Abstract
The objective of this work was to measure the tooth root canals’ diameter, remnant dentin thickness, endodontic post to dentin distance, and resin-matrix cement layer after three types of root canal sha**. Thirty extracted human premolars were endodontically treated and groups of specimens were divided according to the cementation with two different endodontic posts as follow: A) Fibio Fiberglass Post™, Anthogyr, France; B) multi-filament GFRC (Rebilda GT™, VOCO, Germany). Cone beam computed tomography (CBCT) and conventional X-ray analyses were performed before and after the endodontic post cementation. After cementation, specimens were cross-sectioned and inspected by optical microscopy and scanning electron microscopy at magnification ranging from × 30 up to × 2000. Changes in sha** of the root canals caused a decrease in the thickness of the remnant tooth tissues. CBCT and microscopic analyses also revealed a clear variation of resin-matrix cement around the glass fiber-reinforced composite (GFRC) posts. A multi-filament GFRC post provided an adequate distribution of filaments although the resin-matrix cement revealed a high volume among the filaments. An increase in thickness and volume of resin-matrix cement was noticed at the coronal third since the fitting was compromised due to tooth anatomic variations and root canal preparation. Defects such macro-scale pores, cracks, and voids were also detected by microscopic analyses. The root canal sha** can promote a decrease in the thickness of the remnant tooth tissues that can increase the risks of clinical failures by fracture. The thickness and volume of resin-matrix cement varied around both GFRC posts and increased from the apex up to the coronal third due to the lack of fitting.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endodontic treatment is a clinical procedure in dentistry to treat teeth when pulp tissue has become irreversibly injured or necrotic due to caries or dental trauma [1,2,3,4,5,6]. The extensive loss of coronal structure compromises the mechanical behavior of endodontically treated teeth, leading to an increased risk of catastrophic fracture. The excessive loss of the root canal dentin thickness occurs due to caries, access to the canals, over-instrumentation, large tapered endodontic instruments, previous restoration with large-diameter posts, or internal root resorption [3, 6, 7]. Such root canal damage can promote high risks of internal stress-induced fracture since strength is directly proportional to the volume of the remaining dental structure. Previous studies clearly show that a high volume of dentin provides a proper mechanical behavior of the remaining tooth structure [5, 7, 8]. In this way, the ferrule effect is a required principle for restoration of endodontically treated teeth that have been submitted to extensive loss of tooth structure [2, 9, 10]. Thus, the use of tooth root intraradicular posts become an alternative to retain coronal restorations and to provide a proper distribution of stresses through the tooth tissues by the ferrule effect [1, 2, 11,12,13,14,15,16]. However, several factors can be detrimental to the endodontically treated teeth such as the thickness of remnant tooth tissues, resin-matrix cement layer, and the materials’ properties. A mismatch in mechanical properties among synthetic materials and tooth tissues can result in concentration of stresses at the interfaces and failures by fracture [1, 2, 11,12,13,14]. Thus, the main factor that dictates the strength and long term survival of endodontically treated teeth is mainly related to the volume of remnant tooth tissues structure, selection of materials, cementation, and the integrity of the restorative interfaces [2, 10, 17].
Several types of tooth root intraradicular posts can be used for the restoration of endodontically treated teeth, such as cast metal posts, ceramic or composite standard-shaped posts, and ceramic or composite custom-made posts [1, 12, 14, 15]. Yttria stabilized tetragonal zirconia polycrystals (3Y-TZP) can be used as standard or custom-made post, considering its high strength (3-point bending strength at ~ 1200 MPa) and fracture toughness (10–14 MPa m1/2) [18, 19]. Metal and ceramic posts have been used for many years, although some clinical limitations have been related to the over-instrumentation and the mismatch in elastic modulus that increases the risks of catastrophic fractures of endodontically treated teeth [11]. In recent times, glass fiber-reinforced composite (GFRC) posts became an alternative material to replace casting metal post systems because the decreased risks of tooth fracture and less corrosion issues associated with metal posts. Commercially available GFRC posts are often composed of glass fibers (60–80 wt%) embedded in epoxy resin. Nowadays, GFRC have been the first choice materials considering the balanced elastic modulus [12, 14, 20] (30–50 GPa) and adequate strength (3-point bending strength at around 433–677 MPa) [12, 14, 20]. In fact, those values of mechanical properties and the custom-made shape decrease the probability of catastrophic fractures when endodontically treated teeth are subjected to occlusal forces [11, 15]. Cast metal or Y-TZP posts can induce vertical fracture pattern with consequent unrepairable prognosis. Since GFRC posts are cemented into the tooth root canals, restorative materials placed over the posts should also provide an adequate wear resistance to avoid restorative damage that could compromise the mechanical performance of endodontically treated teeth [21,22,23,24]. Also, studies have shown that GFRC posts provide low risks of the toxicity when compared to metallic posts regarding their chemical composition and the chemical stability to the oral environment [16, 25].
The most common failure of endodontically treated teeth restored with GFRC posts is the debonding from the resin-matrix cement [12, 26, 27]. Additionally, fractures at the resin-matrix cement to adhesive system and dentin interfaces can also take place. Thus, the debonding and fractures on GFRC posts can be associated with several factors related to materials, anatomic features, root canal sha**, remnant tooth tissues, and cementation [3, 20, 27,28,29]. Differences in anatomical and restorative design along the root canal cause a spatial variation between the post and the intracanal dentin surface. Such space is filled by the resin-matrix cement on cementation, resulting in regions with variable thick and thin layers of resin-matrix cement [27, 30]. Multi-filaments GFRC posts have been used to enhance the fitting and decrease the resin-matrix cement layer although further studies are required to validate the advantages and limitations of multi-filament GFRC posts. Thick layers of resin-matrix cements are prone to defects like macro- and micro-scale pores, cracks, and voids. An adequate fitting of the GFRC post along the intraradicular regions can promote a well-distribution of the resin-matrix cement volume that decreases the risks of defects such as voids and cracks. According to previous studies, the highest bond strength values of GFRC posts to intracanal surfaces were recorded when an appropriate fitting promoted a resin-matrix cement layer thickness at 0.1–0.3 mm [12, 26, 27]. The resin-matrix cement layer should be at micro-scale thickness, providing adequate retention and avoiding failures by crack propagation at those defects.
The main aim of this study was to measure the tooth root canals’ diameter, remnant dentin thickness, GFRC post to dentin distance, and resin-matrix cement layer after three types of root canal sha**. It was hypothesized that the dentin thickness decreases after invasive tooth root canal sha** and the post to dentin distance varies considering anatomic and sha** factors. Thus, the measurement of the tooth root canal sha** and resin-matrix cement layer using different methods such as X-Ray and microscopy analyses is the novelty of the present work. Also, the preparation of specimens considering the interface plane for measurement at different regions can provide a plenty of data on GFRC fitting and the thickness dimensions of the resin-matrix cement.
Materials and Methods
Preparation of Endodontically Treated Teeth
The manuscript of this laboratory study has been written according to Preferred Reporting Items for Laboratory studies in Endodontology 2021 guidelines [31]. The project was previously reviewed and approved by an institutional review board from the University Institute of Health Sciences (IUCS), CESPU, Portugal, with the following Ethics protocos reference: CE/IUCS/CESPU-18/2022. All procedures performed involving human participants followed the ethics standards of the IUCS ethics committee and they were in agreement with the 1964 Helsinki declaration and its later amendments or comparable Ethics Standards. Informed consent was unnecessary following the national regulations and since all data were processed anonymously. The need for informed consent was waived by the ethics committee/Institutional Review Board of IUCS at CESPU, Portugal.
Fifteen particpants were involved in the present study. Each participant was in good oral health, with no history of antibiotic treatment during the previous 6 months. Thirty extracted human premolars (mean root length at 15 mm) with completely formed apex were selected considering root sizes and absence of caries, visible fracture lines, or cracks (Fig. 1A). Teeth were selected according to the Schneider method and then stored in 5% Chloramine for 7 days followed by immersion in distilled water at 4 °C for 7 days. The anatomic crowns were initially sectioned, and all teeth were endodontically treated. The working length was determined by using an endodontic file type K-flexofile ISO # 10 until it is visible through the apical foramen and then 1 mm was subtracted. Physically assisted instrumentation was carried out by reciprocating friction instrumentation using the following diameter of reciprocating stainless steel files (25 mm in length): 25/07 (small), 35/06 (medium), and 45/05 (large) (Wave One™, Dentsply-Maillefer, Switzerland). Thus, groups of teeth were divided regarding the use of different diameter leading to the wear of intraradicular dentin, as follow: minimally invasive (small), standard (medium); and invasive (large). The canal was disinfected using 3% sodium hypochlorite solution (NaOCl) between each filing on which permeabilization procedure was performed with 10 K file between every 3 reciprocating movements using a syringe with lateral irrigation needle (30G). The canals of the teeth were dried with calibrated paper cones (Dentsply-Maillefer, Switzerland). At last, the tooth root canals were filled using calibrated primary gutta-percha cones (Dentsply Maillefer, Switzerland) and cold lateral compaction technique which was embedded within resin-matrix cement (AH-Plus™, Dentsply-Maillefer, Switzerland), as seen in Fig. 1C and D. After gutta-percha compaction, periapical X-ray analyses were performed for confirmation of the filling integrity.
A View of the first premolar selected for root canal preparation. B Physically assisted instrumentation on reciprocating friction instrumentation with Wave One™ primary # 25.08 files, 25 mm (Dentsply-Maillefer, Switzerland). C Tooth toot canals filled with cement and gutta-percha on obturation. D Preparation for cementation was initiated by enlarging the root canals with Largo Peeso Reamers™ (Dentsply, USA)
Gutta-percha was removed using reamers with size at 2, 3, 4 (Largo Peeso reamers™; Dentsply Intl, USA) (2A). A parallel-sided twist drill nº 6 (Parapost Black P-42™; Coltène/Whaledent Inc, USA) was used at low speed. No attempt to generate pressure on instruments against the intraradicular dentin surfaces was carried out when using either Largo reamers or drills. Silicone stops (Dentsply Intl, USA) were placed on each drill to ensure that the canal sha** was achieved as previously determined lengths. The debris generated after each instrumentation were rinsed away with 2 mL of 3% NaOCl. After preparation, tooth root canals were thoroughly dried using paper points.
Glass fiber-reinforced composite (GFRC) (Fibio Fiberglass Post™, Anthogyr, France) or mutli-filament GFRC (Rebidla™, VOCO, Germany) posts were passively placed in the tooth root canals for cementation. On cementation, an adhesive primer (ParaBond primer™, Coltène, Whaledent,USA) was applied to the tooth root canals using a fine microbrush at reciprocating friction movement for 30 s. The excessive layer of primer was removed using paper tips and a light air stream was applied for 2 s. A mixture of primer and bond adhesive system (Parabond A & B adhesive™, Coltène, Whaledent Inc, USA) was applied to the tooth root canal with a fine microbrush at reciprocating friction movement for 30 s. The excessive adhesive layer was removed using paper tips and a light air stream was applied for 2 s. At last, the resin-matrix cement material (ParaCore Automix™, Coltene Whaledent, USA) was applied directly into the intraradicular space using a syringe tip. GFRC posts were also coated with the cement and then inserted into the tooth root canal on slight pressure. The excessive cement layer was removed and the cement was then light-cured using a light curing unit at 420–480 nm wavelength (LY-A180™, Anyang Zongyan Dental Material Co, Ltd, China) for 120 s. After cementation procedure, periapical X-ray analyses were performed for confirmation of the filling integrity. Specimens were then assembled with a self-curing acrylic resin (Ortho resin™; Dentsply, USA) in a short length of polyvinyl chloride mold. To increase root retention in the acrylic resin block, each root was previously scratched on the buccal and lingual surfaces with a tungsten carbide bur [32,33,34,35].The dental inspector apparatus (Ney surveyor, Germany) was used to align the post space with the long axis of the tooth.
X-Ray and CBCT Analyses
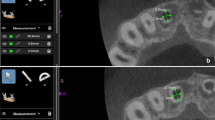
Periapical X-ray images of tooth roots were acquired by using a X-ray clinical apparatus (Corix 70 Plus KVP X-ray™, CORAMEX S.A, Mexico). X-ray analyses were performed on triangular scanning technique at 70 kVp and 8 mA for 53 s [36]. As seen in Fig. 2, cone beam computed tomography (CBCT) was performed to measure the tooth root canals’ diameter, remnant dentin thickness, and the endodontic post to dentin distance. The CBCT unit KaVo OP 3D™ (KAVO, Germany) used in this study operates in different set up, expanding from panoramic-only through cephalometric, and three-dimensional capabilities to accomplish three-in-one configuration.
The CBCT focal spot was at 0.5 mm, IEC 336 (IEC 60336/2005) while the tube voltage and the tube current were set at 60–95 kV and 3.2–16 mA, respectively. Image voxel size ranged from 80 up to 400 μm and the scanning was performed for 27–45 s. A fast scan time was provided by the complementary metal-oxide semiconductor (CMOS) X-ray detectors. The image volume sizes (H × Ø) were the following: 5 × 5, 6 × 9, 9 × 11, and 9 × 14 cm. Different resolution levels could be evaluated such as: low dose technology scan, standard resolution scan, high resolution scan, and endo resolution scan. CBCT was coupled to the Blue Sky Plan 4™ software program (BlueSkyBio, USA). Two hundred and seventy-five axial cross-sectioned CBCT images were acquired for each tooth root specimen. Cross-sections were evaluated at each tooth root third: coronal, middle, and apex. Tooth root canal diameter was measured prior to the placement of the GFRC post (Fig. 2B). Then, the GFRC post to dentin distance was measured at mesial, distal, buccal, and lingual regions. Navigation and evaluation of the anatomical details was supported by the Blue Sky Plan software as previously reported in literature [37, 38].
Microstructural Analyses
Randomly endodontically treated teeth specimens were embedded in autopolymerizing polyether modified resin (Technovit 400™; Kulzer GmbH, Germany) and then cross-sectioned at 90 degrees relative to the plane of the GFRC post to resin-matrix cement interface. Surfaces were wet ground down to 2400 Mesh using SiC abrasive papers and then polished with 1 µm Al2O3 particles. Then, surfaces were ultrasonically cleaned in isopropyl alcohol for 10 min and then in distilled water for 10 min [2, 5, 9].
At first, cross-sectioned specimens were inspected by optical microscopy at magnification ranging from × 10 up to × 500. Microstructural analyses were performed using an optical microscope (Leica DM 2500 M™; Leica Microsystems, Germany) connected to a computer for image processing, using Leica Application Suite™ software (Leica Microsystems, Germany). A number of six micrographs were acquired at × 500 magnification, for each specimen (n = 18). The software Adobe Photoshop™ (Adobe Systems Software, Ireland) was used to analyze black and white images, with the black regions representing the pores while the white regions represented the bulk material. Image J™ software (National Institutes of Health, USA) was used to quantify the porosity on the cross-sections.
Afterwards, surfaces were sputter coated with a AgPd thin layer for scanning electron microscopy (SEM) analyses by using a SEM (TM3030™, Hitachi, Japan) coupled to energy dispersive spectroscopy (EDX, Swift 2000, Hitachi, Japan). SEM analyses were carried out at 10 kV under secondary electrons (SE) to provide the topographic information of the microstructure of resin-matrix cement and tooth tissues. SEM images of the specimens were recorded at high magnification ranging from × 1000 up to × 20,000 under SE mode [38,39,40]. Microstructural analyses were carried out at different regions. On each specimen, a total of three micrographs were acquired at × 1000 magnification (n = 9). EDX was performed at 15 kV under backscattered electrons (BSE) following standard guidelines for chemical analyses of the inorganic fillers [38,39,40]. The chemical composition was acquired by rearranging the oxygen content to estimate the weight percentage of oxides regarding the most stable stoichiometric arrangement.
Statistical Analyses
Results were statistically analyzed by normality test Shapiro–Wilk and two-way ANOVA to determine statistical differences in values of diameter of the tooth root canals, GFRC post to dentin distance, and thickness of the remnant tooth structure between groups. Tukey test was applied to compare the results of GFRC post to dentin distance and thickness of the remnant tooth structure between the groups. A probability (p) value less than 0.05 (significance level at 5%) was considered statistically significant while a p value below 0.001 (significance level at 0.1%) was considered highly significant. The power analysis performed by ANOVA, to determine the number of specimens for each group (n), revealed a test power of 100% in the present study. Statistical analyses were carried out using OriginLab statistical software (OriginPro 2023b™, Origin Lab, Northampton, MA, USA).
Results
As seen in Fig. 3, CBCT images revealed differences in diameter at different thirds of the tooth root canal prior to the placement of the endodontic post (Fig. 2B). The endodontic post to dentin distance was measured at mesial, distal, buccal, and lingual regions. The mean values and standard deviation values recorded for tooth remnant thickness are shown in Fig. 4. On mesial and distal regions, invasive preparation revealed the lowest values of remnant tooth tissues at the three thirds (coronal, middle, and apex) compared to the standard preparation and minimally-invasive (conservative) sha**. At mesial side, the mean values of remaining tooth thickness at the coronal third were recorded at 1.63, while mean values of 1.49 and 1.21 mm were recorded at middle and apical thirds, respectively (Fig. 4A). Results showed statistically significant differences regarding the invasive sha** (p < 0.05). At the distal level, the mean values of remaining tooth thickness were recorded at 1.72, 1.46, and 1.45 mm, at coronal, middle, and apical thirds, respectively (Fig. 4B). Thus, thickness of the remnant tooth tissues decreased from the coronal to the apex third region.
Specimens revealed larger remnant tooth tissues at the mesial and distal regions after minimally-invasive (conservative) sha**. As expected, thickness of the remnant tooth tissues also decreased from the coronal to the apex third region. At mesial side, the mean values of remaining tooth thickness were recorded at 2.01, 1.89, and 1.62 mm, at coronal, middle, and apical thirds, respectively (Fig. 4A). At the distal side, the mean values of remaining tooth thickness were recorded at 2.08, 1.85, and 1.31 mm, at coronal, middle, and apical thirds, respectively (Fig. 4B). Regarding coronal and middle thirds, specimens on conservative preparation did not show statistically significant differences (p = 0.16) when compared to the standard preparation. Statistical analyses of the measurements of remnant tooth structure thickness nm are shown in Table 1.
The mean values and standard deviation values recorded for diameter measurement of tooth root canals after endodontic sha** procedures are shown in Fig. 5.
The invasive preparation provided the largest mean values of tooth root canal diameter. The diameter measurement mean values of tooth root canals after endodontic sha** procedures were recorded at 2.07, 1.91, and 1.45 mm, at coronal, middle, and apical thirds, respectively (Fig. 5). Results showed statistically significant differences between coronal or middle and apical third (p < 0.05). Specimens on conservative preparation revealed the smallest mean values of tooth root canal diameter. The diameter measurement mean values of tooth root canals after endodontic sha** procedures were recorded at 1.16, 0.74, and 0.55 mm, for coronal, middle, and apical thirds, respectively (Fig. 5). Results showed statistically significant differences between coronal and apical third (p < 0.05).
The mean values and standard deviation values recorded on the post to intracanal dentin distance measurement are shown in Fig. 6.
As seen in Fig. 6, the invasive sha** resulted in the largest distance measurements from the post to the tooth root intracanal surfaces in the different sections (coronal, middle and apex) at mesial, distal, and vestibular. Results showed statistically significant differences between groups (p < 0.05). However, specimens on standard sha** showed slightly higher values than that recorded for specimens from invasive preparation at the lingual anatomic side. Statistical analyses of the measurements of the post to intracanal dentin distance are shown in Table 2.
At the mesial side of specimens from invasive sha**, the distance mean values from the GFRC post to the intracanal dentin surfaces were recorded at 0.59, 0.42, and 0.13 mm, at coronal, middle, and apical thirds, respectively (Fig. 6A). At the distal side, the mean values were recorded at 0.45, 0.36, and 0.7 mm, at coronal, middle, and apical thirds, respectively (Fig. 6B). At the buccal side, the distance mean values from the GFRC post to the intracanal dentin surfaces were recorded at 1.43, 0.54, and 0.27 mm, respectively, at coronal, middle, and apical thirds, respectively (Fig. 6C). Finally, standard sha** revealed slightly higher values than that recorded for the invasive sha** at the lingual side. On the standard sha**, the distance mean values from the GFRC post to the intracanal dentin surfaces were recorded at 0.86, 0.59 and 0.25 mm, at coronal, middle, and apical thirds, respectively (Fig. 6D).
CBCT images of the GFRC post to dentin after invasive sha** of the tooth root canal are shown in Fig. 7A and C. The distance from the GFRC post to the remaining dentin was much more uniformly than at the coronal level. Microscopic images of the interfaces involving dentin, resin-matrix cement, and GFRC post can be seen in Fig. 7B and D and Fig. 8. As seen in Fig. 7A and B, the invasive tooth preparation promoted a larger destruction of tooth root inner tissues as noticeable by the space from the GFRC post to the intracanal dentin surfaces. Results showed statistically significant differences between groups (p < 0.05). The space was filled by the resin-matrix cement although macro-scale voids were detected (Fig. 7B and D). In Fig. 7C, the post was fitted in the apex third region that decrease the resin-matrix cement layer as seen by the optical microscopy analysis (Fig. 7D and 8).
CBCT and microstructural images of the GFRC post to dentin distance on invasive sha**. CBCT images of a A coronal and C sagittal cross-section plane of the tooth with a GFRC post prior to cementation: zoom view of A coronal and C apical tooth third. B Optical microscopy of a horizontal cross-section of the GFRC post to dentin interface at the B coronal and D apical third after cementation
As seen in Fig. 8, the resin-matrix cement layer varies even though the GFRC post was in a good fit at the apical third region. Also, defects and macro-scale voids were detected at the resin-matrix cement layer (Fig. 8C and D).
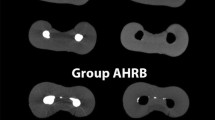
CBCT images of the multi-filament GFRC post to dentin after invasive sha** of the tooth root canal are shown in Fig. 9. Before cementation, there is still noticeable space at the coronal third of the multi-filament GFRC post to dentin region although the apical third region was partially filled with the GFRC filaments.
Microscopic images of the interfaces involving dentin, resin-matrix cement, and multi-filament GFRC post can be seen in Fig. 10. It can be seen the GFRC filaments are distributed in the tooth root canal. However, the resin-matrix cement volume was high among the filaments that increased the presence of defects and macro-scale voids as seen in Fig. 10A–C.
Discussion
In this study, the tooth root canal's diameter, remnant dentin thickness, and the GFRC post to dentin distance were measured by CBCT and traditional X-ray analyses. Tooth root canals were prepared by invasive, standard, or minimally invasive (conservative) endodontic procedures and then inspected by CBCT and traditional X-ray analyses. Then, a second set of analyses was performed after placement of GFRC posts. Also, GFRC posts were cemented and cross-sectioned for microscopic analyses. The results of the present study revealed similar thickness values of remnant dentin between conservative and standard canal sha**. Also, the distance of GFRC post to dentin varied considering the anatomic features. The coronal third showed the highest post to dentin distance that provided the highest values of resin-matrix cement layer thickness. Thus, the present results support the hypothesis that dentin thickness decreases after invasive tooth root canal preparation and the GFRC post to dentin distance varies considering anatomic and sha** factors.
Regarding the thickness of remaining dentin on the mesial and distal side, invasive sha** of tooth root canal resulted in less remaining dentin compared to standard and minimally invasive root canal sha**. At coronal level, the minimally-invasive sha** showed similar values of remnant tooth root tissues when compared to the standard procedure, although the minimally-invasive approach promoted larger remaining tooth root tissues on a high number of anatomical sites, as seen in Fig. 4. Regarding the remaining root thickness on the distal side of the tooth, the standard sha** showed higher mean values at the coronal and the apical level when compared with the invasive approach. Invasive preparation remains the most destructive preparation method considering remaining tooth root thickness (Fig. 4B). Also, the invasive preparation promoted the largest tooth root canal diameter values at the coronal, middle, and apex thirds.
The thin thickness of tooth root tissues can promote a high risk of failures by catastrophic fracture under occlusal loading. A root fracture is a critical type of failure in endodontically treated teeth. Additionally, other several complications can occur during endodontic preparation such as perforations, canal transportation, protrusion, zipper formation, and instrument fracture [39,40,41]. Micro- and macro-scale cracks can appear in the dentin and enamel tissues on reciprocating friction movements over the endodontic treatment [39, 42, 43]. For instance, the rotary and reciprocal NiTi endodontic files cause a significant increase in the percentage of microcracks when compared to the handheld NiTi file [39, 44, 45]. Thus, cracks are spots of stress concentration leading to the catastrophic fracture from crack propagation [39, 42, 43]. A study reported that ProTaper Universal™ and WaveOne™ systems showed significant improvements on the major geometric parameters (area, perimeter, roundness, major diameter, minor diameter, volume, surface area, structure model index) in comparison with the Reciproc™ and SAF™ systems [46]. However, all systems performed similarly regarding the amount of worn dentin surfaces when the brushing motion was applied. Neither technique was capable of completely preparing the oval-shaped root canals [46]. In comparison with the present results, previous findings have reported that an adequate selection of instruments and techniques can prevent excessive intraradicular dentin damage leading to an enhanced stress distribution through the tooth tissues [39, 41, 47,48,49]. A study emphasized instrumentation issues in larger root canals when compared to small and even complex systems [44]. Such anatomic features reveals clinical limitations since tapered instruments for apical sha** might weaken the tooth root structure at the mesiodistal surfaces [46, 50]. Also, variations in sha** and removal of dentin occurs due to the sensitivity of the operator.
Considering the tooth mesial side, standard sha** of tooth root canals provided shorter distances from the GFRC post to the intracanal dentin surfaces when compared to the invasive one (Fig. 6A). In the distal view, the standard sha** showed higher mean values on the distance from the GFRC post to the remaining intracanal dentin at the coronal measurement of the tooth although revealed quite lower values at the apical and middle thirds (Fig. 6B). On the tooth buccal side, the invasive sha** at all different thirds revealed high values of distance from the GFRC post to the remaining intracanal dentin when compared to the standard preparation. However, there were no statistical differences in the invasive sha** at the apical and middle third of the tooth (Fig. 6C). Also, a multi-filament GFRC post revealed misfit of filaments mainly at the coronal third as seen in Fig. 9 and therefore there are limitations regarding the number and diameter of filaments.
On the tooth root canal filling, heating of thermoplastic gutta-percha increases plastic deformation and fitting to the spaces within root canal system with oval-shape design. On the cooling of the gutta-percha, shrinkage occurs and results in macro- and micro-scale voids and gaps along the root canal filling. A recent study also proposed that the use of alternative sealing materials to gutta-percha would be beneficial to prevent microleakage when the size of the apex is larger than ISO #50 [50, 51]. Burs and endodontic files with the same diameter of standard GFRC posts often allow a good fit of the posts within the tooth root canals although unfortunately sha** and anatomical discrepancies cause variations in the thickness of resin-matrix cement, as seen in Figs. 7 and 8. Even though increasing the GFRC post diameter can improve the mechanical behavior of the endodontic assembly, a variation of the resin-matrix cement can occur and therefore risks of further fracture would depend on the thickness and number of defects. In the same way, a large amount of resin-matrix cement can be noticed in the microstructure of the multi-filament GFRC post interface. Indeed, the resin-matrix cement layer tends become thick in clinical situations concerning the misfit of the GFRC post to the intracanal space [47]. Thick layers of resin-matrix cement are susceptible to the presence of defects such as macro- to nano-scale voids, pores, or cracks [27, 47]. Also, the polymerization shrinkage stresses become higher in thick resin-matrix cement layers [47]. In this way, failures related to thick resin-matrix cement layer can occur in the oral environment such as: fracture at the GFRC post to dentin interface, microleakage, and progressive degradation that can further compromise the post-endodontic adhesive interface [52, 53].
On the other hand, the literature has reported controversial results on the influence of resin-matrix cement thickness on the adhesion of standard and custom-made endodontic posts to tooth root canal [47]. Several studies have suggested that a thick layer of cement may induce detachment of GFRC posts [26, 27, 47, 54,55,56]; although other studies [57, 58] have shown that the bond strength of the GFRC interface was not influenced by increasing the thickness of the resin-matrix cement layer. Self-adhesive resin-matrix cements have been recently suggested for the cementation of GFRC posts and indirect restorations since the self-adhesive cements are applied without a previous conditioning system over the surfaces [47, 59]. Nevertheless, the use of self-adhesive resin-matrix cements is limited in enclosed micro-scale spaces. The lack of direct clinical visualization and monitoring of adhesive procedures increase the risks of clinical failures and defects into the resin-matrix cement, leading to a low bond strength of GFRC posts to resin-matrix cements and the root dentin [47]. It should be highlighted that clinicians should seek improved cementation techniques providing the lowest resin-matrix cement thickness around GFRC posts. Furthermore, custom-made procedures involving GFRC posts and resin-matrix composites are strategic approaches to promote an adequate fitting of GFRC posts to different tooth intracanal shapes [46, 52].
Conclusions
In the present study, a novel combination of methods for preparation of specimens and image analyses of dental restorative interfaces provided enough data for measuring the tooth root canal sha**, remnant tissues, and the resin-matrix cement layer after GFRC post cementation. Within the limitations of this in vitro study, the following conclusions can be drawn:
-
A minimally-invasive tooth root canal sha** provides adequate volume of remnant dentin and enamel tissues for further restoration. A minimally-invasive approach can promote a proper fitting of glass fiber- reinforced composite (GFRC) post to the intraradicular dentin allowing a well-distribution of the resin-matrix cement volume that decreases the risks of defects such as voids and cracks. Also, the tooth tissues must be preserved to maintain the mechanical integrity of the restored tooth. On the other hand, the invasive tooth root canal sha** promotes a severe destruction of the tooth root tissues that increases the risks of catastrophic fractures from the propagation of cracks.
-
After invasive sha**, the fitting of the standard or multi-filament GFRC post is compromised that increases the occurrence of spaces from the post to the intraradicular dentin surfaces mainly at the coronal third. Spaces are filled by resin-matrix cements on cementation although thick resin-matrix cement layers increase the probability of defects (i.e., cracks and pores) and stress concentration leading to catastrophic fractures. The fitting of multi-filament GFRC posts has limitations regarding the number and diameter of filaments. Thus, the volume of resin-matrix cement around multi-filament GFRC posts varies among the filaments.
-
Considering the combination of X-ray and microscopy methods used in this study, further studies should assess the percentage of defects in different thickness of resin-matrix cements regarding standard and multi-filament GFRC posts. The chemical composition and viscosity of the resin-matrix cement should also be correlated with the filling of the intraradicular spaces. Also, the number and diameter of filaments of novel GFRC posts should be related to the anatomical conditions and sha** of tooth root canals.
Data Availability
All data generated or analyzed during this study are included in this published article. The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Code Availability
Not applicable.
References
X. Wang, X. Shu, Y. Zhang, B. Yang, Y. Jian, K. Zhao, Evaluation of fiber posts vs metal posts for restoring severely damaged endodontically treated teeth: a systematic review and meta-analysis. Quintessence Int. (Berlin, Germany: 1985) 50, 8–20 (2019)
A.C.L. Faria, R.C.S. Rodrigues, R.P. de Almeida Antunes, M.G.C. de Mattos, R.F. Ribeiro, Endodontically treated teeth: characteristics and considerations to restore them. J. Prosthodont. Res. 55, 69–74 (2011)
G. Corrêa, L.P. Brondani, V.F. Wandscher, G.K.R. Pereira, L.F. Valandro, C.D. Bergoli, Influence of remaining coronal thickness and height on biomechanical behavior of endodontically treated teeth: survival rates, load to fracture and finite element analysis. J. Appl. Oral Sci. 26, 1–11 (2018)
Y. Goto, J. Ceyhan, S.J. Chu, Restorations of endodontically treated teeth: new concepts, materials, and aesthetics. Pract. Proced. Aesthet. Dent. 21, 81–89 (2009)
M. Naumann, M. Schmitter, R. Frankenberger, G. Krastl, “Ferrule Comes First. Post Is Second!” fake news and alternative facts? A systematic review. J. Endod. 44, 212–219 (2018)
P.E. Fontana, T.C. Bohrer, V.F. Wandscher, L.F. Valandro, I.F. Limberger, O.B. Kaizer, Effect of ferrule thickness on fracture resistance of teeth restored with a glass fiber post or cast post. Oper. Dent. 44, E299-308 (2019)
E.S. Reeh, H.H. Messer, W.H. Douglas, Reduction in tooth stiffness as a result of endodontic and restorative procedures. J. Endod. 15, 512–516 (1989)
M.T. Pettiette, C. Phillips, M. Trope, Effect of endodontic instrument taper on post retention. J. Endod. 29, 65–68 (2003)
D. Clark, J. Khademi, Modern molar endodontic access and directed dentin conservation. Dent. Clin. N. Am. 54, 249–273 (2010)
Y. Guruprasada, Restoration of fractured endodontically treated mandibular first molar using custom made cast post and core. Med. J. 71, S221–S223 (2015)
C.J. Soares, M.P. Rodrigues, A.L. Faria-E-Silva, P.C.F. Santos-Filho, C. Veríssimo, H.-C. Kim et al., How biomechanics can affect the endodontic treated teeth and their restorative procedures? Braz. Oral Res. 32, e76 (2018)
G.A. Galhano, L.F. Valandro, R.M. de Melo, R. Scotti, M.A. Bottino, Evaluation of the flexural strength of carbon fiber-, quartz fiber-, and glass fiber-based posts. J. Endod. 31, 209–211 (2005)
R.D. Trushkowsky, Esthetic and functional consideration in restoring endodontically treated teeth. Dent. Clin. N. Am. 55, 403–410 (2011)
E. Bru, L. Forner, C. Llena, A. Almenar, Fibre post behaviour prediction factors. A review of the literature. J. Clin. Exp. Dent. 5, e150–e153 (2013)
R.R. Barcellos, D.P.D. Correia, A.P. Farina, M.F. Mesquita, C.C.R. Ferraz, D. Cecchin, Fracture resistance of endodontically treated teeth restored with intra-radicular post: the effects of post system and dentine thickness. J. Biomech. 46, 2572–2577 (2013)
P.C.F. Santos-Filho, C. Veríssimo, P.V. Soares, R.C. Saltarelo, C.J. Soares, L.R. Marcondes Martins, Influence of ferrule, post system, and length on biomechanical behavior of endodontically treated anterior teeth. J. Endod. 40, 119–123 (2014)
W. Cheung, A review of the management of endodontically treated teeth. Post, core and the final restoration. J. Am. Dent. Assoc. 136, 611–619 (2005)
Y. Zhang, B.R. Lawn, Novel zirconia materials in dentistry. J. Dent. Res. 97, 140–147 (2018)
R.C. Garvie, R.H. Hannink, R.T. Pascoe, Ceramic steel? Nature 258, 703–704 (1975)
M. Abduljawad, A. Samran, J. Kadour, M. Al-Afandi, M. Ghazal, M. Kern, Effect of fiber posts on the fracture resistance of endodontically treated anterior teeth with cervical cavities: an in vitro study. J. Prosthet. Dent. 116, 80–84 (2016)
A. Talekar, G. Chaudhari, S.K. Mallineni, S. Kothare, A. Patil, P. Musale et al., Ex vivo assessment of natural teeth wear against zirconia and novel glass-fiber-reinforced composite crowns in primary teeth by a three-dimensional assessment method. Int. J. Dent. (2021). https://doi.org/10.1155/2021/9670982
J.C.M. Souza, C.S. Silva, J. Caramês, B. Henriques, A.P. Novaes de Oliveira, F.S. Silva et al., Wear behavior of dental glass-ceramics: a sco** review on the damage of opposing tooth enamel surfaces. Biotribology 21, 100116 (2020)
J.C.M. Souza, A.C. Bentes, K. Reis, S. Gavinha, M. Buciumeanu, B. Henriques et al., Abrasive and sliding wear of resin composites for dental restorations. Tribol. Int. 102, 154–160 (2016). https://doi.org/10.1016/j.triboint.2016.05.035
J.C.M. Souza, M.S.T. Correia, B. Henriques, A.P. Novaes De Oliveira, F.S. Silva, J.R. Gomes, Micro-scale abrasion wear of novel biomedical PEEK composites for restorative dentistry. Surf. Topogr. (2019). https://doi.org/10.1088/2051-672X/ab0324
K. Bitter, J. Noetzel, O. Stamm, J. Vaudt, H. Meyer-Lueckel, K. Neumann et al., Randomized clinical trial comparing the effects of post placement on failure rate of postendodontic restorations: preliminary results of a mean period of 32 months. J. Endod. 35, 1477–1482 (2009)
C. D’Arcangelo, M. Cinelli, F. De Angelis, M. D’Amario, The effect of resin cement film thickness on the pullout strength of a fiber-reinforced post system. J. Prosthet. Dent. 98, 193–198 (2007)
V. Fernandes, A.S. Silva, O. Carvalho, B. Henriques, F.S. Silva, M. Özcan et al., The resin-matrix cement layer thickness resultant from the intracanal fitting of teeth root canal posts: an integrative review. Clin. Oral Investig. 25, 5595 (2021)
P. Ausiello, S. Ciaramella, M. Martorelli, A. Lanzotti, F. Zarone, D.C. Watts et al., Mechanical behavior of endodontically restored canine teeth: effects of ferrule, post material and shape. Dent. Mater. 33, 1466–1472 (2017)
A.V. Barbosa Kasuya, I.N. Favarão, A.C. Machado, P.H. Rezende Spini, P.V. Soares, R.B. Fonseca, Development of a fiber-reinforced material for fiber posts: evaluation of stress distribution, fracture load, and failure mode of restored roots. J. Prosthet. Dent. 123, 829–838 (2020)
P.C. Lazari, R.C.N. de Oliveira, R.B. Anchieta, E.O. de Almeida, A.C. Freitas Junior, S. Kina et al., Stress distribution on dentin-cement-post interface varying root canal and glass fiber post diameters. A three-dimensional finite element analysis based on micro-CT data. J. Appl. Oral Sci. 21, 511–517 (2013)
V. Nagendrababu, P.E. Murray, R. Ordinola-Zapata, O.A. Peters, I.N. Rôças, J.F.J. Siqueira et al., PRILE 2021 guidelines for reporting laboratory studies in Endodontology: explanation and elaboration. Int. Endod. J. 54, 1491–1515 (2021)
K. Ambica, K. Mahendran, S. Talwar, M. Verma, G. Padmini, R. Periasamy, Comparative evaluation of fracture resistance under static and fatigue loading of endodontically treated teeth restored with carbon fiber posts, glass fiber posts, and an experimental dentin post system: an in vitro study. J. Endod. 39, 96–100 (2013)
E.M. Souza, L.M. do Nascimento, E.M. Maia Filho, C.M.C. Alves, The impact of post preparation on the residual dentin thickness of maxillary molars. J. Prosthet. Dent. 106, 184–190 (2011)
G.C. Lopes, A. Ballarin, L.N. Baratieri, Bond strength and fracture analysis between resin cements and root canal dentin. Aust. Endod. J. 38, 14–20 (2012)
O. Parlar Oz, A. Secilmis, C. Aydin, Effect of laser etching on glass fiber posts cemented with different adhesive systems. Photomed. Laser Surg. 36, 51–57 (2018)
L.R. Fava, P.M. Dummer, Periapical radiographic techniques during endodontic diagnosis and treatment. Int. Endod. J. 30, 250–261 (1997)
S.Y. Shaikh, S.S. Shaikh, Direct linear measurement of root dentin thickness and dentin volume changes with post space preparation: a cone-beam computed tomography study. Contemp. Clin. Dent. 9, 77–82 (2018)
N.R. Chaudhary, D.J. Singh, R. Somani, S. Jaidka, Comparative evaluation of efficiency of different file systems in terms of remaining dentin thickness using cone-beam computed tomography: an in vitro study. Contemp. Clin. Dent. 9, 367–371 (2018)
E. Çiçek, M.M. Koçak, B.C. Sağlam, S. Koçak, Evaluation of microcrack formation in root canals after instrumentation with different NiTi rotary file systems: a scanning electron microscopy study. Scanning 37, 49–53 (2015)
F. Haupt, M. Meinel, A. Gunawardana, M. Hülsmann, Effectiveness of different activated irrigation techniques on debris and smear layer removal from curved root canals: a SEM evaluation. Aust. Endod. J. 46, 40–46 (2020)
H.-C. Kim, Y.-J. Hwang, D.-W. Jung, S.-Y. You, H.-C. Kim, W. Lee, Micro-computed tomography and scanning electron microscopy comparisons of two nickel-titanium rotary root canal instruments used with reciprocating motion. Scanning 35, 112–118 (2013)
Y.-M. Kim, T. Yi, J.-S. Choi, S. Lee, Y.H. Jang, C.-H. Kim et al., Bone marrow-derived clonal mesenchymal stem cells as a source of cell therapy for promoting vocal fold wound healing. Ann. Otol. Rhinol. Laryngol. 122, 121–130 (2013)
G. Kesler, R. Gal, A. Kesler, R. Koren, Histological and scanning electron microscope examination of root canal after preparation with Er:YAG laser microprobe: a preliminary in vitro study. J. Clin. Laser Med. Surg. 20, 269–277 (2002)
A.P. Farina, A.L. Weber, B.P. Severo, M.A. Souza, D. Cecchin, Effect of length post and remaining root tissue on fracture resistance of fibre posts relined with resin composite. J. Oral Rehabil. 42, 202–208 (2015)
B.H. Kivanç, T. Alaçam, O.I.A. Ulusoy, O. Genç, G. Görgül, Fracture resistance of thin-walled roots restored with different post systems. Int. Endod. J. 42, 997–1003 (2009)
M.A. Versiani, G.B. Leoni, L. Steier, G. De-Deus, S. Tassani, J.D. Pécora et al., Micro-computed tomography study of oval-shaped canals prepared with the self-adjusting file, Reciproc, WaveOne, and ProTaper universal systems. J. Endod. 39, 1060–1066 (2013)
R.M.H.-C. Marcos, G.R. Kinder, E. Alfredo, T. Quaranta, G.M. Correr, L.F. da Cunha et al., Influence of the resin cement thickness on the push-out bond strength of glass fiber posts. Braz. Dent. J. 27, 592–598 (2016)
J.P.M. Tribst, A.M.O. Dal Piva, M.M. Penteado, A.L.S. Borges, M.A. Bottino, Influence of ceramic material, thickness of restoration and cement layer on stress distribution of occlusal veneers. Braz. Oral Res. 32, e118 (2018)
Z. Wang, Y. Shen, M. Haapasalo, Root canal wall dentin structure in uninstrumented but cleaned human premolars: a scanning electron microscopic Study. J. Endod. 44, 842–848 (2018)
A. Keleş, C. Keskin, Apical root canal morphology of mesial roots of mandibular first molar teeth with Vertucci Type II configuration by means of micro-computed tomography. J. Endod. 43, 481–485 (2017)
C.H. Wang, J.K. Du, H.Y. Li, H.C. Chang, K.K. Chen, Factorial analysis of variables influencing mechanical characteristics of a post used to restore a root filled premolar using the finite element stress analysis combined with the Taguchi method. Int. Endod. J. 49, 690–699 (2016)
G. Maroulakos, J. He, W.W. Nagy, The post-endodontic adhesive interface: theoretical perspectives and potential flaws. J. Endod. 44, 363–371 (2018)
F. Mannocci, J. Cowie, Restoration of endodontically treated teeth. Br. Dent. J. 216, 341–346 (2014)
G.M. Gomes, E.C. Rezende, O.M. Gomes, J.C. Gomes, A.D. Loguercio, A. Reis, Influence of the resin cement thickness on bond strength and gap formation of fiber posts bonded to root dentin. J. Adhes. Dent. 16, 71–78 (2014)
E. Özcan, A.R. Çetin, A.R. Tunçdemir, M. Ülker, The effect of luting cement thicknesses on the push-out bond strength of the fiber posts. Acta Odontol. Scand. 71, 703–709 (2013)
F. Egilmez, G. Ergun, I. Cekic-Nagas, P.K. Vallittu, L.V.J. Lassila, Influence of cement thickness on the bond strength of tooth-colored posts to root dentin after thermal cycling. Acta Odontol. Scand. 71, 175–182 (2013)
V. Nova, L. Karygianni, M.J. Altenburger, M. Wolkewitz, A.M. Kielbassa, K.-T. Wrbas, Pull-out bond strength of a fibre-reinforced composite post system luted with self-adhesive resin cements. J. Dent. 41, 1020–1026 (2013)
J. Perdigão, G. Gomes, V. Augusto, The effect of dowel space on the bond strengths of fiber posts. J. Prosthodont. 16, 154–164 (2007)
C. Pulido, C.A.G. Arrais, G.M. Gomes, A.P.G.B. Franco, H.J. Kalinowski, A. Dávila-Sánchez et al., Kinetics of polymerization shrinkage of self-adhesive and conventional dual-polymerized resin luting agents inside the root canal. J. Prosthet. Dent. 125, 535–542 (2021)
Acknowledgements
The authors acknowledge the Portuguese Foundation for Science and Technology (FCT), Portugal, and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil, for the finnancial support. The authors also acknowledge Coltene Whaledent (USA) and VOCO (Germany) for providing materials used in the present study.
Funding
Open access funding provided by FCT|FCCN (b-on). This work was supported by FCT-Portugal in the subject of the following projects: UIDB/04436/2020, UIDP/04436/2020, and PTDC/EMEEME/ 4197/2021. Additionally this study was partially financed by CAPES through the projects: Project CAPES-PRINT/88881.310728/2018-01; CAPES-HUMBOLDT Program (Grant number: 88881.197684/2018-01) and CAPES-DAAD PROBRAL Programme (Ref: 88887.628082/2021-00).
Author information
Authors and Affiliations
Contributions
Conceptualization: JCMS, BH, VF, CS; methodology: VF, CS, OC, and JCMS; investigation: VF, CS, OC; writing—original draft preparation: VF, CS; writing—review and editing, JCMS, MO, FS, BH, Supervision: FS, JCMS, and MO. All authors participated in the writing process, read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that there is no conflict of interests.
Ethical Approval
All procedures performed involving human participants followed the ethics standards of the research committee of the University Institute of Health Sciences (IUCS) at Cooperativa Ensino Superior Politécnico Universitário (CESPU), Portugal, and therefore with the 1964 Helsinki declaration and its later amendments or comparable ethics standards. The project for the present study was previously reviewed and approved by the IUCS Ethics committe with the following Ethics Protocols Reference Number: CE/IUCS/CESPU-18/2022.
Informed Consent
Informed consent was unnecessary following the national regulations and since all data were processed anonymously. The need for informed consent was waived by the ethics committee/Institutional Review Board of IUCS at CESPU, Portugal.
Consent for Publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Souza, J.C.M., Soares, C., Fernandes, V. et al. Intraradicular Diameter, Remnant Dentin Thickness, and Endodontic Post to Dentin Distance: CBCT and Microscopic Analyses. Biomedical Materials & Devices 2, 384–396 (2024). https://doi.org/10.1007/s44174-023-00088-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44174-023-00088-7