Abstract
Background
Few studies have estimated cumulative health care costs post-diagnosis for individuals with autism spectrum disorder (ASD).
Objectives
Using an incidence-based approach, the objective of this analysis was to estimate cumulative costs of ASD to the Ontario health care system of children and adolescents.
Methods
Using administrative health records from Ontario, Canada’s most populous province, a retrospective, population-based, incident cohort study of children and adolescents aged 0–19 years old diagnosed with ASD was undertaken to estimate cumulative health care costs of ASD to the health care system from 2010 to 2019. Cumulative health care costs in 2021 Canadian dollars (CAD) from diagnosis to death or end of observation period were estimated using a consistent estimator based on the inverse probability weighting technique. Cumulative health care costs (and respective 95% confidence intervals [CI]) were estimated for 1, 5 and 10 years post-diagnosis by sex, age group and health service.
Results
In 2010, there were 2867 diagnosed cases of ASD; in 2019, the number of incident cases had risen to 6072. The first year (i.e., 1-year) post-diagnosis cost of ASD was $4710.18 CAD (95% CI 4560.28–4860.08); just under a third of costs were for physician services. Total cumulative 5- and 10-year discounted costs were $16,025.95 CAD (15,371.64–16,680.26) and $32,635.76 CAD (28,906.94–36,364.58), respectively. Mean costs were higher for females and older age groups.
Conclusions
These results suggest that costs of ASD are high in the year of diagnosis and then increase at a steady rate thereafter. This information will help with future resource planning within the health care sector to ensure individuals with ASD are supported once their diagnosis is established.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The economic burden of autism spectrum disorder (ASD) is large, in particular during the first year post-diagnosis. |
In the first year post-diagnosis, physicians have an important role in coordinating care for individuals with ASD, referring them to specialised services and managing comorbidities. |
As treatments for ASD are developed, knowledge of when costs are incurred will be required for clinical decision making and cost-effectiveness analysis efforts. |
1 Introduction
Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how individuals interact with others, behave, communicate, and learn [1]. Although ASD is typically thought of as a childhood disorder, associated costs can also occur in adolescence and beyond [2]. A recent systematic review found that the overall medical and health care costs of people with ASD increase steadily over the lifetime [3]. However, few studies have estimated cumulative health care costs post-diagnosis for individuals with ASD. One study estimated direct medical costs due to ASD in the United States using a hypothetical incident cohort of individuals born in 2000 and diagnosed with ASD in 2003 and estimates of health care utilisation and costs of direct medical care obtained from a literature review and database analysis [2]. The study found lifetime per capita direct medical costs due to ASD of $305,956 (2003 USD). Another study produced updated estimates of societal lifetime economic costs associated with ASD for the United States (US) and the United Kingdom (UK) by undertaking a literature review [4]. The study found that the total societal lifetime cost of individuals with ASD and intellectual disability was estimated at US$2.4 million for the US and £1.5 million (US$2.2 million) for the UK, while the respective costs for individuals with ASD without intellectual disability was estimated at US$1.4 million in the US and £0.92 million (US$1.4 million) in the UK. Based on previous work, which suggests that direct medical costs make up <5% of total societal costs [3], it is likely that direct medical costs for individuals with ASD with and without intellectual disability would be at most US$120,000 and US$70,000 in the US and US$110,000 and US$70,000 in the UK.
Although these studies estimated lifetime costs (i.e., cumulative costs from diagnosis to death) [2, 4], these estimates were derived using data from a range of different published studies, some now dated, which employed different methodologies and were of differing quality, and obtained through modelling, which required making assumptions. While there is great value in understanding lifetime costs, it is also important to have estimates that are based on real-world data, particularly during the earlier years post-ASD diagnosis. Using administrative health care data, one study from Quebec, Canada estimated incidence costs for youth for the first 5 years post-diagnosis but only focused on costs of psychiatric care (i.e., psychiatric hospitalisations, GP and specialist visits and emergency department visits and drugs) [5]. The authors found mean costs of psychiatric care of $11,009, $6937, $4812, $5971 and $5636 (2016 CAD) in the first, second, third, fourth and fifth years, respectively. This present study employed real-world data on most health services provided through the administration of Ontario’s health insurance plan and included virtually all children and adolescents diagnosed with ASD in Ontario. Using an incidence-based approach, the objective of this analysis was to estimate cumulative costs to the Ontario health care system of ASD in children and adolescents. Cumulative costs were estimated for the first year post-diagnosis (i.e., 1-year costs), by sex and health service, as well as for 5- and 10-year periods post-diagnosis. These estimates will help inform decision makers to understand the costs of ASD to the health care system and thus guide decisions around resource allocation regarding early life interventions, which may help inform policies that seek to reduce high health care expenditures later in early adulthood.
2 Methods
2.1 Study Design and Setting
We undertook a retrospective, population-based, incident cohort study of children and adolescents aged 0–19 years old diagnosed with ASD to estimate total cumulative health care costs to the health care system, using data from Ontario, Canada’s most populous province (2019 population 14.6 million).
2.2 Data
We employed health records obtained through the administration of Ontario’s health insurance system and made available at ICES, an independent, non-profit research institute in Toronto, Ontario. The ICES data repository contains individual-level linkable and longitudinal data on most publicly funded health care services for all legal residents of Ontario. The following health services databases were used in this analysis: Discharge Abstract Database, Ontario Mental Health Reporting System, Continuing Care Reporting System, National Rehabilitation Reporting System, National Ambulatory Care Reporting System, Ontario Health Insurance Plan claims database, Ontario Drug Benefit Program database, and Home Care Database. In addition, the Registered Persons Database, a population-based registry, which contains data on individuals who contacted the health care system, was used to obtain patients’ date of birth, sex, eligibility for universal health care and status changes, and postal code of residence, while the 2011 and 2016 Census data were employed to obtain neighbourhood-level data, such as household income expressed in quintiles, and level of rurality of residence. A full description of each database can be found in Appendix Table A1 (see electronic supplementary material [ESM]). All databases were linked using unique encoded identifiers and analysed at ICES, in compliance with Ontario privacy legislation. The use of these data was authorised under section 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a Research Ethics Board.
2.3 Patient Population
All children and adolescents (ages 0–19 years old) with a valid health card number, residing in Ontario and diagnosed with ASD were included in the analysis. This age range was chosen based on a meta-analysis, which found a mean age at diagnosis of 60.48 months (i.e., 5 years) (95% CI 50.12–70.83) with a range of 30.90–234.57 months (i.e., 2.6–19.5 years old) [6]. To identify all incident cases of children and adolescents with ASD, a previously validated algorithm [7] was employed, where individuals were selected into the cohort if they had an ASD diagnostic code (ICD-9 code 299.x/ICD-10 code F84.x [autism, atypical autism, Asperger’s syndrome, other pervasive developmental disorders, pervasive developmental disorders unspecified], any diagnosis) for a single hospital discharge, emergency department visit or outpatient surgery, or three ASD physician billing codes (ICD-9 code 299 – child psychoses) within 3 years since birth. To ensure an incident cohort was obtained, all health records for each individual since database inception or date of birth, whichever came first when looking back, were examined. Incident cases were estimated from 2010 to 2019, for the total sample and by sex.
Incident cases of children and adolescents with ASD were characterised in terms of their socio-demographic characteristics—sex, age, neighbourhood income quintile and rural residence—and presence of chronic physical, mental and behavioural health conditions and intellectual disabilities common among children and adolescents with and without ASD—asthma, cancer, diabetes mellitus, ADHD, mood and/or anxiety disorders, learning and developmental disorders, Down syndrome, and Prader-Willi syndrome—ascertained either through disease registries (the Pediatric Oncology Group of Ontario Networked Information System and the Ontario Cancer Registry), validated algorithms or algorithms defined elsewhere [8,9,10,11,12,13].
2.4 Estimation of Observation Time
The number of days alive (and eligible for public health insurance) were estimated from diagnosis until the end of the observation period (i.e., December 31, 2020) for each child/adolescent. The sample was then divided into two groups: (i) censored (i.e., those who were alive during the entire observation period and whose death was not observed) and (ii) non-censored (i.e., those who died, moved out of the province, or who lost eligibility for public health insurance before the end of the observation period and for whom death or end of observation window was observed). See Appendix Table A3 in the ESM for the number of censored and non-censored groups of patients each year.
2.5 Estimation of Health Care Costs Incurred by the Public Third-Party Payers
A costing algorithm was used to estimate total direct patient-level health care costs of children and adolescents with ASD borne by the public third-party payers, the Ontario Ministries of Health and Long-term Care [14]. The algorithm’s costing methodology uses a bottom-up/micro-costing approach to cost services at the patient level, which identifies individual episodes of care or utilisation in the health care system and respective prices, or costs paid. Given Ontario’s public health insurance system, providers in a private marketplace rarely set prices; therefore, costs or amounts paid by the third-party payer were used. Where individual unit costs were not available (e.g., long-term care), a top-down approach, which allocates corporate aggregate costs to individual visits or cases/episodes of care, was employed. For hospital/institution-based care, such as hospitalisations and emergency departments, a measure of utilisation (which accounts for resource intensity using appropriate weights) was multiplied by a unit cost (e.g., cost per standard hospital stay, cost per Comprehensive Ambulatory Classification System weighted case). For other services, such as physician visits and outpatient prescription drugs, utilisation (i.e., number of visits, units) was multiplied by a unit cost (i.e., fee paid) obtained from Ontario Health Insurance Plan and Ontario Drug Benefit Program claims data, respectively, while for home care, utilisation was multiplied by a unit cost (i.e., cost per visit) obtained from the Ontario Ministry of Health [14]. Costs captured by the algorithm account for over 90% of all government-paid health care services, given the availability of relevant databases at ICES, and include costs directly related to ASD as well as other non-ASD related costs [14]. Further details on the costing methodology can be found elsewhere [14]. Costs were categorised into several health service categories—psychiatric hospitalisations, medical hospitalisations, other hospital/institution-based care (i.e., complex continuing care, inpatient rehabilitation and long-term care), hospital outpatient clinic visits, emergency department visits, other ambulatory care (i.e., same-day surgery, dialysis clinic visits and cancer clinic visits), physician services, outpatient prescription drug covered under the public provincial drug plan and home care—and reported in 2021 Canadian dollars (CAD, where 1 CAD = 0.7978 USD in 2021).
2.6 Estimation of Cumulative Mean Health Care Costs Incurred by the Public Third-Party Payers
One way to estimate mean cumulative health care costs when censoring is present is to reweight each case so that it represents not only itself but also some number of incomplete/censored cases [15]. Several estimators have been proposed to estimate cumulative mean health care costs [15]. Bang and Tsiatis proposed a consistent estimator based on the inverse probability weighting technique, which can be used to estimate cumulative costs [16]. The total cost of children and adolescents who died or were lost to attrition and those with complete cost information during the analysis period was weighted by one over the Kaplan-Meier (i.e., 1/KM) survival probability estimator, with reverse censoring (where deaths/attritors are denoted as 0 and censored cases as 1). The weighted costs were then summed and divided by the total study sample size to determine the mean total cost estimate in the presence of censoring. However, when the patient’s cost history is available, the Bang and Tsiatis estimator is not efficient since it does not use the cost information from censored observations. A more efficient (but also consistent) estimator is the one proposed by Zhao and Tian [17]. Given that we are estimating costs of children and adolescents, who typically do not have a long history of health care costs, and among whom death is rare, the estimator proposed by Zhao and Tian did not seem appropriate. Therefore, cumulative health care costs from diagnosis to death or end of observation period were estimated using the Bang and Tsiatis estimator, which employed data on observation time and health care costs incurred by the public third-party payers. Total mean cumulative health care costs for the first year after diagnosis, including date of diagnosis (i.e., 1-year costs), and respective 95% confidence intervals (CIs) were estimated for the full sample as well as by health service, sex and age group at diagnosis. In addition, total mean cumulative health care costs, undiscounted and discounted at 1.5% (in line with the Canadian Agency for Drugs and Technologies in Health recommendations [18]), were estimated for the 5- and 10-year periods, for the full sample, by sex and by age group at diagnosis. As a sensitivity analysis, we also estimated cumulative costs using the Zhao and Tian estimator as well as cumulative costs for the fully observed observations to assess the robustness of our findings.
3 Results
3.1 Characterisation of Patient Cohort
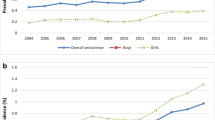
In 2010, there were 2867 diagnosed cases of ASD; in 2019, the number of incident cases had risen to 6072, a 2-fold increase (see Appendix Table A2 in the ESM). There were substantially more males diagnosed with ASD (76%–81%) than females (19%–24%) for all years; however, while the number of males doubled from 2010 to 2019 (from 2329 to 4648), it more than doubled for females (538 to 1424).The mean age at diagnosis was 6.93, with about two-fifths (40.6%) of the sample diagnosed between the ages of 4 and 8 (Table 1). For females, the mean follow-up time (in days) was 1850.75, while for males it was 1936.85. There were slightly more children and adolescents in the lowest neighbourhood income quintile (24.4%); most children and adolescents with ASD lived in urban settings (94.6%). Regarding clinical characteristics, a large percentage of children and adolescents with ASD had mood and/or anxiety disorders (46.4%) and learning and developmental disorders (40.6%) at diagnosis; 19.4% had asthma. Males and females did not look different on socio-demographic and clinical characteristics, as evidenced by the standardised mean difference (SMD) ≤0.10, except for age at diagnosis where females were slightly older than males (7.32 vs 6.82, respectively; SMD = 0.11).
3.2 Estimation of Mean Cumulative Health Care Costs Incurred by the Public Third-Party Payers
Mean cumulative health care costs for children and adolescents with ASD in the first year post-diagnosis was $4710.18 CAD (95% CI 4560.28–4860.08) (Table 2). Costs of physician services made up the largest proportion of total costs in the first year post-diagnosis (30%); other relevant costs included those for hospitalisations (17.9% and 15.4% for psychiatric and medical hospitalisations, respectively). The top diagnoses for psychiatric and medical hospitalisations included ASD, adjustment disorders and ADHD, and cancer treatment, epilepsy and pneumonia, respectively (not shown). Females had higher health care costs than males, overall ($6271.62 CAD [95% CI 5825.72–6717.52] vs $4281.40 CAD [95% CI 4135.06–4427.74]) and for most cost categories. Mean health care costs also differed by age group at diagnosis, with older individuals incurring higher costs (e.g., $10,975.24 CAD [95% CI 8905.29–13,045.20] for those aged 18–19 years vs $3169.43 CAD [95% CI 2985.55–3353.32] for 0- to 3-year-olds) (Table 3). For several health services, such as psychiatric hospitalisations, other hospital/institution-based care, physician services and outpatient prescription drugs, mean cumulative health care costs also increased with age at diagnosis.
Total mean cumulative 5- and 10-year discounted costs were $16,025.95 CAD (95% CI 15,371.64–16,680.26) and $32,635.76 CAD (95% CI 28,906.94–36,364.58), respectively (Table 4); 10-year costs were roughly two times the amount of 5-year costs, suggesting that, after the first year of diagnosis, cumulative costs increased at a constant rate. Cumulative costs were almost 50% higher for females than males for both 5 and 10 years ($21,090.61 CAD [95% CI 19,192.38–22,988.85] and $44,227.73 CAD [95% CI 35,964.85–52,490.61] vs $14,735.91 CAD [95% CI 14,073.66–15,398.17] and $29,881.73 CAD [95% CI 25,713.65–34,049.81]). Moreover, mean cumulative costs increased with age at diagnosis, where 18- to 19-year-olds had total mean cumulative 5- and 10-year discounted costs of $33,620.30 CAD (95% CI 25,838.98–41,401.63) and $65,419.36 CAD (95% CI 33,875.40–96,963.32), while 0- to 3-year-olds had total cumulative 5- and 10-year discounted costs of $11,410.36 CAD (95% CI 10,668.92–12,151.80) and $23,413.14 CAD (95% CI 18,902.54–27,923.74), respectively (Table 5). In the sensitivity analysis, it was found that the estimates of cumulative costs using the Zhao and Tian estimator and for the fully observed sample did not differ substantially from those obtained in the main analysis (though the latter values were more similar)—5-year discounted costs of $15,394.39 CAD (95% CI 14,875.11–15,913.66) and $15,963.32 CAD (95% CI 15,305.56–16,621.08) and 10-year discounted costs of $27,976.72 CAD (95% CI 27,129.99–28,823.44) and $32,938.07 CAD (95% CI 29,069.42–36,806.72), respectively (see Appendix Table A4 in the ESM for discounted costs by sex).
4 Discussion
Estimating cumulative long-term costs is important to obtain an understanding of how costs change over the life course. Few studies have estimated cumulative long-term costs for individuals with ASD. This study estimated cumulative 1-, 5- and 10-year costs. The first year post-diagnosis mean cost of ASD was estimated at $4710.18 CAD. Just under a third (30%) of total costs incurred were for physician services; other relevant costs included costs of psychiatric and medical care hospitalisations, which combined made up 33% of total costs. Total cumulative 5- and 10-year discounted mean costs were $16,025.95 CAD and $32,635.76 CAD. These results suggest that costs of ASD are high in the year of diagnosis and then increase at a steady rate thereafter.
These findings are in line with previous research estimating lifetime costs of ASD. One study from the US found that direct medical costs were highest in the first few years post-diagnosis between the ages of 3 and 7 years ($35,370 2003 USD) and then started to decline by the age of 8 years ($6013, 2003 USD) until the end of the life (between the ages of 63 and 66 years) to around $1027 (2003 USD) per capita, for a total lifetime cost of $305,956 (2013 USD) per capita (using a 3% discount rate) [2]. Moreover, excluding behavioural therapies, this study found that the largest proportion of direct medical costs were for physician and dental care in the first few years post-diagnosis, followed by hospital and emergency care [2]. Another study from Quebec, Canada also found that health care costs were higher in the first year post-diagnosis and then decreased over time, despite only focusing on costs of psychiatric care [5]. The authors found first year costs of $11,009 (2016 CAD), which are larger than those obtained in this study ($4710, 2021 CAD); this could be due to the inclusion of older individuals, as indicated in the Quebec study.
These results shed light on first-year costs post-diagnosis, namely the services that make up most of the costs incurred; this information will be helpful to inform future planning around resource allocation within the health care sector to ensure individuals with ASD are supported once their diagnosis is established. Health care costs were relatively high in the first year post-diagnosis. It was found that just under one-third of health care costs in the first year post-diagnosis were due to physician services alone. This is not surprising as physicians have an important role in coordinating care for individuals with ASD, referring them and their families to specialised services and managing their comorbidities, such ADHD and mood and/or anxiety disorders [19]. Thus, it is important to ensure that resources are devoted to ensuring children and adolescents with ASD have timely access to a physician. Although ASD is a lifelong condition, appropriate management of the condition through primary care can improve prognosis [19]. Hospitalisations (both psychiatric and medical) also made up a large portion of the total first-year cost (18% and 15%, respectively). These are costly episodes of care, which explain in part the high costs of care in the first year post-diagnosis. Some of these hospitalisations can likely be avoided in subsequent years with regular access to primary care. Moreover, this work provides long-term cumulative cost estimates, which will be an important input in understanding the future needs of individuals with ASD as they age. As treatments for ASD are developed, knowledge of when costs are incurred, relative to when benefits are expected, will be required for informed clinical decision making and cost-effectiveness analysis efforts [2].
This study employed a population-based sample, which included virtually all children and adolescents diagnosed with ASD in a jurisdiction with a universal health care system. Moreover, this study followed children and adolescents with ASD over a 10-year period to estimate cumulative costs. Prior work estimating cumulative costs, namely lifetime costs, has mainly used modelling, making use of data from several different data sources, which required making assumptions. This study included over 90% of all health care costs covered by the public third-party payer, thus providing a comprehensive estimate of the economic burden of ASD to the health care system. Furthermore, this work provided insight into cost incurred in the first year post-diagnosis. Finally, to our knowledge, this is the first study to estimate comprehensive cumulative total costs of ASD using data from Canada; existing work estimating cumulative costs has mainly used data from the US and the UK.
4.1 Limitations
Nonetheless, this study has some limitations. We were unable to include the costs of mental health care provided in community-based agencies; these data are not currently available for research purposes at ICES, the data provider. Thus, our cost estimates are likely an underestimate of the total cumulative costs incurred by children and adolescents with ASD, though these costs are likely a small portion of the overall burden to the health care system. Previous work has estimated lifetime costs. We estimated 10-year cumulative costs for incident cases between the ages of 0 and 19 years. After 10 years, these individuals were between the ages of 10 and 29 years and thus our 10-year cumulative cost estimates represent cumulative costs incurred from childhood to early adulthood, which are only a fraction of an individual’s lifetime. Future work should seek to follow incident cases of ASD over a longer period of time to obtain cumulative costs of longer duration. Moreover, other relevant costs of caring for individuals with ASD include therapeutic costs, (special) education costs, costs of lost productivity for adults with ASD, costs of informal care and lost productivity for family/caregivers, costs of accommodation and respite care, and out-of-pocket expenses. Future research should also consider estimating the cumulative costs of these components. Finally, while determining the costs associated with ASD is important, determining the incremental costs of ASD is also an important avenue of future research. Notwithstanding, these estimates will still be relevant for decision makers who require this information for resource allocation purposes as well as researchers undertaking ASD-related economic evaluations.
5 Conclusion
Understanding cumulative health care costs over the lifetime can help shed light on how costs vary over time and are important inputs for decision making. This study estimated 1-, 5- and 10-year costs for individuals with ASD using real-world data from a jurisdiction with a universal health care system. The first year (i.e., 1-year) post-diagnosis cost of ASD was $4710.18 CAD, where just under a third of costs were for physician services. Total cumulative 5- and 10-year discounted costs were $16,025.95 CAD and $32,635.76 CAD. These results suggest that costs of ASD are high in the year of diagnosis and then increase at a steady rate thereafter.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publ. 2013.
Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161(4):343–9.
Rogge N, Janssen J. The economic costs of autism spectrum disorder: a literature review. J Autism Dev Disord. 2019;49(7):2873–900.
Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168(8):721–8.
Croteau C, Mottron L, Dorais M, Tarride JE, Perreault S. Use, costs, and predictors of psychiatric healthcare services following an autism spectrum diagnosis: Population-based cohort study. Autism. 2019;23(8):2020–30.
van’t Hof M, Tisseur C, van Berckelear-Onnes I, van Nieuwenhuyzen A, Daniels AM, Deen M, Hoek HW, Ester WA. Age at autism spectrum disorder diagnosis: A systematic review and meta-analysis from 2012 to 2019. Autism. 2021;25(4):862–73.
Brooks JD, Arneja J, Fu L, Saxena FE, Tu K, Pinzaru VB, Anagnostou E, Nylen K, Saunders NR, Lu H, McLaughlin J, Bronskill SE. Assessing the validity of administrative health data for the identification of children and youth with autism spectrum disorder in Ontario. Autism Res. 2021;14(5):1037–45.
Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying patients with physician diagnosed asthma in health administrative databases. Can Respir J. 2009;16:183–8.
Prodhan S, King MJ, De P, et al. Health services data: the Ontario Cancer Registry (a unique, linked, and automated population-based registry). In: Levy A, Goring S, editors., et al., Data and measures in health services research. Health Services Research; 2016.
Greenberg ML, Barr RD, DiMonte B, McLaughlin E, Greenberg C. Childhood cancer registries in Ontario, Canada: lessons learned from a comparison of two registries. Int J Cancer. 2003;105(1):88–91.
Hux JE, Ivis F, Flintoft V, et al. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25:512–6.
Hauck TS, Lau C, Wing LLF, Kurdyak P, Tu K. ADHD treatment in primary care: demographic factors, medication trends, and treatment predictors. Can J Psychiat. 2017;62(6):393–402.
Mental Health and Addictions Program Framework Research Team. Mental Health and Addictions System Performance in Ontario: 2021 Scorecard. Technical Appendix. Toronto, ON: ICES; 2021.
Wodchis W, Bushmeneva K, Nikitovic M, et al. Guidelines on person-level costing using administrative databases in Ontario. Working Paper Series Vol. 1. Toronto: Health System Performance Research Network; 2013.
Wijeysundera HC, Wang X, Tomlinson G, Ko DT, Krahn MD. Techniques for estimating health care costs with censored data: an overview for the health services researcher. Clinicoecon Outcomes Res. 2012;4:145–55.
Bang H, Tsiatis AA. Estimating medical costs with censored data. Biometrika. 2000;87:329–43.
Zhao H, Tian L. On estimating medical cost and incremental cost-effectiveness ratios with censored data. Biometrics. 2001;57:1002–8.
Guidelines for the economic evaluation of health technologies. Canada. 4th ed. Ottawa: CADTH; 2017.
Carbone PS, Farley M, Davis T. Primary care for children with autism. Am Fam Physician. 2010;81(4):453–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding/support
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministries of Health and Ministry of Long-term Care. The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The opinions, results and conclusions reported in this article are also independent from the other sources that provided data and funding. No endorsement by ICES, the Ontario Ministries of Health and Ministry of Long-term Care is intended or should be inferred. Furthermore, parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed in the material are those of the authors and not necessarily those of CIHI. In addition, parts of this material are based on data and information provided by Ontario Health (Cancer Care Ontario) (OH [CCO]). The opinions, results, views and conclusions reported in this paper are those of the authors and do not necessarily reflect those of OH (CCO). No endorsement by OH (CCO) is intended or should be inferred.
Conflict of Interest
All authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethics Approval
Not applicable.
Data Availability Statement
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (e.g., healthcare organisations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Author Contributions
Concept and design: de Oliveira. Acquisition of data: de Oliveira, Tanner. Analysis and interpretation of data: de Oliveira, Tanner. Drafting of the manuscript: de Oliveira. Critical revision of the paper for important intellectual content: de Oliveira, Tanner. Obtaining funding: Not applicable. Administrative, technical, or logistic support: de Oliveira, Tanner. Supervision: de Oliveira.
Consent to participate
Not applicable.
Consent for publication (from patients/participants)
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
de Oliveira, C., Tanner, B. Estimating Cumulative Health Care Costs of Childhood and Adolescence Autism Spectrum Disorder in Ontario, Canada: A Population-Based Incident Cohort Study. PharmacoEconomics Open 7, 987–995 (2023). https://doi.org/10.1007/s41669-023-00441-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41669-023-00441-y