Abstract
Background and Objective
Recently, studies have pointed to a link between coronavirus disease 2019 vaccinations and myocarditis. Myocarditis following an influenza vaccine has been sporadically reported. However, it is not known whether this adverse event occurs among elderly individuals who have received influenza vaccines. We used a population-based database and a self-controlled case-series design to estimate the incidence of myocarditis following an influenza vaccination.
Methods
Data were extracted from Taiwan’s National Health Insurance Research Database. The study population consisted of elderly people aged ≥ 65 years who had de novo myocarditis, which required hospitalization, within 6 months after receiving an influenza vaccination between 2003 and 2017. The first 1–7, 1–14, and 1–42 days after vaccination were defined as risk intervals, and the other periods were defined as control intervals. Poisson regression was used to calculate the incidence rate ratio for myocarditis between the risk and control periods.
Results
Within 180 days following a vaccination, 191 people were hospitalized for myocarditis among 19,678,904 people. In comparison with control intervals, the incidence rate ratios of an admission for myocarditis for days 1–7, 1–14, and 1–42 were 0.80 (95% confidence interval 0.36–1.81), 0.72 (95% confidence interval 0.39–1.32), and 0.73 (95% confidence interval 0.50–1.05), respectively. Subgroup analyses by sex, age, Charlson Comorbidity Index scores, and comorbidities did not yield significant differences in the incidence rate ratio.
Conclusions
Regardless of the post-vaccination time and underlying baseline characteristics, the incidence risk of myocarditis is not significantly increased in the elderly following an influenza vaccination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We used a population-based database and a self-controlled case-series design to estimate the incidence of myocarditis following an influenza vaccination. |
Regardless of the post-vaccination time and underlying baseline characteristics, the incidence risk of myocarditis is not significantly increased in the elderly following an influenza vaccination. |
1 Background
Myocarditis is an uncommon but potentially life-threatening disease. Clinical onset varies from subclinical to devastating disease [1]. Except for smallpox vaccines [2, 3], myocarditis was rarely considered to be caused by vaccines before the coronavirus disease 2019 (COVID-19) vaccination campaign [4]. Initially, with the BNT162b2 (Pfizer-BioNTech Comirnaty) mRNA vaccine, the estimated incidence of myocarditis was 2.13 cases per 100,000 persons; the highest incidence was among male patients between the ages of 16 and 29 years [4]. Now, the correlation of an increased risk of myocarditis following an mRNA-based COVID vaccination is well known especially in the young male population [4,5,6], but the precise cause remains a mystery. Despite its rarity, its high clinical impact and the social fear toward vaccinations should not be overlooked as these often cause great anxiety among the public.
However, vaccine-related myocarditis might not only happen following mRNA COVID vaccines. Next, there was a report of an excess of myocarditis cases following the first dose of the ChAdOx1 (AstraZeneca Vaxzevria) vaccine, an adenovirus-based COVID vaccine; and the excess was observed among both men and women of any age [5]. The observation is not the same as with mRNA-based vaccines, which occurs mainly in young male adults. These data pique our curiosity as to whether the risk of myocarditis occurs in other vaccine types, and whether it appears in a different age group, such as older individuals. The seasonal influenza vaccine has been routinely administered for immunization of the elderly in many countries. There had been no large-scale study of the relationship between myocarditis and the influenza vaccine except a few clinical case reports in which the onset of myocarditis was within days following a vaccination [7,8,9,10]. Notably, there is no laboratory examination that can directly confirm myocarditis is caused by a vaccination, therefore, the link could only be established through a temporal correlation. Here, we conducted a nationwide study that focused on a population aged ≥ 65 years and used the self-controlled case-series design to address the question of “Does the influenza vaccine increase the incidence of myocarditis?”.
2 Materials and Methods
2.1 Data Source
National Health Insurance (NHI) was launched in 1995 in Taiwan, and it is a single-payer, universal health coverage program that covers more than 99.9% of all citizens [11]. Through the NHI program, free influenza vaccinations have been offered to older individuals aged over 65 years since 2001 [12]. Data of this retrospective study were extracted from the NHI Research Database, released by the Health and Welfare Data Science Center, Ministry of Health and Welfare of Taiwan. The NHI Research Database contained the details of beneficiaries enrolled in the NHI program, including clinical records of outpatient visits, hospitalizations, diagnostic codes, and prescriptions [11]. The database is de-identified, and the Health and Welfare Data Science Center provides scrambled random identification numbers to protect the privacy of insured patients. Informed consent was waived. The Taichung Jen-Ai Hospital, Taiwan approved the study protocol after a complete ethical review (Institutional Review Board No. 108-83).
2.2 Study Design and Populations
The association between influenza vaccine and myocarditis was evaluated using a self-controlled case-series design [13]. The study population was elderly people aged ≥ 65 years who had de novo myocarditis within 6 months after an influenza vaccination between 2003 and 2017. On the basis of the admission record, we identified an incident of myocarditis based on the principal admission diagnostic code based on the International Classification of Diseases, Ninth Revision, Clinical Modification codes 422 and 429.0 and the International Classification of Diseases, Tenth Revision, Clinical Modification codes I40, I41, and I51.4, which have been validated in a previous study [14].
A total of 19,678,904 elderly people aged ≥ 65 years received the influenza vaccination from 2003 to 2017. After excluding (1) patients who received an influenza vaccination more than once in the same year, (2) patients who died within 6 months after receiving an influenza vaccination (not including the death caused by myocarditis), and (3) patients with missing values for any study variables, we included 191 patients who were hospitalized for myocarditis within 6 months after receiving an influenza vaccination. Control variables in this study included sex, age, Charlson Comorbidity Index (CCI) severity [15], and comorbidities. Age was categorized into the groups of 65–74, 75–84, and ≥ 85 years. The CCI scores were categorized as 0, 1, and ≥ 2. Comorbidities comprised cancer and autoimmune diseases, which were identified according to data in the registry for catastrophic illness under the NHI and were classified as yes or no.
2.3 Definition
The date of myocarditis onset was defined as the admission date with myocarditis coded during the study period. The follow-up period was 180 days from the date of vaccination. The first 7, 14, and 42 days after receiving an influenza vaccination were defined as risk intervals, and the other periods were defined as control intervals. Figure 1 presents a schematic algorithm of the study. If myocarditis was not related to the influenza vaccination, the incidence of myocarditis in the study patients would presumably be distributed equally during the entire observation period.
Schematic of study design. Myocarditis (A) represents the elderly who are hospitalized (or died) for myocarditis at any time during the 7-day, 14-day, and 42-day risk interval after an influenza vaccination. Another myocarditis (B) represents the elderly who are hospitalized (or died) for myocarditis during the control interval. The study assessed the relative incidence of myocarditis during the risk interval as compared with the control interval
2.4 Statistical Analyses
All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA). We performed Poisson regression to analyze the incidence rate ratio (IRR) and 95% confidence interval (CI) for incident myocarditis during the risk and control intervals. The model accounted for hospitalization episodes for myocarditis per study patient during the observation period. In addition, we evaluated the risk during days 1–7, 1–14, and 1–42 after receiving the influenza vaccination. Moreover, we performed a stratified analysis in subgroups according to sex, age (65–74, 75–84, and ≥ 85 years), CCI (score 0, 1, and ≥ 2), autoimmune disease, and cancer (with or without). A p-value of < 0.05 was considered to indicate a significant difference in this study.
3 Results
There were 191 eligible cases, among which 101 (52.88%) were male. The mean age was 76.34 ± 6.03 years, while the proportions of age 65–74, 75–84, and ≥ 85 years were 40.84%, 43.98%, and 15.18%, respectively. Among the comorbid conditions, 19 (9.95%) had cancer and four (2.09%) had autoimmune disease (Table 1).
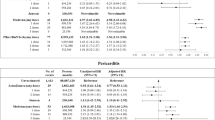
The IRRs of myocarditis after an influenza vaccination are listed in Table 2. The IRR for days 1–7 (risk interval) compared with days 8–180 (control interval) was 0.80 (95% CI 0.36–1.81); the IRR for days 1–14 (risk interval) compared with days 15–180 (control interval) was 0.72 (95% CI 0.39–1.32); and the IRR for days 1–42 (risk interval) compared with days 43–180 (control interval) was 0.73 (95% CI 0.50–1.05). After the influenza vaccination, the incidence of myocarditis did not increase significantly on days 1–7, 1–14, and 1–42.
A subgroup analysis was performed to explore the roles of sex, age, and underlying comorbidities (including CCI scores, cancer, and autoimmune diseases). The results are shown in Table 3. There was no significantly increased risk of myocarditis after an influenza vaccination, regardless of the post-vaccination time and the underlying characteristics.
4 Discussion
The possible risk of vaccines causing myocarditis has recently become an important issue. Although most cases of myocarditis related to the COVID vaccines are mild or moderate in severity, this information increases physicians’ awareness of this possible side effect. It also causes great panic and concern to the public as well as the government. Myocarditis has been reported in different types of COVID vaccines other than BNT162b2, including mRNA-based (mRNA-1273 [Moderna Spikevax]), adenovirus-based (ChAdOx1 [AstraZeneca Vaxzevria]), and subunit-based (NVX-CoV2373 [Novavax Nuvaxovid]) vaccines [16]. There was also concern over the use of NVX-CoV2373 in the USA [17].
Previously, only smallpox vaccines had been linked to myocarditis [3, 18]. According to the US Department of Defense Smallpox Vaccination Clinical Evaluation Team in 2002, there was a significant rise in myocarditis after widespread smallpox vaccination (with a live attenuated virus) among young military personnel whose mean age was in the late third decade [3, 19]. The following smaller scale study (which included 1081 smallpox vaccine recipients and 189 influenza vaccine recipients) concluded that passive surveillance underestimates the true incidence of myocarditis after smallpox vaccination [2]. Although that study noted that myocarditis was not increased following an influenza vaccination, the number of cases was too small, and the participants were primarily young healthy adults. Therefore, the findings may not apply to elderly individuals. Notably, the rate of clinical or subclinical myocarditis and pericarditis after a smallpox vaccination was approximately 1:5500, despite the fact that the rate of elevation of a laboratory marker (troponin level) was 1:200. It suggested that many cases had been overlooked as they had only subclinical or mild disease activity. Without a high clinical alert or routine screening, it would be impossible to examine the case for myocarditis.
As COVID-19 mRNA vaccine-associated myocarditis has been mostly reported to develop in young people, it will be fascinating to see whether there is a similar effect in the same age group that received the influenza vaccine. Despite this, elderly individuals must be included in this study for a variety of reasons. Influenza is a common cause of hospitalization and death among the elderly, especially those with chronic diseases. As a result, since 2001, Taiwan’s Center for Disease Control has been providing a free annual influenza vaccination to all individuals aged 65 years and older through the NHI program [20]. For the younger age group, only children, students, those with major diseases, and healthcare workers have access to the free influenza vaccine. Thus, using Taiwan’s data to analyze the effects on young people is not ideal because of the existence of selection biases. However, COVID-19 vaccine-related myocarditis might not only happen in young people, as the first dose of the ChAdOx1 (AstraZeneca Vaxzevria) vaccine is reported to increase the risk of myocarditis among men and women of any age [5].
Serial or multi-session vaccination is also an important factor to consider in examining the risk of myocarditis arising following a COVID vaccination, as repeated vaccinations may impose an additional increased risk. It has been reported that most cases of myocarditis occurred following the second dose of the COVID vaccine [6, 21]. Although the current study does not further analyze this cohort, the subsequent injection might not matter for the influenza vaccine because the observation period (from 2003 to 2017) was long enough to include many people who had received annual vaccinations many times.
The influenza virus can directly infect myocardial cells and indirectly impair cardiovascular functions. Influenza is linked to increased risks of major cardiovascular diseases, such as myocardial infarction, heart failure, and stroke [22]. The influenza vaccine is proven to reduce myocardial infarction in high-risk groups [22, 23]. Influenza virus-induced myocarditis is also a significant concern, although its epidemiology is difficult to determine. It is unknown, however, whether the influenza vaccination can reduce the risk of influenza-induced myocarditis. In contrast, patients and clinicians may worry that any form of myocarditis, including mild forms, can threaten a specific population. If new myocarditis occurs, specifically in patients with a lower reserve of heart function, such as those with heart failure and underlying heart disease, any further insults may tip the balance toward decompensation. Therefore, some clinicians might recommend that patients in a poor general condition should not receive an influenza vaccine. Our study found no increase in the risk of myocarditis following the influenza vaccine among those with a high CCI score, cancer, or autoimmune diseases.
This study has several limitations. First, because health insurance data are declaration data and not medical records, detailed examination results cannot be obtained, thus we used the principal admission diagnostic code to identify myocarditis. Whereas, in reality, the diagnosis of myocarditis is only made after other possible differential diagnoses have been ruled out through a series of laboratory and imaging studies, which have been validated in the past [14]. Second, in this study, disease severity and long-term complication of myocarditis were not provided. Furthermore, only those who had been hospitalized were included. Therefore, those who experienced mild myocarditis and received outpatient treatment without having to be hospitalized have not been included. We cannot completely exclude the possibility that the influenza vaccine may increase subclinical myocarditis, thus a prospective study with frequent laboratory testing might be worth conducting to answer this question in the future. Third, despite the previous literature indicating that COVID vaccine-associated myocarditis occurs predominantly in young individuals, this study was unable to compare whether the incidence of myocarditis increases after the influenza vaccination in younger individuals. The main reason is that among young individuals, only children, students, those with major diseases, and healthcare workers have access to the free influenza vaccine in Taiwan. Thus, it is not suitable to use Taiwan’s NHI Research Database to analyze the incidence of myocarditis after the influenza vaccination in young healthy people because of the existence of selection biases. Finally, because there is no large-scale research examining the association of myocarditis with the influenza vaccination, the risk period has not been determined properly. According to the current knowledge of smallpox and COVID, vaccine-related myocarditis occurs within a few days following administration of the vaccine [3,4,5,6, 19]. Guillain–Barré syndrome deserves a mention here as another possible adverse reaction of the influenza vaccination. It is reported that the risk of Guillain–Barré syndrome increases within 42 days of vaccination, with the highest risk occurring between days 8 and 21 after vaccination [24]. Therefore, we adopted the similar risk periods (days 1–7, 1–14, 1–42) to analyze the risk of myocarditis after receiving an influenza vaccination.
5 Conclusions
Our study reveals that for elderly individuals (aged ≥ 65 years), the risk of myocarditis is not significantly increased following an influenza vaccination during days 1–7, 1–14, and 1–42, irrespective of age (65–74, 75–84, ≥ 85 years), sex, comorbidities, and autoimmune diseases. In light of these results, the public, clinicians, and policymakers can dismiss the fear of this potentially adverse event of the influenza vaccination.
References
Kociol RD, Cooper LT, Fang JC, Moslehi JJ, Pang PS, Sabe MA, et al. Recognition and initial management of fulminant myocarditis: a scientific statement from the American Heart Association. Circulation. 2020;141(6):e69-92.
Engler RJ, Nelson MR, Collins LC Jr, Spooner C, Hemann BA, Gibbs BT, et al. A prospective study of the incidence of myocarditis/pericarditis and new onset cardiac symptoms following smallpox and influenza vaccination. PLoS ONE. 2015;10(3): e0118283.
Halsell JS, Riddle JR, Atwood JE, Gardner P, Shope R, Poland GA, et al. Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel. JAMA. 2003;289(24):3283–9.
Witberg G, Barda N, Hoss S, Richter I, Wiessman M, Aviv Y, et al. Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med. 2021;385(23):2132–9.
Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022;28(2):410–22.
Buchan SA, Seo CY, Johnson C, Alley S, Kwong JC, Nasreen S, et al. Epidemiology of myocarditis and pericarditis following mRNA vaccination by vaccine product, schedule, and interdose interval among adolescents and adults in Ontario, Canada. JAMA Netw Open. 2022;5(6): e2218505.
Nagano N, Yano T, Fujita Y, Koyama M, Hasegawa R, Nakata J, et al. Hemodynamic collapse after influenza vaccination: a vaccine-induced fulminant myocarditis? Can J Cardiol. 2020;36(9):1554.e5-7.
Nakamura R, Ando S-I, Kato S, Kadokami T. Acute lymphocyte myocarditis associated with influenza vaccination. Intern Med. 2022;61(15):2307–13.
Kim Y-J, Bae J-I, Ryoo SM, Kim WY. Acute fulminant myocarditis following influenza vaccination requiring extracorporeal membrane oxygenation. Acute Crit Care. 2019;34(2):165.
Cheng MP, Kozoriz MG, Ahmadi AA, Kelsall J, Paquette K, Onrot JM. Post-vaccination myositis and myocarditis in a previously healthy male. Allergy Asthma Clin Immunol. 2016;12(1):1–6.
Hsieh C-Y, Su C-C, Shao S-C, Sung S-F, Lin S-J, Yang Y-HK, et al. Taiwan’s national health insurance research database: past and future. Clin Epidemiol. 2019;11:349.
Chang YC, Chou YJ, Liu JY, Yeh TF, Huang N. Additive benefits of pneumococcal and influenza vaccines among elderly persons aged 75 years or older in Taiwan: a representative population-based comparative study. J Infect. 2012;65(3):231–8.
Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, et al. Acute Myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378(4):345–53.
Chang JJ, Lin MS, Chen TH, Chen DY, Chen SW, Hsu JT, et al. Heart failure and mortality of adult survivors from acute myocarditis requiring intensive care treatment: a nationwide cohort study. Int J Med Sci. 2017;14(12):1241–50.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Heath PT, Galiza EP, Baxter DN, Boffito M, Browne D, Burns F, et al. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N Engl J Med. 2021;385(13):1172–83.
Buntz B. FDA considers possible myocarditis link in Novavax COVID-19 vaccine recipients 2022. Available from: https://www.drugdiscoverytrends.com/fda-considers-possible-myocarditis-link-in-novavax-covid-19-vaccine-recipients/. [Accessed 23 Jun 2022].
Su JR, McNeil MM, Welsh KJ, Marquez PL, Ng C, Yan M, et al. Myopericarditis after vaccination, vaccine adverse event reporting system (VAERS), 1990–2018. Vaccine. 2021;39(5):839–45.
Arness MK, Eckart RE, Love SS, Atwood JE, Wells TS, Engler RJ, et al. Myopericarditis following smallpox vaccination. Am J Epidemiol. 2004;160(7):642–51.
Yang CL, Chen TY, Chih YC, Chou SM, Chen CH, Yang CH. The overview of government-funded influenza vaccination program during influenza season 2011–2012. Taiwan Epidemiol Bull. 2013;29(20):252–9.
Fazlollahi A, Zahmatyar M, Noori M, Nejadghaderi SA, Sullman MJ, Shekarriz-Foumani R, et al. Cardiac complications following mRNA COVID-19 vaccines: a systematic review of case reports and case series. Rev Med Virol. 2022;32(4): e2318.
Yedlapati SH, Khan SU, Talluri S, Lone AN, Khan MZ, Khan MS, et al. Effects of influenza vaccine on mortality and cardiovascular outcomes in patients with cardiovascular disease: a systematic review and meta-analysis. J Am Heart Assoc. 2021;10(6): e019636.
Smeeth L, Thomas SL, Hall AJ, Hubbard R, Farrington P, Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351(25):2611–8.
Schonberger LB, Bregman DJ, Sullivan-Bolyai JZ, Keenlyside RA, Ziegler DW, Retailliau HF, et al. Guillain-Barré syndrome following vaccination in the national influenza immunization program, United States, 1976–1977. Am J Epidemiol. 1979;110(2):105–23.
Acknowledgments
This study is based, in part, on data released by the Health and Welfare Data Science Center, Ministry of Health and Welfare. The interpretation and conclusions contained herein do not represent those of the Ministry of Health and Welfare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no external funding.
Conflicts of Interest
Wen-Hwa Wang, Kai-Che Wei, Yu-Tung Huang, Kuang-Hua Huang, Tung-Han Tsai, Yu-Chia Chang have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
This study protocols were reviewed and approved by the Institutional Review Board of Taichung Jen-Ai Hospital, Taiwan (Institutional Review Board No. 108-83).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Data used in the analysis were released by the Health and Welfare Data Science Center, Ministry of Health and Welfare, Taiwan, which provide scrambled random identification numbers for insured patients to protect the privacy of beneficiaries. The database was anonymous, therefore, the requirement for informed consent was waived.
Code Availability
Not applicable.
Authors’ Contributions
W-HW, K-CW, and Y-CC designed and performed the study. Y-TH, K-HH, and T-HT analyzed the data. W-HW, K-CW, and Y-CC wrote the manuscript in consultation with Y-TH, K-HH, and T-HT. All authors discussed the results and contributed to the final manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, WH., Wei, KC., Huang, YT. et al. The Incidence of Myocarditis Following an Influenza Vaccination: A Population-Based Observational Study. Drugs Aging 40, 145–151 (2023). https://doi.org/10.1007/s40266-022-00997-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-022-00997-0