Abstract
Treatment-resistant depression (TRD) affects approximately 2.8 million people in the U.S. with estimated annual healthcare costs of $43.8 billion. Deep brain stimulation (DBS) is currently an investigational intervention for TRD. We used a decision-analytic model to compare cost-effectiveness of DBS to treatment-as-usual (TAU) for TRD. Because this therapy is not FDA approved or in common use, our goal was to establish an effectiveness threshold that trials would need to demonstrate for this therapy to be cost-effective. Remission and complication rates were determined from review of relevant studies. We used published utility scores to reflect quality of life after treatment. Medicare reimbursement rates and health economics data were used to approximate costs. We performed Monte Carlo (MC) simulations and probabilistic sensitivity analyses to estimate incremental cost-effectiveness ratios (ICER; USD/quality-adjusted life year [QALY]) at a 5-year time horizon. Cost-effectiveness was defined using willingness-to-pay (WTP) thresholds of $100,000/QALY and $50,000/QALY for moderate and definitive cost-effectiveness, respectively. We included 274 patients across 16 studies from 2009–2021 who underwent DBS for TRD and had ≥12 months follow-up in our model inputs. From a healthcare sector perspective, DBS using non-rechargeable devices (DBS-pc) would require 55% and 85% remission, while DBS using rechargeable devices (DBS-rc) would require 11% and 19% remission for moderate and definitive cost-effectiveness, respectively. From a societal perspective, DBS-pc would require 35% and 46% remission, while DBS-rc would require 8% and 10% remission for moderate and definitive cost-effectiveness, respectively. DBS-pc will unlikely be cost-effective at any time horizon without transformative improvements in battery longevity. If remission rates ≥8–19% are achieved, DBS-rc will likely be more cost-effective than TAU for TRD, with further increasing cost-effectiveness beyond 5 years.
Similar content being viewed by others
Introduction
Neuropsychiatric disorders are a major cause of morbidity and mortality worldwide, yet treatment options for many of these conditions are limited in their specificity and long-term efficacy. Major depressive disorder (MDD), in particular, has an estimated annual prevalence of 8.3% among US adults [1] and is the leading cause of disability as well as death from suicide, globally [2, 3]. MDD is characterized by the presence of a persistently depressed mood and/or anhedonia, as well as a number of debilitating somatic and psychological symptoms [4]. Clinical severity is measured using a variety of questionnaires, including the Hamilton Depression Rating Scale (HDRS) [5] and the Montgomery-Åsberg Depression Rating Scale (MADRS) [6]. The treatment of MDD is complicated by its multifactorial nature, high degree of comorbidity, and phenotypic heterogeneity [7].
Conventional treatment for MDD consists of psychotherapy and pharmacotherapy, but a significant proportion (up to 30%) of patients fail to respond to these treatment modalities [8]. While the definition of treatment-resistant depression (TRD) has not been standardized [9], patients whose symptoms do not adequately improve after multiple treatment trials are classified as having TRD [10, 11]. TRD is associated with increased health care costs, reduced quality of life (QoL), high rates of unemployment, and high suicidality [12]. The poor prognosis and limited recourse for patients with TRD demonstrates a need for the development of new therapeutic methods.
In the last decade, more targeted treatment approaches that modulate specific networks in the brain have emerged as promising therapeutic candidates for decreasing symptom burden and improving QoL in individuals with TRD. In some developed countries, additional treatment options for TRD now include transcranial magnetic stimulation (TMS), electroconvulsive therapy (ECT), and vagus nerve stimulation (VNS). These non-invasive (TMS, ECT) and invasive (VNS) neurmodulatory treatments have been shown to be highly effective and even reduce medical costs for TRD [13,14,15]. However, some patients with depression do not attain meaningful improvement even with these additional therapies. Deep brain stimulation (DBS) is a neurosurgical intervention that involves stereotactically implanting electrodes to deliver continuous, yet adjustable, electrical stimulation to specific anatomic targets in the brain. The procedure has gained FDA approval for movement disorders, epilepsy, and obsessive-compulsive disorder, but is still experimental for TRD. Several DBS targets for TRD have been studied, including the subcallosal cingulate (SCC) [16,17,18,19,20,21], nucleus accumbens (NAcc) [22, 23], ventral capsule/ventral striatum (VC/VS) or anterior limb of the internal capsule (ALIC) [24,25,26], bed nucleus of the stria terminalis (BNST) [27, 28], and medial forebrain bundle (MFB) [29,30,31]. Although open-label trials showed encouraging response rates (20–92%), two randomized-controlled trials (RCTs) [17, 32] were aborted by their industry sponsors out of concern that they would fail to demonstrate effectiveness relative to sham stimulation. Developments in targeting strategies since these trials have demonstrated significant promise in more recent open-label studies [33, 34] and a pivotal new industry-sponsored RCT is being planned with FDA breakthrough therapy designation [35].
As this therapy is further investigated, it is worth considering its potential position within the health economic marketplace. We therefore used existing literature to conduct a cost-effectiveness analysis (CEA) of DBS compared to treatment-as-usual (TAU) for TRD. This CEA is unique in that DBS for TRD is not yet approved or commonly utilized, so our analyses determined effectiveness thresholds that would need to be demonstrated by future trials in order for the therapy to be cost-effective should it receive FDA approval. Specifically, we calculated the remission rates necessary to achieve acceptable incremental cost-effectiveness ratios (ICER) relative to TAU and propose future improvements that could increase its cost-effectiveness.
Methods
Using a decision analytic model [36, 37], we compared DBS to TAU, which was defined as maintenance antidepressant medication (with or without augmentation therapies) along with concomitant non-pharmacologic treatments (i.e. psychotherapy, TMS, and/or ECT). Our base case for the model is an adult (age 22–70) diagnosed with a severe major depressive episode (HDRS-17 ≥ 18 or MADRS > 22), who has received at least 2 years of TAU without treatment response. Since patients who are eligible for DBS represent a particularly severe form of TRD, we chose to follow more thorough criteria for treatment-resistance compared to the standard definition including: lack of antidepressant response to 1) at least 3 medications from 3 different classes, 2) an adequate course of psychotherapy (>6 weeks), and 3) an adequate trial (>6 bilateral sessions) of ECT. The time horizon is 5 years following DBS, as is typical for novel surgical cost-effectiveness analyses [38, 39]. All model inputs were derived from a retrospective review of relevant literature.
Literature review – efficacy
A PubMed search to identify clinical trials establishing the efficacy of DBS for TRD was conducted using the following terms: “Deep Brain Stimulation” AND “Treatment Resistant” AND “Depression” AND “Trial”. The search was completed in March 2023. We selected studies with original patient data that had at least 1 year of follow-up with response, remission, and complication rates and excluded any studies that were not either patient-blinded, sham-controlled, or included target-optimization. Open-label trials with fewer than 3 patients were also excluded. Data collected from selected studies included study design, patient inclusion/exclusion criteria, sample size, patient sex, patient age, follow-up time, patient-level pre-operative HDRS-17 or MADRS scores, 12- and 24-month post-operative HDRS-17 or MADRS scores, response/remission criteria, response/remission rates, and complication rates.
We presumed that the probability of remission from TAU in our model patients would be particularly low, given the rigorous eligibility criteria for classification as extremely treatment-resistant and for consideration as a neurosurgical candidate. In the patient sample we analyzed, for example, the average duration of TRD was approximately 20 years without clinical benefit, making spontaneous remission highly unlikely. However, in an effort to make as rigorous a model as possible, we sought to include some non-zero probability in the TAU treatment arm. As such, we conducted a general search of the literature for longitudinal studies (≥5 years follow-up) focusing on outcomes of patients with TRD on TAU [40,41,42].
Complications
Serious adverse events were limited to those related to DBS and were divided into three categories based on management strategy: lead revision/replacement, implantable pulse generator (IPG) revision/replacement, and short-hospitalization (e.g., 3–7 days for infection, skin erosion, etc.). Only complications that significantly added to costs or detracted from effectiveness were considered for our model, so self-limited complications were not included. No complications were considered for the TAU arm as these would fall into the self-limited category and would not affect model outputs.
Effectiveness – the utility model
Utility is a quantitative measure of a patient’s subjective improvement in QoL and ranges from 1 (perfect health) to 0 (death). In cost-effectiveness analyses, effectiveness is calculated by multiplying the net gain in utility by the duration (in years). The product is reported in quality-adjusted life-years (QALYs), where 1 QALY equals 1 year in perfect health [43]. Because the HDRS and MADRS are not designed to specifically measure QoL, and due to the paucity of available QoL data in our selected studies, we employed a utility model. Using published utility values for remission and non-remission in TRD [44], remission status was converted to a utility value for each patient in our sample and averaged to reflect mean QoL after treatment. A separate disutility value from the literature was assigned to complications to approximate the negative impact of post-operative DBS complications on QoL [45].
Cost
We conducted our analysis from both healthcare sector and societal perspectives. The healthcare sector approach accounts for all monetary costs of healthcare associated with an intervention (DBS or TAU), regardless of who bears the cost: the third-party payer (i.e., Medicare), the hospital, or the patient (out-of-pocket expenses). It does not consider costs of transportation, patient and caregiver time, productivity loss, or non-monetary costs—all of which are instead included in the societal perspective. While the societal perspective was previously considered the gold standard for cost-effectiveness analyses, recommendations from the Second Panel on Cost-Effectiveness in Health and Medicine have moved to include analyses from two perspectives [46]. Additionally, we created separate models to account for the varying costs of DBS using non-rechargeable (DBS-pc) versus rechargeable (DBS-rc) devices. While there was considerable variability between specific protocols, most of our selected studies used DBS-pc at initial implantation and switched patients to DBS-rc at the first IPG replacement. To estimate cost-effectiveness with this combined approach, we ran additional analyses using costs of DBS-pc with one battery replacement for the first 18 months and DBS-rc for the following 42 months.
The aggregate cost of DBS was defined as a sum of the cost of one pre-operative assessment, one pre-operative magnetic resonance imaging (MRI), one pre- and one post-operative computed tomography (CT), one bilateral stereotactic DBS lead and neurostimulator device implantation procedure, fifty-four follow-up programming office visits, and any hospital (facility) fees or additional out-of-pocket expenses. Additionally, the 5-year cost for DBS-pc included three IPG replacements. Costs associated with TAU included costs of pharmacotherapy (e.g. selective serotonin reuptake inhibitors [SSRIs], serotonin-norepinephrine reuptake inhibitors [SNRIs], tricyclic antidepressants, monoamine oxidase inhibitors, atypical antipsychotics, esketamine), cognitive-behavioral therapy (CBT), and TMS or ECT with a wide range and standard error to account for variability in individual treatment plans. Under the assumption that most remitters with either DBS or TAU would remain on some form of pharmacological therapy while discontinuing additional neuromodulation therapies, we defined a separate variable for the cost of pharmacotherapy alone and designated it as an incremental cost each year after remission. All cost data, including costs associated with complications, were collected from the 2023 Centers for Medicare & Medicaid Services (CMS) Physician Fee Schedule (based on HCPCS/CPT codes) [47] and from published health economics literature [48,49,50,51,52,53,54,55,56,57,58,59,60].
Decision analytic model
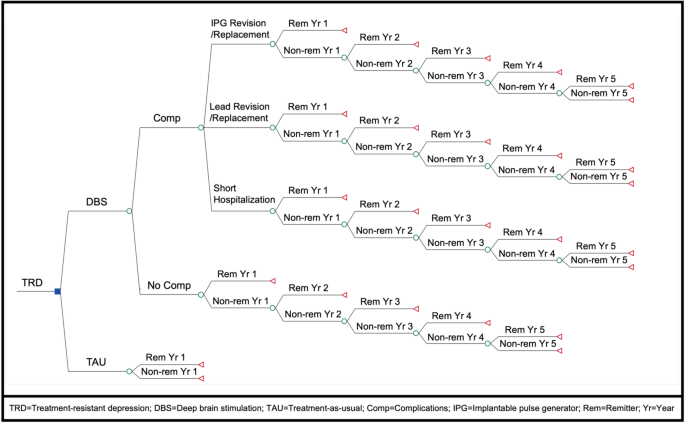
We created our model using TreeAge Pro Healthcare 2023 (TreeAge Software, Williamstown, MA). The model placed patients in one of two treatment arms: DBS or TAU. Patients undergoing DBS had the opportunity to become remitters at 1, 2, 3, 4, and 5 years. The 5-year time horizon was chosen to capture the longer-term trajectory of DBS treatment response in our patient sample, including an initial 6–12 month optimization phase, 1–3 years of varying response, and a period of follow-up beyond 3 years with relatively sustained remission rates (see Fig. 1 for the time to remission in our analyzed sample). When a DBS patient remitted, their subsequent incremental cost per year after surgery transitioned from the costs of TAU to the cost of pharmacotherapy alone. Those who did not respond to DBS within the first year remained on TAU, thus accumulating the costs of TAU for each year of non-remission in addition to the initial costs of DBS. On the other hand, patients on TAU alone were given 1 year to remit. This decision was made based on prior studies, which showed that ~80–90% of patients with MDD who recover with TAU do so within the first 2 years of initiating treatment [61,62,63,64,65], with earlier response (typically within the first 4 weeks of initial treatment) predicting positive treatment outcomes [66, 67]. Previous prospective studies found that after 5 years, the probability of MDD recovery with each additional year is only between 2% and 15% [40, 68]. In TRD patients, particularly the severely treatment-resistant population eligible for DBS, the likelihood of response to TAU is inevitably even lower with each passing year [41, 69].
For DBS patients, all post-operative complications throughout the 5-year treatment period were assigned prior to year 1 on the model for simplicity. By extension, costs and disutilities associated with complications were factored into final calculations once and did not accumulate over time. For both treatment arms, there was no incremental utility or disutility for continuing as a non-remitter, as the utility of non-remission was applied to those who failed to remit at the end of each treatment arm. Finally, mortality rate was not considered in our model given the relatively short time horizon and negligible added mortality risk of either treatment [70,71,72,73,74,75].
Analysis
We analyzed our model using TreeAge Pro Healthcare 2023 (TreeAge Software, Williamstown, MA). To account for uncertainty and variability, model inputs were parametrized using pooled means and standard deviations, and a Monte Carlo (MC) simulation (n = 100,000) was performed. We examined the primary model output, the incremental cost-effectiveness ratio (ICER), using a willingness-to-pay (WTP) threshold approach. The ICER ($/QALY) is calculated by dividing incremental cost – the difference in net cost ($) between two treatment arms – by incremental effectiveness – the difference in QALYs gained between two treatment arms. Based on current accepted definitions of cost-effectiveness, unequivocal cost-effectiveness was considered an ICER less than $0/QALY, definitive cost-effectiveness was achieved at less than $50,000/QALY, moderate cost-effectiveness between $50,000 and $100,000/QALY, and cost-ineffectiveness at greater than $100,000/QALY gained [76]. Results of the MC simulation were further analyzed using both probabilistic and deterministic sensitivity analyses. Finally, using one-way sensitivity analyses, we analyzed the minimum 1-year remission rate necessary to achieve cost-effectiveness at each WTP threshold.
Results
Literature review
Our PubMed search yielded 76 initial results (see Fig. 2 for our PRISMA [77] flowchart). From the 16 studies selected for data collection (published 2009–2021), we found a total of 274 unique patients who underwent DBS for TRD [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Six additional studies (three narrative reviews [25, 78, 79] and three systematic reviews and meta-analyses [80,81,82]) were used to cross-reference data and eliminate duplicates. Across all patients, mean baseline (pre-operative) MADRS and HDRS-17 scores were 34.09 (±5.11) and 23.68 (±3.96), respectively. Based on the established remission criteria of MADRS score ≤10 or HDRS-17 score ≤7, overall remission rate was 24.2% at 1 year (n = 260). Mean follow-up time was 33.17 (±26.65) months. Using observed-case analysis from studies that included long-term follow-up data, remission rates were 23.7% at 2 years (n = 177), 40% at 3 years (n = 60), 33.3% at 4 years (n = 39), and 36.7% at 5 years (n = 30). Comprehensive outcomes and complications data from our systematic review can be found in Table 1.
Decision analytic model
For an overview of our completed model, see Fig. 3. All base case model inputs and distributions are included in Table 2. The average 5-year cost of DBS-rc, which included one pre-operative office visit ($167.40), one pre-operative MRI ($160.63), one pre-operative and one post-operative CT ($81.34), electrodes and neurostimulator device ($2,731.31), IPG implant ($20,378.78), estimated hospital fees ($2,607.00), and post-operative follow-up ($3,397.59) was $29,524.05 (±$817.66). The average 5-year cost of DBS-pc, which included all of the same costs as DBS-rc plus 3 IPG replacements ($91,042.80), was $120,566.85 (±$817.66). The standard deviation represents the variability in hospital fees and number of follow-up programming visits required (other values in this calculation are fixed and based on Medicare reimbursement amounts). Estimated costs from complications were $27,066.84 (lead revision/replacement), $30,347.60 (IPG revision/replacement), and $13,035.00 (short hospitalization). Mean yearly cost of TAU, which was calculated as the average of either psychotherapy and medications alone ($7,721.84), psychotherapy and medications with ECT ($17,097.84) and psychotherapy and medications with ECT and TMS ($23,277.84) was $16,032.51 (±$7,832.53) from a healthcare sector perspective and $38,575.86 (±$5,722.14) from a societal perspective. The annual cost of pharmacotherapy alone was $1,576 (±$1,174.00). Using published utility scores [44], we included the following utility values in our model: 0.84 (±0.15) for remission, and 0.54 (±0.25) for non-remission.
MC simulation
Based on the results of our MC simulation (n = 100,000), after 5 years DBS-pc was less cost-effective than TAU from both healthcare sector (ICER = $254,719.81/QALY) and societal (ICER = $178,949.98/QALY) perspectives. DBS-rc, however, was definitively more cost-effective than TAU from a healthcare sector perspective (ICER = $31,878.61/QALY) and unequivocally more cost-effective than TAU from a societal perspective (ICER = −$43,924.23/QALY). See Table 3 for a summary of cost-effectiveness rankings. A combined approach (DBS-pc switched to DBS-rc at first IPG replacement) was just shy of being moderately more cost-effective than TAU (ICER = $105,831.71/QALY) from the healthcare sector perspective and was definitively more cost-effective than TAU (ICER = $30,195.12/QALY) from the societal perspective.
Net cost for TAU over 5 years was approximately $79,500.00 from the healthcare sector perspective and $191,000.00 from the societal perspective. Net cost of DBS-pc over 5 years was $183,529.00 from the healthcare sector perspective and $264,039.00 from the societal perspective. Net cost of DBS-rc over 5 years was $92,549.00 from the healthcare sector perspective and $173,065.00 from the societal perspective. Net effectiveness of DBS over 5 years was 3.12 QALYs, compared to 2.71 QALYs for TAU. The incremental effectiveness of DBS was therefore 0.41 QALYs.
Sensitivity analyses
Using probabilistic sensitivity analysis, outputs from the MC simulation were plotted on cost-effectiveness acceptability curves (Fig. 4). MC simulation revealed that TAU was more cost-effective than DBS-pc (Fig. 4A) in 100% (at $50,000/QALY) and 100% (at $100,000/QALY) of iterations from the healthcare sector perspective and in 100% (at $50,000/QALY) and 97% (at $100,000/QALY) of iterations from the societal perspective. Conversely, DBS-rc (Fig. 4B) was more cost-effective than TAU in 72.8% (at $50,000/QALY) and 100% (at $100,000/QALY) of iterations from the healthcare sector perspective and in 100% (at $50,000/QALY) and 100% (at $100,000/QALY) of iterations from the societal perspective.
Show results from Monte Carlo simulation (n = 100,000) and probabilistic sensitivity analysis. For DBS-pc (A), the TAU (red) curves dominate the DBS (blue) curves. TAU is thus shown to be more cost-effective than DBS-pc in 100% of iterations from both the healthcare sector (dark red) and societal sector (light red) perspectives at $50,000/QALY. For DBS-rc (B), the DBS (blue) curves dominate the TAU (red) curves. DBS-rc is thus shown to be more cost-effective than TAU in 72.8% of iterations from the healthcare sector perspective (dark blue) and 100% of iterations from the societal sector perspective (light blue) at $50,000/QALY. The black vertical line marks the broadly-accepted WTP threshold of $50,000 per QALY.
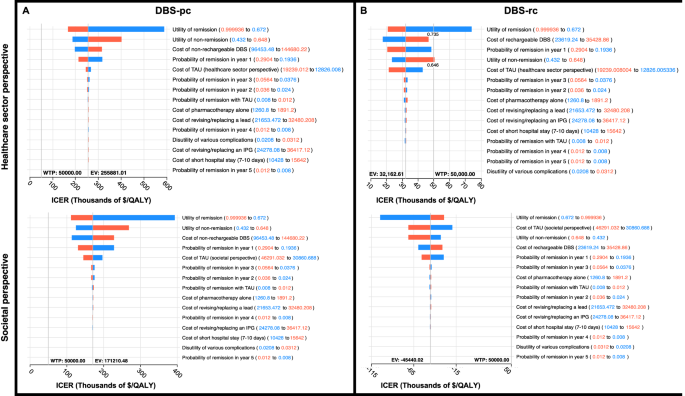
Using 1-way sensitivity analyses, we determined the minimum 1-year remission rates needed to achieve acceptable ICERs at WTP thresholds of $50,000 (for definitive cost-effectiveness) and $100,000 (for moderate cost effectiveness) per QALY (Fig. 5). DBS-pc (Fig. 5A) requires 55% remission for moderate cost-effectiveness and 85% remission for definitive cost-effectiveness from a healthcare sector perspective. From a societal perspective, DBS-pc requires 35% and 46% remission for moderate and definitive cost-effectiveness, respectively. DBS-rc (Fig. 5B) requires 11% and 19% remission for moderate and definitive cost-effectiveness, respectively, from a healthcare sector perspective. From a societal perspective, DBS-rc requires 8% and 10% remission for moderate and definitive cost-effectiveness, respectively. A combined approach (DBS-pc switched to DBS-rc at first IPG replacement) requires 26% and 41% remission for moderate and definitive cost-effectiveness, respectively, from a healthcare sector perspective. From a societal perspective, DBS with this approach requires 16% and 21% remission for moderate and definitive cost-effectiveness, respectively.
Show minimum 1-year remission rates necessary for DBS for TRD to achieve acceptable incremental cost-effectiveness ratios (ICER) at accepted willingness-to-pay (WTP) thresholds of $50,000 (for moderate cost-effectiveness) and $100,000 (for definitive cost-effectiveness) per QALY. DBS-pc (A) requires 55% remission for moderate cost-effectiveness and 85% remission for definitive cost-effectiveness from a healthcare sector perspective (dark blue), and 35% remission for moderate cost-effectiveness and 46% remission for definitive cost-effectiveness from a societal perspective (light blue). DBS-rc (B) requires 11% remission for moderate cost-effectiveness and 19% remission for definitive cost-effectiveness from a healthcare sector perspective (dark blue), and 8% remission for moderate cost-effectiveness and 10% remission for definitive cost-effectiveness from a societal perspective (light blue).
Finally, deterministic sensitivity analyses were used to create tornado diagrams (Fig. 6) that illustrate the effects of varying each parametrized input in our decision analytic model on the overall ICER for non-rechargeable (Fig. 6A) and rechargeable (Fig. 6B) DBS for TRD, from both healthcare sector and societal perspectives. All costs, probabilities, and utilities were varied within sensitivity ranges 20% above and below mean values. For all four scenarios, the parameter (with sensitivity ranges) that had the greatest impact on ICER variance was utility of remission (0.67 to 0.99). Other parameters with the greatest impact for all four scenarios included: utility of non-remission (0.43 to 0.65), cost of DBS ($96,453.48 to $144,680.22 for non-rechargeable; $23,619.24 to $35,428.86 for rechargeable), probability of remission in year 1 (0.19 to 0.29), and cost of TAU ($12,826.01 to $19,239.01 for the healthcare sector perspective; $30,860.69 to $46,291.03 for the societal perspective). For utility of remission, cost of TAU, and probability of remission in year 1, lower values increased the ICER. Conversely, for utility of non-remission and cost of DBS, higher values increased the ICER.
Displays the effect of varying each parametrized input on the ICER for DBS with non-rechargeable (A) and rechargeable (B) devices from both the healthcare sector (top) and societal sector (bottom) perspectives. All costs, probabilities, and utilities were varied within a sensitivity range 20% above and below mean values. Red bars show the impact of an increase and blue bars show the impact of a decrease in the variable value on overall ICER.
Importantly, none of the parameters in any of the scenarios affected the ICER in a way that impacted the cost-effectiveness of DBS at a WTP threshold of $100 K. Only in the scenario of DBS-rc from the healthcare sector perspective, a utility of remission lower than 0.735 and a utility of non-remission above 0.648 would increase the ICER beyond a WTP threshold of $50 K. Based on previously published literature [44], the lower limit for utility of remission was 0.76, while the upper limit for utility of non-remission was 0.58, so these parameter values would be outside the expected range and are unlikely to impact our cost-effectiveness results. Overall, DBS-pc did not reach cost-effectiveness compared to TAU, while DBS-rc remained cost-effective compared to TAU (from both healthcare sector and societal perspectives) under a broad range of cost and effectiveness values.
Discussion
This study, which to our knowledge is the first economic evaluation comparing DBS to TAU for TRD, shows that regardless of economic perspective, DBS-pc would not be more cost-effective than TAU. However, with a 1-year remission rate of at least 20%, DBS-rc would be more cost-effective than TAU for TRD, particularly when considering the large societal costs of TRD. With a mean 1-year remission of 24.2% in our sample, DBS-rc had a higher probability of being cost-effective, even despite having higher upfront costs compared to TAU from either economic perspective. From a healthcare sector perspective, under the broadly accepted WTP threshold of $50,000/QALY, DBS-rc had a 72.8% probability of being cost-effective after 5 years, reaching 100% probability of cost-effectiveness at a WTP of $100,000/QALY. From a societal perspective, DBS-rc had a 100% probability of being cost-effective after 5 years at both WTP thresholds.
As this is the first cost-effectiveness study of DBS for TRD, there are no directly comparable analyses, however the cost-effectiveness of DBS for non-psychiatric indications has been explored in several studies. In a cost-utility analysis of DBS vs long-term medical management for Parkinson’s disease, Dams et al. [83] found the average 5-year cost of treatment with DBS to be €67,374.12 (~$75,693.81) with an average 5-year incremental cost-utility ratio (ICUR) of €36,065.82/QALY (~$40,483.70/QALY) from a healthcare provider perspective, adapted to 2023 values. It is likely that the total DBS costs presented in that study are lower than those we used for DBS-pc because battery replacement costs were only included every 4 years, rather than every 1.5 years as in our study. DBS battery depletion is assumed to be quicker in TRD due to the higher amplitudes typically required for TRD than for Parkinson’s disease [84], but if battery life for non-rechargeable IPGs can be extended to 4 years or more, it is likely that the cost-effectiveness of DBS-pc would increase substantially.
Chan et al. [85] compared the cost-effectiveness of DBS vs. VNS for patients with refractory epilepsy and found the cost of DBS over 5 years to be €72,251 (~$81,129.93) with an expected effectiveness of 3.42 QALYs (5-year ICER = €21,126.02, ~$23,728.53) from a healthcare sector perspective. In this study, the authors also only accounted for costs of IPG replacement every 5 years (compared to 1.5 years in our study) and used response (defined as ≥50% reduction in seizure frequency) rather than remission status as the primary outcome, resulting in both lower costs and higher effectiveness for DBS-pc. As previously discussed, a longer battery life would improve the cost-effectiveness of DBS-pc for any indication. While we chose to employ remission as a more stringent outcome metric, it is likely that the threshold for cost-effectiveness of DBS for TRD would also be lower if response (defined as ≥50% reduction in symptom severity) was considered instead.
Growing evidence has suggested the potential of DBS for treating other highly debilitating and costly medical conditions such as chronic pain, obesity, and dementia, with several clinical trials now underway [86]. Mahajan et al. [38] examined the cost-effectiveness of DBS compared to laparoscopic Roux-en-Y gastric bypass (LRYGB) for obesity using a societal perspective and calculated the overall 5-year cost of DBS to be $29,951. While the study did not specify between rechargeable and non-rechargeable devices, this value is very similar to our average 5-year cost of $29,524.05 for DBS-rc.
DBS has been used off-label for a variety of other psychiatric conditions including Tourette’s, bipolar disorder, post-traumatic stress disorder, eating disorders, and substance use disorders, yet economic evaluations have been limited by low case numbers and lack of published clinical trial data. Taking a societal perspective and using Medicare reimbursement as a proxy for direct costs, Kuijper et al. [39] conducted a threshold and cost-effectiveness analysis of DBS compared to contingency management for cocaine use disorder. The 1-year cost of DBS-rc for cocaine use disorder was calculated to be $27,988.45, which is very close to our 1-year cost of DBS-rc at $28,071.09.
Finally, cost-effectiveness analyses of DBS vs TAU for treatment-resistant obsessive-compulsive disorder (TROCD) offer perhaps the most relevant comparison for our findings. Separate studies from Ooms et al. [87] and Moon et al. [88] both compared the cost-effectiveness of DBS vs TAU for patients with TROCD. While each of these models were applied to countries outside of the United States (the Netherlands, Korea, and the U.K.) and used different time horizons (4, 10, and 2 years) as well as different effect measures (area under the curve analysis and response status) than our study, their results are nonetheless informative and allow for a reasonable comparison of direct and indirect costs. Ooms et al. [87]. found the cost of DBS-pc (including battery changes every 14 months) over 4 years to be €127,112.74 from a societal perspective. Moon et al. [88] found the cost of DBS-pc over 10 years (including battery replacements every 3 years) to be $44,672 in Korea and $42,322 in the U.K., from a healthcare payer perspective. In the former study, the costs for DBS-pc are very close to those in our study, likely due to a similar frequency of battery replacements. In the latter study, a lower frequency (every 3 years) and substantially lower cost ($2,232 in Korea and $760 in the U.K.) of battery replacements account for the overall lower costs of DBS-pc compared to our findings. The longer time horizon of 10 years in the Moon et al. [88] study highlights the increasing cost-effectiveness of DBS over time relative to TAU. Unlike Parkinson’s patients, those receiving DBS for psychiatric conditions are relatively young with fewer surgical risk factors [72, 89, 90] and therefore have a longer time horizon to benefit from DBS treatment. Extending the time horizon for economic analyses of DBS for psychiatric indications would better capture the true cost-effectiveness of this intervention. Relatedly, the area under the curve (AUC) approach for measuring antidepressant effect over time in the Ooms et al. [87] study may better capture overall symptom improvement throughout the course of treatment and is likely more representative of the patient’s subjective gain in QoL [31]. While our selected studies lacked sufficient patient-level QoL data for this approach, this method of calculating QALYs would improve future economic evaluations and underscores the need to include QoL measures in clinical trials.
Considering the lack of consistency in reported costs for DBS across multiple indications, our study highlights the need for greater public access to healthcare economics data. Though societal costs are highly variable and difficult to estimate, and exact healthcare costs may not be readily accessible in a complex system such as that in the U.S., accurate cost data are nonetheless imperative for future cost-effectiveness analyses to capture the full economic burden of disease. Ideally, in addition to safety and efficacy data, large prospective trials would collect cost and utility data across multiple institutions to account for cost differences. For DBS, in particular, it is important for studies to also provide patient-level data on specific stimulation targets and parameters, as well as effects on battery life to most accurately compare costs and efficacy across studies. This approach would enable more generalizable conclusions, and results of these studies would influence medical decision making not only at the physician and patient levels, but also for hospital administrators, insurance companies, and government healthcare programs such as Medicare and Medicaid [91]. Despite promising preliminary results for multiple conditions, public acceptance of and insurance coverage for surgical treatment of psychiatric illness is still disproportionately lower than for other non-psychiatric indications [92,93,94]. As the field of psychiatric neurosurgery develops, there is a growing need for high-quality cost-effectiveness analyses.
It is important to remember that TRD patients who meet eligibility criteria for DBS are a smaller percentage of all patients with TRD, as they must have also failed to respond to additional treatments such as augmentation strategies with ketamine and non-invasive neuromodulation. Furthermore, considering the high incidence of treatment-resistance in MDD and the low probability of response to TAU after 3 years in this population, it is possible that the criteria for surgical treatment of TRD are overly stringent in terms of disease duration. At least 5 years since MDD onset is commonly required for DBS eligibility, but there is evidence that it would be reasonable to enroll patients sooner, as long as they have significant symptom severity and have proven to be treatment-refractory (multiple failed SSRIs, adjunctive medication trials, CBT, and either TMS or ECT). Multiple studies have found that longer duration of untreated disease is a major prognostic factor for poor treatment response and worse long-term outcomes [95,96,97,98]. Compared to MDD, TRD patients utilize twice the number of outpatient healthcare resources, triple the number of inpatient stays, and have 23% higher all-cause mortality [99]. Additionally, rates of intentional self-harm and suicide are significantly higher in TRD [100], further increasing the risk of negative outcomes in these refractory patients while they wait to fulfill DBS eligibility criteria. Thus, continued TAU may unnecessarily prolong suffering with severe disease and simultaneously increase cost burden to patients, caregivers, healthcare systems, and society at large. Given these results, earlier treatment of TRD with DBS may be both clinically and economically more effective.
With rising incidence and high rates of untreated depression [101, 102], the economic impact of TRD on society at large cannot be overstated. In addition to decreased quality of life, higher healthcare resource utilization, and increased all-cause mortality for patients themselves [12], TRD also has a wide sphere of impact on others including family members, caregivers, and employers [103]. Mrazek et al. [49]. found that the societal burden of major depressive disorder for the United States in 2012 was $188 billion-- $57 billion dollars more than the societal cost of cancer and $15 billion dollars more than that of diabetes. Providing new cost-effective treatment options to patients with TRD would provide substantial benefit in diminishing not only their TRD-related healthcare costs, but also other non-TRD healthcare costs, while also allowing them to return to work and reengage in society in meaningful ways. According to society preferences, willingness-to-pay is higher for patients with a higher level of disease, younger age, and larger QOL gains [104]. Since TRD patients have a high disease burden, are relatively young in age, and benefit from substantial increases in QOL with remission, raising WTP thresholds in accordance to society preferences would make DBS for TRD more cost-effective even with higher total costs and lower remission rates. As new treatments for highly prevalent and debilitating conditions like TRD become available and their safety is established, the economic threshold for their approval should be adjusted in the broader context of societal impact.
Several important limitations apply to this study. One limitation was the high variability of TAU costs between patients. These costs vary widely depending on the specific combination of medications, psychotherapy, TMS, and ECT that any given patient may be using prior to DBS, as well as on the high variability in costs attributed to transportation, lost productivity, and healthcare utilization unrelated to depression for each patient. To account for this variability, we included very large standard deviations for these parameters.
Second, we chose to only include remission and non-remission as outcomes, as response rates likely do not accurately reflect meaningful patient outcomes due to the arbitrary nature of a 50% reduction criterium and high rates of return to non-response status [31]. Further, it is unlikely that a single utility value could accurately represent the range in QoL changes associated with varying levels of treatment response. For refractory illnesses, such as TRD, it is likely that even small sub-threshold reductions in symptoms could still provide considerable improvement in QoL. As such, response status may likely underestimate effectiveness and therefore inflate ICERs.
Additionally, we did not include relapse as a possible outcome in our model, though up to 80% of TRD patients experience relapse within 5 years of response despite continued maintenance treatment [63, 105,106,107]. Remission, on the other hand, is the ideal outcome of depression treatment with a low risk of relapse [108,109,110]. Thus, we assumed that remitters in either treatment arm would remain remitters for the duration of the model. This was supported by previous literature and the data reported in our selected studies. Although most patients in our sample who achieved remission with DBS did so by year 3, we still included non-zero probability for remission with DBS in years 4 and 5, the same as was used to represent a non-zero probability of remission with TAU. This small but non-zero value reflects stability of remission status in either treatment arm. Nevertheless, it is possible that some patients, particularly those with residual symptoms, would relapse despite remission [111, 112]. Due to a lack of longitudinal data on residual symptoms or utility values associates with these symptoms, it is impossible to include these variables in this analysis. While considerably more complex, a Markov model that accounts for patient response, relapse, and remission at each year of the decision tree could more fully account for every possible outcome in depression treatment and would allow for a more thorough analysis. At this time, a paucity of detailed individual patient-level data reflecting the transitions between these outcomes limits the feasibility of accurately using such an approach.
Third, our utility model is based on prior prospective cohort studies and cost-effectiveness analyses that collected direct measures of health-related quality-of-life (HRQoL) scores and health utilities. Thus, utilities associated with remission status and disutilities associated with complications are indirect derivations for our cohort and should be interpreted as approximations of true utility. Importantly, two main sources from which utility values in these studies were derived are based on MDD [113, 114]. For TRD, the transition from non-remission to remission is likely associated with an even greater improvement in health utility, so our utility values are likely conservative. Further, we assumed that non-remission in this context did not necessarily mean non-response, so we included a wider range of values for our estimate—from severe depression (~0.2–0.55) on the lower end to response without remission (0.67–0.72) on the higher end [44]. As there is no prior literature defining the disutility of DBS complications in TRD specifically, we assumed that the disutility of complications related to DBS would be similar across psychiatric disorders. Clinical trials for TRD should move to include direct measures of QoL (e.g., EQ-5D, SF-36, etc.) in addition to standard efficacy measures (e.g., HDRS, MADRS, etc.) to assess for these potential differences between indications and ensure that future health economics studies have sufficient data to support more generalizable claims of cost-effectiveness.
Our 5-year time horizon restricts complications to those occurring up to 60 months after surgery. In our aggregate sample, this captured greater than 99% of all complications. Previous work has found that the majority of DBS-related complications occur within the first 5 years and complication rates with DBS do not increase in the long-term [115, 116]. While recent reports have published outcomes of DBS for TRD for up to 8 years of follow-up, we found that available data were still insufficient to carry the model past 5 years without adding significant uncertainty. Additionally, there was significant variation in the timepoint of the last observation (range = 0.50–142.92 months) where such an analysis would inappropriately represent the efficacy of DBS treatment and the confidence interval would be much too large for meaningful interpretation. As more data become available, it will be important to assess cost-effectiveness with this additional efficacy and complication information in the long-term. In our study, we assumed a non-staged approach for initial implantation and that all complications occurred after initial implantation for model simplicity. Although we did not include the probability of additional post-operative complications for each IPG replacement, it is important to note that non-rechargeable devices incur extra costs, not only for the new IPG itself, but also for the associated surgical procedure, hospitalization, and any post-operative complications, such as infection or hemorrhage, which further increase the incremental cost of DBS-pc each year.
Finally, though there is a well-documented risk of suicidality in TRD patients, this outcome was not included in our model for several reasons. First, estimates of the monetary cost or specific disutility associated with either suicidal ideation or suicide attempt (e.g., emergency psychiatric hospitalization, medication changes, intensive inpatient therapy, various medical and neurologic sequelae, etc.) are limited by lack of available data. Second, while 11% (n = 29) of patients in our DBS sample experienced suicidality and 4% (n = 12) completed suicide, there is no evidence to support that these adverse events were directly related to DBS. Suicide is unfortunately common in TRD, regardless of treatment approach, so it was assumed that any additional costs incurred due to suicide would be the same for each treatment arm and would therefore not affect the model.
Conclusion
While the efficacy of DBS for TRD has not yet been definitively established, prior studies report remission rates of approximately 25–45% [20, 21, 26, 32, 80, 81, 107, 117,118,119,120,121]. From our analyses, DBS-pc is unlikely to be cost-effective compared to TAU even at remission rates at the higher end of this range. DBS-rc, however, would only need remission rates in the 10–20% range to reach cost-effectiveness compared to TAU. Based on outcomes from 274 patients with TRD across 16 studies showing an average 1-year remission rate of 24.2%, we found that DBS with a rechargeable device would be more cost-effective than treatment as usual for treatment-resistant depression, under a range of possible cost and effectiveness values.
DBS with rechargeable devices is particularly well suited for psychiatric indications. Patients report increased satisfaction with rechargeable IPGs [122], psychiatric indications require high amplitude stimulation settings for treatment compared to other DBS conditions and therefore more quickly deplete battery life [84], and the longer time horizon of treatment in these relatively young patients allows for the extended benefits of DBS to outweigh high upfront costs. Our analyses show that an approach of initial implantation with a non-rechargeable device and subsequent transition to a rechargeable IPG in patients who experience response at the time of first battery replacement would reach both moderate and definitive cost-effectiveness at 5 years, with increasing cost-effectiveness each following year.
Our results demonstrate that, using current estimates of treatment efficacy, DBS with rechargeable devices for TRD already represents a cost-effective approach compared to current treatments. As DBS strategies continue to improve, so will justification for its use as an effective treatment for patients with TRD.
References
Major Depression [Internet]. National Institute of Mental Health (NIMH). Available from: https://www.nimh.nih.gov/health/statistics/major-depression
Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317:1517.
World Health Organization. Mental and behavioural disorders team. Preventing suicide: a resource for primary health care workers [Internet]. World Health Organization; 2000. Report No.: WHO/MNH/MBD/00.4. Available from: https://apps.who.int/iris/handle/10665/67603
American psychiatric association and american psychiatric association - 2013 diagnostic and statistical manual of mental disorders (2013).
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9.
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, et al. Major depressive disorder. Nat Rev Dis Prim. 2016;2:1–20.
Voineskos D, Daskalakis ZJ, Blumberger DM. Management of treatment-resistant depression: challenges and strategies. Neuropsychiatr Dis Treat. 2020;16:221–34.
Keller MB. Issues in treatment-resistant depression. J Clin Psychiatry. 2005;66 Suppl 8:5–12.
Al-Harbi KS. Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence. 2012;6:369–88.
Warden D, Rush AJ, Trivedi MH, Fava M, Wisniewski SR. The STAR*D Project results: a comprehensive review of findings. Curr Psychiatry Rep. 2007;9:449–59.
Johnston KM, Powell LC, Anderson IM, Szabo S, Cline S. The burden of treatment-resistant depression: a systematic review of the economic and quality of life literature. J Affect Disord. 2019;242:195–210.
Noda Y, Miyashita C, Komatsu Y, Kito S, Mimura M. Cost-effectiveness analysis comparing repetitive transcranial magnetic stimulation therapy with antidepressant treatment in patients with treatment-resistant depression in Japan. Psychiatry Res. 2023;330:115573.
Fitzgibbon KP, Plett D, Chan BCF, Hancock-Howard R, Coyte PC, Blumberger DM. Cost–utility analysis of electroconvulsive therapy and repetitive transcranial magnetic stimulation for treatment-resistant depression in Ontario. Can J Psychiatry. 2020;65:164–73.
Cohen LJ, Allen JC Jr. Estimating the potential savings with vagus nerve stimulation for treatment-resistant depression: a payer perspective*. Curr Med Res Opin. 2008;24:2203–17.
Ramasubbu R, Clark DL, Golding S, Dobson KS, Mackie A, Haffenden A, et al. Long versus short pulse width subcallosal cingulate stimulation for treatment-resistant depression: a randomised, double-blind, crossover trial. Lancet Psychiatry. 2020;7:29–40.
Crowell AL, Riva-Posse P, Holtzheimer PE, Garlow SJ, Kelley ME, Gross RE, et al. Long-term outcomes of subcallosal cingulate deep brain stimulation for treatment-resistant depression. AJP. 2019;176:949–56.
Merkl A, Aust S, Schneider GH, Visser-Vandewalle V, Horn A, Kühn AA, et al. Deep brain stimulation of the subcallosal cingulate gyrus in patients with treatment-resistant depression: a double-blinded randomized controlled study and long-term follow-up in eight patients. J Affect Disord. 2018;227:521–9.
Holtzheimer PE, Husain MM, Lisanby SH, Taylor SF, Whitworth LA, McClintock S, et al. Subcallosal cingulate deep brain stimulation for treatment-resistant depression: a multisite, randomised, sham-controlled trial. Lancet Psychiatry. 2017;4:839–49.
Puigdemont D, Pérez-Egea R, Portella MJ, Molet J, de Diego-Adeliño J, Gironell A, et al. Deep brain stimulation of the subcallosal cingulate gyrus: further evidence in treatment-resistant major depression. Int J Neuropsychopharmacol. 2012;15:121–33.
Kennedy SH, Giacobbe P, Rizvi SJ, Placenza FM, Nishikawa Y, Mayberg HS, et al. Deep brain stimulation for treatment-resistant depression: follow-up after 3 to 6 years. Am J Psychiatry. 2011;168:502–10.
Millet B, Jaafari N, Polosan M, Baup N, Giordana B, Haegelen C, et al. Limbic versus cognitive target for deep brain stimulation in treatment-resistant depression: accumbens more promising than caudate. Eur Neuropsychopharmacol. 2014;24:1229–39.
Bewernick BH, Kayser S, Sturm V, Schlaepfer TE. Long-term effects of nucleus accumbens deep brain stimulation in treatment-resistant depression: evidence for sustained efficacy. Neuropsychopharmacol. 2012;37:1975–85.
Hitti FL, Cristancho MA, Yang AI, O’Reardon JP, Bhati MT, Baltuch GH. Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression: a decade of clinical follow-up. J Clin Psychiatry. 2021;82:37487.
van der Wal JM, Bergfeld IO, Lok A, Mantione M, Figee M, Notten P, et al. Long-term deep brain stimulation of the ventral anterior limb of the internal capsule for treatment-resistant depression. J Neurol Neurosurg Psychiatry. 2020;91:189–95.
Malone DA, Dougherty DD, Rezai AR, Carpenter LL, Friehs GM, Eskandar EN, et al. Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol Psychiatry. 2009;65:267–75.
Fitzgerald PB, Segrave R, Richardson KE, Knox LA, Herring S, Daskalakis ZJ, et al. A pilot study of bed nucleus of the stria terminalis deep brain stimulation in treatment-resistant depression. Brain Stimul. 2018;11:921–8.
Raymaekers S, Luyten L, Bervoets C, Gabriëls L, Nuttin B. Deep brain stimulation for treatment-resistant major depressive disorder: a comparison of two targets and long-term follow-up. Transl Psychiatry. 2017;7:e1251–e1251.
Coenen VA, Bewernick BH, Kayser S, Kilian H, Boström J, Greschus S, et al. Superolateral medial forebrain bundle deep brain stimulation in major depression: a gateway trial. Neuropsychopharmacol. 2019;44:1224–32.
Fenoy AJ, Schulz PE, Selvaraj S, Burrows CL, Zunta-Soares G, Durkin K, et al. A longitudinal study on deep brain stimulation of the medial forebrain bundle for treatment-resistant depression. Transl Psychiatry. 2018;8:1–11.
Bewernick BH, Kayser S, Gippert SM, Switala C, Coenen VA, Schlaepfer TE. Deep brain stimulation to the medial forebrain bundle for depression- long-term outcomes and a novel data analysis strategy. Brain Stimul. 2017;10:664–71.
Dougherty DD, Rezai AR, Carpenter LL, Howland RH, Bhati MT, O’Reardon JP, et al. A randomized sham-controlled trial of deep brain stimulation of the ventral capsule/ventral striatum for chronic treatment-resistant depression. Biol Psychiatry. 2015;78:240–8.
Riva-Posse P, Choi KS, Holtzheimer PE, Crowell AL, Garlow SJ, Rajendra JK, et al. A connectomic approach for subcallosal cingulate deep brain stimulation surgery: prospective targeting in treatment-resistant depression. Mol Psychiatry. 2018;23:843–9.
Riva-Posse P, Crowell AL, Wright K, Waters AC, Choi K, Garlow SJ, et al. Rapid antidepressant effects of deep brain stimulation and their relation to surgical protocol. Biol Psychiatry. 2020;88:e37–9.
Abbott receives FDA’s breakthrough device designation to explore use of deep brain stimulation to manage severe depression [internet]. abbott media room. Available from: https://abbott.mediaroom.com/2022-07-12-Abbott-Receives-FDAs-Breakthrough-Device-Designation-to-Explore-Use-of-Deep-Brain-Stimulation-to-Manage-Severe-Depression
Grutters JPC, Joore MA, van der Horst F, Stokroos RJ, Anteunis LJC. Decision-analytic modeling to assist decision making in organizational innovation: the case of shared care in hearing aid provision. Health Serv Res. 2008;43:1662–73.
Najera RA, Gregory ST, Shofty B, Anand A, Gadot R, Youngerman BE, et al. Cost-effectiveness analysis of radiosurgical capsulotomy versus treatment as usual for treatment-resistant obsessive-compulsive disorder. J Neurosurg. 2022;138:347–57.
Mahajan UV, Ojukwu DI, Azagury DE, Safer DL, Cunningham T, Halpern CH. Can responsive deep brain stimulation be a cost-effective treatment for severe obesity? Obes (Silver Spring). 2022;30:338–46.
Kuijper FM, Mahajan UV, Ku S, Barbosa DAN, Alessi SM, Stein SC, et al. Deep brain stimulation compared with contingency management for the treatment of cocaine use disorders: a threshold and cost-effectiveness analysis. Neuromodulation. 2022;25:253–62.
Keller MB, Lavori PW, Mueller TI, Endicott J, Coryell W, Hirschfeld RMA, et al. Time to recovery, chronicity, and levels of psychopathology in major depression: a 5-year prospective follow-up of 431 subjects. Arch Gen Psychiatry. 1992;49:809–16.
Aaronson ST, Sears P, Ruvuna F, Bunker M, Conway CR, Dougherty DD, et al. A 5-year observational study of patients with treatment-resistant depression treated with vagus nerve stimulation or treatment as usual: comparison of response, remission, and suicidality. AJP. 2017;174:640–8.
Gronemann FH, Jorgensen MB, Nordentoft M, Andersen PK, Osler M. Incidence of, risk factors for, and changes over time in treatment-resistant depression in denmark: a register-based cohort study. J Clin Psychiatry. 2018;79:21247.
Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276:1253–8.
Hannah LA, Walsh CM, Jopling L, Perez J, Cardinal RN, Cameron RA Economic evaluation of interventions for treatment-resistant depression: a systematic review. Front Psychiatry. 2023;14:1056210.
Kumar KK, Appelboom G, Lamsam L, Caplan AL, Williams NR, Bhati MT, et al. Comparative effectiveness of neuroablation and deep brain stimulation for treatment-resistant obsessive-compulsive disorder: a meta-analytic study. J Neurol Neurosurg Psychiatry. 2019;90:469–73.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316:1093.
CMS 2019 medicare physician fee schedule [Internet]. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files-Items/RVU19A
Sussman M, O’sullivan AK, Shah A, Olfson M, Menzin J. Economic burden of treatment-resistant depression on the U.S. health care system. J Manag Care Spec Pharm. 2019;25:823–35.
Mrazek DA, Hornberger JC, Altar CA, Degtiar I. A review of the clinical, economic, and societal burden of treatment-resistant depression: 1996-2013. Psychiatr Serv. 2014;65:977–87.
Ross EL, Zivin K, Maixner DF. Cost-effectiveness of electroconvulsive therapy vs pharmacotherapy/psychotherapy for treatment-resistant depression in the United States. JAMA Psychiatry. 2018;75:713–22.
Voigt J, Carpenter L, Leuchter A. Cost effectiveness analysis comparing repetitive transcranial magnetic stimulation to antidepressant medications after a first treatment failure for major depressive disorder in newly diagnosed patients – a lifetime analysis. PLOS ONE. 2017;12:e0186950.
Amos TB, Tandon N, Lefebvre P, Pilon D, Kamstra RL, Pivneva I, et al. Direct and indirect cost burden and change of employment status in treatment-resistant depression: a matched-cohort study using a US commercial claims database. J Clin Psychiatry. 2018;79:5360.
Olfson M, Amos TB, Benson C, McRae J, Marcus SC. Prospective service use and health care costs of medicaid beneficiaries with treatment-resistant depression. JMCP. 2018;24:226–36.
Olchanski N, McInnis Myers M, Halseth M, Cyr PL, Bockstedt L, Goss TF, et al. The economic burden of treatment-resistant depression. Clin Ther. 2013;35:512–22.
Taneja C, Papakostas GI, **g Y, Baker RA, Forbes RA, Oster G. Cost-effectiveness of adjunctive therapy with atypical antipsychotics for acute treatment of major depressive disorder. annals of pharmacotherapy. 2012;46:642–49.
Ivanova JI, Birnbaum HG, Kidolezi Y, Subramanian G, Khan SA, Stensland MD. Direct and indirect costs of employees with treatment-resistant and non-treatment-resistant major depressive disorder. Curr Med Res Opin. 2010;26:2475–84.
Teresa B, Gibson P, Yonghua **g P, Ginger Smith Carls P, Edward Kim MD, Erin Bagalman J, et al. Cost burden of treatment resistance in patients with depression. Am J Manag Care. 2010;16:370–7.
Russell JM, Hawkins K, Ozminkowski RJ, Orsini L, Crown WH, Kennedy S, et al. The cost consequences of treatment-resistant depression. J Clin Psychiatry. 2004;65:341–7.
Corey-Lisle PK, Birnbaum HG, Greenberg PE, Claxton AJ. Identification of a claims data. J Clin Psychiatry. 2002;63:8441.
Russell WHCJM. The impact of treatment-resistant depression on health care utilization and costs. J Clin Psychiatry. 2002;63:8690.
Keller MB, Shapiro RW, Lavori PW, Wolfe N. Recovery in major depressive disorder: analysis with the life table and regression models. Arch Gen Psychiatry. 1982;39:905–10.
Kennedy N, Abbott R, Paykel ES. Longitudinal syndromal and sub-syndromal symptoms after severe depression: 10-year follow-up study. Br J Psychiatry. 2004;184:330–6.
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. AJP. 2006;163:1905–17.
Verduijn J, Verhoeven JE, Milaneschi Y, Schoevers RA, van Hemert AM, Beekman ATF, et al. Reconsidering the prognosis of major depressive disorder across diagnostic boundaries: full recovery is the exception rather than the rule. BMC Med. 2017;15:215.
Rush AJ, Warden D, Wisniewski SR, Fava M, Trivedi MH, Gaynes BN, et al. STAR*D. CNS Drugs. 2009;23:627–47.
Beard JIL, Delgadillo J. Early response to psychological therapy as a predictor of depression and anxiety treatment outcomes: a systematic review and meta-analysis. Depress Anxiety. 2019;36:866–78.
Henkel V, Seemüller F, Obermeier M, Adli M, Bauer M, Mundt C, et al. Does early improvement triggered by antidepressants predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord. 2009;115:439–49.
Mueller TI, Keller MB, Leon AC, Solomon DA, Shea MT, Coryell W, et al. Recovery after 5 years of unremitting major depressive disorder. Arch Gen Psychiatry. 1996;53:794–9.
Dunner DL, Rush AJ, Russell JM, Burke M, Woodard S, Wingard P, et al. Prospective, long-term, multicenter study of the naturalistic outcomes of patients with treatment-resistant depression. J Clin Psychiatry. 2006;67:15790.
Kennedy SH, Lam RW. Enhancing outcomes in the management of treatment resistant depression: a focus on atypical antipsychotics. Bipolar Disord. 2003;5:36–47.
O’Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry. 2007;62:1208–16.
Saleh C, Fontaine D. Deep brain stimulation for psychiatric diseases: what are the risks? Curr Psychiatry Rep. 2015;17:33.
Tørring N, Sanghani SN, Petrides G, Kellner CH, Østergaard SD. The mortality rate of electroconvulsive therapy: a systematic review and pooled analysis. Acta Psychiatr Scand. 2017;135:388–97.
Watts BV, Peltzman T, Shiner B. Mortality after electroconvulsive therapy. Br J Psychiatry. 2021;219:588–93.
Voges J, Waerzeggers Y, Maarouf M, Lehrke R, Koulousakis A, Lenartz D, et al. Deep-brain stimulation: long-term analysis of complications caused by hardware and surgery—experiences from a single centre. J Neurol Neurosurg Psychiatry. 2006;77:868–72.
ICER_2020_2023_VAF_013120-4-2.pdf [Internet]. Available from: https://icer.org/wp-content/uploads/2021/03/ICER_2020_2023_VAF_013120-4-2.pdf
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Roet M, Boonstra J, Sahin E, Mulders AEP, Leentjens AFG, Jahanshahi A. Deep brain stimulation for treatment-resistant depression: towards a more personalized treatment approach. J Clin Med. 2020;9:2729.
Dandekar MP, Diaz AP, Rahman Z, Silva RH, Nahas Z, Aaronson S, et al. A narrative review on invasive brain stimulation for treatment-resistant depression. Braz J Psychiatry. 44:317–30.
Zhou C, Zhang H, Qin Y, Tian T, Xu B, Chen J, et al. A systematic review and meta-analysis of deep brain stimulation in treatment-resistant depression. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018;82:224–32.
Wu Y, Mo J, Sui L, Zhang J, Hu W, Zhang C, et al. Deep brain stimulation in treatment-resistant depression: a systematic review and meta-analysis on efficacy and safety. Front Neurosci. 2021;15:655412.
Hitti FL, Yang AI, Cristancho MA, Baltuch GH. Deep brain stimulation is effective for treatment-resistant depression: a meta-analysis and meta-regression. J Clin Med. 2020;9:2796.
Dams J, Siebert U, Bornschein B, Volkmann J, Deuschl G, Oertel WH, et al. Cost-effectiveness of deep brain stimulation in patients with Parkinson’s disease. Mov Disord. 2013;28:763–71.
van Riesen C, Tsironis G, Gruber D, Klostermann F, Krause P, Schneider GH, et al. Disease-specific longevity of impulse generators in deep brain stimulation and review of the literature. J Neural Transm. 2016;123:621–30.
Chan HY, Wijnen BFM, Majoie MHJM, Evers SMAA, Hiligsmann M. Economic evaluation of deep brain stimulation compared with vagus nerve stimulation and usual care for patients with refractory epilepsy: a lifetime decision analytic model. Epilepsia. 2022;63:641–51.
Harmsen IE, Elias GJB, Beyn ME, Boutet A, Pancholi A, Germann J, et al. Clinical trials for deep brain stimulation: current state of affairs. Brain Stimul. 2020;13:378–85.
Ooms P, Blankers M, Figee M, Bergfeld IO, van den Munckhof P, Schuurman PR, et al. Cost-effectiveness of deep brain stimulation versus treatment as usual for obsessive-compulsive disorder. Brain Stimul. 2017;10:836–42.
Moon W, Kim SN, Park S, Paek SH, Kwon JS. The cost-effectiveness of deep brain stimulation for patients with treatment-resistant obsessive-compulsive disorder. Med (Baltim). 2017;96:e7397.
Alonso P, Cuadras D, Gabriëls L, Denys D, Goodman W, Greenberg BD, et al. Deep brain stimulation for obsessive-compulsive disorder: a meta-analysis of treatment outcome and predictors of response. PLOS One. 2015;10:e0133591.
Appleby BS, Duggan PS, Regenberg A, Rabins PV. Psychiatric and neuropsychiatric adverse events associated with deep brain stimulation: a meta-analysis of ten years’ experience. Mov Disord. 2007;22:1722–8.
Kim DD, Basu A. How does cost-effectiveness analysis inform health care decisions? AMA J Ethics. 2021;23:639–47.
Hitti FL, Widge AS, Riva-Posse P, Malone DA, Okun MS, Shanechi MM, et al. Future directions in psychiatric neurosurgery: proceedings of the 2022 American Society for Stereotactic and Functional Neurosurgery meeting on surgical neuromodulation for psychiatric disorders. Brain Stimul. 2023;16:867–78.
Davis RA, Giordano J, Hufford DB, Sheth SA, Warnke P, Widge AS, et al. Restriction of access to deep brain stimulation for refractory OCD: failure to apply the federal parity act. Front Psychiatry. 2021;12:706181.
Visser-Vandewalle V, Andrade P, Mosley PE, Greenberg BD, Schuurman R, McLaughlin NC, et al. Deep brain stimulation for obsessive-compulsive disorder: a crisis of access. Nat Med. 2022;28:1529–32.
Ghio L, Gotelli S, Marcenaro M, Amore M, Natta W. Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta-analysis. J Affect Disord. 2014;152-4:45–51.
Hung CI, Liu CY, Yang CH. Untreated duration predicted the severity of depression at the two-year follow-up point. PLOS One. 2017;12:e0185119.
Kautzky A, Dold M, Bartova L, Spies M, Kranz GS, Souery D, et al. Clinical factors predicting treatment resistant depression: affirmative results from the European multicenter study. Acta Psychiatr Scand. 2019;139:78–88.
Kraus C, Kadriu B, Lanzenberger R, Zarate CA Jr., Kasper S. Prognosis and improved outcomes in major depression: a review. Transl Psychiatry. 2019;9:1–17.
Lundberg J, Cars T, Lööv SÅ, Söderling J, Sundström J, Tiihonen J, et al. Association of treatment-resistant depression with patient outcomes and health care resource utilization in a population-wide study. JAMA Psychiatry. 2023;80:167–75.
Gronemann FH, Jørgensen MB, Nordentoft M, Andersen PK, Osler M. Treatment-resistant depression and risk of all-cause mortality and suicidality in Danish patients with major depression. J Psychiatr Res. 2021;135:197–202.
Goodwin RD, Dierker LC, Wu M, Galea S, Hoven CW, Weinberger AH. Trends in U.S. depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. 2022;63:726–33.
Moreno-Agostino D, Wu YT, Daskalopoulou C, Hasan MT, Huisman M, Prina M. Global trends in the prevalence and incidence of depression: a systematic review and meta-analysis. J Affect Disord. 2021;281:235–43.
Greenberg PE, Birnbaum HG. The economic burden of depression in the US: societal and patient perspectives. Expert Opin Pharmacother. 2005;6:369–76.
Reckers-Droog V, van Exel J, Brouwer W. Willingness to pay for health-related quality of life gains in relation to disease severity and the age of patients. Value Health. 2021;24:1182–92.
Nierenberg AA, DeSecco L. Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry. 2001;62:5–9.
Nierenberg AA. Long-term management of chronic depression. Prim Care Companion CNS Disord. 2001;3:10692.
Holtzheimer PE, Kelley ME, Gross RE, Filkowski MM, Garlow SJ, Barrocas A, et al. Subcallosal cingulate deep brain stimulation for treatment-resistant unipolar and bipolar depression. Arch Gen Psychiatry. 2012;69:150–8.
Gaynes BN, Warden D, Trivedi MH, Wisniewski SR, Fava M, Rush AJ. What did STAR*D teach us? results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv. 2009;60:1439–45.
Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression remission and beyond. JAMA. 2003;289:3152–60.
Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53:649–59.
Paykel ES. Partial remission, residual symptoms, and relapse in depression. Dialogues Clin Neurosci. 2008;10:431–7.
Cowen PJ, Anderson IM. New approaches to treating resistant depression. BJPsych Adv. 2015;21:315–23.
Sapin C, Fantino B, Nowicki ML, Kind P. Usefulness of EQ-5D in assessing health status in primary care patients with major depressive disorder. Health Qual Life Outcomes. 2004;2:20.
Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord. 1998;48:25–36.
Blomstedt P, Hariz MI. Hardware-related complications of deep brain stimulation: a ten year experience. Acta Neurochir (Wien). 2005;147:1061–4.
Jung IH, Chang KW, Park SH, Chang WS, Jung HH, Chang JW. Complications after deep brain stimulation: a 21-year experience in 426 patients. Front Aging Neurosci. 2022;14:819730.
Lozano AM, Mayberg HS, Giacobbe P, Hamani C, Craddock RC, Kennedy SH. Subcallosal cingulate gyrus deep brain stimulation for treatment-resistant depression. Biol Psychiatry. 2008;64:461–7.
Merkl A, Schneider GH, Schönecker T, Aust S, Kühl KP, Kupsch A, et al. Antidepressant effects after short-term and chronic stimulation of the subgenual cingulate gyrus in treatment-resistant depression. Exp Neurol. 2013;249:160–8.
Schlaepfer TE, Bewernick BH, Kayser S, Mädler B, Coenen VA. Rapid effects of deep brain stimulation for treatment-resistant major depression. Biol Psychiatry. 2013;73:1204–12.
Accolla EA, Aust S, Merkl A, Schneider GH, Kühn AA, Bajbouj M, et al. Deep brain stimulation of the posterior gyrus rectus region for treatment resistant depression. J Affect Disord. 2016;194:33–7.
Bergfeld IO, Mantione M, Hoogendoorn MLC, Ruhé HG, Notten P, van Laarhoven J, et al. Deep brain stimulation of the ventral anterior limb of the internal capsule for treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry. 2016;73:456–64.
Hitti FL, Vaughan KA, Ramayya AG, McShane BJ, Baltuch GH. Reduced long-term cost and increased patient satisfaction with rechargeable implantable pulse generators for deep brain stimulation. J Neurosurg. 2018;131:799–806.
Ramasubbu R, Anderson S, Haffenden A, Chavda S, Kiss ZHT. Double-blind optimization of subcallosal cingulate deep brain stimulation for treatment-resistant depression: a pilot study. J Psychiatry Neurosci. 2013;38:325–32.
Schlaepfer TE, Cohen MX, Frick C, Kosel M, Brodesser D, Axmacher N, et al. Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression. Neuropsychopharmacology. 2008;33:368–77.
Acknowledgements
This work was funded by the McNair Foundation (SAS) as well as the National Institutes of Health (NIH) under award number T32GM136611 and by BRASS: Baylor Research Advocates for Student Scientists (KEK).
Author information
Authors and Affiliations
Contributions
KK, RN, and SS contributed to conceptualization of the study. KK and RN contributed to article selection and data collection. KK conducted quantitative analysis and figure preparation. KK prepared the initial manuscript. All authors contributed to manuscript editing and critical review.
Corresponding author
Ethics declarations
Competing interests
Dr. Sheth is a consultant for Boston Scientific, Neuropace, Zimmer Biomet, Koh Young, Sensoria Therapeutics, and Varian Medican and is co-founder of Motif Neurotech. Dr. Mathew has served as a consultant for Abbott, Almatica Pharma, Biohaven, BioXcel Therapeutics, Boehringer-Ingelheim, Brii Biosciences, Clexio Biosciences, COMPASS Pathways, Delix Therapeutics, Douglas Pharmaceuticals, Eleusis, Engrail Therapeutics, Freedom Biosciences, Janssen, Liva Nova, Levo Therapeutics, Merck, Neumora, Neurocrine, Perception Neurosciences, Praxis Precision Medicines, Relmada Therapeutics, Sage Therapeutics, Seelos Therapeutics, Signant Health, Sunovion, Xenon Pharmaceuticals, and XW Pharma.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kabotyanski, K.E., Najera, R.A., Banks, G.P. et al. Cost-effectiveness and threshold analysis of deep brain stimulation vs. treatment-as-usual for treatment-resistant depression. Transl Psychiatry 14, 243 (2024). https://doi.org/10.1038/s41398-024-02951-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-024-02951-7
- Springer Nature Limited