Abstract
Background
To explore the influencing factors for complication with aneurysm rupture of the fetal posterior communicating artery after clip** through the lateral supraorbital (LSO) approach and prognosis.
Methods
A total of 119 patients with posterior communicating artery aneurysm (PCoAA) accompanied by fetal posterior cerebral artery (fPCA), who underwent clip** through the LSO approach from January 2014 to December 2019, were selected. They were aged 50–70 years old, (60.5 ± 13.7) on average. The treatment outcome, incidence of complications and follow-up results were analyzed. Based on the follow-up results, univariate comparative analysis was conducted for the clinical data of patients with good or poor prognosis. The statistically significant factors were incorporated into multivariate Cox regression analysis, and the nomogram prediction model for prognosis was established. The accuracy of the model was assessed using the Hosmer–Lemeshow goodness-of-fit test.
Results
Clip** through the LSO approach was successful in all cases. Perioperative complications occurred in 41 patients. According to the follow-up results, 89 patients had good prognosis, while 30 had poor prognosis. Age of > 65 years old, history of hypertension, high Hunt–Hess grade and high modified Fisher grade were independent risk factors for the poor prognosis of patients with PCoAA accompanied by fPCA after clip** through the LSO approach. The results obtained by the established model were consistent with the actual ones.
Conclusion
Age, history of hypertension, Hunt–Hess grade and modified Fisher grade are independent risk factors for the prognosis of patients with PCoAA accompanied by fPCA after clip** through the LSO approach.
Similar content being viewed by others
1 Introduction
Posterior communicating artery aneurysm (PCoAA) is a clinically common internal carotid aneurysm, which refers to protrusion at the internal carotid artery-PCoA bifurcation, accounting for approximately 20–30% of intracranial aneurysms [1]. Ruptured intracranial aneurysm is mainly manifested as subarachnoid hemorrhage, sudden severe headache, nuchal rigidity, photophobia, nausea, and vomiting. The fatality rate of aneurysm hemorrhage is 25–50%, and nerve dysfunction may still occur in patients after treatment [2]. The treatment is difficult due to the complex anatomical structure of PCoA and existence of fetal posterior cerebral artery (fPCA) [3].
Intracranial aneurysm is mainly treated with craniotomy and interventional therapy. As a common method for treating intracranial aneurysm, clip** can be performed through the pterional, keyhole or lateral supraorbital (LSO) approach [4]. The formation of fPCA can be attributed to the absence or dysplasia of P1 segment of the ipsilateral brain PCA, so the blood supply of P2 segment originates from the thickened PCoA on the ipsilateral side. CT angiography shows that the diameter of PCoA is larger than that of P1 segment of the ipsilateral PCA, and the ipsilateral P1 segment is small or absent [5]. There is a higher risk of ischemic injury in the surgical treatment of PCoAA accompanied by fPCA than that of PCoAA alone [6]. Clip** aneurysms through the pterional or LSO approach is most common, and this approach has wide visual field which reduces the strain on brain tissues while separating each cistern during operation. Meanwhile, this method can well control bleeding during operation by fully exposing the A1 and A2 segments of bilateral anterior cerebral arteries simultaneously [7, 8]. Thereby motivated, we herein explored the efficacy of clip** through the LSO approach on PCoAA accompanied by fPCA, and the influencing factors for the prognosis, aiming to provide valuable evidence for clinical treatment.
2 Materials and Methods
2.1 Subjects
A total of 119 patients undergoing vascular therapy in our hospital from January 2014 to December 2019 were retrospectively analyzed. Inclusion criteria: (1) patients diagnosed as PCoAA through CTA or DSA, (2) those with subarachnoid hemorrhage shown in head CT, (3) those with preoperative Hunt–Hess grade 1–3 undergoing clip** through the LSO approach, and (4) those with complete clinical data. Exclusion criteria: (1) patients complicated with severe diseases in the heart or lungs, (2) those with malignant tumors, (3) those with multiple intracranial aneurysms unable to be clipped by unilateral craniotomy, (4) those with modified Fisher grade III or above, or with brain swelling shown in head CT, (5) those with distal middle cerebral artery (M1) aneurysm or distal anterior cerebral artery (A2) aneurysm, or (6) those receiving conservative or endovascular treatment. This study was approved by the Hospital Ethics Committee, and the patients or their families were informed of the study and signed the informed consent.
2.2 Evaluation Criteria
The embolization of aneurysm was graded before operation according to the Raymond rating criteria [9]: grade I: there is basically no image developed in the aneurysm, grade II: there is image developed at the aneurysmal neck, and grade III: there is image developed in the aneurysmal body. Preoperative Hunt–Hess grading criteria [10]: grade 0: un-ruptured aneurysm, grade 1: asymptomatic or mild headache, and mild nuchal rigidity, grade 2: moderate–severe headache and nuchal rigidity, without other neurological deficits except cranial nerve palsy, grade 3: lethargy, confusion or mild focal neurological deficits, grade 4: stupor, moderate or severe incomplete paralysis, and possibly early decerebrate rigidity and vegetative nervous system dysfunction, and grade 5: deep coma, decerebrate rigidity, and dying state. Based on CT results, the subarachnoid hemorrhage of patients was graded using the modified Fisher scale before operation [11]: grade 0: no hemorrhage, or only intraventricular or intra-parenchymal hemorrhage, grade 1: hemorrhage only in the basilar cistern, grade 2: hemorrhage only in the surrounding cistern or lateral fissure cistern, grade 3: extensive subarachnoid hemorrhage accompanied by intraventricular hematoma, and grade 4: thick hematocele in the basilar cistern, surrounding cistern and lateral fissure cistern.
2.3 Imaging Examinations
The imaging data of all patients were assessed by more than two radiologists and neurosurgeons. Diagnostic criteria for PCoAA: filling defects in the cerebral veins were mainly shown in preoperative CTA, manifested as venous stenosis or no image development.
Diagnostic criteria for fPCA: it was observed in internal carotid angiography that PCoA was open, and PCA was mainly supplied by the internal carotid artery. The basilar artery angiography displayed little or no blood supply to PCA, accompanied by dysplasia or absence of P1 segment of PCA.
2.4 Surgical Methods
Under general anesthesia with tracheal intubation, the cutaneous muscle flap was turned to the orbital side, and a single bone hole was made at the temporal line of the temporal muscle attachment margin. A bone flap (about 3 × 4 cm) was dissociated with a milling cutter. The sphenoid ridge was partially abraded out, and the dura mater was cut open in an arc shape and hung on the edge of the bone window. In the case of high intracranial pressure, lumbar cistern drainage was performed to release the cerebrospinal fluid, the lateral fissure was separated under a microscope, and the upper segment of the internal carotid artery was exposed. Then the frontal lobe was gently lifted using an automatic brain spatula, the skull base was opened, and the cerebrospinal fluid was aspirated to further cause brain tissue collapse. Afterward, the PCoA complex was fully exposed, and the aneurysmal neck was clipped, followed by indocyanine green angiography. The aneurysmal body was cut, hemostatized and washed before operation, and several gelatin sponges soaked with papaverine and hemocoagulase were placed to prevent vasospasm and bleeding in the operative region. Finally, the skull was routinely closed, and the patient was sent back to NICU for subsequent treatment.
2.5 Postoperative Follow-up
Head CT was performed within 24 h after operation to determine whether there was new ischemic cerebral infarction, new intracranial hematoma and traction injury of brain tissues. The neurological prognosis of patients was evaluated using the Glasgow outcome scale (GOS) score before and 6 weeks, 6 months and 12 months after operation [12]: 5 points: well recovered, able to live normally, but accompanied by mild defects, 4 points: mildly disabled, but able to live independently and work under protection, 3 points: severely disabled, sober, and unable to live independently, 2 points: vegetative, with minimal responses, and 1 point: dead. The GOS score of 5 points indicates good prognosis, while that of 1–4 point(s) indicates poor prognosis.
2.6 Statistical Analysis
IBM SPSS 19.0 software was used for statistical analysis. The normality of continuous data was detected by Kolmogorov–Smirnov test. Normally distributed continuous variables were expressed as (\(\overline{x} \pm s\)), and t test was performed to compare whether there are statistical differences between two groups. Abnormally distributed continuous variables were expressed as median, and Mann–Whitney U test was performed to compare whether there were statistical differences between two groups. The difference in categorical variables was compared by χ2 test. The influencing factors for the prognosis of PCoAA patients were explored through multivariate Cox regression analysis. Based on the independent risk factors for the prognosis of patients, a nomogram prediction model was established using R software and rms software package. The calibration of the model was assessed using the Hosmer–Lemeshow goodness-of-fit test. P < 0.05 suggested that a difference was statistically significant, and α = 0.05 was set as the test level.
3 Results
3.1 General Conditions
A total of 119 patients were enrolled in this study, including 98 females and 21 males aged (60.5 ± 13.7) years old on average. The preoperative examination results and grading of patients are shown in Table 1.
3.2 Surgical Outcomes and Perioperative Complications
Head CTA conducted 7–10 d after operation confirmed that aneurysm clip** was successful in all cases. Perioperative complications occurred in 41 of 119 patients, including 5 cases of postoperative infarction, 7 cases of severe cerebral vasospasm, 18 cases of hydrocephalus and 11 cases of intracranial infection.
3.3 Follow-up Results
All patients were followed up for 12 months after operation, and their prognoses were assessed using GOS scores. There were 89 cases of good recovery, 28 cases of moderate disability, and 2 cases of severe disability. Besides, focal cerebral infarction and early hydrocephalus were found in 7 and 10 cases, respectively, which were mitigated through lumbar cistern drainage.
3.4 Univariate Analysis Results of Factors for Prognosis
The results of univariate analysis revealed that age, history of hypertension, Hunt–Hess grade and modified Fisher grade had significant differences between good and poor prognosis groups. The poor prognosis group was older, and the proportion of patients with history of hypertension, high Hunt–Hess grade and high Fisher grade was higher in poor prognosis group than that in good prognosis group (P < 0.05) (Table 2).
3.5 Cox Regression Analysis Results of Factors for Prognosis
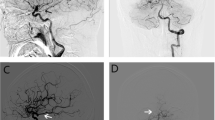
The statistically significant factors in the above univariate analysis were incorporated into multivariate Cox regression analysis. It was found that age of > 65 years old, history of hypertension, Hunt–Hess grade 3 and modified Fisher grade 3 were independent risk factors for the prognosis of patients with PCoAA accompanied by fPCA (Fig. 1).
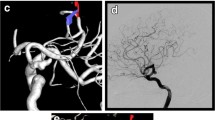
3.6 Prediction Model for Prognosis and Efficacy Assessment
The nomogram prediction model for the prognosis of PCoAA patients was established based on the above independent risk factors (Fig. 2). As shown in the calibration curve of the model (Fig. 3), the gray diagonal line was the reference line, the blue curve was the prediction fitting line, and the gray shadow indicated 95%CI. When the event incidence rate was < 32% or > 78%, the risk of poor prognosis was underestimated by the model. When the rate was 32–78%, the risk was overestimated by the model. Overall, the result obtained by the nomogram prediction model was highly consistent with the actual ones, verifying a high accuracy.
4 Discussion
PCoAA refers to all aneurysms at the initial part of PCoA in a broad sense, and the aneurysm at the internal carotid artery-PCoA bifurcation in a narrow sense, accounting for 50% of internal carotid artery aneurysms [13]. As an important anatomical variation of PCoA, fPCA means that in the later stage of embryonic development, PCoA gradually becomes thinner with the development of brain tissues, and then its diameter is smaller than that of the P1 segment from the basilar artery. The blood to PCA is mainly supplied by the anterior circulation [14]. The incidence rate of fPCA is 7–36% in the population [15]. In terms of imaging, fPCA is manifested as the absence or dysplasia of P1 segment, and PCoA is the P2 segment of the ipsilateral PCA. Ruptured fPCA is a risk factor for PCoA. PCoAA complicated with fPCA, a complex type of aneurysm, easily leads to insufficient blood supply to the occipital lobe and even infarction during operation [16].
Clip** through the LSO approach was first modified by Hernesniemi based on that through the pterional approach. Incision through the pterional approach starts in front of the tragus, so the main superficial temporal artery is prone to damage. In contrast, the lower edge of incision through the LSO approach starts above the main superficial temporal artery, thereby avoiding damage and reducing bleeding [17]. Compared with the pterional approach, the LSO approach is characterized by more exposure of frontal base, less exposure of lateral fissure temporal lobe, short surgical incision, small scope of temporal muscle dissection, and decreased bone window size and defects. Moreover, the incidence rate of postoperative complications, such as intracranial infection, cerebrospinal fluid leakage, temporal muscle atrophy and facial paralysis, declines.
In the present study, 119 PCoAA patients were treated with clip** through the LSO approach. It was confirmed that aneurysm clip** was successful in all cases, and perioperative complications were observed in 41 patients. All patients were followed up for 6 months, of whom 89 patients had good prognosis (GOS score = 5 points) while the remaining 30 had poor prognosis (GOS score = 2–4 points). The univariate analysis results revealed that age, history of hypertension, Hunt–Hess grade and modified Fisher grade were influencing factors for the prognosis of patients.
There were more female patients than male patients in this study. However, the prognosis of patients showed no statistically significant difference in terms of gender. The higher incidence rate of PCoAA in female patients may be related to the estrogen level. The risk of degenerative lesions in organs rises with aging, and the incidence rate of underlying diseases, such as hypertension, diabetes mellitus and cardio-cerebrovascular diseases, is higher in the elderly [18]. Elderly patients have decreased ability of cerebrovascular auto-regulation and weakened compensatory ability of collateral circulation, so they are prone to cerebral ischemia after clip** through the LSO approach [19]. History of hypertension is an influencing factor for the poor prognosis of patients with aneurysms. Hypertension can lead to vascular sclerosis and even calcification in patients, thus increasing the operation difficulty and risk of aneurysm clip** and inducing aneurysm rupture in the perioperative period [20]. The Hunt–Hess scale is used for the grading of clinical symptoms of patients with subarachnoid hemorrhage. It is recommended that patients with low grade should be treated with early surgery, and those with high grade should undergo late surgery after the vasospasm stage due to obvious clinical symptoms including peripheral nerve injury and neurological impairment [21]. Besides, the modified Fisher scale is used for the head CT grading of patients with subarachnoid hemorrhage, which can reflect the bleeding site, presence or absence of hematoma, and hematoma volume [23]. Ding et al. [24] analyzed the clinical data of 80 PCoAA + fPCA patients undergoing microsurgical clip**. They found that age, preoperative Hunt–Hess grade and modified Fisher grade were independent risk factors for the surgical outcomes and prognosis, and the risk of poor prognosis of patients with high-grade aneurysm was 2.1 times that of patients with low-grade aneurysm. The aneurysm size is a risk factor for aneurysm rupture, and the diameter of aneurysm > 7 mm is a risk factor for incomplete aneurysm clip** and second operation [25, 26]. Herein, good and poor prognosis groups had similar aneurysm sizes. Probably, PCoA was adjacent to the oculomotor nerve, and the patients visited the hospital due to oculomotor nerve palsy in the early stage, so the aneurysm developed for a short time.
In a study involving 55 ruptured fPCA aneurysm patients, Mardjono et al. [27] found that clip** through the LSO approach was safe and effective, being consistent with the results in this study. We herein found through multivariate Cox regression analysis that age of > 65 years old, history of hypertension, high Hunt–Hess grade and high modified Fisher grade were independent risk factors for the prognosis of PCoAA + fPCA patients undergoing clip** through the LSO approach. The nomogram prediction model established with the above factors had high accuracy and effectively predicted the prognosis after clip** through the LSO approach.
5 Conclusion
In conclusion, age, history of hypertension, Hunt–Hess grade and modified Fisher grade are independent risk factors for the prognosis of patients with PCoAA accompanied by fPCA after clip** through the LSO approach.
Data Availability
The data that support the findings of this study are available from the corresponding author, Y.J.F., upon reasonable request.
References
Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103–10.
Tan W, He ZH. [Analysis on influencing factors of occurrence and prognosis of brain edema occurrence after surgical clip** of ruptured aneurysms]. Chongqing Med. 2019;48:1822–6.
Chen Z, Niu Y, Tang J, Li L, Feng Z, Feng H, et al. Endovascular treatment of posterior communicating artery aneurysms in the presence of the fetal variant of posterior cerebral artery. Interv Neuroradiol. 2015;21:456–61.
Cha KC, Hong SC, Kim JS. Comparison between lateral supraorbital approach and pterional approach in the surgical treatment of unruptured intracranial aneurysms. J Korean Neurosurg Soc. 2012;51:334–7.
Veras WR, Veras G. Variation of the posterior cerebral artery and its embryological explanation: a cadaveric study. Bol Asoc Med Puert Rico. 2010;102:55–8.
Thiarawat P, Jahromi BR, Kozyrev DA, Intarakhao P, Teo MK, Choque-Velasquez J, et al. Are fetal-type posterior cerebral arteries associated with an increased risk of posterior communicating artery aneurysms? Neurosurgery. 2019;84:1306–12.
Hage ZA, Charbel FT. Clip** of bilateral MCA aneurysms and a coiled ACOM aneurysm through a modified lateral supraorbital craniotomy. Neurosurg Focus 2015;38:Video19.
Yu K, Yuan J. [Comparison between lateral supraorbital approach and pterional approach for clip** anterior communicating artery aneurysm]. Chin J Minim Invas Neurosurg. 2019;24:49–52.
Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–403.
Sun Q, You WC, Sun XO, Shao Z, Zhu J. Chen G [Effect analysis of different treatment modalities in patients with paraclinoid aneurysm]. Chin J Cerebrovasc Dis. 2018;15:561–6.
van den Berg R, Foumani M, Schröder RD, Peerdeman SM, Horn J, Bipat S, et al. Predictors of outcome in World Federation of Neurologic Surgeons grade V aneurysmal subarachnoid hemorrhage patients. Crit Care Med. 2011;39:2722–7.
Smith MJ, Sanborn MR, Lewis DJ, Faught RW, Vakhshori V, Stein SC. Elderly patients with intracranial aneurysms have higher quality of life after coil embolization: a decision analysis. J Neurointervent Surg. 2015;7:898–904.
Hu T, Wang D. Association between anatomical variations of the posterior communicating artery and the presence of aneurysms. Neurol Res. 2016;38:981–7.
Bonow RH, Young CC, Bass DI, Moore A, Levitt MR. Transcranial Doppler ultrasonography in neurological surgery and neurocritical care. Neurosurg Focus. 2019;47:E2.
Xu J, Xu L, Wu Z, Chen X, Yu J, Zhang J. Fetal-type posterior cerebral artery: the pitfall of parent artery occlusion for ruptures P-2 segment and distal aneurysms. J Neurosurg. 2015;4:906–14.
Taweesomboonyat C, Tunthanathip T, Kaewborisutsakul A, Saeheng S, Oearsakul T, Riabroi K, et al. Outcome of ruptured posterior communicating artery aneurysm treatment comparing between clip** and coiling techniques. World Neurosurg. 2019;125:e183–8.
Hernesniemi J, Ishii K, Niemelä M, Smrcka M, Kivipelto L, Fujiki M, et al. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl. 2005;94:17–21.
Zhang CW, Wang CH, Xu D. [Prognostic analysis of endovascular embolization and surgical clip** for posterior communicating artery aneurysm caused oculomotor palsy in elder patients]. Clin Misdiagn Misther. 2017;30:65–8.
Xu J, Liu BY. [Safety and clinical efficacy of microsurgical clip** compared with endovascular coiling in treatment of ruptured aneurysm of middle cerebral artery]. J Clin Exp Med. 2018;17:1751–4.
Shi L, Yu J, Zhao Y, Xu K, Yu J. Clip** treatment of posterior communicating artery aneurysms associated with arteriosclerosis and calcification: a single center study of 136 cases. Exp Ther Med. 2018;15:1647–53.
Hsu CE, Lin TK, Lee MH, Lee ST, Chang CN, Lin CL, et al. The impact of surgical experience on major intraoperative aneurysm rupture and their consequences on outcome: a multivariate analysis of 538 microsurgical clip** cases. PLoS ONE. 2016;11: e0151805.
Zhao Q, Tang YY, Li S, Qiu DZ, **e MY, Wang Q, et al. [Analysis on factors of postoperative recovery of oculomotor nerve palsy caused by posterior communicating artery aneurysm]. J Region Anat Oper Surg. 2019;28:369–73.
Tang YY, Wang XD, Wang JX, Zhao Q, **]. J Region Anat Oper Surg. 2019;28:143–7.
Ding F, Liu P, Fang Y, Hua L, ** on prognosis of patients with fetal-type posterior cerebral artery and posterior communicating artery aneurysms]. J Region Anat Oper Surg. 2020;29:22–5.
Malhotra A, Wu X, Forman HP, Matouk CC, Gandhi D, Sanelli P. Management of tiny unruptured intracranial aneurysms: a comparative effectiveness analysis. JAMA Neurol. 2018;75:27–34.
Huhtakangas J, Lehecka M, Lehto H, Jahromi BR, Niemelä M, Kivisaari R. CTA analysis and assessment of morphological factors related to rupture in 413 posterior communicating artery aneurysms. Acta Neurochir. 2017;159:1643–52.
Tjahjadi M, Kivelev J, Serrone JC, Maekawa H, Kerro O, Jahromi BR, et al. Factors determining surgical approaches to basilar bifurcation aneurysms and its surgical outcomes. Neurosurgery. 2016;78:181–91.
Acknowledgements
This study was financially supported by Provincial Key Research and Development Program (No. 2019C03044).
Author information
Authors and Affiliations
Contributions
Y.X.C. and Y.J.F. designed this study and prepared this manuscript; Y.R.C., H.H.C., X.F.L., G.Z.Z. and J.L.Y. collected and analyzed clinical data. All authors approved the submission and publication of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Y., Cai, Y., Chen, H. et al. Influencing Factors for Complication with Aneurysm Rupture of the Fetal Posterior Communicating Artery After Clip** Through the Lateral Supraorbital Approach and Prognosis. Artery Res 27, 186–193 (2021). https://doi.org/10.1007/s44200-021-00007-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44200-021-00007-5