Abstract
Introduction
Manipulation under anesthesia (MUA) is often used for frozen shoulder treatment, but controversy still exists regarding MUA compared with conservative treatment. This research was conducted to compare the outcome between MUA and celecoxib (CLX) in secondary frozen shoulder.
Methods
Patients with secondary frozen shoulder were randomized into two groups, an MUA plus exercise (EX) group and a CLX plus EX group. Clinical outcomes were documented at baseline and at 1 day, 2, 4, and 12 weeks after intervention, including Constant–Murley Score (CMS) for function, Pain Rating Index (PRI) and Present Pain Intensity (PPI) for pain, passive range of motion (ROM) measurements including external rotation, internal rotation, forward flexion, and abduction. Primary outcome was CMS. Secondary outcomes were PRI, PPI, and passive ROM.
Results
Sixty-seven patients out of 68 in the MUA group and 66 out of 68 in the CLX group finished the entire study period. There were no significant differences in basic properties of the two groups before intervention. As the primary outcome, CMS changes in the MUA group improved faster than the CLX group. Secondary outcomes, passive ROM, and pain PPI were faster and significant in the MUA group from 1 day after intervention compared with CLX (P < 0.05). At 12 weeks, a statistically significant difference was not observed in the PPI (P > 0.05). A statistically significant difference was not observed in the PRI between groups in 1 day (P > 0.05). For the primary outcome, from 0 to 12 weeks the mean changes in CMS were 44.00 for MUA plus EX (95% CI 43.07–44.93, P < 0.001) and 27.09 for CLX plus EX (26.20–27.98, P < 0.001). The significant difference in improvement appeared from 2 weeks.
Conclusion
To treat secondary frozen shoulder with MUA, this treatment could achieve better therapeutic effects on improvement of function, pain, and passive ROM than CLX did.
Clinical Trial Registration
The trial was registered at www.chictr.org.cn, identifier ChiCTR2200060269.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Treatment for secondary frozen shoulder remains a challenge. |
Manipulation under anesthesia is an attractive choice for primary frozen shoulder. |
We hypothesized that manipulation under anesthesia compared with conservative treatment, each combined with exercise, could yield better effects in terms of improvement in Constant–Murley Score, pain, passive range of motion, and function of secondary frozen shoulder. |
What was learned from the study? |
Manipulation under anesthesia could improve the function, passive range of motion, and relieve pain of secondary frozen shoulder. |
It is reasonable to incorporate manipulation under anesthesia into the treatment strategy in patients with secondary frozen shoulder. |
Introduction
Frozen shoulder (FS) is a common cause of shoulder pain and disability that affects approximately 2–4% of the general population [1]. It most generally influences people in the sixth decade of life [2, 3]. The etiology can be caused by primary or secondary rationales [4]. The condition of the shoulder is affected by unexplained pain, stiffness, and limitation in the active and passive range of motion (ROM) in two or more planes, which leads to progressive shoulder dysfunction. FS is traditionally divided into three phrases [5]: freezing phase, frozen phase, and thawing phase. Previous research showed that FS was a self-limiting, reversible condition [5, 6]. It can spontaneously resolve, but the recovery may be slow. Although it may take 2–3 years, most patients are satisfied with the recovery [7, 8]. Approximately 40% of patients still have persistent symptoms 4 years after onset [9]. About 15% of patients will have sequelae of long-term disability [10]. The pathophysiology of primary FS is still little known [11]. It may be associated with diabetes, thyroid conditions, Dupuytren contracture, smoking, etc. [4]. Secondary FS is defined by having definite etiology leading to shoulder stiffness such as trauma or surgery. People with FS have difficulty performing basic daily activities and sleep disturbance because of shoulder pain [12], which increases at night [13].
Although there is not a well-defined model pattern for the medical management of FS, a variety interventions still can be applied to it, including conservative and invasive treatment [14]. The therapeutic management usually is based on expert personal experience instead of approved evidence [15]. Conservative treatment is composed of medication, physical therapy, exercise (EX), steroid injection or nerve blocks which can relieve symptoms [16]. The conservative treatment is considered appropriate for the majority of patients with FS [14]. However, up to 50% of patients have persistent pain with conservative treatment [17, 18]. There are several invasive treatments, such as manipulation under anesthesia (MUA), open or arthroscopic capsular release, and hydrodilation. These methods may improve the shoulder range of motion and relieve pain but may leave other complications [16].
At present, there is no unified medical management for secondary FS. It is formulated accord to the principle of primary FS. Traditionally, if conservative treatment does not improve the symptoms of FS, MUA is an appropriate choice [19]. MUA is a simple and effective procedure. After treatment, the capsular adhesions are torn apart which results in the rapid restoration of ROM and relief of symptoms [20]. Even so, there is still some controversy regarding its use. In rare cases, some serious adverse events occur that include humeral fracture, glenohumeral dislocation, and brachial plexus traction injury [21]. There is only one research study about MUA for secondary FS following breast cancer [22]. The results suggested that MUA, corticosteroid injection, and physiotherapy achieved good final results [22]. However, in that study, the experiment group mixed corticosteroid injection and physiotherapy treatment. Therefore, no firm conclusion can be drawn about MUA for secondary FS.
The objective of this trial was to assess the effectiveness of MUA plus EX compared to celecoxib (CLX) plus EX in the treatment of patients with secondary FS. We hypothesize that for secondary FS the MUA treatment would have a quicker functional recovery and faster pain relief compared to celecoxib treatment.
Methods
Study Design
This trial is a prospective, single-center randomized controlled trial conducted in accordance with the principles of the Declaration of Helsinki. The data reported from this trial comply with the Consolidated Standards of Reporting Trials (CONSORT) statement. The study was conducted in the local hospital and was approved by the local ethics committee board (Shuguang Hospital, ChiECRCT20200121). An informed consent form was signed by all participants prior to study. The clinical trial was registered in the Chinese Clinical Trial Registry (ChiCTR2200060269).
Randomization and Blinding
The CONSORT diagram for participants is shown in Fig. 1. Patients were randomly assigned to one of the two following groups by one researcher independently: an MUA plus EX group or a CLX plus EX group. Randomization was done by using a computer program that included a randomized table of numbers, which was created by an independent individual who was not involved in the recruitment and treatment of patients. Numbered cards with a random assignment and containing information about the group allocation in opaque, sealed envelopes were prepared by the independent individual. All participants were blinded to their treatment assignment.
Sample Size Calculation
Power analysis was conducted before the commencement of patient recruitment. Constant–Murley Score (CMS) is the primary outcome parameter. Based on the ability to confirm a difference between treatment groups of at least 10 points of CMS, the reported minimum clinically important difference (MCID) of CMS is 10 points [23]. According to previous research, the study shows an estimated mean CMS of 71 and a standard deviation of 15.5 points [24]. On the basis of these parameters, to achieve 90% power at a two-sided 5% significance, 65 patients were required in each group with a 20% dropout rate. We rounded up it to 68.
Participants
The patients were recruited from outpatients and inpatients of the orthopedics and traumatology department. Patients who were willing to participate in the research were evaluated to decide whether their condition met the study aim. In order to be eligible to participate in this study, patients must meet all of the inclusion criteria and none of the exclusion criteria.
Inclusion criteria were as follows: (1) subjects aged 40–70 years; (2) subjects clinically diagnosed with secondary FS characterized by restriction of function in the affected shoulder; (3) subjects that have definite cause, including trauma, non-osteoporotic fractures around the shoulder, long-term immobilization after lung cancer, breast cancer, or other surgery; (4) subjects that have the ability to comprehend the instructions in the study.
Exclusion criteria were as follows: (1) definitive evidence of rotator cuff tear, fracture, tumor in the shoulder, ligament rupture proved by magnetic resonance imaging (MRI); (2) allergy to narcotic drugs; (3) shoulder symptom resulting from skin contracture caused by cervical radiculopathy, brachial plexus lesion, connective tissue disorders, and scald around the shoulder; (4) other known shoulder pathology such as infection and broken skin; (5) pregnant, lactating women; (6) systemic inflammatory joint disease; (7) inability to give informed consent and fill out questionnaires; (8) unwilling to complete the medical observation.
From June 2019 to December 2020, a total of 136 eligible patients with a diagnosis of secondary FS were enrolled in the trial. The 136 patients were randomized to the MUA followed by EX group (n = 68) and celecoxib followed by EX group (n = 68) (Fig. 1).
Intervention
Anesthesia
The patient was place in a supine position, with head tilting to the healthy side. A soft thin pillow was placed under the neck and shoulder to expose the puncture site. An interscalene block was performed by the anesthesiologist using ultrasound guidance in the operating room. The interscalene block was located at the space between sternocleidomastoid muscle and anterior scalene muscle. A mixture containing 10 mL 75 mg ropivacaine and 10 mL 2% lidocaine was used for brachial plexus block anesthesia.
MUA
The surgeon stands on the affected side of the patient in a supine position. Under anesthesia, the affected arm was held in anteflexion. The shoulder was gently moved in 180° anteflexion. During the process, we hold the elbow of the affected arm with one hand and the other hand is placed on the proximal humerus near the humeral head at the patient’s axilla to prevent shoulder dislocation. This process is performed three times; these maneuvers result in tearing of fibrosed capsule and ligament, which can often be felt or heard. Next, the shoulder is positioned at external rotation, abduction, and flexion to 180°. Forward flexion to 90° for the shoulder and elbow, the shoulder adducted to 45°. At the end, supine position remained, the affected shoulder abducted to 45°, and rotator interval was conducted. Supine with shoulder internal rotation, the thumb can touch the healthy-side shoulder blade at least.
Control Group
Eligible participants randomized to the placebo group received 200 mg celecoxib (Celebrex, Pfizer) every day for 12 days.
Exercises
-
1.
Climbing wall training.
The patient stood facing the wall with feet shoulder-width apart. The toes approach the edge of wall. Five splayed fingers are placed on the wall, climbing high slowly along the wall within the patient’s pain tolerance. If necessary, the process was finished with the aid of the heathy upper limb or others.
-
2.
Putting on the other shoulder training.
The affected-side elbow remained in flexion and close to the chest within pain limitation. The healthy-side hand was placed behind the affected elbow. The affected elbow was pushed up gradually so the affected-side hand reaches the other shoulder.
-
3.
Pulling hand back.
Patients kept the position of sitting or upright. The affected upper limb was placed behind the back, adducted and raised gradually. Another healthy hand was used to help the affected hand raise to the highest position.
Note: repeat the three steps three times a day, three times each time.
Outcomes and Follow-up
An independent physician who was blinded to the intervention collected all the data at 0 week (baseline), 1 day, 2 weeks, 4 weeks, and 12 weeks after treatment. The primary outcome was CMS. Secondary outcomes included the McGill Pain Questionnaire (MPQ) containing Pain Rating Index (PRI) and Present Pain Intensity (PPI) and passive ROM, including forward flexion, abduction, internal rotation, and external rotation with the arm at the side.
The passive flexion, passive abduction, and passive external rotation were measured using a digital angle ruler. The smallest unit of measurement is 5°. The passive internal rotation was expressed as the highest spinous process level at the back reached with the tip of the thumb. The vertebra level of sacrum was recorded as 1 point. From the fifth to first lumbar vertebra, it was numbered serially 2–6, and so on.
Statistical Analysis
R 4.0.3 statistical software was used for all statistical analysis. A P value less than 0.05 was considered statistically significant. The continuous data are expressed as mean and standard deviation (SD), and the categorical data are expressed as frequency and percentages. The chi-square test was used to detect differences between binary variables. The Kolmogorov–Smirnov test was applied to the continuous data to determine if they followed a normal distribution. Baseline demographic characteristics and the mean improvement from baseline in each clinical outcome at each follow-up visit were assessed for each patient. Student t test (for continuous data that were normally distributed), the Mann–Whitney U test (for continuous data that were not normally distributed), or generalized linear mixed model (GLMM) were applied for the study comparison. For outcomes analysis, GLMM was used for repeated measures. The changes from baseline measurements were modeled with GLMM. Differences in mean changes from baseline for each outcome at each time were compared between groups. The outcome model included fixed effects for treatment, time, and the interaction of trial group with time.
Results
A total of 136 participants diagnosed with secondary FS were included in this study. Sixty-eight patients were included in the MUA plus EX group, which contained 23 patients suffering from im**ement or traction injury of the shoulder, 9 patients postoperative of breast cancer, 10 patients postoperative of lung cancer, 13 patients postoperative of shoulder surgery, 8 patients postoperative of pacemaker implantation, 3 patients postoperative of axillary lymph node dissection, and 2 patients with long-term immobilization postoperative of clavicle fracture. The control group comprised 68 patients, including 25 patients suffering from im**ement or traction injury of the shoulder, 8 patients were postoperative of breast cancer, 9 patients were postoperative of lung cancer, 17 patients were postoperative of shoulder surgery, 6 patients were postoperative of pacemaker implantation, and 3 patients were in long-term immobilization of humeral shaft fracture (Table 1).
One patient in the MUA plus EX group and two in the control group withdrew from the study. A total of 133 patients were therefore analyzed, i.e., 67 in the MUA plus EX group and 66 in the control group (Fig. 1). The demographic properties of patients included did not vary between groups (Table 2). There was no difference in clinical characteristics between groups at baseline (Table 3).
Significant differences between the two groups were defined by the test of group-by-time interaction (P < 0.001), suggesting that MUA plus EX was more efficacious than celecoxib plus EX. At each follow-up time point, the CMS in the MUA group was significantly more than that in the control group (P < 0.001), indicating faster relief in the MUA group than that in the control group by time. For intragroup comparisons, a significant improvement in CMS was observed 1 day after treatment in the MUA (P < 0.001) and control (P < 0.001) groups. Improvement in all groups lasted until 12 weeks (Table 4). At the 12-week follow-up, the CMS was 94.45 ± 1.44 in the MUA group and 77.06 ± 1.87 in the control group (P < 0.001) (Table 3), suggesting that the effect of improving shoulder function in MUA was stronger than celecoxib.
Similar to the changes in CMS, there were significant differences in passive ROM, PRI, and PPI according to the group-by-time interaction (P < 0.001 for all). Comparisons at each time point were conducted to further describe the difference between groups. Passive forward flexion, passive abduction, passive internal rotation, and passive external rotation values of the MUA group were significantly better than those of the control group at every time point (P < 0.001). PPI values of the MUA group were significantly better than those of the control group at 1 day (P < 0.001), 2 weeks (P < 0.001), and 4 weeks (P < 0.001), except for a nonsignificant difference between the two groups at 12 weeks (P = 0.341). In the MUA group, PRI value was significantly superior to that of the control group at 2, 4, and 12 weeks, while there was no significant difference in pain rating index at 1 day between the two groups (P = 0.464) (Table 3). These results showed that patients benefited more from MUA than from celecoxib. Considering the time factor, the effect of MUA was faster than celecoxib.
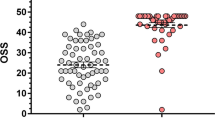
Compared with pre-treatment, passive ROM in the MUA group increased significantly at 1 day and lasted until 12 weeks (P < 0.001 for all four aspects). Passive ROM in the control group also had significant differences. However, only the passive external rotation had a significantly increase at 1 day compared with pre-treatment (P < 0.001). A significant improvement was not observed until 2 weeks in passive forward flexion, passive abduction, and passive internal rotation (P < 0.001 for three aspects) (Table 4). According to the changes of passive ROMs, although an effect of celecoxib was observed, MUA therapy took effect earlier than it. At 12 weeks after treatment, passive external rotation recovered to 75.00° ± 5.00° and 59.70° ± 5.40°, passive internal rotation to 12.70° ± 0.84° and 7.77° ± 1.12°, passive flexion to 172.16° ± 4.37° and 132.12° ± 8.32°, and passive abduction to 164.78° ± 5.87° and 118.79° ± 14.57° in the MUA and celecoxib groups, respectively (Table 3). Figure 2 shows the time course of the mean CMS.
In the follow-up process, one patient in the CLX group had gastrointestinal reactions which gradually improved after discontinuing medication. One patient accepted surgical treatment and withdrew from follow-up. No patient reported other adverse effects during the follow-up.
Discussion
To our knowledge, our study is the first randomized controlled trial to compare the effects of MUA with CLX for secondary FS. The results of this study showed that the MUA and CLX treatment improve shoulder function, but the effect of MUA was faster and stronger than CLX. Compared with the CLX group, CMS of the MUA group had significant restoration with earlier and better recovery. Alleviation of shoulder pain, evaluated via PRI and PPI, was reported in MUA and CLX groups. But patients in the MUA group had greater recovery. Patients receiving MUA and CLX treatment had significant improvement in passive ROMs. The MUA group had earlier and greater recovery.
Although similar, the pathology of primary and secondary FS is not all the same. In idiopathic primary FS, the main feature is inflammatory contracture of glenohumeral synovial capsule, coracohumeral ligament, soft tissues of rotator interval, and subscapularis muscle; and the hyperplastic fibroplasia and excessive type III collagen secretion generated [25]. Biopsy material from shoulder rotator interval showed chronic inflammation and proliferative fibrosis appeared, and existence of high vascularity and nerve tissue. Glenohumeral movement is limited by available intra-articular volume reduction. The aforementioned changes explain the reasons for pain and stiffness in FS [25]. The fibrosed capsule–ligament complex of the shoulder hinders the retrieval of shoulder ROM. FS is generally considered a self-limiting disease. However, few cases may have long-term disability and pain [17]. As for secondary FS, there is little understanding of the pathology until now. Extra rotator cuff and soft tissue contracture may exist which lead to a poor prognosis [14].
According to ISAKOS (International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine) Upper Extremity Committee, secondary FS is defined definite trauma or surgery leading to dysfunction of the shoulder [4]. With the large increase of shoulder trauma and surgery, the incidence of secondary FS is rising. Common shoulder traumas include violent impact or pull, shoulder dislocation, distal humerus fracture, clavicle fracture, rotator cuff injury, etc. Clinically relevant procedures include rotator cuff repair, shoulder instability repair, lung cancer surgery, breast surgery, and pacemaker implantation [22, 26,27,28]. The overall incidence of FS following shoulder surgery and long-term postoperative immobilization is approximately 11% [29]. Frozen shoulder is the most documented cause of morbidity [30]. A study of a large data set found a 3.8% incidence of FS after breast cancer operation [31]. For patients with cancer, myofibroblasts are activated by cytokines released from the accumulated inflammatory cells comprised of neutrophils, macrophages, monocytes, and lymphocytes. Coupled with the vasodilation and angiogenesis after radiotherapy, this activation can lead to increased extracellular matrix deposition and subsequent fibrosis, causing shoulder pain, ROM restriction, and secondary FS [32,33,34].
All the findings of this study provide strong evidence for understanding FS. By MUA treatment, the complex is forcibly broken by maneuvering the shoulder across the ROM under anesthesia. Previous research suggested that MUA can improve function in patients with stage 2 refractory FS [35]. Some studies showed that long-term clinical outcome after MUA is excellent [19, 36, 37]. To date, only a small number of trials have focused on the influence of MUA on secondary FS. Nagata et al. conducted a small observational study on secondary FS resulting from previous anterior dislocation with MUA and injection, and most patients had considerable improvements in Oxford Shoulder Score (OSS) and ROM [26]. The mean improvement in OSS at follow-up after MUA and injection treatment was 18. The ROM improved at a mean of forward flexion 99°, abduction 107°, external rotation 52°, and internal rotation 40°. A preliminary study of MUA for secondary FS following breast cancer suggested that MUA achieved good final results in a series of patients with FS secondary to breast cancer treatment. The mean OSS improved from 31 to 43 [22]. Our research results are consistent with these previous studies.
One article deemed that MUA should not be performed for secondary stiffness of the shoulder and that arthroscopic capsular release must be applied to such patients [38]. Several controversies still remain regarding MUA, such as timing [39], with or without steroid injection [40], and the impact in diabetes [41]. According to literature reports, the overall complication rate of MUA is 0.4% [35]. Although MUA can improve shoulder function including flexion and abduction, surgeons often avoid forcible manipulation in MUA because of the fear of complications. Some articles have reported the common complications, such as humeral shaft fracture, rotator cuff tear, shoulder dislocation, labral tear, nerve injury, and complex regional pain syndrome [42, 43]. One research study performed arthroscopy after MUA and demonstrated iatrogenic superior labrum anterior–posterior lesions and partial tears of the subscapularis tendon [44].
Overall, manipulation under anesthesia for FS is a generally safe and successful operation. Nevertheless, surgeons should be aware of and inform patients of potential consequences because every capsular release approach has the potential to induce tissue injuries.
There are several limitations in our study. First, conservative treatment is used for FS for 6 months. In our study, the clinical stage of FS was not assessed at baseline. This may influence the effect of CLX for patients with long-term course. Second, in patients with FS, psychologic issues have been reported linked to shoulder pain and restrictions [45]. This research did not include psychological evaluation. Third, MRI of the shoulder was not evaluated after MUA. In that case, tissue insults and bone bruises may be omitted as we were unable to verify the shoulder structures, such as capsule and ligaments, after treatment. The positive effect of MUA may also be due to the sympathetic effects of the scalene anesthesia. Nevertheless, the major limitation of the present study was the lack of a placebo group. We cannot rule out the possibility that patients got better despite any treatments they received. However, symptoms in secondary FS generally improve much less without treatment, and the significant differences larger than MCID between the two treatments might well supersede any placebo effect in this trial. Furthermore, as the two comparison methods were commonly prescribed in the study hospitals, it would have been extremely difficult for the researchers to obtain ethical approval for including a control arm with only placebo.
Conclusion
To treat secondary FS with MUA, this treatment could achieve better therapeutic effects on improvement of function, pain, and passive ROM than CLX did.
References
White D, Choi H, Peloquin C, Zhu Y, Zhang Y. Secular trend of adhesive capsulitis. Arthritis Care Res. 2011;63(11):1571–5.
Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004;51(4):642–51.
van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54(12):959–64.
Itoi E, Arce G, Bain GI, et al. Shoulder stiffness: current concepts and concerns arthroscopy. Arthroscopy. 2016;32(7):1402–14.
Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975;4(4):193–6.
Jayson MI. Frozen shoulder: adhesive capsulitis. Br Med J (Clin Res Ed). 1981;283(6298):1005–6.
Hubbard MJ, Hildebrand BA, Battafarano MM, Battafarano DF. Common soft tissue musculoskeletal pain disorders. Prim Care. 2018;45(2):289–303.
**ao RC, DeAngelis JP, Smith CC, Ramappa AJ. Evaluating nonoperative treatments for adhesive capsulitis. J Surg Orthop Adv. 2017;26(4):193–9.
Hand C, Clipsham K, Rees JL, Carr AJ. Long-term outcome of frozen shoulder. J Shoulder Elbow Surg. 2008;17(2):231–6.
Favejee MM, Huisstede BM, Koes BW. Frozen shoulder: the effectiveness of conservative and surgical interventions—systematic review. Br J Sports Med. 2011;45(1):49–56.
Ryan V, Brown H, Minns Lowe CJ, Lewis JS. The pathophysiology associated with primary (idiopathic) frozen shoulder: a systematic review. BMC Musculoskelet Disord. 2016;17(1):340.
Jones S, Hanchard N, Hamilton S, Rangan A. A qualitative study of patients’ perceptions and priorities when living with primary frozen shoulder. BMJ Open. 2013;3(9): e003452.
Jain TK, Sharma NK. The effectiveness of physiotherapeutic interventions in treatment of frozen shoulder/adhesive capsulitis: a systematic review. J Back Musculoskelet Rehabil. 2014;27(3):247–73.
Robinson CM, Seah KT, Chee YH, Hindle P, Murray IR. Frozen shoulder. J Bone Jt Surg Br. 2012;94(1):1–9.
Kwaees TA, Charalambous CP. Surgical and non-surgical treatment of frozen shoulder. Survey on surgeons treatment preferences. Muscles Ligaments Tendons J. 2014;4(4):420–4.
Le HV, Lee SJ, Nazarian A, Rodriguez EK. Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Should Elb. 2017;9(2):75–84.
Shaffer B, Tibone JE, Kerlan RK. Frozen shoulder. A long-term follow-up. J Bone Jt Surg Am. 1992;74(5):738–46.
Binder AI, Bulgen DY, Hazleman BL, Roberts S. Frozen shoulder: a long-term prospective study. Ann Rheum Dis. 1984;43(3):361–4.
Vastamäki H, Vastamäki M. Motion and pain relief remain 23 years after manipulation under anesthesia for frozen shoulder. Clin Orthop Relat Res. 2013;471(4):1245–50.
Dodenhoff RM, Levy O, Wilson A, Copeland SA. Manipulation under anesthesia for primary frozen shoulder: effect on early recovery and return to activity. J Shoulder Elbow Surg. 2000;9(1):23–6.
Amir-Us-Saqlain H, Zubairi A, Taufiq I. Functional outcome of frozen shoulder after manipulation under anaesthesia. J Pak Med Assoc. 2007;57(4):181–5.
Leonidou A, Woods DA. A preliminary study of manipulation under anaesthesia for secondary frozen shoulder following breast cancer treatment. Ann R Coll Surg Engl. 2014;96(2):111–5.
Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22(12):1650–5.
Zhang J, Tan YB, Lie DTT. Outcomes of arthroscopic rotator cuff repair in stiff shoulders are comparable to non-stiff shoulders when combined with manipulation under anesthesia. Arthroscopy. 2020;36(12):2954–61.
Hand GC, Athanasou NA, Matthews T, Carr AJ. The pathology of frozen shoulder. J Bone Jt Surg Br. 2007;89(7):928–32.
Nagata H, Thomas WJ, Woods DA. The management of secondary frozen shoulder after anterior shoulder dislocation – the results of manipulation under anaesthesia and injection. J Orthop. 2016;13(2):100–5.
Anjum R, Aggarwal J, Gautam R, Pathak S, Sharma A. Evaluating the outcome of two different regimes in adhesive capsulitis: a prospective clinical study. Med Princ Pract. 2020;29(3):225–30.
Tzeng CY, Chiang HY, Huang CC, et al. The impact of pre-existing shoulder diseases and traumatic injuries of the shoulder on adhesive capsulitis in adult population: a population-based nested case-control study. Medicine. 2019;98(39):e17204.
Koorevaar RCT, Van’t Riet E, Ipskamp M, Bulstra SK. Incidence and prognostic factors for postoperative frozen shoulder after shoulder surgery: a prospective cohort study. Arch Orthop Trauma Surg. 2017;137(3):293–301.
Stubblefield MD, Custodio CM. Upper-extremity pain disorders in breast cancer. Arch Phys Med Rehabil. 2006;87(3 Suppl 1):S96–9 (quiz S100-1).
Cho CH, Lee KL, Cho J, Kim D. The incidence and risk factors of frozen shoulder in patients with breast cancer surgery. Breast J. 2020;26(4):825–8.
Yarnold J, Brotons MC. Pathogenetic mechanisms in radiation fibrosis. Radiother Oncol. 2010;97(1):149–61.
Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol. 2003;4(9):529–36.
O’Sullivan B, Levin W. Late radiation-related fibrosis: pathogenesis, manifestations, and current management. Semin Radiat Oncol. 2003;13(3):274–89.
Kraal T, Beimers L, The B, et al. Manipulation under anaesthesia for frozen shoulders: outdated technique or well-established quick fix? EFORT Open Rev. 2019;4(3):98–109.
Farrell CM, Sperling JW, Cofield RH. Manipulation for frozen shoulder: long-term results. J Shoulder Elbow Surg. 2005;14(5):480–4.
Thomas WJ, Jenkins EF, Owen JM, et al. Treatment of frozen shoulder by manipulation under anaesthetic and injection: does the timing of treatment affect the outcome? J Bone Jt Surg Br. 2011;93(10):1377–81.
Pandey V, Madi S. Clinical guidelines in the management of frozen shoulder: an update! Indian J Orthop. 2021;55(2):299–309.
Vastamäki H, Varjonen L, Vastamäki M. Optimal time for manipulation of frozen shoulder may be between 6 and 9 months. Scand J Surg. 2015;104(4):260–6.
Kivimäki J, Pohjolainen T. Manipulation under anesthesia for frozen shoulder with and without steroid injection. Arch Phys Med Rehabil. 2001;82(9):1188–90.
Woods DA, Loganathan K. Recurrence of frozen shoulder after manipulation under anaesthetic (MUA): the results of repeating the MUA. Bone Jt J. 2017;99-b(6):812–7.
Nunez FA, Papadonikolakis A, Li Z. Arthroscopic release of adhesive capsulitis of the shoulder complicated with shoulder dislocation and brachial plexus injury. J Surg Orthop Adv. 2016;25(2):114–6.
Magnussen RA, Taylor DC. Glenoid fracture during manipulation under anesthesia for adhesive capsulitis: a case report. J Shoulder Elbow Surg. 2011;20(3):e23–6.
Loew M, Heichel TO, Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg. 2005;14(1):16–21.
Ding H, Tang Y, Xue Y, et al. A report on the prevalence of depression and anxiety in patients with frozen shoulder and their relations to disease status. Psychol Health Med. 2014;19(6):730–7.
Acknowledgements
We thank all the participants of the study.
Funding
This study was supported by the National Natural Science Foundation of China (81973874; 81373665), the Summit Plateau Team Project in Traumatology of Shanghai University of TCM, Shanghai Chronic Musculoskeletal Disease Clinical Medical Research Center (20mc1920600), Shanghai clinical specialty “traditional Chinese medicine orthopaedic traumatology” (shslczdzk03901), Clinical study of traditional Chinese manipulation in the treatment of the Frozen Shoulder Syndrome (22Y21920200). Shuguang hospital affiliated to Shanghai university of Traditional Chinese Medicine fund the journal’s rapid service fees.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Qinguang Xu, Huihui Li, Ding Jiang and Jian Pang. The first draft of the manuscript was written by Qinguang Xu. The draft was edited by Bo Chen. Lin Wang, Yan Chen, Yuyun Wu, Daofang Ding, and **ang Wang, and Yuelong Cao commented on previous versions of the manuscript. All authors reviewed and approved the final manuscript.
Disclosures
Qinguang Xu, Huihui Li, Ding Jiang, Lin Wang, Yan Chen, Yuyun Wu, Daofang Ding, Jian Pang, Bo Chen, Yuxin Zheng, Hongsheng Zhan, **ang Wang, and Yuelong Cao declare that they have no competing interests.
Compliance with Ethics Guidelines
The Ethics Committee of Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine approved the study (ChiECRCT20200121), and informed consent was obtained from all participants. The trial was conducted following the Declaration of Helsinki.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xu, Q., Li, H., Jiang, D. et al. The Effect of Manipulation Under Anesthesia for Secondary Frozen Shoulder: A Randomized Controlled Trial. Pain Ther 11, 1373–1387 (2022). https://doi.org/10.1007/s40122-022-00438-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00438-1