Abstract
Purpose
In this study, we evaluated the impact of risk factors for gestational diabetes on clinical/biochemical parameters and maternal/fetal outcomes.
Methods
One hundred eighty-three (n 183) women (age 33.8 ± 5.5 years, 59% Caucasians, 41% non-Caucasians) with gestational diabetes were included in the study. Anamnestic information, anthropometric and laboratory parameters, and maternal and fetal outcomes at delivery were collected.
Results
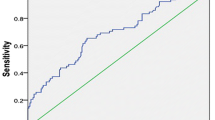
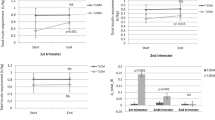
Insulin therapy prevalence was higher in Asians vs Caucasians (p = 0.006), despite lower pre-pregnancy BMI in Asians (p = 0.0001) and in pre-pregnancy overweight vs normal weight patients (p = 0.04). Insulin-treated patients had higher fasting OGTT glucose than patients on diet therapy (p = 0.003). In multivariate analysis, Asian ethnicity, age ≥ 35 years and pre-pregnancy BMI ≥ 25 kg/m2 were independent predictors of insulin therapy. Cesarean section occurred more in women aged ≥ 35 years than < 35 years (p = 0.02). Duration of pregnancy and age showed inverse correlation (r − 0.3 p = 0.013). Week of delivery was lower in patients ≥ 35 years vs patients < 35 years (p = 0.013). Fasting OGTT glucose was higher in overweight than in normal weight patients (p = 0.016). 1-h OGTT glucose was lower in obese vs normal weight (p = 0.03) and overweight patients (p = 0.03). Prevalence of prior gestational diabetes was higher in overweight/obese women (p = 0.002).
Conclusions
Ethnicity, age, and BMI have the heaviest impact on pregnancy outcomes.
Similar content being viewed by others
References
American Diabetes Association (2017) Standards of medical care in diabetes—2017. Diabetes Care 40(Suppl 1):S1–S2. https://doi.org/10.2337/dc17-S001
Yuen L, Wong VW (2015) Gestational diabetes mellitus: challenges for different ethnic groups. World J Diabetes 6(8):1024–1032. https://doi.org/10.4239/wjd.v6.i8.1024
Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, Kourtis AP et al (2010) Diabetes trends among delivery hospitalizations in the US, 1994–2004. Diabetes Care 33(4):768–773. https://doi.org/10.2337/dc09-1801
Chiefari E, Arcidiacono B, Foti D, Brunetti A (2017) Gestational diabetes mellitus: an updated overview. J Endocrinol Invest. https://doi.org/10.1007/s40618-016-0607-5 (Epub ahead of print)
American Diabetes Association (2004) Gestational diabetes mellitus. Diabetes Care 27(Suppl 1):S88–S90
Coustan DR, Lowe LP, Metzger BE, Dyer AR, International Association of Diabetes and Pregnancy Study Groups (2010) The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: paving the way for new diagnostic criteria for gestational diabetes mellitus. Am J Obstet Gynecol 202(6):654.e1-6. https://doi.org/10.1016/j.ajog.2010.04.006
Pu J, Zhao B, Wang EJ, Nimbal V, Osmundson S, Kunz L et al (2015) Racial/ethnic differences in gestational diabetes prevalence and contribution of common risk factors. Paediatr Perinat Epidemiol 29(5):436–443. https://doi.org/10.1111/ppe.12209
Triunfo S, Lanzone A, Lindqvist PG (2017) Low maternal circulating levels of vitamin D as potential determinant in the development of gestational diabetes mellitus. J Endocrinol Invest 40(10):1049–1059
Cozzolino M, Serena C, Maggio L, Rambaldi MP, Simeone S, Mello G et al (2017) Analysis of the main risk factors for gestational diabetes diagnosed with International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria in multiple pregnancies. J Endocrinol Invest 40(9):937–943
Alptekin H, Çizmecioğlu A, Işık H, Cengiz T, Yildiz M, Iyisoy MS (2016) Predicting gestational diabetes mellitus during the first trimester using anthropometric measurements and HOMA-IR. J Endocrinol Invest 39:577–583
Hedderson M, Ehrlich S, Sridhar S, Darbinian J, Moore S, Ferrara A (2012) Racial/ethnic disparities in the prevalence of gestational diabetes mellitus by BMI. Diabetes Care 35(7):1492–1498. https://doi.org/10.2337/dc11-2267
Kjos SL, Buchanan TA (1999) Gestational diabetes mellitus. N Engl J Med 341:1749–1756. https://doi.org/10.1056/NEJM199912023412307
American Diabetes Association (2002) Position Statement. Screening for Diabetes. Diabetes Care 25(supplement 1):S21–S24
Vandorsten JP, Dodson WC, Espeland MA, Grobman WA, Guise JM, Mercer BM et al (2013) NIH consensus development conference: diagnosing gestational diabetes mellitus. NIH Consens State Sci Statements 29(1):1–31
International Association of Diabetes and Pregnancy Study Groups Consensus Panel (2010) International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33:676–682. https://doi.org/10.2337/dc09-1848
Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, HAPO Study Cooperative Research Group et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358:1991–2002. https://doi.org/10.1056/NEJMoa0707943
Sistema nazionale per le linee guida dell’Istituto Superiore di Sanità (2010) Linea guida Gravidanza fisiologica. http://www.snlg-iss.it/cms/files/LG_Gravidanza.pdf. Accessed Nov 2010
AMD SID (2016) Standard italiani per la cura del diabete mellito 2016 http://www.standarditaliani.it/skin/www.standarditaliani.it/pdf/STANDARD_2016_June20.pdf. Accessed 20 June 2016
**ang AH, Li BH, Black MH, Sacks DA, Buchanan TA, Jacobsen SJ et al (2011) Racial and ethnic disparities in diabetes risk after gestational diabetes mellitus. Diabetologia 54(12):3016–3021. https://doi.org/10.1007/s00125-011-2330-2
Pertot T, Molyneaux L, Tan K, Ross GP, Yue DK, Wong J (2011) Can common clinical parameters be used to identify patients who will need insulin treatment in gestational diabetes mellitus? Diabetes Care 34:2214–2216
Wong V, Jalaludin B (2011) Gestational diabetes mellitus: who requires insulin therapy? Aust N Z J Obstet Gynaecol 51:432–436
Akinci B, Celtik A, Yener S, Yesil S (2008) Is fasting glucose during oral glucose tolerance test an indicator of the insulin need in gestational diabetes? Diabetes Res Clin Pract 82:219–225
McFarland MB, Langer O, Conway DL, Berkus MD (1999) Dietary therapy for gestational diabetes: how long is long enough? Obstet Gynecol 93:978–982
Mitra S, Nayak PK, Sahoo J, Mathew A, Padma A, Kamalanathan S et al (2014) Predictors of antenatal insulin requirement in gestational diabetes. Gynecol Endocrinol 30:565–568
Bakiner O, Ozsahin BK, Sariturk C, Ertorer E (2013) Risk factors that can predict antenatal insulin need in gestational diabetes. J Clin Med Res 5:381–388
Barnes RA, Wong T, Ross GP, Jalaludin BB, Wong VW, Smart CE et al (2016) A novel validated model for the prediction of insulin therapy initiation and adverse perinatal outcomes in women with gestational diabetes mellitus. Diabetologia 59:2331–2338
Zhang Y, Shao J, Li F, Xu X (2016) Factors in gestational diabetes mellitus predicting the needs for insulin therapy. Int J Endocrinol 2016:4858976
Watanabe M, Katayama A, Kagawa H, Ogawa D, Wada J (2016) Risk factors for the requirement of antenatal insulin treatment in gestational diabetes mellitus. J Diabetes Res 2016:9648798 (Epub 2016 Nov 23)
Schwartz N, Nachum Z, Green MS (2016) Risk factors of gestational diabetes mellitus recurrence: a meta-analysis. Endocrine 53:662–671
Langer O, Yogev Y, Most O, Xenakis EM (2005) Gestational diabetes: the consequences of not treating. Am J Obstet Gynecol 192(4):989–997
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163
Hsu WC, Araneta MR, Kanaya AM, Chiang JL, Fujimoto W (2015) BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care 38:150–158
Bayrampour H, Heaman M (2010) Advanced maternal age and the risk of cesarean birth: a systematic review. Birth 37(3):219–226
Jolly M, Sebire N, Harris J, Robinson S, Regan L (2000) The risks associated with pregnancy in women aged 35 years or older. Hum Reprod 15:2433–2437
Bell JS, Campbell DM, Graham WJ, Penney GC, Ryan M, Hall MH (2001) Can obstetric complications explain the high levels of obstetric interventions and maternity service use among older women? A retrospective analysis of routinely collected data. BJOG 108(9):910–918
O’Leary CM, de Klerk N, Keogh J, Pennell C, de Groot J, York L et al (2007) Trends in mode of delivery during 1984–2003: can they be explained by pregnancy and delivery complications? BJOG 114(7):855–864 (Epub 2007 May 15)
Gorgal R, Gonçalves E, Barros M, Namora G, Magalhães A, Rodrigues T et al (2012) Gestational diabetes mellitus: a risk factor for non-elective cesarean section. J Obstet Gynaecol Res 38(1):154–159
Diet A, Cupisti S, Beckmann MW, Schwab M, Zollner U (2015) Pregnancy and obstetrical outcomes in women over 40 years of age. Geburtshilfe Frauenheilkd 75(8):827–832
Benli AR, Cetin Benli N, Usta AT, Atakul T, Koroglu M (2015) Effect of maternal age on pregnancy outcome and cesarean delivery rate. J Clin Med Res 7(2):97–102
Berkowitz GS, Skovron ML, Lapinski RH, Berkowitz RL (1990) Delayed childbearing and the outcome of pregnancy. N Engl J Med 322:659–664
Major CA, deVeciana M, Weeks J, Morgan MA (1998) Recurrence of gestational diabetes: who is at risk? Am J Obstet Gynecol 179(4):1038–1042
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Filardi, T., Tavaglione, F., Di Stasio, M. et al. Impact of risk factors for gestational diabetes (GDM) on pregnancy outcomes in women with GDM. J Endocrinol Invest 41, 671–676 (2018). https://doi.org/10.1007/s40618-017-0791-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0791-y