of LC/person was relatively similar in the screening and no-screening scenarios ($7060 vs. $6870 NLST base case; $7000 vs $6640 NELSON base case), and the impact of varying all treatment costs by a factor of 1/2 or 2 on the ICER was moderate (from 6 to 22%). Doubling the healthcare costs of Stage IV disease or reducing the pre-diagnosis cost in the screening scenario by 80% resulted in a slightly more favourable ICER (4–7% change). The effect of varying the average cost of a false positive by 20% was also small (less than 3%).
Varying the overdiagnosis factor between the upper and lower limits of the 95% confidence intervals had a minor effect on the ICER (up to 8% change).
The population estimate of 5-year LC survival in the model was used to estimate the number of LC cases. Varying this parameter (and therefore varying the number of LC cases) in the one-way sensitivity analysis resulted in minor changes in the ICER. The effect of increasing LC survival to reproduce the upper 95% confidence limit of the LC incidence reported in the AIHW, was slightly more significant in the NELSON trial, increasing the ICER estimate to $42,500/QALY gained.
Reducing the time horizon to 20 years increased the ICER results by ~15%. Further reducing the time horizon to 10 years increased the ICER by more than 100%, to $159,350/QALY gained given the NLST or $87,300 given the NELSON scenario.
Given hypothetical increases in smoking cessation rates in the screening scenario (by a factor of 1.2–2), the ICER decreased by 7–26% ($71,000–$56,900/QALY gained) based on NLST and 5–19% ($37,350–$31,850 /QALY gained) based on NELSON.
Discussion
We estimated the cost-effectiveness of LDCT screening for lung cancer to be $39,250 per QALY gained over a lifetime horizon by applying Australian costs and population-based lung cancer mortality and survival rates to the screening outcomes observed in the NELSON trial, using conservative assumptions for most parameters. The results obtained for the NLST setting were less favourable ($76,300/QALY gained) primarily because of the lower mortality benefit, which was the main driver of our model findings, and secondarily because of the higher rates of false positives. ICERs were extremely sensitive to the assumptions made regarding the lung cancer mortality benefit associated with screening during and after the active screening phase as observed in trials. Variation in this parameter resulted in the widest range of ICER values in one-way sensitivity analyses suggesting that cost-effectiveness of lung cancer screening in Australia is particularly contingent on achieving a mortality benefit that is at least equal to that observed in the trials. At an indicative ‘willingness-to-pay’ threshold in Australia of ~$30,000–$50,000, 15–60% of simulations in a probabilistic sensitivity analysis resulted in ICERs that could be considered cost-effective using NELSON-like screening parameters and outcomes.
This updated Australian evaluation for lung cancer screening is more favourable than previous Australian studies, including our 2018 evaluation which was based solely on the NLST setting [14]. Our NLST-like estimates of cost-effectiveness are more favourable in the current study due to a combination of the different time horizons used (lifetime vs 10 years), the population-derived LC mortality and survival rates used in this evaluation (as opposed to the trial rates used previously), and updated assumptions for other parameters. This updated evaluation is the first to incorporate Australian trends in smoking rates, which we simulated in a purpose-built, smoking prevalence forecasting model used to estimate both the number of Australians who currently smoke or have quit, and the competing risk of smoking-related all-cause mortality. We also incorporated updated, comprehensive health-system costs associated with lung cancer, estimated in a large population-based cohort study linked to routinely collected, administrative health databases [25].
A conservative approach was adopted in this analysis, reflected in several base-case assumptions. The first was that data on the cost of treating lung cancer did not capture immuno- and targeted therapies in use after 2016, which have substantially increased the cost of treating advanced and inoperable disease. Preliminary estimates suggest that the total healthcare costs for treating Stage IV lung cancer is almost twofold higher overall in 2021 compared to 2016 (noting that systemic therapy costs, which increased many-fold over this period, only account for a proportion of overall costs) [40]. Higher costs and lower survival associated with later stage disease are averted by screening, thereby potentially improving cost-effectiveness. In our analysis, doubling and quadrupling the total healthcare costs of Stage IV disease resulted in more favourable ICERs. However, even when quadrupling the total healthcare costs of Stage IV disease, variations in the cost of a LDCT scan had a large impact on the ICER. The cost of a LDCT scan could potentially be reduced in a large-scale screening programme, and our threshold analysis demonstrated that in the NELSON-like setting, lung cancer screening would be considered cost-effective in our base case if the scan price was set at $196, given a willingness-to-pay threshold of $30,000/QALY gained.
We conservatively assigned disutilities to the short-term psychological impact of screening and screening results, even though the evidence supporting a measurable effect on the utility scale following a positive or negative screening result is scarce. In the NLST and NELSON trial, there were no clinically relevant changes in quality-of-life detected in the SF-36 and SF-12 mental and physical component scores [29,30,31]. However, in the NELSON trial, the Impact of Event Scale (measuring lung cancer-specific distress) detected significant differences 2 months after a screening result [30, 31]. ICERs generated for the NLST-like setting were particularly sensitive to the degree of these disutilities, mainly due to the higher number of scans requiring follow-up CTs and further diagnostic work-up compared to the NELSON trial. Assigning zero disutilities in relation to screening and screening results, reduced the ICER in the NLST-like setting to from $76,300/QALY gained to $53,900. This implies that effective risk communication and access to appropriate support in relation to receipt of screening results is critical to reducing distress and improving cost-effectiveness. Additional conservative assumptions made in our base case included “no recovery” in quality of life for those diagnosed with lung cancer (i.e., the utility weights assigned at diagnosis were applied for the remainder of the survival period and corrected for age, resulting in a lower number of QALYs gained); and that eligible individuals who had quit smoking had the same all-cause mortality hazard ratio of those who were currently smoking (resulting in an increased number of deaths from other causes and in fewer QALYs gained).
Selecting a high-risk population is critical for optimising the balance of benefits and costs of a screening programme. In an exploratory analysis, we compared the results from two alternate selection criteria: the PLCOm2012 risk calculator and the USPSTF-2021 guidelines [6, 35]. PLCOm2012 is a lung cancer risk prediction model shown to yield a smaller number needed to screen to avert one lung cancer death compared to other criteria (i.e., NLST, NELSON, USPSTF) [41], and has been considered as an approach to define eligibility for a national targeted screening programme [12]. We estimated that selection of participants using a PLCOm2012 risk threshold of ≥1.51% was more cost-effective than the USPSTF-2021 criteria in both trial settings.
An exploratory analysis of smoking cessation, whereby higher smoking cessation rates were assumed in the screening scenario than the no-screening scenario, showed reductions in the ICER of 5–26%. However, we underestimated the costs of smoking cessation by assuming that screening itself had a positive effect on smoking cessation rates, without the additional cost of a cessation intervention. To maximise the benefits, targeted smoking cessation interventions may be, or are likely to be, necessary.
The screening input parameters of our model were closely related to the trial settings and so we did not have the flexibility to explore beyond these parameters. For example, recent lung cancer screening studies have reported more favourable stage shift distributions than the NLST and NELSON [42, 43], which will likely translate into better survival as well as averting the costs of treating inoperable disease. Furthermore, the mortality benefit that would accrue over long-term annual or biennial screens is potentially greater than what was observed in the trials and could result in a more favourable cost-effectiveness outcome for a full programme [44]. We could not simulate long-term annual or biennial screens directly because we modelled the mortality benefit as an independent parameter.
A potential limitation of our study was the assumption that LDCT screening had no effect on mortality from causes other than lung cancer. Specifically, we did not model actionable incidental findings [45,46,47]. Including incidental findings and the associated non-lung cancer mortality benefits may have had a favourable effect on mortality outcomes, however, the potential for overtreatment and complications in relation to these conditions would also need consideration. Similarly, we did not model adverse events, and in particular, fatal complications of diagnostic follow-up (although these are considered rare [3, 4]).
We also did not model variation in participation or screening adherence rates, both of which are key drivers of effectiveness and cost-effectiveness in national screening programmes. Further, the demographic profile of trial participants may not be representative of the eligible Australian population. The differential distribution of participants in the Australian population by characteristics known to be related to both lung cancer risk and screening participation, such as socioeconomic status, were not accounted for and may impact on screening implementation and effectiveness [48]. We also did not include any recruitment or programme overhead costs that would be needed for an equitable, population-based programme targeted at those who would obtain the greatest benefit, especially priority populations that may experience cultural, societal, psychological and/or physical barriers to participation [48].
Our results suggest that lung cancer screening with LDCT could be cost-effective in the Australian setting, dependent on achieving the mortality benefit observed in international trials. These findings contributed to a recent evaluation by the Australian Medical Services Advisory Committee, which in October 2022 recommended the establishment of a national screening programme in Australia. The effective implementation of a potential programme, and how well it is accepted and adopted by local health systems and high-risk communities, will be critical to its effectiveness and cost-effectiveness. If a national, risk-targeted lung cancer screening programme is rolled out in Australia, future economic evaluations using microsimulation models of the natural history of lung cancer to model beyond the direct evidence can be used to guide effective and cost-effective drivers of implementation success. Furthermore, updated evaluations can incorporate more contemporary data on improvements in lung cancer treatment, survival and quality of life as it becomes available, as well as potential variations in screening benefits by lung cancer histological sub-types.
Data availability
This research was completed using data collected through the 45 and Up Study (www.saxinstitute.org.au). The 45 and Up Study is managed by the Sax Institute in collaboration with major partner Cancer Council NSW; and partners: the Heart Foundation; NSW Ministry of Health; NSW Department of Communities and Justice; and Australian Red Cross Lifeblood. Data supporting the findings from this study are available from the Sax Institute, the NSW Department of Health, Cancer Institute NSW, and the Australian Bureau of Statistics, with data linkage conducted by the NSW Centre for Health Record Linkage (CHeReL; https://www.cherel.org.au). Restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, the 45 and Up Study is an open resource, accessible to any researcher upon application (https://www.saxinstitute.org.au/our-work/45-up-study/for-researchers/). All other data were obtained from publicly available sources online and previously published materials.
Code availability
The computer code used for the model is proprietary. The authors can be contacted for further details.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Luo Q, Steinberg J, O’Connell DL, Yu XQ, Caruana M, Wade S, et al. Lung cancer mortality in Australia in the twenty-first century: how many lives can be saved with effective tobacco control? Lung Cancer. 2019;130:208–15.
Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409.
de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382:503–13.
Moyer VA, U.S. Preventive Services Task Force. Screening for lung cancer: US preventive services task force recommendation statement. Ann Intern Med. 2014;160:330–8.
Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, et al. Screening for lung cancer: US preventive services task force recommendation statement. J Am Med Assoc. 2021;325:962–70.
Ngo PJ, Cressman S, Behar-Harpaz S, Karikios DJ, Canfell K, Weber MF. Applying utility values in cost-effectiveness analyses of lung cancer screening: a review of methods. Lung Cancer. 2022;04:122–31. 166
Cressman S, Peacock SJ, Tammemägi MC, Evans WK, Leighl NB, Goffin JR, et al. The cost-effectiveness of high-risk lung cancer screening and drivers of program efficiency. J Thorac Oncol. 2017;12:1210–22. https://doi.org/10.1016/j.jtho.2017.04.021
Hinde S, Crilly T, Balata H, Bartlett R, Crilly J, Barber P, et al. The cost-effectiveness of the Manchester ‘lung health checks’, a community-based lung cancer low-dose CT screening pilot. Lung Cancer. 2018;126:119–24.
Puggina A, Broumas A, Ricciardi W, Boccia S. Cost-effectiveness of screening for lung cancer with low-dose computed tomography: a systematic literature review. Eur J Public Health. 2016;26:168–75.
Ten Haaf K, Tammemägi MC, Bondy SJ, van der Aalst CM, Gu S, McGregor SE, et al. Performance and cost-effectiveness of computed tomography lung cancer screening scenarios in a population-based setting: a microsimulation modeling analysis in Ontario, Canada. PLoS Med. 2017;14:e1002225.
Cancer Australia. Report on the Lung Cancer Screening Enquiry. Surry Hills, NSW: Cancer Australia, 2020. https://www.canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/report-lung-cancer-screening-enquiry.
Manser R, Dalton A, Carter R, Byrnes G, Elwood M. Cost-effectiveness analysis of screening for lung cancer with low dose spiral CT (computed tomography) in the Australian setting. Lung Cancer. 2005;48:171–85.
Wade S, Weber M, Caruana M, Kang YJ, Marshall H, Manser R, et al. Estimating the cost-effectiveness of lung cancer screening with low-dose computed tomography for high-risk smokers in Australia. J Thorac Oncol. 2018;13:1094–105.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020.
RStudio Team. RStudio: integrated development environment for R. Boston, MA: RStudio, PBC; 2020.
National Lung Screening Trial Research Team. Lung cancer incidence and mortality with extended follow-up in the national lung screening trial. J Thorac Oncol. 2019;14:1732–42.
Wade S, Weber MF, Sarich P, Vaneckova P, Behar-Harpaz S, Ngo PJ, et al. Bayesian calibration of simulation models: a tutorial and an Australian smoking behaviour model. ar**v ar**v:220202923 [Preprint] 2022. Available from: https://arxiv.org/abs/2202.02923.
Vaneckova P, Wade S, Weber M, Murray JM, Grogan P, Caruana M, et al. Birth-cohort estimates of smoking initiation and prevalence in 20th century Australia: Synthesis of data from 33 surveys and 385,810 participants. PLoS ONE. 2021;16:e0250824.
Australian Bureau of Statistics. Population projections, Australia, 2017 (base) - 2066, Cat. No. 3222.0 [Internet]. 2018 [cited 2019 Nov 5]. https://www.abs.gov.au/AUSSTATS/abs@.nsf/productsbyCatalogue/5A9C0859C5F50C30CA25718C0015182F.
45 and Up Study Collaborators, Banks E, Redman S, Jorm L, Armstrong B, Bauman A, Beard J, et al. Cohort profile: the 45 and up study. Int J Epidemiol. 2008;37:941–7.
Weber M, Yap S, Goldsbury D, Manners D, Tammemagi M, Marshall H, et al. Identifying high risk individuals for targeted lung cancer screening: Independent validation of the PLCOm2012 risk prediction tool. Int J Cancer. 2017;141:242–53.
Australian Institute of Health and Welfare (AIHW) 2020 Cancer Data in Australia; Canberra: AIHW. https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/data.
Weber MF, Sarich PE, Vaneckova P, Wade S, Egger S, Ngo P, et al. Cancer incidence and cancer death in relation to tobacco smoking in a population-based Australian cohort study. Int J Cancer. 2021;149:1076–88.
Goldsbury DE, Weber MF, Yap S, Rankin NM, Ngo P, Veerman L, et al. Health services costs for lung cancer care in Australia: estimates from the 45 and Up Study. PLoS ONE. 2020;15:e0238018.
Marshall HM, Finn N, Bowman RV, Passmore LH, McCaul EM, Yang IA, et al. Cost of screening for lung cancer in Australia. Intern Med J. 2019;49:1392–9.
Ngo PJ, Wade S, Vaneckova P, Behar-Harpaz S, Caruana M, Cressman S, et al. Health utilities for participants in a population-based sample who meet eligibility criteria for lung cancer screening. Lung Cancer. 2022;169:47–54.
Ngo PJ, Wade S, Banks E, Karikios DJ, Canfell K, Weber MF. Large-scale population-based surveys linked to administrative health databases as a source of data on health utilities in Australia. Value Health. 2022;S1098-3015:00195–4.
Gareen IF, Duan F, Greco EM, Snyder BS, Boiselle PM, Park ER, et al. Impact of lung cancer screening results on participant health-related quality of life and state anxiety in the National Lung Screening Trial. Cancer. 2014;120:3401–9.
van den Bergh KA, Essink-Bot ML, Borsboom GJ, Th Scholten E, Prokop M, de Koning HJ, et al. Short-term health-related quality of life consequences in a lung cancer CT screening trial (NELSON). Br J Cancer. 2010;102:27–34.
van den Bergh KA, Essink‐Bot ML, Bunge EM, Scholten ET, Prokop M, van Iersel CA, et al. Impact of computed tomography screening for lung cancer on participants in a randomized controlled trial (NELSON trial). Cancer. 2008;113:396–404.
Mazzone PJ, Obuchowski N, Fu AZ, Phillips M, Meziane M. Quality of life and healthcare use in a randomized controlled lung cancer screening study. Ann Am Thorac Soc. 2013;10:324–9.
Toumazis I, Tsai EB, Erdogan SA, Han SS, Wan W, Leung A, et al. Cost-effectiveness analysis of lung cancer screening accounting for the effect of indeterminate findings. JNCI Cancer Spectrum. 2019;3:pkz035.
Tramontano AC, Schrag DL, Malin JK, Miller MC, Weeks JC, Swan JS, et al. Catalog and comparison of societal preferences (utilities) for lung cancer health states: results from the Cancer Care Outcomes Research and Surveillance (CanCORS) study. Med Decis Mak. 2015;35:371–87.
Tammemägi MC, Katki HA, Hocking WG, Church TR, Caporaso N, Kvale PA, et al. Selection criteria for lung-cancer screening, published correction appears in N Engl J Med. 2013 Jul 25;369:394]. N Engl J Med. 2013;368:728–36.
Moldovanu D, de Koning HJ, van der Aalst CM. Lung cancer screening and smoking cessation efforts. Transl Lung Cancer Res. 2021;10:1099–109.
Pedersen JH, Tønnesen P, Ashraf H. Smoking cessation and lung cancer screening. Ann Transl Med. 2016;4:157.
Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ. 2000;321:323–9.
Tanner NT, Kanodra NM, Gebregziabher M, Payne E, Halbert CH, Warren GW, et al. The association between smoking abstinence and mortality in the national lung screening trial. Am J Respir Crit Care Med. 2016;193:534–41.
Ngo PJ. Lung cancer control in the immunotherapy era: meeting the need for data. PhD thesis. The University of Sydney; 2021.
Lam S, Tammemagi M. Contemporary issues in the implementation of lung cancer screening. Eur Respir Rev. 2021;30:200288.
Tammemagi MC, Schmidt H, Martel S, McWilliams A, Goffin JR, Johnston MR, et al. Participant selection for lung cancer screening by risk modelling (the Pan-Canadian Early Detection of Lung Cancer [PanCan] study): a single-arm, prospective study. Lancet Oncol. 2017;18:1523–31. https://doi.org/10.1016/S1470-2045(17)30597-1.
Balata H, Ruparel M, O’Dowd E, Ledson M, Field JK, Duffy SW, et al. Analysis of the baseline performance of five UK lung cancer screening programmes. Lung Cancer. 2021;161:136–40. https://doi.org/10.1016/j.lungcan.2021.09.012.
Lew JB, Greuter MJ, Caruana M, He E, Worthington J, St John DJ, et al. Validation of microsimulation models against alternative model predictions and long-term colorectal cancer incidence and mortality outcomes of randomized controlled trials. Med Decis Mak. 2020;40:815–29.
Bartlett EC, Belsey J, Derbyshire J, Morris K, Chen M, Addis J, et al. Implications of incidental findings from lung screening for primary care: data from a UK pilot. npj Prim Care Respir Med. 2021;31:36.
Tsai EB, Chiles C, Carter BW, Godoy MC, Shroff GS, Munden RF, et al. Incidental findings on lung cancer screening: significance and management. Semin Ultrasound CT MR. 2018;39:273–81.
Morgan L, Choi H, Reid M, Khawaja A, Mazzone PJ. Frequency of incidental findings and subsequent evaluation in low-dose computed tomographic scans for lung cancer screening. Ann Am Thorac Soc. 2017;14:1450–6.
Rankin NM, McWilliams A, Marshall HM. Lung cancer screening implementation: complexities and priorities. Respirology. 2020;25:5–23. https://doi.org/10.1111/resp.13963.
Acknowledgements
We thank the many thousands of people participating in the 45 and Up Study. We also acknowledge the role of the Australian Institute of Health and Welfare in collecting and providing access to other data described.
Funding
This work is part of the Cancer-Patient Population Projections project (Cancer-PPP) funded by a Medical Research Future Fund (MRFF) Preventive and Public Health Research Initiative: 2019 Target Health System and Community Organisation Research Grant Opportunity, No. MRF1200535. KF is supported by NHMRC/MRFF; HM is supported by NHMRC/MRFF and Metro North HHS. KC is supported by NHMRC. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
SBH: conceptualisation, methodology, software, formal analysis, writing—original draft preparation, writing—review & editing; MFW: conceptualisation, writing—original draft, writing—review & editing, supervision, project administration and funding acquisition; SW: conceptualisation, methodology, software, data curation, writing—review and editing and funding acquisition; PJN: conceptualisation, data curation, writing—review & editing; PV: writing—review and editing; PS: writing—review and editing; SC: conceptualisation, methodology, writing—review and editing; MCT: conceptualisation, methodology, writing—review and editing; KF: writing—review and editing and funding acquisition; HM: writing—review and editing; AM: writing—review & editing; JZ: writing—review and editing and funding acquisition; MC: conceptualisation, methodology, writing—review and editing, supervision, project administration and funding acquisition; KC: conceptualisation, writing—review and editing, supervision and funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. KC is co-PI of an investigator-initiated trial of cervical screening, Compass, run by the VCS Foundation, which is a government-funded not-for-profit charity; the VCS Foundation has received equipment and a funding contribution from Roche Molecular Diagnostics. She is also co-PI on a major investigator-initiated implementation programme, Elimination of Cervical Cancer in the Western Pacific (ECCWP) which will receive support from the Minderoo Foundation, the Frazer Family Foundation and equipment donations from Cepheid Inc. Neither KC nor her institution on her behalf receives direct funding from industry for any project. KC’s research is supported via a National Health and Research Council Australia Leadership Fellowship (NHMRC; APP1194679). KC chairs and participates in a number of advisory committees to government and not-for-profit agencies; no committee participation for commercial companies. MC is an investigator on an investigator-initiated trial of cytology and primary HPV screening in Australia (‘Compass’) (ACTRN12613001207707 and NCT02328872), which is conducted and funded by the VCS Foundation a government-funded not-for-profit charity. The VCS Foundation has received equipment and a funding contribution for the Compass trial from Roche Molecular Systems. However, neither MC nor his institution on his behalf (The Daffodil Centre, a joint venture between Cancer Council NSW and The University of Sydney) receive direct or indirect funding from industry for Compass Australia or any other project. MW received an honorarium from scientific meeting organisers for a presentation outside the submitted work. MCT developed the PLCOm2012 lung cancer risk prediction model, which is assessed in this study. The model is open access and is available free of charge to non-commercial users. For commercial users, licensing has been assigned to Brock University. MCT has not received any money for the use of the PLCOm2012 model and does not anticipate any payments in the future. KF received travel support from various medical or scientific meeting organisers for participating or being a speaker (or both) and received additional grants or contracts from Olympus and Australian MRFF Next Generation Clinical Researchers Programme and MeVis Medical Solutions AG/HealthInc; and payment or honoraria for lectures, presentations, and speaker’s bureaus from Willey Cochrane Clinical Answers and is the Chair for Lung Cancer Consultative Group (unpaid) and a Council member.
Ethics approval and consent to participate
Ethical approval for the conduct of the 45 and Up Study was provided by the University of New South Wales Human Research Ethics Committee. Ethical approval for the present study was provided by the NSW Population & Health Services Research Ethics Committee (14/CIPHS/54). Individuals gave written informed consent to take part in the study, including consent for follow-up through repeated data collection and linkage of their data to population health databases. The study was performed in accordance with the Declaration of Helsinki.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Behar Harpaz, S., Weber, M.F., Wade, S. et al. Updated cost-effectiveness analysis of lung cancer screening for Australia, capturing differences in the health economic impact of NELSON and NLST outcomes. Br J Cancer 128, 91–101 (2023). https://doi.org/10.1038/s41416-022-02026-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-02026-8
- Springer Nature Limited