Abstract
Psychiatric syndromes are common following recovery from Coronavirus Disease 2019 (COVID-19) infection. This study investigated the prevalence and the network structure of depression, insomnia, and suicidality among mental health professionals (MHPs) who recovered from COVID-19. Depression and insomnia were assessed with the Patient Health Questionnaire (PHQ-9) and Insomnia Severity Index questionnaire (ISI7) respectively. Suicidality items comprising suicidal ideation, suicidal plan and suicidal attempt were evaluated with binary response (no/yes) items. Network analyses with Ising model were conducted to identify the central symptoms of the network and their links to suicidality. A total of 9858 COVID-19 survivors were enrolled in a survey of MHPs. The prevalence of depression and insomnia were 47.10% (95% confidence interval (CI) = 46.09–48.06%) and 36.2% (95%CI = 35.35–37.21%), respectively, while the overall prevalence of suicidality was 7.8% (95%CI = 7.31–8.37%). The key central nodes included “Distress caused by the sleep difficulties” (ISI7) (EI = 1.34), “Interference with daytime functioning” (ISI5) (EI = 1.08), and “Sleep dissatisfaction” (ISI4) (EI = 0.74). “Fatigue” (PHQ4) (Bridge EI = 1.98), “Distress caused by sleep difficulties” (ISI7) (Bridge EI = 1.71), and “Motor Disturbances” (PHQ8) (Bridge EI = 1.67) were important bridge symptoms. The flow network indicated that the edge between the nodes of “Suicidality” (SU) and “Guilt” (PHQ6) showed the strongest connection (Edge Weight= 1.17, followed by “Suicidality” (SU) - “Sad mood” (PHQ2) (Edge Weight = 0.68)). The network analysis results suggest that insomnia symptoms play a critical role in the activation of the insomnia-depression-suicidality network model of COVID-19 survivors, while suicidality is more susceptible to the influence of depressive symptoms. These findings may have implications for develo** prevention and intervention strategies for mental health conditions following recovery from COVID-19.
Similar content being viewed by others
Introduction
Since December 2022, there had been a surge in Coronavirus Disease 2019 (COVID-19) cases in China following a swift relaxation of its stringent zero-COVID restrictions [1,2,3]. According to a key source at the Center of Disease Control and Prevention, approximately 80% of the population in China could have been infected with COVID-19 by the end of January 2023 [4]. The majority of the COVID-19 patients experienced minimal or mild symptoms, with only a few cases of severe respiratory distress or failure requiring ICU care during that time [5]. However, a substantial number of COVID-19 patients might have had post-COVID-19 related symptoms, which could persist for at least 2 months following the acute phase of infection [6, 7].
The post-COVID-19 condition, which is also known as long COVID-19, can include fatigue, pain, dizziness, sore throat, and so on [11]. Additionally, a prospective study of COVID-19 patients found that 22.34% of participants had suffered insomnia after 1 year follow-up [47]; CS-coefficient larger than 0.25 indicated nodes had moderate stability, while values greater than 0.5 indicated strong stability [48]. The network accuracy was assessed by bootstrapped 95% confidence intervals (CIs) through a non-parametric bootstrap** procedure [47], with a narrower CI having a more accurate network. Finally, we performed a bootstrapped difference test between the EI values and between weights of edge to identify whether the nodes and edges were different from each other [47]. Node stability and accuracy were examined using “bootnet” packages [18]. Data analyses were performed using the R program [49].
Results
Participants information
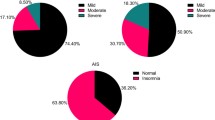
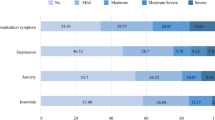
Altogether, 11760 mental health workers were invited to participate in this survey, of whom, 9858 met the inclusion criteria and were included in analyses. Basic demographic and clinical characteristics are shown in Table 1. The mean age of participants was 38.24 years (standard deviation = 8.302), and the majority of the participants were married (73.1%). The prevalence rate of depression and insomnia were 47.10% (95% confidence interval (CI) = 46.09–48.06%) and 36.2% (95%CI = 35.35–37.21%), respectively. The overall prevalence of suicidality was 7.8% (95%CI = 7.31–8.37%), while the prevalence of SI, SP, and SA were 6.5% (95%CI = 6.00–6.97%), 2.7% (95%CI = 2.40–3.04%), and 3.0% (95%CI = 2.64–3.31%), respectively.
Network structure and centrality
Figure 1 presents the network structure of the depression, insomnia, and suicidality model in MHPs who recovered from COVID-19 with a total of 15 nodes. The mean predictability of the nodes was 0.878, suggesting that 87.8% of nodes could be predicted by their neighboring nodes in the model. The top three central nodes that activated the whole network (Z score of expected influence) were “Distress caused by the sleep difficulties” (ISI7) (EI = 1.34), “Interference with daytime functioning” (ISI5) (EI = 1.08), and “Sleep dissatisfaction” (ISI4) (EI = 0.74). The EI values are presented in Table S1.
Figure 2 shows the edges across different clusters in the network and the rank of bridge EI values (1-step Bridge Expected Influence). Expected “Suicidality” (SU) (Bridge EI = 2.66) (which was regarded as a bridge symptom since it was a cluster composed of a single node), “Fatigue” (PHQ4) (Bridge EI = 1.98), “Distress caused by the sleep difficulties” (ISI7) (Bridge EI = 1.71) and “Motor Disturbances” (PHQ8) (Bridge EI = 1.67) were important bridge symptoms that linked the whole network.
Figure 3 shows the flow diagram of the network model, which indicates in descending order that “Guilt” (PHQ6) (Edge weight = 1.17), and “Sad Mood” (PHQ2) (Edge weight = 0.67) in the depression cluster were directly associated with suicidality with strong weights, while the association between guilt and suicidality was the strongest. In addition, “Distress caused by the sleep difficulties” (ISI7) (Edge weight = 0.31) in the insomnia cluster were directly associated with suicidality with weak weights. The edge-weighted values are presented in Table S2.
Network stability and accuracy
In terms of network stability shown in Fig. 4, an excellent level of stability was observed in both EI and bridge EI, with CS-coefficient being 0.75 and 0.67, respectively. Figures S1 and S2 display the Bootstrapped 95% CIs, indicating that the estimated EIs and bridge EI were reliable and stable. The bootstrap difference test in Figs. S3, S4 indicates that most edges and EIs were significantly different from others.
Discussion
To the best of our knowledge, this was the first study globally that examined the prevalence and network structure of depression, insomnia, and suicidality among MHPs who recovered from COVID-19 infection. Our findings found that the three most central symptoms in the network were in the insomnia cluster, whereas the three strongest associations with suicidality were observed in the depressive cluster.
The prevalence of depression and insomnia was high in MHPs who recovered from COVID-19, which is consistent with previous meta-analyses that found that the prevalence of depression among doctors during the COVID-19 pandemic was 20.5% [50], while the pool prevalence of depression in COVID-19 infected patients was 45% [51]. As for insomnia, a meta-analysis conducted during the COVID-19 pandemic showed that the prevalence of insomnia in healthcare workers and COVID-19 patients were 46.4% and 48.7%, respectively, which were roughly twice as high as that in the general population (26.0%) [52]. These findings appear to be consistent with the hypothesis of this study.
It was noted that the rapid lifting of the stringent zero-COVID-19 restrictions had put an unprecedented strain on China’s healthcare system [53]. COVID-19-infected MPHs faced dual pressure from both their work and illness recovery, thus experiencing a greater likelihood of depression or insomnia than the general population. Further, in that period, most MHPs were re-deployed to care for COVID-19 patients and faced with higher work pressure and longer work shifts, which could increase the risk of insomnia [54]. Moreover, during their own recovery from COVID-19, MHPs were often directly involved in treating COVID-19 patients, which increased their risk for secondary infection as well as depressive and insomnia symptoms [55].
“Distress caused by sleep difficulties” (ISI7), which reflects the level of worry caused by sleep problems, was the most central and important bridge symptom among MHPs who had recovered from COVID-19 inflection, thus suggesting it could more readily influence other symptoms within the depression-insomnia-suicidality network model [48]. As a fundamental aspect of anxiety [56], worry also plays a crucial role in maintaining insomnia and predicting depression [57]. This is consistent with the findings of another network analysis study in a community-dwelling population during the COVID-19 pandemic, in which anxiety symptoms were the most important bridge symptoms linking depression and insomnia [22]. One potential explanation is that distress caused by sleep problems is usually accompanied by a range of negative emotions in patients who recovered from an infection [58]. MHPs who had recovered from COVID-19 might worry about various issues such as patients’ safety, shortage of medicine, and the risk of infecting their families and friends, all of which could exacerbate depression [59]. Moreover, there was a direct connection between “Distress caused by sleep difficulties” (ISI7) and “Suicidality” (SU) in the flow network, indicating that interventions aimed at addressing worry and distress arising from sleep difficulties could be useful in reducing both depressive symptoms and suicidality in this subpopulation. For instance, a widely used approach is cognitive behavior therapy, which has good evidence in treating insomnia related worries [60].
Another insomnia symptom “interference with daytime functioning” (ISI5) (i.e., trouble with concentration, mood disturbances, or decreased ability to perform daily activities) was identified as a core symptom in the network model. For patients who recovered from COVID-19, problems with memory, concentration, or sleep were among the most common post-COVID-19 symptoms, even after an extended time following infection [65]. Moreover, self-reported sleep dissatisfaction were found to be significantly associated with suicidal ideation in the past year [66].
Depressive symptom “Fatigue” (PHQ4) was one of the top bridge symptoms within the depression-insomnia-suicidality network model. Previous research found that approximately one-third of people experienced fatigue after being diagnosed with COVID-19 [61]. These findings are consistent with studies in Filipino domestic workers and hospital clinicians, where fatigue was identified as the key symptom in the depression and anxiety network model [67, The data of this study are available from the corresponding author upon reasonable request. Economist T. China is dismantling its zero-covid machine. The Economist. 2022. Kang D. Packed ICUs, crowded crematoriums: COVID roils Chinese towns. AP NEWS. 2022. Ritchie H, Gan N, McCarthy S, Wang S, Zhang M. Leaked notes from Chinese health officials estimate 250 million Covid-19 infections in December: reports. CNN. 2022. CNN. China says 80% of population have had Covid-19, as millions travel for Lunar New Year. CNN. 2023. Chinese Center for Disease Control and Prevention. National outbreak of novel coronavirus infections (in chinese). 2023. Islam MF, Cotler J, Jason LA. Post-viral fatigue and COVID-19: lessons from past epidemics. Fatigue: Biomed Health Behav. 2020;8:61–9. WHO. Post COVID-19 condition (Long COVID). 2021. https://www.who.int/srilanka/news/detail/16-10-2021-post-covid-19-condition. WHO. Coronavirus disease (COVID-19): post COVID-19 condition. 2023. https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition?gclid=CjwKCAjw3POhBhBQEiwAqTCuBu7q**KbwVtDhnPwvVXP2u9K4_ir-Qgl5YpPvWw8Gx8scaVYF2kzOxoCCiYQAvD_BwE. Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021;114:428–42. Nalleballe K, Onteddu SR, Sharma R, Dandu V, Brown A, Jasti M, et al. Spectrum of neuropsychiatric manifestations in COVID-19. Brain Behav Immun. 2020;88:71–4. Shanbehzadeh S, Tavahomi M, Zanjari N, Ebrahimi-Takamjani I, Amiri-arimi S. Physical and mental health complications post-COVID-19: sco** review. J Psychosom Res. 2021;147:110525. Zhao Y, Yang C, An X, **ong Y, Shang Y, He J, et al. Follow-up study on COVID-19 survivors one year after discharge from hospital. Int J Infect Dis. 2021;112:173–82. Staner L. Comorbidity of insomnia and depression. Sleep Med Rev. 2010;14:35–46. Sher L. Post-COVID syndrome and suicide risk. QJM. 2021;114:95–8. Sher L. Are COVID-19 survivors at increased risk for suicide? Acta Neuropsychiatr. 2020;32:270. Nourchene K, Khelifa E, Abassi B, Maatouk O, Bouguerra I, Ben Aissa S, et al. COVID 19 survivors : feeling suicidal ? Eur Psychiatry. 2022;65:S256. S Bernert RA, Joiner TE. Sleep disturbances and suicide risk: a review of the literature. Neuropsychiatr Dis Treat. 2007;3:735–43. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50:195–212. Epskamp S, Kruis J, Marsman M. Estimating psychopathological networks: be careful what you wish for. PLoS ONE. 2017;12:e0179891. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2017;50:195–212. Zhao N, Zhao YJ, An F, Zhang Q, Sha S, Su Z, et al. Network analysis of comorbid insomnia and depressive symptoms among psychiatric practitioners during the COVID-19 pandemic. J Clin Sleep Med. 2023;19:1271–9. Bai W, Zhao Y-J, Cai H, Sha S, Zhang Q, Lei S-M, et al. Network analysis of depression, anxiety, insomnia and quality of life among Macau residents during the COVID-19 pandemic. J Affect Disord. 2022;311:181–8. Cha EJ, Jeon HJ, Chung S. Central symptoms of insomnia in relation to depression and COVID-19 anxiety in general population: a network analysis. J Clin Med. 2022;11:3416. Bai W, Zhao Y, An F, Zhang Q, Sha S, Cheung T, et al. Network analysis of insomnia in Chinese mental health professionals during the COVID-19 pandemic: a cross-sectional study. Nat Sci Sleep. 2021;13:1921–30. **ang YT, Zhao YJ, Liu ZH, Li XH, Zhao N, Cheung T, et al. The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform. Int J Biol Sci. 2020;16:1741–4. Chen S, Fang Y, Chiu H, Fan H, ** T, Conwell Y. Validation of the nine-item Patient Health Questionnaire to screen for major depression in a Chinese primary care population. Asia Pac Psychiatry. 2013;5:61–8. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. Indu PS, Anilkumar TV, Vijayakumar K, Kumar KA, Sarma PS, Remadevi S, et al. Reliability and validity of PHQ-9 when administered by health workers for depression screening among women in primary care. Asian J Psychiatry. 2018;37:10–4. Cai H, Chow IHI, Lei SM, Lok GKI, Su Z, Cheung T, et al. Inter-relationships of depressive and anxiety symptoms with suicidality among adolescents: a network perspective. J Affect Disord. 2023;324:480–8. Zhao YJ, Zhang SF, Li W, Zhang L, Guo T, Cheung T, et al. Associations between depressive symptoms and quality of life among residents of Wuhan, China during the later stage of the COVID-19 pandemic: a network analysis. J Affect Disord. 2022;318:456–64. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. Yu DSF. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66:2350–9. Chen P, Zhang L, Sha S, Lam MI, Lok K-I, Chow IHI, et al. Prevalence of insomnia and its association with quality of life among Macau residents shortly after the summer 2022 COVID-19 outbreak: a network analysis perspective. Front Psychiatry. 2023;14:1113122. McBride O, Murphy J, Shevlin M, Gibson-Miller J, Hartman TK, Hyland P, et al. Monitoring the psychological, social, and economic impact of the COVID-19 pandemic in the population: context, design and conduct of the longitudinal COVID-19 psychological research consortium (C19PRC) study. Int J Methods Psychiatric Res. 2021;30:e1861. Starr J, Falk CF. On the testing of equivalent variables: Perfect correlations and correlational topology. 2022. https://doi.org/10.31234/osf.io/vhgfk. Peckham AD, Jones P, Snorrason I, Wessman I, Beard C, Björgvinsson T. Age-related differences in borderline personality disorder symptom networks in a transdiagnostic sample. J Affect Disord. 2020;274:508–14. Mullen R, Jones ES. Network analysis of competitive state anxiety. Front Psychol. 2021;11:3726. Pan C, Li G, Sun W, Miao J, Wang Y, Lan Y, et al. Psychopathological network for early-onset post-stroke depression symptoms. BMC Psychiatry. 2023;23:114. Farhat LC, Brentani H, de Toledo VHC, Shephard E, Mattos P, Baron‐Cohen S, et al. ADHD and autism symptoms in youth: a network analysis. J Child Psychol Psychiatry. 2022;63:143–51. Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5–13. Jones PJ. networktools: assorted tools for identifying important nodes in networks. R package version 1.0.0. 2017. https://CRAN.R-project.org/package=networktools. Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol. 2016;125:747–57. Bringmann L, Elmer T, Epskamp S, Krause R, Schoch D, Wichers M, et al. What do centrality measures measure in psychological networks? J Abnorm Psychol. 2019;128:892–903. Haslbeck JM, Waldorp LJ. How well do network models predict observations? On the importance of predictability in network models. Behav Res Methods. 2018;50:853–61. Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Stat. Softw. 2012;48:1–18. Haslbeck JMB, Waldorp LJ. mgm: Estimating Time-Varying Mixed Graphical Models in High-Dimensional Data. J Stat Softw. 2020;93:1–46. Chernick MR. Bootstrap methods: a guide for practitioners and researchers. John Wiley & Sons; 2011. Costenbader E, Valente TW. The stability of centrality measures when networks are sampled. Social Netw. 2003;25:283–307. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2022. https://www.R-project.org/. Chen Y, Wang J, Geng Y, Fang Z, Zhu L, Chen Y, et al. Meta-analysis of the prevalence of anxiety and depression among frontline healthcare workers during the COVID-19 pandemic. Front Public Health. 2022;10:984630. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. 2021;1486:90–111. Li Y, Chen B, Hong Z, Sun Q, Dai Y, Basta M, et al. Insomnia symptoms during the early and late stages of the COVID-19 pandemic in China: a systematic review and meta-analysis. Sleep Med. 2022;91:262–72. McCarthy S. As China moves away from zero-Covid, health experts warn of dark days ahead. Hong Kong CNN. 2022. https://edition.cnn.com/2022/12/06/china/china-zero-covid-relaxation-crisis-intl-hnk-mic/index.html. Brown JP, Martin D, Nagaria Z, Verceles AC, Jobe SL, Wickwire EM. Mental health consequences of shift work: an updated review. Curr Psychiatry Rep. 2020;22:7. Mehdi M, Waseem M, Rehm MH, Aziz N, Anjum S, Javid MA. Depression and anxiety in health care workers during COVID-19. Biomedica. 2020;36:247–52. Rapee RM. Generalized anxiety disorder: a review of clinical features and theoretical concepts. Clin Psychol Rev. 1991;11:419–40. Ballesio A, Bacaro V, Vacca M, Chirico A, Lucidi F, Riemann D, et al. Does cognitive behaviour therapy for insomnia reduce repetitive negative thinking and sleep-related worry beliefs? A systematic review and meta-analysis. Sleep Med Rev. 2021;55:101378. Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev. 2010;14:227–38. Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;48:592–8. van der Zweerde T, Bisdounis L, Kyle SD, Lancee J, van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev. 2019;48:101208. Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in Post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022;101:93–135. Koh D, Tan A. Return to work for workers with post-COVID conditions. Saf Health Work. 2022;13:377–8. Mayers AG. Subjective sleep dissatisfaction in depression: Nottingham Trent University; 2006. Park HY, Heo J, Subramanian S, Kawachi I, Oh J. Socioeconomic inequalities in adolescent depression in South Korea: a multilevel analysis. PLoS ONE. 2012;7:e47025. Ohayon MM, Caulet M, Priest RG, Guilleminault C. DSM–IV and ICSD–90 insomnia symptoms and sleep dissatisfaction. Br J Psychiatry. 1997;171:382–8. Im Y, Oh W-O, Suk M. Risk factors for suicide ideation among adolescents: five-year national data analysis. Arch Psychiatr Nurs. 2017;31:282–6. ** Y, Sha S, Tian T, Wang Q, Liang S, Wang Z, et al. Network analysis of comorbid depression and anxiety and their associations with quality of life among clinicians in public hospitals during the late stage of the COVID-19 pandemic in China. J Affect Disord. 2022;314:193–200. Garabiles MR, Lao CK, **ong Y, Hall BJ. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: a network approach. J Affect Disord. 2019;250:85–93. Huang WY, Huang H, Wu CE. Physical activity and social support to promote a health-promoting lifestyle in older adults: an intervention study. Int J Environ Res Public Health. 2022;19:14382. Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019;23:2324–32. Lester D. The association of shame and guilt with suicidality. J Soc Psychol. 1998;138:535–6. DeVylder J, Zhou S, Oh H. Suicide attempts among college students hospitalized for COVID-19. J Affect Disord. 2021;294:241–4. The authors are grateful to all participants and clinicians involved in this study. The study was supported by the National Science and Technology Major Project for Investigational New Drug (2018ZX09201-014), the Bei**g Hospitals Authority Clinical Medicine Development of Special Funding Support (XMLX202128), and the University of Macau (MYRG2019-00066-FHS; MYRG2022-00187-FHS). Study design: Feng-Rong An, Ling Zhang, Yuan Feng, and Yu-Tao **ang. Data collection, analysis, and interpretation: He-Li Sun, Pan Chen, Wei Bai, Zhaohui Su, Teris Cheung, Gabor S. Ungvari, **-Ling Cui, and Feng-Rong An. Drafting of the manuscript: He-Li Sun and Yu-Tao **ang. Critical revision of the manuscript: Chee H. Ng. Approval of the final version for publication: all co-authors. The authors declare no competing interests. The study protocol was approved by the Ethics Committee of the Bei**g Anding Hospital, China. All participants who provided written informed consent were included. Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Sun, HL., Chen, P., Bai, W. et al. Prevalence and network structure of depression, insomnia and suicidality among mental health professionals who recovered from COVID-19: a national survey in China.
Transl Psychiatry 14, 227 (2024). https://doi.org/10.1038/s41398-024-02918-8 Received: Revised: Accepted: Published: DOI: https://doi.org/10.1038/s41398-024-02918-8Data availability
References
Acknowledgements
Author information
Authors and Affiliations
Contributions
Corresponding authors
Ethics declarations
Competing interests
Ethics
Informed consent
Additional information
Supplementary information
Rights and permissions
About this article
Cite this article