Abstract
Nucleophosmin 1 (NPM1) is a nucleus-cytoplasmic shuttling protein which is predominantly located in the nucleolus and exerts multiple functions, including regulation of centrosome duplication, ribosome biogenesis and export, histone assembly, maintenance of genomic stability and response to nucleolar stress. NPM1 mutations are the most common genetic alteration in acute myeloid leukemia (AML), detected in about 30–35% of adult AML and more than 50% of AML with normal karyotype. Because of its peculiar molecular and clinico-pathological features, including aberrant cytoplasmic dislocation of the NPM1 mutant and wild-type proteins, lack of involvement in driving clonal hematopoiesis, mutual exclusion with recurrent cytogenetic abnormalities, association with unique gene expression and micro-RNA profiles and high stability at relapse, NPM1-mutated AML is regarded as a distinct genetic entity in the World Health Organization (WHO) classification of hematopoietic malignancies. Starting from the structure and functions of NPM1, we provide an overview of the potential targeted therapies against NPM1-mutated AML and discuss strategies aimed at interfering with the oligomerization (compound NSC348884) and the abnormal traffic of NPM1 (avrainvillamide, XPO1 inhibitors) as well as at inducing selective NPM1-mutant protein degradation (ATRA/ATO, deguelin, (-)-epigallocatechin-3-gallate, imidazoquinoxaline derivatives) and at targeting the integrity of nucleolar structure (actinomycin D). We also discuss the current therapeutic results obtained in NPM1-mutated AML with the BCL-2 inhibitor venetoclax and the preliminary clinical results using menin inhibitors targeting HOX/MEIS1 expression. Finally, we review various immunotherapeutic approaches in NPM1-mutated AML, including immune check-point inhibitors, CAR and TCR T-cell-based therapies against neoantigens created by the NPM1 mutations.
Similar content being viewed by others
Introduction
Nucleophosmin 1 (NPM1) is a ubiquitous nucleus-cytoplasmic shuttling protein [1] predominantly resident in the nucleolus whose functions are pivotal for many cellular processes including histone assembly, centrosome duplication, ribosome biogenesis and export, maintenance of genomic stability and response to nucleolar stress [2].
Mutations of NPM1 gene are the most frequent genetic lesion in acute myeloid leukemia (AML), being detectable in about one-third of adult AML and 50–60% of AML with normal karyotype [3, 4]. These mutations are a driver genetic lesion and AML defining event that occurs in the context of clonal hematopoiesis, frequently promoted by genes such as DNMT3A and TET2 [4]. Distinctive features of NPM1-mutated AML include the mutual exclusion with recurrent cytogenetic abnormalities, the association with specific gene expression [5] and microRNA [6] profiles and the high stability of NPM1 mutations at relapse [7]. Another characteristic of NPM1-mutated AML is the aberrant cytoplasmic dislocation of the NPM1 mutant and NPM1 wild-type proteins (through heterodimerization) [3, 8, 9]. Moreover, the mutant NPM1 is directly involved in promoting high expression of homeobox (HOX) genes [10] which are necessary for maintaining the undifferentiated state of leukemic cells. Notably, this function is closely dependent on the cytoplasmic localization of the mutant. However, the mechanisms underlying leukemogenesis in NPM1-mutated AML still remain largely unknown [4]. According to the 5th edition of the World Health Organization (WHO) of hematolymphoid tumors, NPM1-mutated AML can be diagnosed irrespective of the percentage of blasts, based on previous observations that cases classified as MDS or MDS/MPN with NPM1 mutations quickly progressed to AML [11]. Because of the above unique features, NPM1-mutated AML is recognized as a distinct entity, within the category of AML with recurrent genetic abnormalities of the WHO classification [11]. The main characteristics of NPM1-mutated AML are summarized in Table 1.
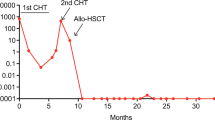
The standard therapy of NPM1-mutated AML in young adults is based upon induction chemotherapy (±FLT3 inhibitors) and consolidation cycles with high/intermediate dose of cytarabine (ARA-C) ± allogeneic hematopoietic stem cell transplantation (HSCT) in first complete remission (CR), depending on the status of the FLT3 gene and measurable residual disease-MRD [12, 13]. However, despite the remarkable advances in the treatment of NPM1-mutated AML, about 50% of patients still died of progressive disease. Thus, there is a need for new therapeutic opportunities. Whole genomic approaches have unraveled the molecular heterogeneity of AML [14, 15] and given a great input to the development of small molecules aimed to target specific genetic abnormalities [16, 17]. Because of their small-size (<500 Da), these compounds can easily penetrate the cell membrane and exert their activity on intracellular proteins involved in cell signaling mechanisms (e.g., kinases) that promote the tumor growth [68], NPM1-mutated AML patients appear to be particularly sensitive to venetoclax (Fig. 2). Whether this efficacy is related to the high expression of HOX genes [5], that in turn are linked to BCL-2 inhibitor sensitivity and responsiveness [69], remains to be defined. NPM1 mutant-primed defect in mitochondrial function may also be responsible for the higher sensitivity to venetoclax [44].
NPM1-mutated AML particularly benefits from venetoclax-based regimens, both at first diagnosis [70, 71] (independently by the FLT3 status [72]) and in the relapsed/refractory setting [4]. Alternatively, recruitment of NPM1 mutants to HOX loci through their interaction with chromatin-bound XPO1 [91] could be responsible for HOX expression maintenance, cytoplasmic delocalization of NPM1 representing a mere epiphenomenon. We previously suggested that NPM1 mutants may induce leukemia by acting both at the chromatin level and by delocalizing NPM1-interacting partners in the cytoplasm [4].
Dependence of NPM1-mutated AML cells on epigenetic machinery for HOX regulation [92] provides the rationale for using inhibitors of KMT2A-menin protein interaction [93, 94] (Fig. 2; Table 2). The VTP-50469 inhibitor showed strong in vitro and in vivo anti-leukemic activity on NPM1-mutated AML cells, causing a dose-dependent reduction in cell proliferation, a significant downregulation of HOXA/B clusters and MEIS1 gene expression, a marked differentiation of leukemic cells, a reduction of AML engraftment and a prolonged survival in mice PDX models [92, 95, 96]. This occurred especially through rapid repression of important co-factors of HOX genes (MEIS1 and PBX3), the effect on expression of HOXA and HOXB genes being not relevant [97]. The MI-3454 inhibitor was very effective in inhibiting cell proliferation and differentiation of NPM1-mutated AML cells, independently from the coexistence of other mutations in patients’ samples, and in reducing blast infiltration of organs and expression of MEIS1 and FLT3 in PDX NPM1-mutated mouse models [95].
Menin inhibitors were reported to prevent the transformation of Npm1-mutated mouse hematopoietic progenitors into leukemic cells, implying that they could also be effective in Npm1-mutated preleukemia [96]. However, we believe that this concept is difficult to translate into clinic because NPM1 mutations in patients do not associate with a preleukemic state [4]. Moreover, myelodysplasia with NPM1 mutations is very rare and cases with these characteristics usually represent already early-stage AML [12]. Thus, we expect that the value of menin inhibitors in clinic will be mainly limited to the therapy of frank NPM1-mutated AML.
Menin inhibitors was also combined with inhibitors of FLT3 (mutated in about 40% of NPM1-mutated AML [3]), demonstrating a synergistic effect that resulted in stronger cell growth inhibition, apoptosis and differentiation of AML blast cells [98] and induction of long-lasting CR in PDX mice models of NPM1-mutated/FLT3-ITD AML [99]. Menin inhibitors have been also combined with XPO1 inhibitors. The rationale for this association is that nuclear relocation of the NPM1 mutant by the XPO1 inhibitors is associated with downregulation of HOX genes [10]. Thus, the two compounds could exert a cumulative effect on downregulation of HOX genes through different mechanisms. The utility of combining menin inhibitors with venetoclax has been already mentioned [83]. All these associations could help preventing the rapid development of resistance to targeted monotherapies.
Menin inhibitors, including KO-539, SNDX-5613, JNJ-75276617 and DS-1594b, are currently evaluated in clinical trials [100, 101]. KO-539 induced CR in 2/6 patients with R/R AML who were evaluable for efficacy analysis. One of them had an NPM1-mutated AML co-mutated for DNMT3A and KMT2D who received KO-539 at 200 mg/die, as the eight line of therapy, achieving an MRD-negative CR [101]. This trial continues to enroll patients with NPM1-mutated and KTM2A-rearranged AML on the doses of 200 and 600 mg (NCT04067336). SNDX-5613 (an analog of VTP-50469) was very active in PDX mouse models of NPM1-mutated AML, including animals remaining in CR 1 year after cessation of therapy [96, 102]. The safety and efficacy of SNDX-5613 in adult patients with R/R NPM1-mutated or KTM2A-rearranged AML is being evaluated in the AUGMENT-101 phase I/II trial (NCT04065399). Preliminary results of this study were released by Syndax in April 2021. By March 2021, the trial had enrolled in the phase 1 cohort, 43 patients (median age 54 years) who had received a median of 3 previous lines of treatment. The most common side effects (>5%) included QT prolongation (14%), differentiation syndrome (5%) and anemia (5%). The overall response rate in the 7 patients with NPM1-mutated AML was 29% (2/7). In kee** with the proposed mechanism of menin inhibitors, RNA-Seq analysis of the bone marrow samples from responding patients exhibited downregulation of MEIS and HOXA9 genes and upregulation of the differentiation antigens CD11b, CD14 and CD13. The phase 2 part of the trial is ongoing. JNJ-75276617 is a potent inhibitor of the binding between menin and KTM2A. Its safety and activity are being tested in NCT04811560 that enrolls AML patients harboring NPM1 mutations or KMT2A rearrangements. However, no data have been released so far. The safety and efficacy of DS-1594b menin inhibitor will be evaluated as single drug or in combination with azacytidine and venetoclax regimens in a phase 1/2 clinical trial (NCT04752163). To maximize the depth and durability of clinical response, the Biomea Fusion, Inc. has recently developed BMF-219, an orally bioavailable, potent and selective irreversible covalent menin inhibitor. Clinical trial with this compound is ongoing (NCT05153330).
Targeting SYK signaling
In a phase 1b/2 trial (NCT02343939), entospletinib, a selective oral inhibitor of the spleen tyrosine kinase (SYK) which is constitutively activated in AML promoting survival and proliferation [103], when combined with chemotherapy, was more active in patients with HOXA9/MEIS1 signature (as in NPM1-mutated AML) than in the whole patient population [104] (Fig. 2). These results suggest that the increased expression and activity of SYK protein is strictly dependent upon the deregulation of HOXA and MEIS genes [105]. Based on this evidence, FDA approved a phase 3 trial to assess the efficacy and safety of entospletinib in combination with chemotherapy in adult patients with newly diagnosed NPM1-mutated AML (NCT05020665).
Immunotherapy of NPM1-mutated AML
Ideally, any target antigen for AML immunotherapy should be expressed at high levels in the whole leukemic population, including leukemic stem cells, and to be absent or low expressed in normal hematopoietic cells and other tissues. Leukemia-associated antigens (e.g., CD33 and CD123) are usually strongly expressed in AML cells (especially in NPM1-mutated AML cells [106,107,108]) but can also be detected in normal hematopoietic stem cells and in extramedullary tissues (e.g., CD123 in endothelial cells). This limits their use as target antigens for immunotherapy because of potential off-target effects.
Conversely, leukemia-specific antigens deriving from altered proteins encoded by leukemogenic mutations (e.g., NPM1), are specifically expressed in malignant clones and therefore represent ideal targets. In particular, the NPM1 mutant neoantigen can be considered an ideal AML target for a number of reasons. First, NPM1 mutations are common driver, gate-keeper events [109], very stable at relapse [4], specific for AML and absent in normal tissues [110]. Second, the NPM1 mutated proteins are detectable in chemoresistant leukemic stem cells [108], making them possibly vulnerable to immune surveillance and eradication. Third, although >50 NPM1 mutations have been identified, the 4 bp frameshift insertion occurring in NPM1 mutant A is responsible for almost 80-85% of all mutations and more rare NPM1 mutations lead to the same amino acidic changes at NPM1 C-terminus. Fourth, the newly acquired amino acid C-terminus sequence of NPM1 mutant proteins is highly immunogenic in animals, eliciting specific antibodies. Fifth, the aberrant localization of the NPM1 mutant proteins in the cytoplasm of leukemic cells may favor their processing by the Human Leukocyte Antigen (HLA) MHC class I degradation pathway leading to HLA presentation and anti-cancer immune response. Indeed, using in silico analysis, we predicted that several peptides could bind to specific HLA class I molecules [111]. Sixth, specific autologous cytotoxic T-cell responses against NPM1 mutant peptides could be detected in NPM1-mutated AML patients [112,113,114,115]. These immune responses associated with molecular CR [116] and may explain the relatively favorable outcome of NPM1-mutated AML [117]. interestingly, NPM1-mutated AML sensitivity to T-cell immunity has been observed not only in the autologous but also in allogeneic setting. Although NPM1-mutated AML patients without FLT3-ITD has a good prognosis, those who underwent allogeneic HSCT showed a particularly long-term disease control [118], probably due to specific graft-versus leukemia effect. Moreover, polyspecific T-cell anti-leukemic responses, even against NPM1-mutated peptides, have been observed following preemptive donor lymphocyte infusions (DLIs) at molecular relapse after allogeneic HSCT [116]. Finally, the importance of eradicating the NPM1-mutated clone to achieve cure of AML is exemplified by the clinical observation of patients with NPM1-DNMT3A double-mutated AML after cessation of therapy. These cases, when achieve long-term molecular (MRD-negative) remission, are likely to be cured, even though the persistence of detectable copies of the DNMT3A mutant (indicating persistent clonal hemopoiesis) may expose them to a low risk of develo** a second AML [4].
Antibodies against CD33 and CD123
CD33 is expressed in all stages of myeloid differentiation [119] and it is detectable in most cases of AML, the expression levels being high in NPM1-mutated AML [106]. Thus, CD33 is an useful target for immunotherapy with an anti-CD33 monoclonal antibody conjugated with a DNA-damaging calicheamicin derivative (Gemtuzumab Ozogamicin-GO) (Fig. 4). In a metanalysis study [120], adding GO to chemotherapy showed a survival benefit for intermediate-risk cytogenetics and NPM1-mutated AML patients because of a reduced relapse risk. Similar results were reported by the ALFA0701 trial that also demonstrated the impact of GO in reducing NPM1-mut transcripts level [121]. Higher reduction of NPM1-mut transcript levels were also observed in the GO arm of the AMLSG study that translated into a lower cumulative incidence of relapse [122]. However, the AMLSG 09-09 Phase III Study failed to meet the early primary end point (event-free survival) due to higher early mortality in the GO arm [123]. Nevertheless, a significant clinical benefit was observed in females older than 70 years with NPM1-mutated/FLT3 wild-type genotype [123] in terms of both event-free-survival and cumulative incidence of relapse. Collectively, the above studies support the incorporation of GO into the frontline treatment of NPM1-mutated AML.
CD123 is highly expressed in NPM1-mutated AML both at diagnosis and relapse (Fig. 4), the highest expression being observed in CD34+ CD38− leukemic cells [107]. Moreover, CD123 expression was enhanced by FLT3 mutations, suggesting that the subset of NPM1/FLT3 double-mutated AML patients could particularly benefit from anti-CD123 targeted therapies [107]. So far, tagraxofusp (SL401) which is formed by the fusion of IL-3 with diphtheria toxin and the CD123-directed chimeric antigen receptor (CAR) T cells (MB-102) developed by Mustang Bio Inc. are approved or received the Orphan drug designation (MB-102) for the treatment of blastocytic plasmacytoid dendritic cell neoplasm [124] which strongly expresses CD123. Only scarce information is available in CD123-positive R/R AML. Main limitation of these products is myelotoxicity [124].
Antibodies against PD-1 and PD-L1
AML is a poorly immunogenic and highly immune-suppressive hematological malignancy. High expression of PD-L1 has been found in NPM1-mutated AML patients, especially in the leukemic progenitors/stem cell compartment (CD34+ CD38−) [125]. High PD-L1 expression in blasts of AML with NPM1-mutated/FLT3-ITD genotype predicted inferior survival [41]. Moreover, in a comprehensive immunogenomic analysis of AML, mutations of NPM1 and FLT3 preferentially associated with low T-cell cytolytic activity and a reduced expression of HLA-II (and/or related genetic determinants of HLA-II expression, as CIITA) [126]. Interestingly, CIITA methylation may limit antigen presentation by primary NPM1mutIDH1mut AML blasts through downregulation of MHC-II, thereby inducing immune evasion [126]. Immune evasion in NPM1-mutated AML is also contributed by VISTA (V-domain Ig suppressor of T-cell activation) and ULBP1 (NKG2 ligand) immunoregulatory circuitries that are both significantly upregulated in NPM1-mutated AML patients [126] (Fig. 4). VISTA-Ig, which shows a partial homology with other B7 family members, is predominantly expressed in hematopoietic cells of myeloid lineage. This circuitry in mainly involved in suppressing proliferation of T cells and blunting the production of T-cell cytokines, making it a potential target for immune check-point blockade combinations [127].
More recently, the anti-PD-1 antibody, nivolumab, was found to increase leukemia-associated antigen-stimulated cytotoxic T cells and cytotoxicity against stem cell-like cells, especially those carrying NPM1 mutations [128]. These findings provide a rationale for the treatment of NPM1-mutated AML, combining anti-PD-1 and anti NPM1-mutation specific immunotherapy (see below). Moreover, targeted immune gene expression and multiplexed digital spatial profiling showed distinct AML immune microenvironments [129]. The immune-infiltrated microenvironment that was characterized by severe immune suppression (high expression of PD-L1, CTLA4, IDO1 and BTLA), higher dependence from IFN-γ driven adaptive immune responses, high T-cell infiltration and expression of major histocompatibility complex, closely clustered with the adverse-risk genetic AML categories (specifically, TP53 and RUNX1 mutated AML) [129]. Conversely, the NPM1-mutated cases (with or without FLT3-ITD) more frequently showed an immune-depleted microenvironment [129]. Finally, NPM1-mutated AML harboring concomitant clonal hematopoiesis driven mutations (e.g., DNMT3A, TET2) showed an enriched tumor inflammation signature score, predicting a clinical benefit from anti-PD-1 treatment [130]. This finding is in kee** with the observation linking in a mouse model a persistent immune stimulation to an accelerated NPM1mut myeloproliferative phenotype in vivo [131].
Although the above findings suggest that NPM1-mutated AML may be a potential candidate for immune check-point inhibition (Fig. 4), the few studies performed so far with anti-PD-L1 antibodies in AML patients have shown only modest clinical activity. Their impact has been evaluated also in combination with hypomethylating agents [132,133,134], since they induce the expression of several immune-related genes, including HLA-I and HLA-II, leukemia-associated antigens (e.g., PRAME, WT1) [135], PD-1 and PD-L1 [136]. Despite most studies did not specifically evaluate NPM1-mutated AML, they showed that patients who might benefit more from these drug combinations are those who are naïve for hypomethylating agents or have <20% blasts and a higher pre-therapy infiltration of bone marrow by CD3+, CD4+ Teff, and CD8+ T cells [132]. The clinical trial NCT03769532 is currently evaluating the safety/efficacy of pembrolizumab plus 5-azacitidine in NPM1-mutated AML patients. The impact of pembrolizumab 200 mg (i.v. on day 14) has been assessed also in association with high-dose cytarabine in 37 R/R AML patients (9/37, 24%, bearing NPM1 mutations) [137]. The overall response rate, composite CR rate and median OS were 46%, 38% and 11.1 months, respectively. Responding patients exhibited a higher percentage of progenitor exhausted TCF1+ CD8+ T cells and an increased diversity of the T-cell receptor at baseline [137].
As previously mentioned, venetoclax is very active in NPM1-mutated AML [70]. This effect is also contributed by the immunomodulatory effect of the drug that enhances the T-cell-mediated anti-leukemic response by increasing reactive-oxygen species (ROS) production [138] and increases the PD1+ T-effector memory cells and anti-tumor efficacy in combination with immune check-point blockade [139]. The NCT02397720 trial is assessing the combination of nivolumab, azacytidine and venetoclax in frontline and R/R AML, while the NCT04284787 trial is assessing the impact of pembrolizumab plus azacytidine and venetoclax in newly diagnosed AML patients unfit for conventional chemotherapy.
CAR and TCR engineered T cell therapy
CAR T cells or T-cell receptor (TCR) gene therapy could be promising approaches against NPM1-mutated AML. Immune targeting can be distinguished into: (1) HLA-dependent therapies relying on the presentation of NPM1 neoantigen [113]; or (2) HLA-independent therapies identifying molecules differentially expressed on leukemic cells relative to normal cells (tumor-associated antigens).
Searching for HLA class I ligandome of primary AMLs, multiple ΔNPM1-derived immunogenic peptides, have been identified, including AIQDLCLAV, AIQDLCVAV, CLAVEEVSL, LAVEEVSLR, AVEEVSLRK 9-mer, and CLAVEEVSLRK 11-mer, representative of the more common NPM1 mutation types. These peptides are able to efficiently bind to at least most common HLA types (A*02:01, A*03:01) which are often detected in the Caucasian population [111,112,113,114,115, 140,141,142]. Using yeast surface display, a human single-chain variable fragment (scFv) that specifically identifies the NPM1 mutant epitope/HLA-A2 complex but not HLA-A2 or HLA-A2 loaded with control peptides was generated and used to construct CAR T cells (Fig. 4). These engineered cells showed strong in vitro and in vivo activity against preclinical models of NPM1-mutated AML cells carrying NPM1-mutant/HLA-A2 complex but not against NPM1 wild-type/HLA-A2+ AML cells or HLA-A2 negative tumor cells [140]. More recently, memory-like NK cells armed with the same neoepitope-specific CAR showed strong activity against NPM1-mutated AML in absence of toxicity [143].
CD123 and CD33 are strongly expressed both in NPM1-mutated AML cells and healthy tissue. Thus, aiming to improve selectivity for leukemic cells while minimizing toxicity towards normal cells, a dual targeting model was exploited through Cytokine Induced Killer (CIK) cells co-expressing a first-generation low affinity anti-CD123 and an anti-CD33 as costimulatory receptor without activation signaling domains. This trans-signaling strategy could allow: i) low toxicity profile against CD123+ endothelial cells and HSPC, due to a reduced cell activation given by the suboptimal first-generation CAR signal; ii) no or low myelotoxicity against CD33+ HSPC cells, due to absence of CIK cell activation upon the sole costimulatory signal engagement; and iii) full CAR-CIK activation only against double expressing CD123+/CD33+ leukemic cells [144] (Fig. 5).
The rationale of CD123/CD33 dual targeting trans-signaling strategy is to induce a full cell activation against only CD123/CD33+ leukemic cells while reducing cell stimulation against CD33+ HSPCs and CD123+ endothelial cells [144].
Specific T cells for HLA-A*02:01-binding CLAVEEVSL have been searched in healthy individuals using peptide-HLA tetramers. Tetramer-positive CD8+ T cells were isolated and their activity towards primary AMLs investigated. The TCR was then isolated from a clone with high anti-leukemic reactivity and its capability to specifically recognize and lyse HLA-A*02:01-positive ΔNPM1 AML demonstrated after retroviral transduction of CD8+ and CD4+ T cells [145]. Moreover, T cells transduced with TCR for HLA-A*02:01-binding CLAVEEVSL efficiently killed AML cells and prolonged OS of NSG mice engrafted with HLA-A*02:01-positive NPM1-mutated OCI-AML3 human cells [145] (Fig. 4). Thus, CLAVEEVSL is a neoantigen that can be efficiently targeted on AML by ΔNPM1 TCR gene transfer. While such TCR gene-engineered T-cell therapy prove to be potent and safe, it must match the TCR haplotype restriction to HLA-A*02:01-positive patients, representing around 40% of Caucasian population. Moreover, HLA class I downregulation or loss of neoantigen expression could be a possible mechanism of immune escape from NPM1-mutated TCR gene-engineered T-cell therapy.
DLI using T cells derived from healthy donors and specifically directed against the NPM1-mutated neoantigen with the aim to elicit graft-versus-leukemia may be a therapeutic option in patients experiencing molecular relapse following allogeneic HSCT. Eliciting endogenous immune responses through vaccination with NPM1 neoantigens is unlikely to be effective in patients with high-burden newly diagnosed or relapsed AML but could be of benefit, possibly in combination with immune check-point inhibitors, to treat pre-emptively NPM1-mutated AML with persistent NPM1 transcripts or in molecular relapse.
Future perspectives
Molecular mechanisms underlying NPM1-mutated AML are still poorly understood. Endogenous tagging of wild-type and mutated NPM1 proteins followed by mass spectrometry may unravel their interactions with other partners and functions in the cytoplasm. How NPM1 mutants deregulate the HOX program remains also to be better defined. Moreover, all current experimental data are based upon the analysis of OCI-AML3 and IMS-M2 human AML cell lines that both carry the most frequent NPM1 mutation (i.e., mutation A). Whether similar results can be extended also to the rarer NPM1 variants remains to be determined. Clarifying these issues may lead to the development of new targeted therapeutic strategies.
Unfit NPM1-mutated AML patients relapsing after venetoclax-based regimens represent a medical need. The mechanisms of resistance to venetoclax and its use in combination with other drugs to prevent relapse should be better investigated. Menin inhibitors are emerging as the most promising agents for targeted therapy of NPM1-mutated AML. The ongoing trials will tell us which is the real impact of these compounds in NPM1-mutated AML and suggest which are the best combinations to maximize the clinical benefit. Menin inhibitors, alone or in combination with venetoclax or other agents, could be incorporated in the treatment algorithm, as that shown in Fig. 3A, to reduce or eradicate NPM1-related MRD, possibly as bridge to allo-HSCT, in eligible patients. Moreover, menin and XPO1 inhibitors have the potential to be used alone or in combination (e.g., with FLT3 inhibitors), at initial diagnosis, especially in patients who are older or unfit for intensive chemotherapy.
Identifying novel drugs for NPM1-mutated AML using synthetic lethality approaches are under way [146]. High-throughput screening technology [147] allows to screen a large number of compound libraries at a rate that may exceed a few thousand compounds per day or per week [148, 149]. Searching for new molecules able to re-localize or reduce the expression of the NPM1 mutated protein, we have established a microscopy-based screening strategy suitable to analyze hundreds selected drugs and compounds using high-throughput microscope technique and image analysis (Fig. 6). Among other compounds, we identified inhibitors with known re-localizing activity on NPM1 mutated protein, thus confirming the value of our experimental strategy (unpublished data).
A Workflow of microscopy-based screening strategy (created with BioRender.com). B Example of 96 well plate subjected to image and data processing (generated with ShinyHTM software). Arrows indicate results obtained with XPO1 inhibitors (KPT-185, KPT-276 and KPT-330). The higher number of points for selinexor (KPT-330) results from its use as a positive control.
References
Borer RA, Lehner CF, Eppenberger HM, Nigg EA. Major nucleolar proteins shuttle between nucleus and cytoplasm. Cell. 1989;56:379–90.
Grisendi S, Mecucci C, Falini B, Pandolfi PP. Nucleophosmin and cancer. Nat Rev Cancer. 2006;6:493–505.
Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, Pasqualucci L, et al. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med. 2005;352:254–66.
Falini B, Brunetti L, Sportoletti P, Martelli MP. NPM1-mutated acute myeloid leukemia: from bench to bedside. Blood. 2020;136:1707–21.
Alcalay M, Tiacci E, Bergomas R, Bigerna B, Venturini E, Minardi SP, et al. Acute myeloid leukemia bearing cytoplasmic nucleophosmin (NPMc+ AML) shows a distinct gene expression profile characterized by up-regulation of genes involved in stem-cell maintenance. Blood. 2005;106:899–902.
Garzon R, Garofalo M, Martelli MP, Briesewitz R, Wang L, Fernandez-Cymering C, et al. Distinctive microRNA signature of acute myeloid leukemia bearing cytoplasmic mutated nucleophosmin. Proc Natl Acad Sci USA. 2008;105:3945–50.
Ivey A, Hills RK, Simpson MA, Jovanovic JV, Gilkes A, Grech A, et al. Assessment of minimal residual disease in standard-risk AML. N Engl J Med. 2016;374:422–33.
Falini B, Bolli N, Shan J, Martelli MP, Liso A, Pucciarini A, et al. Both carboxy-terminus NES motif and mutated tryptophan(s) are crucial for aberrant nuclear export of nucleophosmin leukemic mutants in NPMc+ AML. Blood. 2006;107:4514–23.
Falini B, Bolli N, Liso A, Martelli MP, Mannucci R, Pileri S, et al. Altered nucleophosmin transport in acute myeloid leukaemia with mutated NPM1: molecular basis and clinical implications. Leukemia. 2009;23:1731–43.
Brunetti L, Gundry MC, Sorcini D, Guzman AG, Huang YH, Ramabadran R, et al. Mutant NPM1 maintains the leukemic state through HOX expression. Cancer Cell. 2018;34:499–512.e.
Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, et al. The 5th edition of the world health organization classification of haematolymphoid tumours: myeloid and histiocytic /dendritic neoplasms. Leukemia. 2022;36:1703–19.
Falini B, Brunetti L, Martelli MP. How I diagnose and treat NPM1-mutated AML. Blood. 2021;137:589–99.
Falini B, Sciabolacci S, Falini L, Brunetti L, Martelli MP. Diagnostic and therapeutic pitfalls in NPM1-mutated AML: notes from the field. Leukemia. 2021;35:3113–26.
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016;374:2209–21.
Cancer Genome Atlas Research N, Ley TJ, Miller C, Ding L, Raphael BJ, Mungall AJ, et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368:2059–74.
Aggarwal S. Targeted cancer therapies. Nat Rev Drug Discov. 2010;9:427–8.
Spotlight on cancer genomics. Nat Cancer. 2020;1:265–6.
Zhong L, Li Y, **ong L, Wang W, Wu M, Yuan T, et al. Small molecules in targeted cancer therapy: advances, challenges, and future perspectives. Signal Transduct Target Ther. 2021;6:201.
Lai C, Doucette K, Norsworthy K. Recent drug approvals for acute myeloid leukemia. J Hematol Oncol. 2019;12:100.
Estey E, Karp JE, Emadi A, Othus M, Gale RP. Recent drug approvals for newly diagnosed acute myeloid leukemia: gifts or a Trojan horse? Leukemia. 2020;34:671–81.
Zhang J, Yang PL, Gray NS. Targeting cancer with small molecule kinase inhibitors. Nat Rev Cancer. 2009;9:28–39.
Cela I, Di Matteo A, Federici L. Nucleophosmin in its interaction with ligands. Int J Mol Sci. 2020;21:4885.
Mitrea DM, Grace CR, Buljan M, Yun MK, Pytel NJ, Satumba J, et al. Structural polymorphism in the N-terminal oligomerization domain of NPM1. Proc Natl Acad Sci USA. 2014;111:4466–71.
Di Matteo A, Franceschini M, Chiarella S, Rocchio S, Travaglini-Allocatelli C, Federici L. Molecules that target nucleophosmin for cancer treatment: an update. Oncotarget. 2016;7:44821–40.
Federici L, Falini B. Nucleophosmin mutations in acute myeloid leukemia: a tale of protein unfolding and mislocalization. Protein Sci. 2013;22:545–56.
Qi W, Shakalya K, Stejskal A, Goldman A, Beeck S, Cooke L, et al. NSC348884, a nucleophosmin inhibitor disrupts oligomer formation and induces apoptosis in human cancer cells. Oncogene. 2008;27:4210–20.
Balusu R, Fiskus W, Rao R, Chong DG, Nalluri S, Mudunuru U, et al. Targeting levels or oligomerization of nucleophosmin 1 induces differentiation and loss of survival of human AML cells with mutant NPM1. Blood. 2011;118:3096–106.
Emmott E, Hiscox JA. Nucleolar targeting: the hub of the matter. EMBO Rep. 2009;10:231–8.
Mitrea DM, Cika JA, Guy CS, Ban D, Banerjee PR, Stanley CB, et al. Nucleophosmin integrates within the nucleolus via multi-modal interactions with proteins displaying R-rich linear motifs and rRNA. Elife. 2016;5:e13571.
Feric M, Vaidya N, Harmon TS, Mitrea DM, Zhu L, Richardson TM, et al. Coexisting liquid phases underlie nucleolar subcompartments. Cell. 2016;165:1686–97.
Mitrea DM, Cika JA, Stanley CB, Nourse A, Onuchic PL, Banerjee PR, et al. Self-interaction of NPM1 modulates multiple mechanisms of liquid-liquid phase separation. Nat Commun. 2018;9:842.
Riback JA, Zhu L, Ferrolino MC, Tolbert M, Mitrea DM, Sanders DW, et al. Composition-dependent thermodynamics of intracellular phase separation. Nature. 2020;581:209–14.
Grummitt CG, Townsley FM, Johnson CM, Warren AJ, Bycroft M. Structural consequences of nucleophosmin mutations in acute myeloid leukemia. J Biol Chem. 2008;283:23326–32.
Mukherjee H, Chan KP, Andresen V, Hanley ML, Gjertsen BT, Myers AG. Interactions of the natural product (+)-avrainvillamide with nucleophosmin and exportin-1 Mediate the cellular localization of nucleophosmin and its AML-associated mutants. ACS Chem Biol. 2015;10:855–63.
Wulff JE, Siegrist R, Myers AG. The natural product avrainvillamide binds to the oncoprotein nucleophosmin. J Am Chem Soc. 2007;129:14444–51.
Andresen V, Erikstein BS, Mukherjee H, Sulen A, Popa M, Sornes S, et al. Anti-proliferative activity of the NPM1 interacting natural product avrainvillamide in acute myeloid leukemia. Cell Death Dis. 2016;7:e2497.
Yang K, Wang M, Zhao Y, Sun X, Yang Y, Li X, et al. A redox mechanism underlying nucleolar stress sensing by nucleophosmin. Nat Commun. 2016;7:13599.
Falini B, Brunetti L, Martelli MP. Dactinomycin in NPM1-mutated acute myeloid leukemia. N Engl J Med. 2015;373:1180–2.
Falini B, Gionfriddo I, Cecchetti F, Ballanti S, Pettirossi V, Martelli MP. Acute myeloid leukemia with mutated nucleophosmin (NPM1): any hope for a targeted therapy? Blood Rev. 2011;25:247–54.
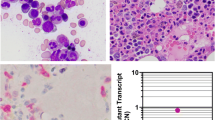
Gionfriddo I, Brunetti L, Mezzasoma F, Milano F, Cardinali V, Ranieri R, et al. Dactinomycin induces complete remission associated with nucleolar stress response in relapsed/refractory NPM1-mutated AML. Leukemia. 2021;35:2552–62.
Brodska B, Otevrelova P, Salek C, Fuchs O, Gasova Z, Kuzelova K. High PD-L1 expression predicts for worse outcome of leukemia patients with concomitant NPM1 and FLT3 mutations. Int J Mol Sci. 2019;20:2823.
Burger K, Muhl B, Harasim T, Rohrmoser M, Malamoussi A, Orban M, et al. Chemotherapeutic drugs inhibit ribosome biogenesis at various levels. J Biol Chem. 2010;285:12416–25.
Martelli MP, Gionfriddo I, Mezzasoma F, Milano F, Pierangeli S, Mulas F, et al. Arsenic trioxide and all-trans retinoic acid target NPM1 mutant oncoprotein levels and induce apoptosis in NPM1-mutated AML cells. Blood. 2015;125:3455–65.
Wu HC, Rerolle D, Berthier C, Hleihel R, Sakamoto T, Quentin S, et al. Actinomycin D targets NPM1c-primed mitochondria to restore PML-driven senescence in AML therapy. Cancer Discov. 2021;11:3198–213.
El Hajj H, Dassouki Z, Berthier C, Raffoux E, Ades L, Legrand O, et al. Retinoic acid and arsenic trioxide trigger degradation of mutated NPM1, resulting in apoptosis of AML cells. Blood. 2015;125:3447–54.
Yi S, Wen L, He J, Wang Y, Zhao F, Zhao J, et al. Deguelin, a selective silencer of the NPM1 mutant, potentiates apoptosis and induces differentiation in AML cells carrying the NPM1 mutation. Ann Hematol. 2015;94:201–10.
Zhang X, Zhao Z, Yi S, Wen L, He J, Hu J, et al. Deguelin induced differentiation of mutated NPM1 acute myeloid leukemia in vivo and in vitro. Anticancer Drugs. 2017;28:723–38.
Chi HT, Ly BT, Vu HA, Sato Y, Dung PC, **nh PT. Down-regulated expression of NPM1 in IMS-M2 cell line by (-)-epigallocatechin-3-gallate. Asian Pac J Trop Biomed. 2014;4:570–4.
Skayneh H, Jishi B, Hleihel R, Hamie M, El Hajj R, Deleuze-Masquefa C, et al. EAPB0503, an imidazoquinoxaline derivative modulates SENP3/ARF mediated SUMOylation, and induces NPM1c degradation in NPM1 mutant AML. Int J Mol Sci. 2022;23:3421.
Nabbouh AI, Hleihel RS, Saliba JL, Karam MM, Hamie MH, Wu HJM, et al. Imidazoquinoxaline derivative EAPB0503: a promising drug targeting mutant nucleophosmin 1 in acute myeloid leukemia. Cancer. 2017;123:1662–73.
Sun X, Gao H, Yang Y, He M, Wu Y, Song Y, et al. PROTACs: great opportunities for academia and industry. Signal Transduct Target Ther. 2019;4:64.
He Y, Khan S, Huo Z, Lv D, Zhang X, Liu X, et al. Proteolysis targeting chimeras (PROTACs) are emerging therapeutics for hematologic malignancies. J Hematol Oncol. 2020;13:103.
Fornerod M, Ohno M, Yoshida M, Mattaj IW. CRM1 is an export receptor for leucine-rich nuclear export signals. Cell. 1997;90:1051–60.
Fukuda M, Asano S, Nakamura T, Adachi M, Yoshida M, Yanagida M, et al. CRM1 is responsible for intracellular transport mediated by the nuclear export signal. Nature. 1997;390:308–11.
Kudo N, Wolff B, Sekimoto T, Schreiner EP, Yoneda Y, Yanagida M, et al. Leptomycin B inhibition of signal-mediated nuclear export by direct binding to CRM1. Exp Cell Res. 1998;242:540–7.
Newlands ES, Rustin GJ, Brampton MH. Phase I trial of elactocin. Br J Cancer. 1996;74:648–9.
Sun Q, Chen X, Zhou Q, Burstein E, Yang S, Jia D. Inhibiting cancer cell hallmark features through nuclear export inhibition. Signal Transduct Target Ther. 2016;1:16010.
Garzon R, Savona M, Baz R, Andreeff M, Gabrail N, Gutierrez M, et al. A phase 1 clinical trial of single-agent selinexor in acute myeloid leukemia. Blood. 2017;129:3165–74.
Bhatnagar B, Zhao Q, Mims AS, Vasu S, Behbehani GK, Larkin K, et al. Selinexor in combination with decitabine in patients with acute myeloid leukemia: results from a phase 1 study. Leuk Lymphoma. 2020;61:387–96.
Fiedler W, Chromik J, Amberg S, Kebenko M, Thol F, Schlipfenbacher V, et al. A Phase II study of selinexor plus cytarabine and idarubicin in patients with relapsed/refractory acute myeloid leukaemia. Br J Haematol. 2020;190:e169–73.
Sweet K, Bhatnagar B, Dohner H, Donnellan W, Frankfurt O, Heuser M, et al. A 2:1 randomized, open-label, phase II study of selinexor vs. physician’s choice in older patients with relapsed or refractory acute myeloid leukemia. Leuk Lymphoma. 2021;62:3192–203.
Hing ZA, Fung HY, Ranganathan P, Mitchell S, El-Gamal D, Woyach JA, et al. Next-generation XPO1 inhibitor shows improved efficacy and in vivo tolerability in hematological malignancies. Leukemia. 2016;30:2364–72.
Etchin J, Berezovskaya A, Conway AS, Galinsky IA, Stone RM, Baloglu E, et al. KPT-8602, a second-generation inhibitor of XPO1-mediated nuclear export, is well tolerated and highly active against AML blasts and leukemia-initiating cells. Leukemia. 2017;31:143–50.
Fischer MA, Friedlander SY, Arrate MP, Chang H, Gorska AE, Fuller LD, et al. Venetoclax response is enhanced by selective inhibitor of nuclear export compounds in hematologic malignancies. Blood Adv. 2020;4:586–98.
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med. 2020;383:617–29.
Jones CL, Stevens BM, D’Alessandro A, Reisz JA, Culp-Hill R, Nemkov T, et al. Inhibition of amino acid metabolism selectively targets human leukemia stem cells. Cancer Cell. 2018;34:724–40.
Pollyea DA, Stevens BM, Jones CL, Winters A, Pei S, Minhajuddin M, et al. Venetoclax with azacitidine disrupts energy metabolism and targets leukemia stem cells in patients with acute myeloid leukemia. Nat Med. 2018;24:1859–66.
Bisaillon R, Moison C, Thiollier C, Krosl J, Bordeleau ME, Lehnertz B, et al. Genetic characterization of ABT-199 sensitivity in human AML. Leukemia. 2020;34:63–74.
Kontro M, Kumar A, Majumder MM, Eldfors S, Parsons A, Pemovska T, et al. HOX gene expression predicts response to BCL-2 inhibition in acute myeloid leukemia. Leukemia. 2017;31:301–9.
Lachowiez CA, Loghavi S, Kadia TM, Daver N, Borthakur G, Pemmaraju N, et al. Outcomes of older patients with NPM1-mutated AML: current treatments and the promise of venetoclax-based regimens. Blood Adv. 2020;4:1311–20.
DiNardo CD, Tiong IS, Quaglieri A, MacRaild S, Loghavi S, Brown FC, et al. Molecular patterns of response and treatment failure after frontline venetoclax combinations in older patients with AML. Blood. 2020;135:791–803.
Konopleva M, Thirman MJ, Pratz KW, Garcia JS, Recher C, Pullarkat V, et al. Impact of F LT3 mutation on outcomes after venetoclax and azacitidine for patients with treatment-naive acute myeloid leukemia. Clin Cancer Res. 2022;28:2744–52.
Stahl M, Menghrajani K, Derkach A, Chan A, **ao W, Glass J, et al. Clinical and molecular predictors of response and survival following venetoclax therapy in relapsed/refractory AML. Blood Adv. 2021;5:1552–64.
Labrador J, Saiz-Rodriguez M, de Miguel D, de Laiglesia A, Rodriguez-Medina C, Vidriales MB, et al. Use or venetoclax in patients with relapsed or refractory acute myeloid leukemia: the PETHEMA registry experience. Cancers. 2022;14:1734.
Wang YW, Tsai CH, Lin CC, Tien FM, Chen YW, Lin HY, et al. Cytogenetics and mutations could predict outcome in relapsed and refractory acute myeloid leukemia patients receiving BCL-2 inhibitor venetoclax. Ann Hematol. 2020;99:501–11.
Winters AC, Gutman JA, Purev E, Nakic M, Tobin J, Chase S, et al. Real-world experience of venetoclax with azacitidine for untreated patients with acute myeloid leukemia. Blood Adv. 2019;3:2911–9.
Wei AH, Strickland SA Jr., Hou JZ, Fiedler W, Lin TL, Walter RB, et al. Venetoclax combined with low-dose cytarabine for previously untreated patients with acute myeloid leukemia: results from a phase Ib/II Study. J Clin Oncol. 2019;37:1277–84.
Wei AH, Montesinos P, Ivanov V, DiNardo CD, Novak J, Laribi K, et al. Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: a phase 3 randomized placebo-controlled trial. Blood. 2020;135:2137–45.
Chua CC, Roberts AW, Reynolds J, Fong CY, Ting SB, Salmon JM, et al. Chemotherapy and venetoclax in elderly acute myeloid leukemia trial (CAVEAT): a Phase Ib dose-escalation study of venetoclax combined with modified intensive chemotherapy. J Clin Oncol. 2020;38:3506–17.
DiNardo CD, Lachowiez CA, Takahashi K, Loghavi S, **ao L, Kadia T, et al. Venetoclax combined with FLAG-IDA induction and consolidation in newly diagnosed and relapsed or refractory acute myeloid leukemia. J Clin Oncol. 2021;39:2768–78.
Chua CC, Hammond D, Kent A, Tiong IS, Konopleva MY, Pollyea DA, et al. Treatment-free remission after ceasing venetoclax-based therapy in patients with acute myeloid leukemia. Blood Adv. 2022;6:3879–83.
Tiong IS, Dillon R, Ivey A, Teh TC, Nguyen P, Cummings N, et al. Venetoclax induces rapid elimination of NPM1 mutant measurable residual disease in combination with low-intensity chemotherapy in acute myeloid leukaemia. Br J Haematol. 2021;192:1026–30.
Carter BZ, Tao W, Mak PY, Ostermann LB, Mak D, McGeehan G, et al. Menin inhibition decreases Bcl-2 and synergizes with venetoclax in NPM1/FLT3-mutated AML. Blood. 2021;138:1637–41.
Fiskus W, Boettcher S, Daver N, Mill CP, Sasaki K, Birdwell CE, et al. Effective Menin inhibitor-based combinations against AML with MLL rearrangement or NPM1 mutation (NPM1c). Blood Cancer J. 2022;12:5.
Zhu HH, Qian JJ, Sun WJ, You LS, Wang QQ, Naranmandura H, et al. Venetoclax and arsenic showed synergistic anti-leukemia activity in vitro and in vivo for acute myeloid leukemia with the NPM1 mutation. Am J Hematol. 2020;95:E55–7.
Matkar S, Thiel A, Hua X. Menin: a scaffold protein that controls gene expression and cell signaling. Trends Biochem Sci. 2013;38:394–402.
Chandrasekharappa SC, Guru SC, Manickam P, Olufemi SE, Collins FS, Emmert-Buck MR, et al. Positional cloning of the gene for multiple endocrine neoplasia-type 1. Science. 1997;276:404–7.
Hughes CM, Rozenblatt-Rosen O, Milne TA, Copeland TD, Levine SS, Lee JC, et al. Menin associates with a trithorax family histone methyltransferase complex and with the hoxc8 locus. Mol Cell. 2004;13:587–97.
Argiropoulos B, Humphries RK. Hox genes in hematopoiesis and leukemogenesis. Oncogene. 2007;26:6766–76.
Spencer DH, Young MA, Lamprecht TL, Helton NM, Fulton R, O’Laughlin M, et al. Epigenomic analysis of the HOX gene loci reveals mechanisms that may control canonical expression patterns in AML and normal hematopoietic cells. Leukemia. 2015;29:1279–89.
Oka M, Mura S, Otani M, Miyamoto Y, Nogami J, Maehara K, et al. Chromatin-bound CRM1 recruits SET-Nup214 and NPM1c onto HOX clusters causing aberrant HOX expression in leukemia cells. Elife. 2019;8:e46667.
Kuhn MW, Song E, Feng Z, Sinha A, Chen CW, Deshpande AJ, et al. Targeting chromatin regulators inhibits leukemogenic geneeExpression in NPM1 mutant leukemia. Cancer Discov. 2016;6:1166–81.
Grembecka J, He S, Shi A, Purohit T, Muntean AG, Sorenson RJ, et al. Menin-MLL inhibitors reverse oncogenic activity of MLL fusion proteins in leukemia. Nat Chem Biol. 2012;8:277–84.
Ozyerli-Goknar E, Nizamuddin S, Timmers HTM. A box of chemistry to inhibit the MEN1 tumor suppressor gene promoting leukemia. ChemMedChem. 2021;16:1391–402.
Klossowski S, Miao H, Kempinska K, Wu T, Purohit T, Kim E, et al. Menin inhibitor MI-3454 induces remission in MLL1-rearranged and NPM1-mutated models of leukemia. J Clin Investig. 2020;130:981–97.
Uckelmann HJ, Kim SM, Wong EM, Hatton C, Giovinazzo H, Gadrey JY, et al. Therapeutic targeting of preleukemia cells in a mouse model of NPM1 mutant acute myeloid leukemia. Science. 2020;367:586–90.
Gundry MC, Goodell MA, Brunetti L. It’s all about MEis: Menin-MLL inhibition eradicates NPM1-mutated and MLL-rearranged acute leukemias in mice. Cancer Cell. 2020;37:267–9.
Dzama MM, Steiner M, Rausch J, Sasca D, Schonfeld J, Kunz K, et al. Synergistic targeting of FLT3 mutations in AML via combined menin-MLL and FLT3 inhibition. Blood. 2020;136:2442–56.
Miao H, Kim E, Chen D, Purohit T, Kempinska K, Ropa J, et al. Combinatorial treatment with menin and FLT3 inhibitors induces complete remission in AML models with activating FLT3 mutations. Blood. 2020;136:2958–63.
Issa GC, Ravandi F, DiNardo CD, Jabbour E, Kantarjian HM, Andreeff M. Therapeutic implications of menin inhibition in acute leukemias. Leukemia. 2021;35:2482–95.
Swaminathan M, Bourgeois W, Armstrong SA, Wang ES. Menin inhibitors in acute myeloid leukemia-What does the future hold? Cancer J. 2022;28:62–6.
Krivtsov AV, Evans K, Gadrey JY, Eschle BK, Hatton C, Uckelmann HJ, et al. A Menin-MLL inhibitor induces specific chromatin changes and eradicates disease in models of MLL-rearranged leukemia. Cancer Cell. 2019;36:660–73.e11.
Cremer A, Ellegast JM, Alexe G, Frank ES, Ross L, Chu SH, et al. Resistance mechanisms to SYK inhibition in acute myeloid leukemia. Cancer Discov. 2020;10:214–31.
Walker AR, Byrd JC, Blachly JS, Bhatnagar B, Mims AS, Orwick S, et al. Entospletinib in combination with induction chemotherapy in previously ontreated acute myeloid leukemia: response and predictive significance of HOXA9 and MEIS1 expression. Clin Cancer Res. 2020;26:5852–9.
Mohr S, Doebele C, Comoglio F, Berg T, Beck J, Bohnenberger H, et al. Hoxa9 and Meis1 cooperatively induce addiction to Syk signaling by suppressing miR-146a in acute myeloid leukemia. Cancer Cell. 2017;31:549–62.e11.
De Propris MS, Raponi S, Diverio D, Milani ML, Meloni G, Falini B, et al. High CD33 expression levels in acute myeloid leukemia cells carrying the nucleophosmin (NPM1) mutation. Haematologica. 2011;96:1548–51.
Perriello VM, Gionfriddo I, Rossi R, Milano F, Mezzasoma F, Marra A, et al. CD123 Is consistently expressed on NPM1-mutated AML Cells. Cancers. 2021;13:496.
Martelli MP, Pettirossi V, Thiede C, Bonifacio E, Mezzasoma F, Cecchini D, et al. CD34+ cells from AML with mutated NPM1 harbor cytoplasmic mutated nucleophosmin and generate leukemia in immunocompromised mice. Blood. 2010;116:3907–22.
Sportoletti P, Varasano E, Rossi R, Mupo A, Tiacci E, Vassiliou G, et al. Mouse models of NPM1-mutated acute myeloid leukemia: biological and clinical implications. Leukemia. 2015;29:269–78.
Liso A, Bogliolo A, Freschi V, Martelli MP, Pileri SA, Santodirocco M, et al. In human genome, generation of a nuclear export signal through duplication appears unique to nucleophosmin (NPM1) mutations and is restricted to AML. Leukemia. 2008;22:1285–9.
Liso A, Colau D, Benmaamar R, De Groot A, Martin W, Benedetti R, et al. Nucleophosmin leukaemic mutants contain C-terminus peptides that bind HLA class I molecules. Leukemia. 2008;22:424–6.
Narayan R, Olsson N, Wagar LE, Medeiros BC, Meyer E, Czerwinski D, et al. Acute myeloid leukemia immunopeptidome reveals HLA presentation of mutated nucleophosmin. PLoS ONE. 2019;14:e0219547.
van der Lee DI, Reijmers RM, Honders MW, Hagedoorn RS, de Jong RC, Kester MG, et al. Mutated nucleophosmin 1 as immunotherapy target in acute myeloid leukemia. J Clin Investig. 2019;129:774–85.
Kuzelova K, Brodska B, Fuchs O, Dobrovolna M, Soukup P, Cetkovsky P. Altered HLA class I profile associated with type A/D nucleophosmin mutation points to possible anti-nucleophosmin immune response in acute myeloid leukemia. PLoS ONE. 2015;10:e0127637.
Forghieri F, Riva G, Lagreca I, Barozzi P, Vallerini D, Morselli M, et al. Characterization and dynamics of specific T cells against nucleophosmin-1 (NPM1)-mutated peptides in patients with NPM1-mutated acute myeloid leukemia. Oncotarget. 2019;10:869–82.
Hofmann S, Gotz M, Schneider V, Guillaume P, Bunjes D, Dohner H, et al. Donor lymphocyte infusion induces polyspecific CD8(+) T-cell responses with concurrent molecular remission in acute myeloid leukemia with NPM1 mutation. J Clin Oncol. 2013;31:e44–7.
Greiner J, Schneider V, Schmitt M, Gotz M, Dohner K, Wiesneth M, et al. Immune responses against the mutated region of cytoplasmatic NPM1 might contribute to the favorable clinical outcome of AML patients with NPM1 mutations (NPM1mut). Blood. 2013;122:1087–8.
Aldoss I, Nakamura R, Yang D, Salhotra A, Stein AS, Pullarkat V, et al. Favorable outcomes for allogeneic hematopoietic cell transplantation in elderly patients with NPM1-mutated and FLT3-ITD-negative acute myeloid leukemia. Bone Marrow Transplant. 2020;55:473–5.
Laszlo GS, Estey EH, Walter RB. The past and future of CD33 as therapeutic target in acute myeloid leukemia. Blood Rev. 2014;28:143–53.
Hills RK, Castaigne S, Appelbaum FR, Delaunay J, Petersdorf S, Othus M, et al. Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: a meta-analysis of individual patient data from randomised controlled trials. Lancet Oncol. 2014;15:986–96.
Fournier E, Duployez N, Ducourneau B, Raffoux E, Turlure P, Caillot D, et al. Mutational profile and benefit of gemtuzumab ozogamicin in acute myeloid leukemia. Blood. 2020;135:542–6.
Kapp-Schwoerer S, Weber D, Corbacioglu A, Gaidzik VI, Paschka P, Kronke J, et al. Impact of gemtuzumab ozogamicin on MRD and relapse risk in patients with NPM1-mutated AML: results from the AMLSG 09-09 trial. Blood. 2020;136:3041–50.
Schlenk RF, Paschka P, Krzykalla J, Weber D, Kapp-Schwoerer S, Gaidzik VI, et al. Gemtuzumab Ozogamicin in NPM1-mutated acute myeloid leukemia: early results from the prospective randomized AMLSG 09-09 Phase III study. J Clin Oncol. 2020;38:623–32.
Pemmaraju N, Konopleva M. Approval of tagraxofusp-erzs for blastic plasmacytoid dendritic cell neoplasm. Blood Adv. 2020;4:4020–7.
Greiner J, Hofmann S, Schmitt M, Gotz M, Wiesneth M, Schrezenmeier H, et al. Acute myeloid leukemia with mutated nucleophosmin 1: an immunogenic acute myeloid leukemia subtype and potential candidate for immune checkpoint inhibition. Haematologica. 2017;102:e499–501.
Dufva O, Polonen P, Bruck O, Keranen MAI, Klievink J, Mehtonen J, et al. Immunogenomic landscape of hematological malignancies. Cancer Cell. 2020;38:424–8.
Lines JL, Pantazi E, Mak J, Sempere LF, Wang L, O’Connell S, et al. VISTA is an immune checkpoint molecule for human T cells. Cancer Res. 2014;74:1924–32.
Greiner J, Goetz M, Schuler PJ, Bulach C, Hofmann S, Schrezenmeier H, et al. Enhanced stimulation of antigen-specific immune responses against nucleophosmin 1 mutated acute myeloid leukaemia by an anti-programmed death 1 antibody. 2022. Br J Haematol. https://doi.org/10.1111/bjh.18326.
Vadakekolathu J, Minden MD, Hood T, Church SE, Reeder S, Altmann H, et al. Immune landscapes predict chemotherapy resistance and immunotherapy response in acute myeloid leukemia. Sci Transl Med. 2020;12:eaaz0463.
Damotte D, Warren S, Arrondeau J, Boudou-Rouquette P, Mansuet-Lupo A, Biton J, et al. The tumor inflammation signature (TIS) is associated with anti-PD-1 treatment benefit in the CERTIM pan-cancer cohort. J Transl Med. 2019;17:357.
Tripodo C, Burocchi A, Piccaluga PP, Chiodoni C, Portararo P, Cappetti B, et al. Persistent immune stimulation exacerbates genetically driven myeloproliferative disorders via stromal remodeling. Cancer Res. 2017;77:3685–99.
Daver N, Garcia-Manero G, Basu S, Boddu PC, Alfayez M, Cortes JE, et al. Efficacy, safety, and biomarkers of response to azacitidine and nivolumab in relapsed/refractory acute myeloid leukemia: a nonrandomized, open-label, Phase II study. Cancer Discov. 2019;9:370–83.
Goswami M, Gui G, Dillon LW, Lindblad KE, Thompson J, Valdez J, et al. Pembrolizumab and decitabine for refractory or relapsed acute myeloid leukemia. J Immunother Cancer. 2022;10:e003392.
Saxena K, Herbrich SM, Pemmaraju N, Kadia TM, DiNardo CD, Borthakur G, et al. A phase 1b/2 study of azacitidine with PD-L1 antibody avelumab in relapsed/refractory acute myeloid leukemia. Cancer. 2021;127:3761–71.
Vago L, Gojo I. Immune escape and immunotherapy of acute myeloid leukemia. J Clin Invest. 2020;130:1552–64.
Chen X, Pan X, Zhang W, Guo H, Cheng S, He Q, et al. Epigenetic strategies synergize with PD-L1/PD-1 targeted cancer immunotherapies to enhance antitumor responses. Acta Pharm Sin B. 2020;10:723–33.
Zeidner JF, Vincent BG, Ivanova A, Moore D, McKinnon KP, Wilkinson AD, et al. Phase II trial of pembrolizumab after high-dose cytarabine in relapsed/refractory acute myeloid leukemia. Blood Cancer Discov. 2021;2:616–29.
Lee JB, Khan DH, Hurren R, Xu M, Na Y, Kang H, et al. Venetoclax enhances T cell-mediated antileukemic activity by increasing ROS production. Blood. 2021;138:234–45.
Kohlhapp FJ, Haribhai D, Mathew R, Duggan R, Ellis PA, Wang R, et al. Venetoclax increases intratumoral effector T cells and antitumor efficacy in combination with immune checkpoint blockade. Cancer Discov. 2021;11:68–79.
**e G, Ivica NA, Jia B, Li Y, Dong H, Liang Y, et al. CAR-T cells targeting a nucleophosmin neoepitope exhibit potent specific activity in mouse models of acute myeloid leukaemia. Nat Biomed Eng. 2021;5:399–413.
Greiner J, Ono Y, Hofmann S, Schmitt A, Mehring E, Gotz M, et al. Mutated regions of nucleophosmin 1 elicit both CD4(+) and CD8(+) T-cell responses in patients with acute myeloid leukemia. Blood. 2012;120:1282–9.
Kuzelova K, Brodska B, Schetelig J, Rollig C, Racil Z, Walz JS, et al. Association of HLA class I type with prevalence and outcome of patients with acute myeloid leukemia and mutated nucleophosmin. PLoS ONE. 2018;13:e0204290.
Dong H, Ham JD, Hu G, **e G, Vergara J, Liang Y, et al. Memory-like NK cells armed with a neoepitope-specific CAR exhibit potent activity against NPM1 mutated acute myeloid leukemia. Proc Natl Acad Sci USA. 2022;119:e2122379119.
Perriello VM, Rotiroti RM, Pisani I, Alberti G, Pianigiani G, Rossi R, et al. CD123 and CD33 co-targeting by balanced signaling on CAR-CIK cells reduces potential off-target toxicity while preserving the anti-leukemic activity of acute myeloid leukemia. Blood. 2021;138:1699.
van der Lee DI, Koutsoumpli G, Reijmers RM, Honders MW, de Jong RCM, Remst DFG, et al. An HLA-A*11:01-binding neoantigen from mutated NPM1 as target for TCR gene therapy in AML. Cancers. 2021;13:5390.
Zhang B, Tang C, Yao Y, Chen X, Zhou C, Wei Z, et al. The tumor therapy landscape of synthetic lethality. Nat Commun. 2021;12:1275.
Carnero A. High throughput screening in drug discovery. Clin Transl Oncol. 2006;8:482–90.
Hoelder S, Clarke PA, Workman P. Discovery of small molecule cancer drugs: successes, challenges and opportunities. Mol Oncol. 2012;6:155–76.
Coussens NP, Braisted JC, Peryea T, Sittampalam GS, Simeonov A, Hall MD. Small-molecule screens: a gateway to cancer therapeutic agents with case studies of Food and Drug Administration-approved drugs. Pharm Rev. 2017;69:479–96.
Acknowledgements
This work has been supported by the European Research Council (ERC Adv grant 2016 n. 740230 to BF and ERC Cons grant 2016 n. 725725 to MPM) and the Italian Association for Cancer research (AIRC grant n. 23604 to BF and grant Start-Up 2019 n. 22895 to LB).
Author information
Authors and Affiliations
Contributions
BF had the original idea and wrote and supervised the work together with MPM and LB. RR, GP, SP, FM and IG contributed to the drug screening and to wrote the section of molecular therapeutic targeting of NPM1-mutated AML. SS take care of NPM1-mutated AML patients treated with venetoclax. VC followed the trial on actinomycin D in NPM1-mutated AML. VMP and AM contributed to write the section on immunotherapy of NPM1-mutated AML.
Corresponding author
Ethics declarations
Competing interests
MPM declares honoraria from Rasna Therapeutics, Inc for scientific advisor activities and serves as consultant for scientific advisory boards of Abbvie, Amgen, Celgene, Janssen, Novartis, Pfizer and Jazz Pharmaceuticals. LB declares consultancy at scientific advisory boards for Abbvie and Amgen. BF licensed a patent on NPM1 mutants (n. 102004901256449) and declares honoraria from Rasna Therapeutics, Inc for scientific advisor activities. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ranieri, R., Pianigiani, G., Sciabolacci, S. et al. Current status and future perspectives in targeted therapy of NPM1-mutated AML. Leukemia 36, 2351–2367 (2022). https://doi.org/10.1038/s41375-022-01666-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-022-01666-2
- Springer Nature Limited
This article is cited by
-
Arsenic trioxide: applications, mechanisms of action, toxicity and rescue strategies to date
Archives of Pharmacal Research (2024)
-
Biomarkers as targets for CAR-T/NK cell therapy in AML
Biomarker Research (2023)
-
Causal linkage of presence of mutant NPM1 to efficacy of novel therapeutic agents against AML cells with mutant NPM1
Leukemia (2023)
-
Targeting the undruggable: menin inhibitors ante portas
Journal of Cancer Research and Clinical Oncology (2023)
-
Targeting of epigenetic co-dependencies enhances anti-AML efficacy of Menin inhibitor in AML with MLL1-r or mutant NPM1
Blood Cancer Journal (2023)