Abstract
Purpose
Osteoid Osteomas (OO) and Osteoblastomas (OB) are relatively rare benign bone lesions necessitating effective treatment to alleviate associated pain and functional limitations. Radiofrequency Thermal Ablation (RFA) and Focused Ultrasound (MRgFUS) have emerged as minimally invasive techniques for their management. This study aims to retrospectively evaluate and compare the selection criteria for these two treatments.
Methods
A retrospective analysis was conducted on 102 cases of OO/OB treated between January 2013 and July 2020. Eight potential factors influencing treatment selection were assessed, including lesion characteristics and proximity to critical structures. Statistical regression using the Wilcoxon test was performed to compare treatment outcomes.
Results
Significant differences were observed between the RFA and MRgFUS groups concerning the proximity of vascular-nervous structures to the lesion (p = 0.001), lesion depth (p < 0.001), nidus size (p < 0.001), and the presence of an acoustic window (p < 0.001). Additionally, lesion depth (p < 0.001), sclerosis (p = 0.03), and nidus size (p = 0.02) were significant factors.
Conclusions
Our findings underscore the importance of considering multiple factors when selecting a treatment modality for OO and OB. While both RFA and MRgFUS offer comparable efficacy, careful assessment of patient-specific features, particularly the presence of an acoustic window and sclerosis, should guide treatment decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoid Osteomas (OO) and Osteoblastomas (OB) are relatively rare benign bone lesions, accounting for approximately 12% and 3%, respectively, of all benign skeletal tumors [1,2,3]. While these lesions are infrequent, they are often encountered in the first three decades of life. Despite their benign nature, they necessitate treatment due to the significant associated pain symptoms, which can lead to considerable functional limitations and adversely affect the quality of life in young patients.
Historically, surgical resection or curettage were the primary therapeutic options [4, 5]. However, while effective, these techniques often required surgery with resection margins larger than the actual size of the lesion, prolonged hospital stays, rehabilitation, and increased risk of pathological fractures. Consequently, minimally invasive techniques have gained prominence in recent years as the preferred treatments for these lesions [6,7,8]. Among these, Radiofrequency Thermal Ablation (RFA) and Magnetic Resonance-guided Focused Ultrasound (MRgFUS) have emerged as the most utilized [9, 10], with RFA now considered the gold standard [11,12,13,14]. Both techniques have demonstrated high efficacy, reduced complication rates, and minimal invasiveness [15, 16].
Using both RFA and MRgFUS in our clinical practice, we undertook a retrospective evaluation to assess the selection criteria guiding the choice between these treatments and determine whether statistically significant differences exist between them.
We examined a series of variables, including the intra/extra-articular localization of the lesion, maximum nidus size, presence of intranidal calcifications, type of sclerosis, proximity to critical vascular-nervous structures, maximum extension of intraosseous edema, and presence of an adequate acoustic window. It is important to note that the evaluations of the proposed selection criteria are influenced by the experience and preferences of the operator performing the procedure. With the exception of the presence of an acoustic window, the other parameters assessed may not absolutely preclude the use of radiofrequency thermal ablation (RFA) over magnetic resonance-guided focused ultrasound (MRgFUS), but rather reflect individual clinical decisions based on subjective interpretation of the imaging data.
Methods
The objective of our study was to evaluate the selection criteria for determining the optimal treatment modality, either RFA or MRgFUS, for Osteoid Osteomas and/or Osteoblastomas, considering the cost/benefit ratio and the statistical significance of these criteria.
We retrospectively analyzed 102 cases of OO/OB treated in our Radiology Department between January 2013 and July 2020 using RFA under CT guidance or MRgFUS. Of the 102 patients evaluated, 82 had Osteoid Osteomas and 20 had Osteoblastomas.
We performed 51 MRgFUS treatments and 51 RFA treatments. However, ten patients opted for RFA despite the recommended alternative, and thus, they were excluded from the statistical analysis (Table 1).
Eight potential factors influencing treatment selection for these lesions were evaluated (Table 2):
-
1.
Maximum nidus diameter (mm)
-
2.
Nidal depth from bone surface (mm)
-
3.
Presence of calcifications within the nidus (yes/no)
-
4.
Perilesional sclerosis (absence, non-compact, compact)
-
5.
Intra- or extra-articular lesion localization (yes/no)
-
6.
Maximum extension of bone edema surrounding the lesion (mm)
-
7.
Proximity of critical vascular-nervous structures to the lesion (≤ 1 cm cutoff: yes/no)
-
8.
Acoustic Window, defined as the absence of structures obstructing the progression of the Focused Ultrasound beam (yes/no).
All variables were assessed via CT and/or MRI prior to treatment; For RF ablation, a 320-Slices Spiral CT Scanner (TAC Toshiba Aquilion One) was utilized, while a 3 Tesla MRI system (GE) was used for HIFU treatment. The parameters were evaluated by experienced operators trained in the respective techniques.
The inclusion criteria for patient selection included a confirmed diagnosis of OO/OB and treatment with either RFA or MRgFUS during the specified period.
Statistical analysis
Statistical analysis involved calculating frequency and dispersion indices and performing statistical regression using the Wilcoxon test. The patients treated were divided into three groups for statistical comparison: Group A (patients treated with MRgFUS), Group B (patients treated with RFA), and Group C, which evaluated the statistical significance of parameters arbitrarily defined by the operator to justify RFA treatment even in the presence of an acoustic window: compact sclerosis and non-compact sclerosis with depth > 7 mm.
Results
Of the 102 patients evaluated, 82 were diagnosed with Osteoid Osteomas and 20 with Osteoblastomas. Diagnosis was obtained through a combination of clinical-radiological assessment and biopsy in cases where necessary for confirmation.
The study included both Osteoid Osteomas and Osteoblastomas to encompass a broader spectrum of benign bone lesions. While the type of tumor could indeed influence the choice of treatment modality, our aim was to evaluate the selection criteria for both types of lesions and determine whether statistically significant differences exist between MRgFUS and RFA treatments.
Our study did not delve into the analysis of complications associated with RFA and MRgFUS treatments; however, the complication rate was poor, typically ranging from 1 to 6% [17, 18].
We performed 51 MRgFUS treatments and 51 RFA treatments, with 10 patients opting for RFA despite the recommended alternative and thus being excluded from statistical analysis.
We subsequently analyzed the data of 92 patients, 51 treated with MRgFUS and 41 with RFA. The most common lesion locations were the femur (41), tibia (16), humerus (13), vertebral bodies (8), and talus (7). The femur was the most frequently affected skeletal segment, with 25 and 16 patients treated with RFA and MRgFUS, respectively. Lesions were found to be cortical in 50 patients, subperiosteal in 28, and intramedullary in 14.
In Group A (MRgFUS), 24 patients had intra-articular lesions, 27 had extra-articular lesions, and 34 exhibited calcifications within the nidus. Additionally, 45 lesions were located more than 1 cm from critical vascular-nervous structures, and all patients had an adequate acoustic window. In Group B (RFA), 24 lesions were intra-articular, 30 had calcifications, and 24 were more than 1 cm from critical structures, but only 18 had an adequate acoustic window. Group C (RFA with an adequate acoustic window) comprised 18 patients, with similar distributions of intra/extra-articular lesions and calcifications, and all patients had an adequate acoustic window.
Statistical comparisons between Groups A and B revealed no significant differences in intra/extra-articular localization, presence of intranidal calcifications, sclerosis, or bone edema extension (p > 0.05). However, significant differences were observed in lesion proximity to vascular-nervous structures, lesion depth, nidus size, and presence of an acoustic window (p < 0.001).
Significant differences were also noted between Groups A and C in lesion depth (p < 0.001), sclerosis (p = 0.03), and nidus size (p = 0.02). Conversely, no significant differences were observed in intra/extra-articular localization, intranidal calcifications, proximity to vascular-nervous structures, or bone edema extension (p > 0.05).
Discussion and conclusions
Our study provides insights into the selection criteria guiding the choice between RFA and MRgFUS for the treatment of OO and OB [19]. While both techniques have demonstrated high efficacy and minimal complication rates [20,21,22], our analysis aimed to identify key factors influencing treatment selection and any statistically significant differences between them.
RFA has established itself as highly effective, with primary success rates ranging from 76 to 100% and secondary success rates, following repeated ablations, between 87 and 100% [23, 24] (Fig. 1).
OO treated by RFA. a OO localized to the femoral head: the absence of an adequate acoustic window and the intramedullary localization do not allow treatment using MRgFUS. b The electrode tip is located perfectly in the center of the nidus: in this way, it is possible to obtain an adequate necrotic area to cover the entire lesion
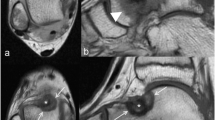
Similarly, MRgFUS has shown efficacy rates between 89 and 100%, with absence of pain after 1 year of follow-up and minimal complications [25, 26]. Notably, MrRgFUS offers advantages such as the absence of needles and exposure to ionizing radiation. However, it does have limitations, including the requirement for an adequate acoustic window, the inability to perform biopsies, and the inability to treat deep lesions (Fig. 2).
Tibial OO treated with MRgFUS. The presence of an acoustic window and the superficial localization of the lesion allow the treatment to be carried out easily. The MRI (PRF) sequences acquired during the treatment provide a real-time thermometric map of the region of interest, allowing the temperature reached at the focus and at the level of the surrounding structures to be assessed
Our retrospective evaluation focused on several variables, including intra/extra-articular lesion localization, nidus size, presence of intranidal calcifications, type of sclerosis, proximity to critical vascular-nervous structures, maximum extension of intraosseous edema, and presence of an adequate acoustic window.
Our analysis identified the presence of an adequate acoustic window as the primary selection criterion, crucial for enabling treatment with Focused Ultrasound. We found that the absence of an acoustic window significantly impacted treatment feasibility, highlighting the importance of considering alternative options in such cases.
Additionally, sclerosis emerged as a significant factor, with the presence of compact sclerosis favoring RFA due to the potential difficulty of achieving adequate concentrations of Focused Ultrasound energy at the nidus (Fig. 3).
Nidus size also played a crucial role, with larger lesions often favoring RFA due to the need for broader Focused Ultrasound action, which carries the risk of necrosis in healthy bone tissue (Fig. 4).
While proximity to critical vascular-nervous structures was considered, it was found to be less influential compared to other parameters and should be evaluated in conjunction with them.
However, our study has several limitations that should be considered when interpreting the results. First, it is important to note that measurements of the variables analyzed, such as nidus size, lesion depth, and presence of sclerosis, may be influenced by the operator performing them. Despite careful efforts to standardize measurement procedures, there is always the risk of intra-observer and inter-observer variability, which could impact the consistency and reliability of the collected data.
Additionally, our study did not delve into the analysis of complications associated with RFA and MRgFUS treatments. Although both techniques have minimal complication rates, it is important to recognize that adverse events, such as skin burns, local infections, or post-treatment bone fractures, can occur. The absence of a detailed analysis of complications may limit a comprehensive understanding of the risks associated with treatments and safety considerations.
In conclusion, our findings underscore the importance of considering multiple factors when selecting a treatment modality for OO and OB. While both RFA and MRgFUS offer comparable efficacy and complication rates, careful assessment of patient-specific features and lesion characteristics, particularly the presence or absence of an acoustic window and sclerosis, should guide treatment decisions. These findings provide valuable insights for clinicians in optimizing treatment outcomes for patients with OO and OB.
Data availability
All data supporting the findings of this study are available within the paper and its supplementary information.
References
Kransdorf MJ, Stull MA, Gilkey FW, Moser RP (1991) Osteoid osteoma. Radiographics 11(4):671–696. https://doi.org/10.1148/radiographics.11.4.1887121
Greenspan A (1993) Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma—clinical, imaging, pathologic, and differential considerations. Skeletal Radiol 22(7):485–500. https://doi.org/10.1007/BF00209095
Koh YH, Lee JW, Choi J, Kang HS (2010) Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics 30:737–749
Xu K, **e Y, Yan F, Deng Z, Lei J, Cai L (2019) Diagnostic and management options of osteoblastoma in the spine. Med Sci Monit 25:1362–1372. https://doi.org/10.12659/MSM.913666
Pourfeizi HH, Tabrizi A, Bazavar M, Sales JG (2014) Clinical findings and results of surgical resection of thoracolumbar osteoid osteoma. Asian Spine J 8(2):150–155. https://doi.org/10.4184/asj.2014.8.2.150
Masciocchi C, Zugaro L, Arrigoni F et al (2016) Radiofrequency ablation versus magnetic resonance guided focused ultrasound surgery for minimally invasive treatment of osteoid osteoma: a propensity score matching study. Eur Radiol 26(8):2472–2481. https://doi.org/10.1007/s00330-015-4111-7
Ghanem I (2006) The management of osteoid osteoma: Updates and controversies. Curr Opin Pediatr 18(1):36–41. https://doi.org/10.1097/01.mop.0000193277.47119.15
Masciocchi C, Arrigoni F, La Marra A, Mariani S, Zugaro L, Barile A (2016) Treatment of focal benign lesions of the bone: MRgFUS and RFA. Br J Radiol 89(1066):20150356. https://doi.org/10.1259/bjr.20150356
Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ (2003) Osteoid osteoma: Percutaneous treatment with radiofrequency energy. Radiology 229(1):171–175. https://doi.org/10.1148/radiol.2291021053
Arrigoni F, Napoli A, Bazzocchi A et al (2019) Magnetic-resonance-guided focused ultrasound treatment of non-spinal osteoid osteoma in children: multicentre experience. Pediatr Radiol 49(9):1209–1216. https://doi.org/10.1007/s00247-019-04426-0
Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, Wörtler K (2001) Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Jt Surg Ser B 83(3):391–396. https://doi.org/10.1302/0301-620X.83B3.11679
Rehnitz C, Sprengel SD, Lehner B et al (2012) CT-guided radiofrequency ablation of osteoid osteoma and osteoblastoma: clinical success and long-term follow up in 77 patients. Eur J Radiol 81(11):3426–3434. https://doi.org/10.1016/j.ejrad.2012.04.037
Arrigoni F, Barile A, Zugaro L et al (2018) CT-guided radiofrequency ablation of spinal osteoblastoma: treatment and long-term follow-up. Int J Hyperth 34(3):321–327. https://doi.org/10.1080/02656736.2017.1334168
De FM, Russo U, Papapietro VR et al (2018) Radiofrequency ablation of osteoid osteoma. Acta Biomed 89:175–185. https://doi.org/10.23750/abm.v89i1-S.7021
Earhart J, Wellman D, Donaldson J, Chesterton J, King E, Janicki JA (2013) Radiofrequency ablation in the treatment of osteoid osteoma: results and complications. Pediatr Radiol 43(7):814–819. https://doi.org/10.1007/s00247-013-2636-y
Donkol RH, Al-Nammi A, Moghazi K (2008) Efficacy of percutaneous radiofrequency ablation of osteoid osteoma in children. Pediatr Radiol 38(2):180–185. https://doi.org/10.1007/s00247-007-0690-z
Beyer T, van Rijswijk CSP, Villagrán JM et al (2019) Correction to: European multicentre study on technical success and long-term clinical outcome of radiofrequency ablation for the treatment of spinal osteoid osteomas and osteoblastomas (Neuroradiology, (2019), 61, 8, (935-942), 10.1007/s00234-019-02226-9). Neuroradiology 61(8):943. https://doi.org/10.1007/s00234-019-02246-5
Lassalle L, Campagna R, Corcos G et al (2017) Therapeutic outcome of CT-guided radiofrequency ablation in patients with osteoid osteoma. Skeletal Radiol 46(7):949–956. https://doi.org/10.1007/s00256-017-2658-x
Koch G, Cazzato RL, Gilkison A, Caudrelier J, Garnon J, Gangi A (2018) Percutaneous treatments of benign bone tumors. Semin Intervent Radiol 35(4):324–332. https://doi.org/10.1055/s-0038-1673640
Baal JD, Pai JS, Chen WC, Joseph GB, O’Donnell RJ, Link TM (2019) Factors associated with osteoid osteoma recurrence after CT-guided radiofrequency ablation. J Vasc Interv Radiol 30(5):744–751. https://doi.org/10.1016/j.jvir.2018.11.014
Arrigoni F, Bruno F, Palumbo P et al (2019) Magnetic resonance-guided focused ultrasound surgery treatment of non-spinal intra-articular osteoblastoma: feasibility, safety, and outcomes in a single-center retrospective analysis. Int J Hyperth 36(1):768–775. https://doi.org/10.1080/02656736.2019.1639833
Arrigoni F, Barile A, Zugaro L et al (2017) Intra-articular benign bone lesions treated with magnetic resonance-guided focused ultrasound (MRgFUS): imaging follow-up and clinical results. Med Oncol. https://doi.org/10.1007/s12032-017-0904-7
Hage AN, Chick JFB, Gemmete JJ, Grove JJ, Srinivasa RN (2018) Percutaneous radiofrequency ablation for the treatment of osteoid osteoma in children and adults: a comparative analysis in 92 patients. Cardiovasc Intervent Radiol 41(9):1384–1390. https://doi.org/10.1007/s00270-018-1947-7
Paladini A, Lucatelli P, Cappelli F, Pizzi G, Anelli V, Amodeo E (2018) Osteoid osteoma treated with radiofrequency ablation in non-operating room anesthesia. Eur Rev Med Pharmacol Sci 22:5438–5446
Masciocchi C, Conchiglia A, Gregori LM, Arrigoni F, Zugaro L, Barile A (2014) Critical role of HIFU in musculoskeletal interventions. Radiol Medica 119(7):470–475. https://doi.org/10.1007/s11547-014-0414-z
Napoli A, Mastantuono M, Marincola BC et al (2013) Osteoid osteoma: MR-guided focused ultrasound for entirely noninvasive treatment. Radiology 267(2):514–521. https://doi.org/10.1148/radiol.13120873
Funding
No funding was received to assist with the preparation of this manuscript. This retrospective study was approved by our local institutional review board (IRB) and informed consent was obtained from all patients at the time of MRI and CT-guided ablations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Spano, G., Daffinà, J., Izzo, A. et al. Selection criteria for osteoid osteomas/osteoblastoma’s treatment by ablation with radiofrequency needles or high intensity focused ultrasound: our experience. J Med Imaging Intervent Radiol 11, 11 (2024). https://doi.org/10.1007/s44326-024-00018-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44326-024-00018-x