Abstract
Introduction
Despite high prevalence of hypertension, few studies have analysed the adverse effects (AEs) of antihypertensive medications, especially in older patients.
Aim
To investigate the prevalence and associated factors of antihypertensive-related AEs, focusing on the influence of age on treatment tolerability.
Methods
We retrospectively investigated antihypertensive-related AEs in patients evaluated at the Hypertension Clinic of Careggi Hospital, Florence, Italy, between January 2017 and July 2020. Multivariable regression models were generated to analyse variables associated with AEs in the overall sample and in participants ≥75 years.
Results
Among 622 subjects (mean age 64.8 years, 51.4% female), the most frequently reported AEs were calcium-channel blockers (CCB)-related ankle swelling (26.8%) and ACEi-induced cough (15.1%). Ankle swelling was more common in older patients (35.7% vs 22.3%, p = 0.001; odds ratio [OR] 1.94, 95%CI 1.289-2.912) and was independently associated with Body Mass Index (BMI, adjOR 1.073) and angiotensin-receptor antagonists (adjOR 1.864). The association with BMI was confirmed in older patients (adjOR 1.134). ACEi-induced cough showed similar prevalence in younger and older patients (13.9% vs 15.6%, p = 0.634), being independently associated with female sex (adjOR 2.118), gastroesophageal reflux disease (GERD, adjOR 2.488) and SNRI therapy (adjOR 8.114). The association with GERD was confirmed in older patients (adjOR 3.238).
Conclusions
CCB-related ankle swelling and ACEi-induced cough represent the most common antihypertensive-related AEs, also at old age. Older patients showed a two-fold increased risk of ankle swelling, that was also independently associated with BMI. ACEi-induced cough had similar prevalence at younger and old ages, being independently associated with GERD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hypertension represents one of the leading modifiable risk factors for cardiovascular morbidity and mortality, affecting more than 1.28 billion adults worldwide with increasing prevalence in advancing age [1]. Recent literature has provided clear evidence on the beneficial effects of blood pressure (BP) reduction, also in older adults [2, 3]. Yet, at old age, comorbidities, polypharmacy and age-related changes in pharmacokinetics and pharmacodynamics may contribute to increase the risk of drug-related adverse effects (AEs), i.e., any noxious, undesired, or unintended response to a therapeutic agent, which occur at therapeutic doses [4].
It is estimated that drug-related AEs occur in approximately 20–85% of patients receiving anti-hypertensive medications, with distinct and specific tolerability profiles for different drug classes [5,6,7]. AEs associated with antihypertensive medications may negatively impact patient’s compliance [8], leading to poor BP control and increased cardiovascular risk [9].
The HYVET trial reported a 40% prevalence of drug-related AEs among subjects aged 80 or older receiving antihypertensive therapy [10]. Despite the known predisposition of older patients to drug-related AEs, the influence of age on tolerability of antihypertensive medications has been poorly investigated to date, except for the well-known risk of hypotension, electrolyte imbalances and renal function worsening [11, 12]. Therefore, although treatment tolerability can significantly influence patients’ compliance and therapeutic management, the risk and predisposing factors for antihypertensive-related AEs in older adults remain currently unclear [13].
The present study analysed the prevalence and associated factors of antihypertensive-related AEs in a sample of hypertensive outpatients, with the final purpose to investigate the influence of age on antihypertensive treatment tolerability.
2 Methods
We conducted a retrospective cross-sectional analysis of data from all treated hypertensive patients evaluated at the Hypertension Clinic of Careggi University Hospital, Florence, Italy, between January 2017 and July 2020. The Hypertension Clinic of Careggi University Hospital evaluates hypertensive adults of all ages from Florence and its surroundings, offering specialized geriatric care for older hypertensive patients. Tolerability of antihypertensive medications and past history of treatment-related AEs are routinely investigated during the visit and any current/previous AE is recorded in medical charts. For the purpose of the present study, a medical chart review was carried out to collect data on medical history, comorbidities and BP values. Detailed information on medical therapy was recorded, focusing on antihypertensive drug classes (ACE–inhibitors [ACEi], angiotensin receptor blockers [ARBs], calcium channel blockers [CCBs], beta-blockers, diuretics [loop diuretics, thiazide diuretics, mineralcorticoid receptor antagonists], doxazosin and other alpha receptor blockers). Moreover, tolerability of antihypertensive medications was assessed by recording any current/previous AE spontaneously reported by the patient or detected by the physician during routine visits. Antihypertensive-related AEs were defined as any adverse effect resulting in treatment discontinuation or dose reduction. The prevalence of AEs was assessed based on the total number of patients who were receiving or had previously received a specific drug class, i.e., the total number of patients with ongoing treatment and of those with previous treatment discontinuation because of AE (prior treatment).
2.1 Statistical Analysis
Continuous variables were expressed as means and standard deviations (SD) or as medians and interquartile ranges (IQRs, 25th–75th percentiles), according to what was most appropriate based on variables distribution. Categorical variables were expressed as absolute frequencies with percentages.
To investigate the influence of age on treatment tolerability, the prevalence of antihypertensive-related AEs was analysed in two age-stratified subgroups (< 75 and ≥ 75 years). Moreover, for the most frequently reported AEs, bivariate analyses were performed to compare patients with and without each adverse effect, in the overall sample and in the subgroup ≥ 75 years. The Pearson chi-square test was used for comparison of categorical variables between groups, while the T-test for independent samples (parametrical) or the Mann-Whitney test (non-parametrical) were used as appropriate for comparison of continuous variables. Multivariable binary logistic regression models were generated with backward stepwise selection approach to identify factors independently associated with each adverse effect. Logistic regression models were adjusted for demographics and other clinical variables of interest including those showing an association with the outcome in univariate analysis. To avoid multicollinearity, inter-correlations among the tested variables were verified by using a correlation matrix of the Spearman’s Rho correlation coefficients on two sides; variables with a correlation coefficient equal or superior to 0.50 were excluded from the model. Results of logistic regression were expressed as odds ratios (OR) and 95% confidence intervals (CI). Statistical significance was set at p < 0.05. Statistical analysis was performed using SPSS Statistics software version 26 (SPSS Inc. IBM, Chicago, IL).
3 Results
The study sample included 622 patients (mean age 64.8 ± 14.8 years, 51.4% female). Their characteristics are detailed in Table 1. The study participants were receiving a median number of 2 antihypertensive medications, with renin-angiotensin system inhibitors (79.4%) and CCBs (57.2%) being the most commonly prescribed drug classes.
Table 2 describes antihypertensive-related AEs observed in our study sample. CCB-related ankle swelling (26.8% of patients receiving prior/ongoing CCBs treatment) and ACEi-induced cough (15.1% of patients receiving prior/ongoing ACEi treatment) were the most frequently reported, while other AEs were rare.
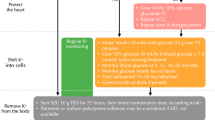
CCBs-related ankle swelling was significantly more common in older than in younger patients (35.7% vs 22.3%, p = 0.001), with an OR of 1.94 (95% CI 1.289–2.912, p = 0.002). Prevalence of ACEi-induced cough was similar in the two age groups (13.9% vs 15.6%, p = 0.634) (Fig. 1).
3.1 ACEi-induced cough
Patients suffering from ACEi-induced cough were more frequently female (65.7% vs 45.5%, p = 0.002) and showed a higher prevalence of gastroesophageal reflux disease (20.9% vs 9.5%, p = 0.007). Moreover, they were more commonly receiving benzodiazepines (19.4% vs 10.1%, p = 0.027) and SNRI antidepressants (6% vs 0.8%, p = 0.002) (Supplementary table 1).
In a multivariable logistic regression model adjusted for benzodiazepine therapy, COPD and current smoking, ACEi-induced cough remained significantly associated with female sex (OR 2.118, 95% CI 1.218–3.683, p = 0.008), gastroesophageal reflux disease (GERD) (OR 2.488, 95% CI 1.241–4.987, p = 0.01) and SNRI therapy (OR 8.114, 95% CI 1.723–38.202, p = 0.008). Age was not associated with ACEi-induced cough.
In the subgroup of older patients, univariate analysis provided similar results, showing the association of ACEi-induced cough with GERD, benzodiazepines and SNRI antidepressants (Table 3). GERD was the only variable independently associated with ACEi-induced cough in older patients (OR 3.238, 95% CI 1.046–10.022, p = 0.042).
3.2 CCBs-Related Ankle Swelling
Patients reporting CCB-related ankle swelling were older (mean age 69.2 vs 64.9 years, p = 0.003) and showed higher mean Body Mass Index (BMI) values (29.1 vs 27.5 kg/m2, p = 0.004). Moreover, these patients were more likely to receive ARBs (47.4% vs 32.8%, p = 0.003), thiazide diuretics (40.6% vs 30%, p = 0.026) and doxazosin (18% vs 10.5%, p = 0.024). By contrast, ACEi therapy was less common among patients with CCB-related ankle swelling (38.3% vs 49.9%, p = 0.023) (Supplementary Table 2). The association between CCB-related ankle swelling and ARBs was also confirmed in a multivariable logistic regression model adjusted for demographics, doxazosin and diuretic therapy, heart failure and venous insufficiency (OR for ARBs 1.864, 95% CI 1.127–3.082, p = 0.015). Additional variables independently associated with ankle swelling included age (OR 1.020, 95% CI 1.002–1.038, p = 0.030) and BMI (OR 1.073, 95% CI 1.016–1.133, p = 0.012), but not ACEi (OR 0.411, 95% CI 0.155–1.094, p = 0.075) (Supplementary Table 3).
In the older patient subgroup, the association of CCB-related ankle swelling with BMI values and ARBs was marginally significant at univariate analysis (Table 3). At multivariable logistic regression analysis, the occurrence of ankle swelling was independently associated with BMI values (OR 1.134, 95% CI 1.017–1.264, p = 0.023) and inversely associated with loop diuretics (OR 0.206, 95% CI 0.048–0.879, p = 0.033). Similar results were reported when adjusting for ACEi, while ARBs were not retained in the multivariable model (Supplementary Table 3).
4 Discussion
AEs associated with antihypertensive medications represent a common concern for both patients and physicians and might negatively impact treatment compliance and effectiveness. The occurrence and unfavourable consequences of antihypertensive-related AEs might be magnified in older patients, who typically present an increased risk of both cardiovascular events and drug-related AEs [14, 15]. Although some previous studies have investigated antihypertensive-related AEs, data referring to older hypertensive patients remain scarce.
The present study analysed antihypertensive treatment tolerability in a sample of 622 hypertensive outpatients evaluated at a specialised hypertension clinic. The most frequently reported AEs were CCB-related ankle swelling and ACEi-induced cough, also in older patients. Patients aged ≥75 years showed a two-fold increased risk of CCB-related ankle swelling, with approximately one third of patients in this subgroup reporting consequent CCB discontinuation or dose reduction. By contrast, prevalence of ACEi-induced cough was not influenced by age. Other antihypertensive-related AEs were rare both in younger and in older patients.
ACEi-induced cough occurred in the 15.1% of patients receiving ACEi, consistently with previous literature reports [16, 17]. However, available data on ACEi-induced cough are highly variable and inconsistent, due to different characteristics of the study samples and different methods of assessment of AEs. Indeed, some studies reported significantly higher incidence rates [18, 19], while others described a much lower incidence, particularly among patients presenting with chronic cough. Moreover, some data indicate that, in a minority of patients, cough may not recur if ACEi therapy is reintroduced [20,21,22]. It follows that cough reported during ACEi treatment may not always be attributable to the drug, and other causes of the symptom should be considered. In our study sample, ACEi-induced cough was found to be associated with GERD independently of other conditions potentially predisposing to cough, such as chronic obstructive pulmonary disease and smoking. This result supports the hypothesis that cough reported during ACEi treatment may be promoted or caused by different clinical conditions, such as GERD. Prospective studies are needed to confirm this hypothesis.
ACEi-induced cough was more common in female patients, confirming previous literature results [23]. We also observed an association between ACEi-induced cough and SNRI antidepressants. To our knowledge, no similar data are available in the literature. A possible explanation involves the mechanism of action of SNRIs, which induce an increase in blood levels of norepinephrine and serotonin. Increased serotonin levels have been described in patients with asthma [24] and a pathogenetic role of serotonin in asthma exacerbations has been hypothesized, although the underlying mechanism remains unknown. We could thus speculate that the increase in serotonin levels induced by SNRIs could favour the occurrence of cough in patients receiving ACEi. However, given the limited number of patients treated with SNRIs in our sample, this association should be further investigated in larger studies.
A randomised controlled trial involving 27,492 hypertensive patients showed an increased risk of ACEi-induced cough in individuals aged 65 or older as compared to younger subjects [25]. The present study did not identify an association between ACEi-induced cough and age, consistently with other literature data [26]. Moreover, the independent association between cough and GERD was confirmed in the older subgroup, implying that ACEi therapy might be only partially causative of this symptom also at old age.
CCB-related ankle swelling was the most common AEs in our sample, being reported by one in four patients receiving CCBs (26.8%). Lower rates have been described in previous studies, ranging from 1 to 15% [27, 28]. Again, this difference might be related to different assessment methods and different clinical characteristics of the studied populations. Our study focused on older hypertensive patients, showing a significantly higher probability of ankle swelling in subjects ≥75 years (35.7% vs 22.2%). Indeed, age was significantly associated with the occurrence of CCB-related ankle swelling, independently of other predisposing conditions and therapies, such as heart failure, venous insufficiency and vasodilators. This finding agrees with previous literature results [29] and might be explained by ageing phenomena of vascular endothelium that promote vascular hyperpermeability [30] and fluid accumulation in interstitial spaces [31]. Moreover, in older patients, concomitant conditions may be present, such as low protein levels, venous insufficiency and heart disease, which further contribute to swelling.
Our results also indicate an independent association between BMI and CCB-related ankle swelling, which was confirmed in the older subgroup. It can be hypothesised that subjects with higher BMI have an increased abdominal pressure which might hamper venous return, predisposing to peripheral swelling. Indeed, an association between BMI and body swelling has been previously described in hypertensive patients [32], although not in reference to CCBs therapy.
It is known that inhibitors of the renin-angiotensin-aldosterone system may reduce the incidence of CCB-related ankle swelling [33, 34], probably due to a reduction of intracapillary hydrostatic pressure [29]. In our study, however, CCB-related swelling was found to be directly and independently associated with ARBs. By contrast, an inverse association was observed between ankle swelling and ACEi, although not confirmed in multivariable analysis. A possible explanation for this result is provided by the different pharmacokinetics of these drug classes. Indeed, ACEi act through a reduction of angiotensin II levels, while ARBs act as antagonists of angiotensin type 1 receptors, thus allowing for and favouring the stimulation of type 2 receptors, which mediate vasodilation and, possibly, vasodilatory oedema [35].
The association between ankle swelling and diuretics was conflicting in our study, showing a direct association with thiazide diuretics in the overall sample and an inverse association with loop diuretics in the older subgroup. The cross-sectional design of our research did not allow to further explore this association. However, it is likely that patients reporting CCB-related swelling had received thiazide diuretics as alternative therapy to achieve blood pressure control. By contrast, a concomitant therapy with loop diuretics might have reduced the risk of swelling in older patients, although a prescriptive cascade (i.e., prescription of loop diuretics to avoid/treat swelling) cannot be excluded.
Other antihypertensive-related AEs were rare in the present study. CCB-induced headache was reported by the 1.8% of the overall sample and by the 0.6% of subjects ≥ 75 years, less frequently than observed in previous studies [17, 36]. Similarly, the occurrence of CCB-related palpitations was uncommon, consistently with a previous meta-analysis [37]. Notably, CCB-related palpitations were not described in any patients of the older subgroup, suggesting an age-related reduction of this AE. Indeed, CCB-related palpitations likely derive from a compensatory heart rate increase induced by vasodilation. It might thus be supposed that this response less commonly occurs at old age, due to a less efficient autonomic nervous system function and blunted chronotropic responses. Constipation related to CCB was observed in the 0.8% of the study population and in the 1.8% of the older subgroup. However, as constipation is common at old age, it cannot be excluded that this drug-related AE might have been underestimated. Gynecomastia was reported by the 3.9% of patients receiving mineralcorticoid receptor antagonists, a lower prevalence than previously described [38]. Gynecomastia was observed only in patients ≥ 75 years, probably due to the reduction of testosterone levels occurring at old age [39, 40].
4.1 Limitations
Our results must be interpreted in the context of some study limitations. First, the cross-sectional design of the study did not allow for drawing conclusions on causal factors of AEs. Second, AEs were assessed based on medical records and patient reports, so an underreport of events cannot be excluded. Moreover, detailed information on treatment adherence was not available, so patients with low adherence could not be excluded from the analysis. As rates of low adherence are known to be considerable among hypertensive patients, we cannot exclude that this might have influenced our estimate of AEs prevalence. Finally, the retrospective analysis approach limited the investigation of some common antihypertensive-related AEs, such as electrolyte disorders, hypotensive events, renal worsening, metabolic effects.
5 Conclusions
CCB-related ankle swelling and ACEi-induced cough represent the most common AEs of antihypertensive therapy, also at old age. Older patients showed a two-fold increased risk of CCB-related ankle swelling, that was also independently associated with BMI values. ACEi-induced cough had similar prevalence at young and old ages, being independently associated with gastro-oesophageal reflux disease.
Data Availability
All datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from. to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 1990;2021(398):957–80.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, Yang J, Jiang Y, Xu X, Wang TD, Chen Y, Li Y, Yao L, Li D, Wang L, Shen X, Yin X, Liu W, Zhou X, Zhu B, Guo Z, Liu H, Chen X, Feng Y, Tian G, Gao X, Kario K, Cai J. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–79.
Deng Y, Bai J, Yang X, Liu W, Guo Z, Zhang J, Huang R, Yang X, Yu C, Yu J, Guo X, Wu H, Liu P, Zhang W, Cai J, et al. Achieved systolic blood pressure and cardiovascular outcomes in 60–80-year-old patients: the Strategy of Blood Pressure Intervention in the Elderly Hypertensive Patients (STEP) trial. Eur J Prev Cardiol. 2023;30:1017–27.
WHO. International drug monitoring: the role of national centres, report of a WHO meeting [Geneva, September 20-25 1971]. 1972. https://iris.who.int/handle/10665/40968. Accessed 30 Dec 2023
Tedla YG, Bautista LE. Drug side effect symptoms and adherence to antihypertensive medication. am J Hypertens. 2016;29:772–9.
Rivasi G, Rafanelli M, Mossello E, Brignole M, Ungar A. Drug-related orthostatic hypotension: beyond anti-hypertensive medications. Drugs Aging. 2020;2020(37):725–38.
Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. 2019;124:1045–60.
Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: A review of systematic reviews. Front Pharmacol. 2013;4:91.
Burnier M. Drug adherence in hypertension. Pharmacol Res. 2017;125(Pt B):142–149. https://doi.org/10.1016/j.phrs.2017.08.015.
Butt TF, Branch RL, Beesley L, Martin U. Managing hypertension in the very elderly: effect of adverse drug reactions (ADRs) on achieving targets. J Hum Hypertens. 2010;24:514–8.
Rivasi G, Ceolin L, Capacci M, Matteucci G, Testa GD, Ungar A. Risks associated with intensive blood pressure control in older patients. Kardiol Pol. 2023;81:446–54.
Sheppard JP, Koshiaris C, Stevens R, Lay-Flurrie S, Banerjee A, Bellows BK, Clegg A, Hobbs FDR, Payne RA, Swain S, Usher-Smith JA, McManus RJ. The association between antihypertensive treatment and serious adverse events by age and frailty: a cohort study. PLoS Med. 2023. https://doi.org/10.1371/journal.pmed.1004223.
Alhawassi TM, Krass I, Pont LG. Antihypertensive-related adverse drug reactions among older hospitalized adults. Int J Clin Pharm. 2018;40:428–35.
Sharabi Y, Illan R, Kamari Y, Cohen H, Nadler M, Messerli FH, Grossman E. Diuretic induced hyponatraemia in elderly hypertensive women. J Hum Hypertens. 2002;16:631–5.
Dharmarajan TS, Dharmarajan L. Tolerability of antihypertensive medications in older adults. Drugs Aging. 2015;32:773–96.
Bangalore S, Kumar S, Messerli FH. Angiotensin-converting enzyme inhibitor associated cough: deceptive information from the physicians’ desk reference. Am J Med. 2010;123:1016–30.
Vukadinović D, Vukadinović AN, Lavall D, Laufs U, Wagenpfeil S, Böhm M. Rate of cough during treatment with angiotensin-converting enzyme inhibitors: a meta-analysis of randomized placebo-controlled trials. Clin Pharmacol Ther. 2019;105:652–60.
Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy. Ann Intern Med. 1992;117:234–42.
Gregg LP, Richardson PA, Herrera MA, Akeroyd JM, Jafry SA, Gobbel GT, Wydermyer S, Arney J, Hung A, Matheny ME, Virani SS, Navaneethan SD. Documented adverse drug reactions and discontinuation of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in chronic kidney disease. Am J Nephrol. 2023;54:126–35.
Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough. Chest. 2006;129:169S-173S.
Wyskida K, Jura-Szołtys E, Smertka M, Owczarek A, Chudek J. Factors that favor the occurrence of cough in patients treated with ramipril–a pharmacoepidemiological study. Med Sci Monit. 2012;18:Pl21–8.
Borghi C, Veronesi M. Cough and ACE inhibitors: the truth beyond placebo. Clin Pharmacol Ther. 2019;105:550–2.
Cimolai N. Risk factors for angiotension-converting enzyme inhibitor-associated cough. J Clin Pharmacol. 2021;61:1251–2.
Cazzola I, Matera MG. 5-HT modifiers as a potential treatment of asthma. Trends Pharmacol Sci. 2000;21:13–6.
Brugts JJ, Arima H, Remme W, Bertrand M, Ferrari R, Fox K, DiNicolantonio J, MacMahon S, Chalmers J, Zijlstra F, Caliskan K, Simoons ML, Mourad JJ, Boersma E, Akkerhuis KM. The incidence and clinical predictors of ACE-inhibitor induced dry cough by perindopril in 27,492 patients with vascular disease. Int J Cardiol. 2014;176:718–23.
Yeşil S, Yeşil M, Bayata S, Postaci N. ACE inhibitors and cough. Angiology. 1994;45:805–8.
Sica DA. Pharmacotherapy review: calcium channel blockers. J Clin Hypertens (Greenwich). 2006;8:53–6.
Liang L, Kung JY, Mitchelmore B, Cave A, Banh HL. Comparative peripheral edema for dihydropyridines calcium channel blockers treatment: A systematic review and network meta-analysis. J Clin Hypertens (Greenwich). 2022;24:536–54.
Fogari R, Zoppi A, Derosa G, Mugellini A, Lazzari P, Rinaldi A, Fogari E, Preti P. Effect of valsartan addition to amlodipine on ankle oedema and subcutaneous tissue pressure in hypertensive patients. J Hum Hypertens. 2007;21:220–4.
Oakley R, Tharakan B. Vascular hyperpermeability and aging. Aging Dis. 2014;5:114–25.
Fogari R, Malamani GD, Zoppi A, Preti P, Vanasia A, Fogari E, Mugellini A. Comparative effect of lercanidipine and nifedipine gastrointestinal therapeutic system on ankle volume and subcutaneous interstitial pressure in hypertensive patients: a double-blind, randomized, parallel-group study. Curr Ther Res. 2000;61:850–62.
Paracha MY, Khalid F, Qamar MA, Ali SL, Singh S, Rubab U, Anwar A, Hashmi AA. Relationship between clinical features and body mass index among hypertensive patients: a cross-sectional study. Cureus. 2020;12: e11615. https://doi.org/10.7759/cureus.
Fogari R, Zoppi A. Effects of antihypertensive therapy on sexual activity in hypertensive men. Curr Hypertens Rep. 2002;4:202–10.
Messerli FH. Vasodilatory edema: a common side effect of antihypertensive therapy. Curr Cardiol Rep. 2002;4:479–82.
Savoia C, D’Agostino M, Lauri F, Volpe M. Angiotensin type 2 receptor in hypertensive cardiovascular disease. Curr Opin Nephrol Hypertens. 2011;20:125–32.
Makarounas-Kirchmann K, Glover-Koudounas S, Ferrari P. Results of a meta-analysis comparing the tolerability of lercanidipine and other dihydropyridine calcium channel blockers. Clin Ther. 2009;31:1652–63.
Borghi C. Lercanidipine in hypertension. Vasc Health Risk Manag. 2005;1:173–82.
Quach K, Lvtvyn L, Baigent C, Bueti J, Garg AX, Hawley C, Haynes R, Manns B, Perkovic V, Rabbat CG, Wald R, Walsh M. The safety and efficacy of mineralocorticoid receptor antagonists in patients who require dialysis: a systematic review and meta-analysis. Am J Kidney Dis. 2016;68:591–8.
Lamberts SW, van den Beld AW, van der Lely AJ. The endocrinology of aging. Science. 1997;278:419–24.
Rose LI, Underwood RH, Newmark SR, Kisch ES, Williams GH. Pathophysiology of spironolactone-induced gynecomastia. Ann Intern Med. 1977;87:398–403.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Giulia Rivasi, Antonio Coscarelli, Marco Capacci, Ludovica Ceolin, Giada Turrin, Virginia Tortù and Maria Flora D’Andria. The first draft of the manuscript was written by Giulia Rivasi, Antonio Coscarelli, Marco Capacci and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Data Availability Statement
All datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no conflict of interest.
Financial Interests
The authors declare they have no financial interests.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Local Research Ethics Committee (protocol reference number: 16627/OSS).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rivasi, G., Coscarelli, A., Capacci, M. et al. Tolerability of Antihypertensive Medications: The Influence of Age. High Blood Press Cardiovasc Prev 31, 261–269 (2024). https://doi.org/10.1007/s40292-024-00639-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-024-00639-z