Abstract
Every day our sensory systems perceive and integrate a variety of stimuli containing information vital for our survival. Pain acts as a protective warning system, eliciting a response to remove harmful stimuli; it may also be a symptom of an illness or present as a disease itself. There is a growing need for additional pain-relieving therapies involving the multisensory integration of smell and taste in pain modulation, an approach that may provide new strategies for the treatment and management of pain. While pain, smell, and taste share common features and are strongly linked to emotion and cognition, their interaction has been poorly explored. In this review, we provide an overview of the literature on pain modulation by olfactory and gustatory substances. It includes adult human studies investigating measures of pain threshold, tolerance, intensity, and/or unpleasantness. Due to the limited number of studies currently available, we have structured this review as a narrative in which we comment on experimentally induced and clinical pain separately on pain–smell and pain–taste interaction. Inconsistent study findings notwithstanding, pain, smell, and taste seem to interact at both the behavioral and the neural levels. Pain intensity and unpleasantness seem to be affected more by olfactory substances, whereas pain threshold and tolerance are influenced by gustatory substances. Few pilot studies to date have investigated these effects in clinical populations. While the current results are promising for the future, more evidence is needed to elucidate the link between the chemical senses and pain. Doing so has the potential to improve and develop novel options for pain treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a need for alternative pain treatments that do not involve the use of analgesic drugs. |
Research in the last few decades hints at smell and taste as possibilities for pain modulation. |
This review provides an overview of the literature on the multisensory integration of pain, smell, and taste in adults. |
Under conditions of experimentally induced pain, smell and taste substances seem to have an effect on pain, while results obtained under clinical conditions can only be considered preliminary. |
More evidence is needed to highlight the link between pain, smell, and taste to improve complementary pain-relieving therapies. |
Digital Features
This article is published with digital features, including a summary slide to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13953392.
Introduction
Pain, smell, and taste are phylogenetically archaic perceptual systems that have played a central role in our evolutionary history for survival [1,2,3]. Pain is a protective mechanism that elicits a response to remove harmful stimuli [4], while smell and taste provide us with meaningful information about food sources in the environment. While smell helps us process environmental cues, including danger and social stimuli [5], taste is more differentiated in function: sour and salty tastes signal changes in the body’s pH level and mineral balance; sweet and umami (savoriness) tastes indicate sources of energy, while a bitter taste serves as a defense, alerting us against potentially toxic food and poisons [6].
By definition, pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage [7], occurring in either acute or chronic form. Acute pain is the awareness of noxious signaling from recently damaged tissue, while chronic pain lasts or recurs for more than 3 months [8]. Pain may present as a disease in itself or as a symptom of an underlying condition. Pain can be induced experimentally and influenced by numerous factors, such as biological features, other senses, previous experiences, fears, beliefs, lifestyles, and affective and cognitive processes [9,10,11].
Although the neural underpinnings of pain processing have not yet been completely identified, painful sensations arise from a complex network of areas in the brain: mainly the primary and secondary somatosensory cortices (S1 and S2, respectively), the insula, and the anterior cingulate cortex (ACC). These pain-related neural areas are commonly referred to as the pain matrix, although it has been shown that within this network diverse salient stimuli are processed [12]. In general, pain is described as a multidimensional concept. Two different pathways carry nociceptive information to the brain: the anterolateral spinothalamic (connected to the somatosensory cortex and the lateral thalamus, parietal operculum, and insula) and the medial spinoreticulothalamic pathway (connected to the insula, amygdala, hippocampus, S2, parabrachial nucleus, locus caeruleus, periaqueductal gray substance, intra-laminar and medial thalamic nuclei, thalamic ventral caudal parvocellular nucleus, and ventral caudal portae) [4, 13]. The lateral pathway conveys sensory-discriminative pain features to the S1 and the S2, while the medial pathway conveys affective-motivational pain features to the insula and the ACC [14, 15]. The former refers to the spatial, temporal, and qualitative (intensity) characteristics of pain, while the latter evokes unpleasantness and triggers a protective response, thereby highlighting the complex nature of pain [4, 16]. These two dimensions (the sensory-discriminative and the affective-motivational) form the bases of pain’s dual nature, and thus the objectivity of pain cannot be separated from a person’s own interpretation: they are always integrated in a person’s evaluation of pain.
Likewise, odors and tastes are often associated and combined to create flavors [17, 18]; both are closely linked to emotion and cognition [19, 20]. In the human brain, olfactory stimuli received by the olfactory bulb and without a thalamic relay are centrally processed in the piriform cortex, the amygdala, and the orbitofrontal cortex [21, 22]. Gustatory stimuli, relayed by the thalamus, are processed in the insula, the operculum, and the orbitofrontal cortex [23, 24].
There is growing evidence for common neural correlates between pain and chemical senses in the ACC, the amygdala, and the orbitofrontal cortex, three areas implicated in the reward system and motivational behavior in addition to their involvement in pain perception and emotional processing [25,26,27,28,29]. For these reasons, and given that our everyday life is deeply immersed in a stimuli-rich environment that we perceive altogether [30], painful, olfactory, and gustatory stimuli interact on several levels and modulate each other.
Studies carried out in the last two decades have investigated the relationship between diverse olfactory–gustatory stimuli and pain perception and the mechanisms underlying these effects. This interaction is, however, not well documented. In this review, we provide a comprehensive description of studies that have investigated the modulation of pain through the use of smell and taste substances, with different paradigms, under both experimental and pathological pain conditions, and of studies on painful clinical procedures in adults.
Methods
A literature search of the PubMed and Scopus electronic databases was performed independently by three of the authors (AS, AZ, RN). An advanced search in PubMed used the terms (“Pain” [MeSH] OR “Pain perception” [MeSH] OR “Analgesia” [MeSH]) AND (“Smell” [MeSH]) OR “Odorants” [MeSH] OR (“Taste” [MeSH]) OR (“Taste perception” [MeSH]); in Scopus, the advanced search used the terms (“Pain” OR “Analgesia” OR “Pain perception”) AND (“Smell” OR “Odorants” OR “Odors”) OR (“Taste” OR “Taste perception”). The search was limited to articles published up to 20 August 2020. The titles and abstracts were screened against the following predefined inclusion criteria: (1) papers published in English; (2) experimental studies in adult humans (psychophysical, neurophysiological, and neuroimaging; either clinical populations or healthy volunteers); and (3) investigation of pain measures (threshold, tolerance, intensity, or unpleasantness). Full-text articles were screened for eligibility.
This review is based on previously conducted studies and does not contain any new studies performed by any of the authors and involving human participants or animals.
Results
A total of 2404 potentially relevant articles were retrieved in the primary literature search, of which 2373 were excluded because they did not meet the inclusion criteria based on title/abstract screening (Fig. 1). The full text of the remaining studies was read, and ultimately 30 studies were included in this review (Tables 1, 2) [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. A narrative review was chosen due to differences in study methodologies that made comparison across studies difficult. For example, studies varied by population studied (clinical populations, healthy adults), outcome measures (studies often investigated only one or two pain measures), and methodology to induce pain in healthy population experiments. Prior to reviewing the literature, we briefly describe the methods that were used to induce experimental pain, stimulate the olfactory and gustatory senses, and measure the outcome, with the aim to guide readers in understanding the varied methodologies used in current research. The results for experimentally induced and clinical pain are summarized by pain–smell and pain–taste interactions separately. We discuss the results in relation to related papers and direct the reader to reviews that support interactions of the sort. To conclude, we summarize the state of the art and highlight the limits and gaps that need to be filled by future research in this field.

Adapted from Moher et al. [31]
PRISMA flowchart of the study
Experimental Pain: How to Induce and Measure Pain
Pain can be experimentally elicited by applying physical, chemical, mechanical, and thermal stimuli. Hot or cold water induces a painful sensation lasting several seconds to a few minutes. The temperature for hot thermal stimulation is usually set at 45–50 °C, then adjusted to a participant’s sensitivity [32]. In experimental settings of cold water stimulation, namely, the cold pressor test (CPT) or its variant (ice), the water temperature is usually set at 0–10 °C [36, 38, 50,51,52,53,54,55,56, 61]. Heat and electrical stimuli can also be applied to induce pain. Heat stimuli are delivered by a contact thermode stimulator attached directly to the skin [33, 34, 39, 58]. Electrical stimuli are delivered by electrodes connected to an electrophysiological amplifier and stimulator (digitimer or digital stimulator) [42, 43, 46]. In both cases, the stimuli can be delivered in a single pulse or a train of consecutive pulses. A physical test which induces pain is the submaximal effort tourniquet test [62] which induces ischemic pain. In this test, a subject raises his arm above the heart, and circulation is occluded with a blood pressure cuff; after lowering his arm, the subject performs hand-grip exercises [34]. In another type of physical test, a grade pressure algometer is used to induce pressure or mechanical pain by gradually increasing compressive force at a constant rate of grams per second [34, 35, 49, 61]. Hypertonic saline can also be injected to elicit muscle pain into the deep masseter muscle [58]. Exposure to capsaicin is a chemical method used to induce pain. Capsaicin, a natural component of chili peppers, produces a chemesthetic burning sensation that stimulates a subset of polymodal C and Aδ nociceptive fibers [63], mimicking symptoms observed in chronic neuropathic pain [64]. Capsaicin can generate both peripheral and central hypersensitivity, as well as activate pain-sensing afferents and induce central sensitization. It is used as a pain model of excitatory and inhibitory effects in animals and humans [65,66,67]. Finally, many odorants can stimulate the trigeminal nerve, triggering diverse sensations as burning, cooling, and stinging pain [68].
Pain measures can be recorded and categorized either quantitatively (use of a device to measure units in a discrete system, such as temperature or time) or qualitatively (asking participants to rate their subjective experience). This distinction between quantitative and qualitative measures serves to simplify the experimental results. A quantitative measurement can be used to assess the pain threshold and tolerance to pain. The pain threshold refers to the intensity of the stimulation at which a subject reports a change in sensation from painless to slightly painful that identifies the sensory-discriminative component of pain. In contrast, pain tolerance refers to the intensity of stimulation at which a subject reports an intolerable painful sensation that identifies the affective-cognitive component of pain [69]. Qualitative measures are based on a participant’s subjective rating on a visual (VAS) or a numerical scale (NRS) of pain intensity (the sensory-discriminative dimension) and unpleasantness (the affective dimension) [70].
Olfactory-Gustatory Stimulation in Pain Experiments
Chemosensory stimulation can be delivered by various methods. There is an ample body of literature available on the administration of smell and taste substances (e.g., functional magnetic resonance imaging [fMRI], olfactory/gustatory event-related potentials). One of the most commonly used devices to deliver odors is the olfactometer: subjects inhale odors through a nasal canula inserted in the nose [33, 37, 39, 41, 42, 46, 48]. When substances are delivered via a diffuser or humidifier in the testing room [34, 36, 40], participants are not always aware of the stimulation. Another way to deliver stimuli is by placing essences on cotton balls/pads [32, 38, 44, 45] or on litmus strips [43] or by diluting them in a solvent [33, 37, 39, 42] kept in airtight bottles or fastened inside an air-permeable mask. Finally, a pen-like odor-dispensing device can be used, which works with a tampon imbibed with a liquid odorant or an odorant substance dissolved in a solution [47]. In gustatory stimulation, subjects are asked to ingest or to retain either something solid [49, 55, 58, 61] or a liquid substance in their mouth [50,51,52,53,54, 56, 59, 60] after drinking from a cup or exposure to a liquid spray [46, 48].
Subjects are asked to evaluate smell and taste substances by indicating on a scale (VAS, NRS) how much they liked (or disliked) a substance or their mood perception after olfactory stimulation. This can be done in a pilot study phase to select a preferred/disliked substance for each participant (for example [32, 33]) or to choose the substances or the optimal concentration in experiments later involving a different pool of participants [36, 38, 40]. Alternatively, evaluation may take place after a substance is administered to determine whether it was perceived as intended [43, 46, 48].
Researchers have often been found to fail to check study participants’ perceptual status of smell and taste. Few studies have reported that subjects had been screened with either validated tests [43, 46,47,48, 57] or an experimental paradigm devised to detect gross dysfunction in their perception of the stimuli [33, 39, 42]. Some studies simply asked subjects to self-report their history of smell or taste dysfunction that would exclude them from participation [36, 53, 54] or assessed the sense of smell with alcohol swabs [44].
Interplay Between Smell and Experimental Pain
Research on the smell–pain interaction in healthy adults has used a variety of methodologies and odors, making it difficult to compare findings across studies. Most studies to date were focused on qualitative pain measures (intensity and unpleasantness), while only a few explored the pain threshold and/or pain tolerance. Reporting of qualitative pain measures of pain intensity has sometimes been inconsistent. For example, pain intensity was reportedly not modified by odors in studies in which pain was induced by hot or cold thermal stimulation [33, 38, 39] or with capsaicin cream applied to the back of the right hand at the level of the first dorsal interosseous muscle [48] or with phasic nicotine stimuli to induce burning and stinging pain [41]. One study applied three different modes of stimulation (thermode, pressure algometer, ischemic) and reported reduced pain intensity associated with essential oil of lavender only in men [34]. Another study reported a reduction in pain intensity following thermal stimulation of around 46–48 °C only in women when the most pleasant odor selected for each participant was delivered [32]. Pain intensity was reported to be increased with the delivery of an unpleasant odor of machine oil (selected in a pilot study) at the CPT [36], while other studies, by means of electrical stimuli, reported that pain intensity decreased and increased with the delivery of pleasant (vanillin) and unpleasant (N-valeric acid) odors, respectively [42], and decreased with lavender oil [43]. More recently, these findings were confirmed in a study applying electrical stimulation and delivering the pleasant odor (banana), whereas no effect was found for the unpleasant odor (fish) [46].
Studies have reported convergent results for the effect of odors on modulating pain unpleasantness: pain unpleasantness evoked by painful stimuli was reduced by pleasant odors and/or increased by unpleasant odors [32, 34, 43, 46, 48]. These observations are shared by Villemure and collaborators [33, 39], who reported a strong connection between pain response and subjects’ mood. These authors showed that the pleasant odor induced a positive mood and decreased pain-related activity within the ACC, the medial thalamus, the S1, and the S2 [39].
Two studies in quantitative pain assessment reported that the pain threshold for electrical, thermode, pressure algometer and ischemic stimulation was not modified by odors [34, 46]. Only one study found that mechanical painful stimulation was modified at the pain threshold by a “green” odor, but information on the number of subjects tested and the experimental design were not available [35]. In contrast, pain tolerance was significantly longer in the sweet-smelling condition at the CPT [38], but not with the use of other painful stimuli (electrical, thermode, pressure algometer stimulation, ischemic procedure) [34, 46].
Interplay Between Taste and Experimental Pain
The majority of studies that have investigated the pain–taste interaction to date induced pain with the CPT and administered sweet substances. Several focused on pain threshold and tolerance, while a few evaluated the qualitative measures of pain. Pain threshold at the CPT was found to be increased in adult males when the subjects held sugar diluted in water or sugar tablets in their mouth [53, 55, 56, 59]. The pain threshold was also increased by spicy and sweet stimulation at the CPT and the pressure algometer [61]. Other studies found no effect of sugar preparations on the pain threshold as measured with the CPT [50, 51] or with a pressure algometer and sweet soft drinks and palatable food [49]. Bitter and sweet tastes were found to have no effect on the pain threshold measured with thermal stimulation [58]. Recent studies using electrical stimulation have reported no change in the pain threshold after the administration of sweet and bitter substances [46]; similarly, no change in pain threshold was recorded after heat thermal stimulation and the administration of sweet substances [60].
Pain tolerance was found to be increased by sugar at the CPT [50, 54, 59], also when the algometer pressure test was used together with the administration of palatable food−but only in women [49]. Nevertheless, no effect on pain tolerance was found at the CPT or after applying either electrical or thermal stimulation [46, 51, 53, 56, 58].
None of the studies investigating the qualitative measures of pain reported an effect of taste on pain intensity [46, 48,49,50, 52,53,54, 56, 58, 60]. Furthermore, pain unpleasantness was not influenced by taste as measured with a pressure algometer [49], the CPT [50,51,52] or application of a capsaicin cream [48]. In one study evaluating phasic pain evoked by brief electrical skin stimuli, pain unpleasantness was reduced with the administration of a sucrose solution [46].
Only one study in healthy adults explored the interaction between pain and taste at the central level. Pain-related neural networks (e.g., ACC, insula, posterior parietal cortex, thalamus) can be activated by the CPT, and this activation was found to be reduced in the sweet taste condition [55].
The Influence of Smell and Taste in Pain in Pathological Conditions
A major area of health care concerns illness-related pain, and many diseases are the causes of pain (e.g., cancer, neurological and dental disease). The pharmaceutical industry is a major driver of research on and the development of analgesic drugs, concomitant with the search for new and alternative treatments [9, 71]. Moreover, complementary treatments are needed to make routine painful healthcare procedures more sustainable. Few studies to date have directly investigated the effect of smell and taste on the modulation of pain.
Smell and Pain
Certain types of odors encountered in daily life can exacerbate neuropathic pain, as noted in a patient with neuropathic pain secondary to cervical myelopathy of unclear origin, most often affecting the right hand, wrist, and elbow but also the hip and spine [37]. When tested with unpleasant and pleasant odors, the patient rated pain intensity and unpleasantness according to the valence of the odors. Moreover, evidence from fMRI revealed increased activation in pain processing areas (e.g., thalamus, amygdala, insular cortex, ACC) when the patient was exposed to an unpleasant odor.
In a recent study, a 4-week olfactory training program was evaluated in patients with chronic low back pain [47]. Post-training results showed a higher pain threshold during electrical cutaneous stimulation, suggesting that olfactory training might be useful in desensitizing pain perception circuits.
The pain intensity of patients attending dental clinics was found not to be affected by orange and apple odors [40]. Pain intensity was however decreased after needle insertion in patients with end-stage chronic renal failure [44] and in pregnant women in labor [45], both with the use of essential lavender oil.
Taste and Pain
Only one study has directly explored pain modulation through taste: lower pain intensity scores immediately after sucralose administration were recorded in three patients with burning mouth syndrome (BMS) [57].
Discussion
Pain–Smell Interaction
Findings of a pain–smell interaction in experimental pain models underline the effect of odors on the qualitative measures of pain [32,33,34, 36, 39, 42, 43, 46, 48]. There is growing body of evidence supporting the neurobiological role of olfaction. Olfaction has been linked to depression [72] and odor sensitivity has been associated with personality traits [73], indicating a strong connection to the affective domain. Olfactory substances are known to exert beneficial effects on physiological and psychological processes in animals and humans alike [74,75,76].
On one study, chemical stimuli was found to activate the olfactory and the trigeminal system [41]. In the same study, although nicotine burning and stinging painful sensations were not altered by menthol, a nicotine effect on menthol concentrations was noted, with the highest nicotine concentration eliminating participants’ ability to discriminate the menthol concentrations for odor intensity and cooling [41]. Moreover, carbon dioxide (CO2) can elicit trigeminal painful perception: subjects with a higher sensitivity to CO2 pain thresholds (women and older participants) were found to score better in odor identification [68]. Exposure to various intensities of these stimuli demonstrated the primary role of the S2 and the piriform cortex in coding subjectively perceived intensity of intranasal trigeminal stimuli [77] and how trigeminal and smell painful sensations can interact at the peripheral and the central level, suggesting a strong connection between the senses. These observations are in agreement with imaging findings that showed decreasing pain-related activity within the ACC, the medial thalamus, the S1, and the S2 after the administration of a pleasant odor [39]. Taken together, the results suggest an effective modulatory role for odors in nociception, especially the effect of smell on the affective dimension of pain.
Studies on quantitative measures of pain and smell are few and the results are inconsistent [34, 35, 38, 46]. While only two studies have reported an effect of smell on pain threshold and pain tolerance, respectively [35, 38], an effect of pleasant and unpleasant odors on the magnitude of the nociceptive withdrawal reflex (NWR) was reported in another study [42]. The NWR is the electromyographical (EMG) response recorded in the biceps femoris at 80–150 ms (RIII) after electrical stimulation of the sural nerve corresponding to a nociceptive reflex [69]. Bartolo and collaborators [42] found the reflex magnitude to be reduced by the pleasant odor and increased by the unpleasant odor during constant electrical stimulation at a fixed intensity. To our knowledge, these are the only findings for an effect of odors on a defense response mediated by acute spinal nociception in humans. More research using quantitative measures is needed to clarify the regulatory role of olfaction.
In summary, the few human studies conducted to date in this area indicate that the pain threshold and pain tolerance for most types of painful stimulation are not significantly modified by odors. However, odors do seem to influence the qualitative measures of pain in response to a variety of painful stimuli. Mostly, pleasant odors reduce pain unpleasantness while unpleasant odors increase it. This difference may be related to mood and activation of the ACC, the medial thalamus, and the somatosensory cortices.
Pain–Taste Interaction
The results of experimental studies on pain threshold and tolerance in pain–taste interaction are inconsistent, although the majority of studies reported at least an effect on one of those measures [49, 50, 52,53,54,55,56, 59, 61]. Some studies reported a gender effect, with an effect of taste on the pain threshold and/or pain tolerance in men [53,54,55,56, 59] but no effect on the pain threshold in women [49, 51, 60]. One study explored gender differences by means of the CPT and found an effect of sweet substances on the pain threshold but not on pain tolerance [56]. This observation is partially shared by another study that reported an effect of the nociceptive flexion reflex [78]. Despite the small sample size of this latter study, the analgesic effect of sucrose after electrical stimulation was found to be shorter in women (< 10 min) but longer in men (up to 15–20 min) [78]. An effect on pain tolerance with palatable food among the women was found using the algometer pressure test [49]. More research is needed to better explore these gender-related differences.
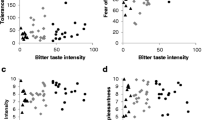
No effect on pain intensity has been found after taste stimulation [46, 48,49,50, 52,53,54, 56, 58, 60], but a positive correlation was found between pain intensity and intensity of bitter taste perception, as elicited by the CPT and the PROP (6-n-propythiouracil) papers test: the subjects who perceived the more intense pain perceived the bitter taste as more intense [79].
To date, nearly all studies exploring experimental pain–taste interaction used sweet substances. A few administered a quinine hydrochloride solution to induce a bitter taste but no effect on the pain measurement was elicited [46, 48, 50, 58]. The question of whether bitter substances tend to increase pain perception (like an unpleasant smell does) remains unanswered.
Taste is involved in the oral perception of food and derived chemicals, which allows us to recognize potentially harmful and healthy foods [80]. Taste anatomy is complex: cranial nerve (CN) VII, CN IX, and CN X carry gustatory information, each from a specific area [81]. The five common tastes (sweet, salty, sour, bitter, umami) are usually perceived in combination with one another while eating food. We experience a complex sensation from smell plus taste (flavor) and activation of the trigeminal and glossopharyngeal nerves (i.e., chemesthesis), which in turn generates pungency or irritation [18, 82]. Chemesthesis and painful sensations are merged and mediated by transient receptor potential (TRP) channels that detect visceral pain and taste, highlighting the role they play in sensory nervous systems and their wide range of sensory capacities [83, 84].
A subset of gustatory fibers can be stimulated by capsaicin in the mouth: lower capsaicin concentrations have been identified in adults as a basic taste, especially bitter [85]. In one study, the burning sensation elicited by capsaicin was misidentified as bitter taste on a discrimination task, with the subjects identifying bitter and capsaicin as perceptually similar on a similarity/dissimilarity scale compared to other basic tastes [86]. This qualitative similarity between bitter taste and capsaicin suggests a common function as sensory signals of potentially harmful stimuli of these two sensations. Capsaicin can also be used as a prototypical stimulus to induce pain in the oral cavity, where it induces a burning and painful sensation that activates both taste and trigeminal nerve fibers. Sucrose can reduce the burning sensation in the mouth induced by the oral application of capsaicin in healthy subjects [87]. Similarly, other compounds, such as menthol, seem to exert an analgesic countereffect on capsaicin [88] and on the irritant intensity of nicotine [89]. In contrast, a spicy stimulation can increase the pain threshold at the CPT and pressure pain, appearing to have analgesic effects similar to sweet stimulation [61]. These results reveal how trigeminal pain and taste sensations interact with different modalities at the peripheral level.
Another limitation in the pain–taste interaction is that almost all studies administered sucrose and induced pain with the CPT. Differences in the procedures may explain differences in the results: the temperature at which the CPT was conducted (range 0–2 °C to 10 °C) or the experimental design (some experiments performed on different days, others all in one session). Only a few studies used different methods [46, 48, 49, 58, 60, 61].
A future area of focus would be to test other basic tastes besides sweetness and a variety of palatable foods, as was done by two studies [49, 61], which is well documented in rats [90,91,92]. Food is a strong reward: in one study, substances (palatable food) similar to others that modulate pain tolerance [49] were used to investigate the enjoyment, pleasantness, and taste intensity of food after the presence or absence of a painful situation (i.e., CPT) [93]. The authors reported that the palatable food was rated as more enjoyable and more intense and that the flavors were named quicker after the pain condition [93]. The relationship between pain and taste seems to be bidirectional: not only can taste affect a painful experience but nociceptive sensations can impact on taste perception.
Finally, one study reported that the sweet taste condition reduced pain-related neural networks (e.g., ACC, insula, posterior parietal cortex, thalamus) activated by the CPT [55]. This network partly overlaps with situations of induced pain and smell in healthy subjects [39]. The brain areas modulated by olfactants were the ACC, the medial thalamus, the S1, and the S2. More research into these networks is needed. Studies on the role of the ACC in the interaction between pain, smell, and taste have postulated the central involvement of this area in emotional processing and pain perception [27, 42]. The role of the thalamus has not yet been elucidated although recent evidence suggests that it may be involved in mental integration and regulation and not just function as a point of relay [94].
Taken together, these findings underline that common substrates may influence the integration of inputs from different sensory systems. However, the results of the studies conducted to date are often contradictory and less robust than those from studies exploring the link between pain and smell. The pain threshold and tolerance for painful stimuli are modulated by taste substances, but pain intensity is not. No firm conclusion can be drawn on pain unpleasantness because of the paucity of studies exploring this measure of the affective component of pain.
Interaction Pain–Smell in Pathological Conditions
It is notoriously difficult to treat pain in the context of an illness. However, using experimental pain models, researchers can simulate clinical conditions and investigate pain in a meaningful context. There is mounting evidence supporting a modulatory effect of smell and taste on pain in healthy subjects, laying the basis for research into pain conditions.
The few published studies that have explored the interaction between pain and smell in clinical conditions can be considered to be preliminary, although the neuroimaging findings in one patient (increased activation of thalamus, amygdala, insular cortex, ACC with unpleasant odor) [37] highlight the existence of common neural areas shared by pain and chemical sensation [26,27,28,29, 42]. These results are consistent with those found in healthy subjects (both behavioral and with fMRI) [33, 39], with the exception that the related activated network involved the ACC, the medial thalamus, the S1, and the S2 [39]. This difference in activation pattern may have been due to the kind of pain and the odors administered. Specifically, the patient was tested with pyridine (unpleasant and known to increase pain) and aquaflore (evoking little or no change in pain perception), while the healthy subjects were tested with the odors they liked or disliked most. Neuroimaging studies are needed to corroborate these results, although the chronic use of analgesics can lead to reduced perception of intranasal trigeminal stimuli and olfactory function [95], again suggesting multisensory interaction at the central level. Abnormalities of the limbic system have also been suggested, involving olfactory and pain processing, by a study investigating odor identification and pain-related somatosensory-evoked potentials (SEPs) electrically stimulated on the faces of patients with Parkinson’s disease (PD) [96]. A positive correlation was found between the amplitude of the SEPs and smell identification scores (the higher the olfactory score, the greater the pain-related SEP amplitude).
The pilot study reporting a change in pain threshold after olfactory training [47] adds to the evidence from a previous clinical case report on chronic pain in a woman with a 10-year history of burning pain in both feet and abdominal pain attacks and odor hypersensitivity who experienced short-term pain relief after continuous odor exposure training [97]. Genetic analysis revealed a mutation within the SCN9A gene encoding voltage-gated sodium channel [Na(v)1.7] with gain-of-function in olfactory and pain sensation. Loss of function of the channel altered pain perception and olfaction acuity [98], demonstrating a strong neurobiological link between pain and smell. Studies have reported a congenital inability to experience pain accompanied by anosmia in mice and humans [99,100,101], and lower responsiveness to CO2 pain stimuli in patients with olfactory loss [68].
In three other studies, apple and orange odors [40] were used in one and lavender oil was applied in two [44, 45]. An effect on pain intensity was reported only by the studies that applied lavender oil [44, 45]. Widely applied in aromatherapy, lavender oil can reduce migraine headache severity [102]. In one case report, migraine attacks triggered by the smell of onions and garlic were relieved by inhalation of peppermint oil [103]. Odors are known to trigger migraine attacks; studies have found atrophy of the olfactory bulb in migraine patients [104] and increased activity in response to olfactory stimulation in the brain areas (piriform, insular and orbitofrontal cortices, amygdala, hippocampus) [105] that process pain and chemical sensation, showing, once again, a link at the neural level.
There are contradictory results for aromatherapy by inhalation (e.g., do they provide relief and comfort and reduce stress?) although an extensive body of research exists on clinical procedural pain in infants and its relation with smell [106,107,108,109,110]. Aromatherapy may therefore have an effect on pain intensity modulation and be a useful treatment in clinical practice. Taken together and in line with results from healthy subjects, these clinical findings highlight behavioral and neural interactions between pain and smell. Odors can alter pain perception, with a differential effect on pain-related areas involved in processing the emotional aspects of pain. The inhalation of essential oils may be a useful means to manage pain when combined with conventional treatments. These recent findings hold promise for the use of odors in pain management [47], although more research is needed.
Interaction Pain–Taste in Pathological Conditions
The interaction between pain and taste sensation in adults has been little studied to date, with only one study reporting on pain–taste interaction in clinical conditions; although preliminary, the findings are of interest [57]. BMS is an unusual idiopathic condition in which pain and taste disturbances are often linked. The oral pain is not caused by a clinically evident lesion (International Classification of Headache Disorders, 3rd edition, 2018; https://ichd-3.org/wp-content/uploads/2018/01/The-International-Classification-of-Headache-Disorders-3rd-Edition-2018.pdf). Frequent complaints are taste disturbances, particularly bitter or metallic phantom tastes, and dysgeusia [111,112,113,114,115]. Various study results hint at peripheral dysfunction [111, 113,114,115,116,117], whereas other findings account for changes in the pain matrix, suggesting a deficit in the central organization of pain [118].
An interaction between taste and pain perception may arise from injury to the nerves carrying gustatory information. Damage to the facial nerve (CN VII) at the chorda tympani can cause abnormal pain and taste sensation, often occurring together [119]. The chorda tympani nerve is an important branch of the facial nerve; it conveys gustatory information from the anterior two-thirds of the tongue, and together with the lingual branch of the trigeminal nerve (CN V) it transmits lingual somatosensory signals (e.g., pain, temperature, touch) [120]. Patients with nerve damage report that a sour or bitter taste can cause unbearable pain and an oral phantom (metallic, bitter, salty) sensation: the greater the taste loss, the greater the pain experienced, including extra-oral pain [119]. Also, unilateral damage to a single chorda tympani nerve can increase contralateral non-taste oral sensation, including oral burning produced by capsaicin [87]. There is evidence for intertalk between the chorda tympani (CN VII) and the trigeminus (CN V) [121, 122]. In addition, a central interaction was found in patients with chronic back pain who were more sensitive to detecting citric acid solutions and rated bitter and salty solutions more intense than healthy controls [27].
As per the pain–smell interaction, a consistent line of research exists in children and taste during painful procedures [123,124,125,126,127,128]. Summarizing, these findings point towards an interaction between pain and taste during clinical procedures, at least at the peripheral level, which need to be largely explored in adults.
Conclusion
The main findings of this review are that odors may alter the qualitative components of pain, especially pain unpleasantness, as shown by the higher scores for unpleasant odors and the lower scores for pleasant odors. This effect has been consistently reported in healthy subjects [32,33,34, 36, 39, 42, 43, 46, 48], and the results in pain management are promising [37]. Very recent preliminary results show a considerably higher pain threshold in persons with chronic low back pain after olfactory training and the benefit of regular use of odors as an adjunct in pain management [47]. Consistent with this approach, aromatherapy is beginning to gain a place in the complementary management of clinical pain [44, 45]. These findings are supported by neuroimaging studies that show the involvement of a network of brain areas related to the affective dimension of pain (e.g., ACC and thalamus) [37, 39]. Such results are to be considered preliminary, given the absence of a control condition versus substance administration and the fact that in the clinical pain experiment only a single patient was tested.
In comparison, research results are few and less consistent for taste. In experimental pain models, sweet substances appear to modulate the quantitative measures of pain [49, 50, 52,53,54,55,56, 59, 61] while qualitative measures documented no effect on pain in healthy adults, with the exception of one study that reported lower ratings of pain unpleasantness with a sweet substance in comparison with a bitter one [46]. Sucralose has been shown to modulate pain intensity in the context of pain in illness [57], although this was a pilot study involving only three patients. Future studies will need to better assess the effect of taste substances in experiments on populations subject to induced pain and clinical pain, with the inclusion of other basic tastes and more complex substances to gain a more comprehensive understanding of such interactions. The modulation of pain by a sweet taste seems to involve the ACC, the thalamus, and other brain areas in healthy adults [55]. This type of evidence needs to be confirmed by functional imaging studies and also in comparative studies with olfactory substances to identify the common neural areas shared by pain, smell, and taste. Finally, potential gender-related differences should be explored, taking into account that the findings in studies on the pain–taste interaction reveal an effect on pain threshold in men [56] and on pain tolerance in women [49], and the lack of studies investigating the pain–smell interaction. Summarizing, pain, smell, and taste seem to interact at both the peripheral and the central level, but additional evidence is needed to fill the present knowledge gaps. The use of different methodologies can extend the results to different pain experiences, but better high-quality procedures will be needed for future research. While we do not suggest the use of complementary therapy to analgesics, the research lines reviewed here open new avenues in pain management and improved quality of life of patients with pain. Just as smell and taste are rarely experienced separately but rather together as flavors, so, too, pain is often a much more complex emotional experience in real life.
Current Limitations and Future Perspectives
The main limitation in this field is that few pilot studies have investigated the effect of odor and taste on clinical populations with different types of pain. The results presented here provide a basis for future studies to elucidate the link between the chemical senses and pain. Multicenter studies applying the same experimental paradigm to larger samples of patients with different pain conditions could lead to the discovery of novel options to pain treatment.
References
Elwood RW. Pain and suffering in invertebrates? ILAR J. 2011;52(2):175–84.
Krieger J, Breer H. Olfactory reception in invertebrates. Science. 1999;286(5440):720–3.
Yarmolinsky DA, Zuker CS, Ryba NJP. Common sense about taste: from mammals to insects. Cell. 2009;139(2):234–44.
Talbot K, Madden VJ, Jones SL, Moseley GL. The sensory and affective components of pain: are they differentially modifiable dimensions or inseparable aspects of a unitary experience? A systematic review. Br J Anaesth. 2019;123(2):e263–72.
Stevenson RJ. An initial evaluation of the functions of human olfaction. Chem Senses. 2010;35(1):3–20.
Beauchamp GK. Why do we like sweet taste: a bitter tale? Physiol Behav. 2016;164(Part B):432–7.
Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–82.
Saastamoinen P, Leino-Arjas P, Laaksonen M, Lahelma E. Socio-economic differences in the prevalence of acute, chronic and disabling chronic pain among ageing employees. Pain. 2005;114(3):364–71.
Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron. 2007;55:377–91.
Wachholtz AB, Pearce MJ, Koenig H. Exploring the relationship between spirituality, co**, and pain. J Behav Med. 2007;30:311–8.
Wager TD, Atlas LY. How is pain influenced by cognition? Neuroimaging weighs. Perspect Psychol Sci. 2013;8(1):91–7.
Iannetti GD, Mouraux A. From the neuromatrix to the pain matrix (and back). Exp Brain Res. 2010;205:1–12.
Fil A, Cano-de-la-Cuerda R, Muñoz-Hellín E, Vela L, Ramiro-González M, Fernández-de-las-Peñas C. Pain in Parkinson disease: a review of the literature. Parkinsonism Relat Disord. 2013;3:285–94.
Albe-Fessar D, Berklet KJ, Kruger L, Ralston HJ III, Willis WD Jr. Diencephalic mechanisms of pain sensation. Brain Res Rev. 1985;9(3):217–96.
Avenanti A, Bueti D, Galati G, Aglioti SM. Transcranial magnetic stimulation highlights the sensorimotor side of empathy for pain. Nat Neurosci. 2005;8:955–60.
Price DD. Psychological and neural mechanisms of the affective dimension of pain. Science. 2000;288:1769–72.
Prescott J, Johnstone V, Francis J. Odor–taste interactions: effects of attentional strategies during exposure. Chem Senses. 2004;29(4):331–40.
Shepherd GM. Smell images and the flavor system in the human brain. Nature. 2006;444:316–21.
Phillips ML, Heining M. Neural correlates of emotion perception: from faces to taste. In: Rouby C, Schaal B, Dubois D, Gervais R, Holley A, editors. Olfaction, taste and cognition. Cambridge: Cambridge University Press; 2002. p. 196–208.
Krusemark EA, Novak LR, Gitelman DR, Li W. When the sense of smell meets emotion: anxiety-state-dependent olfactory processing and neural circuitry adaptation. J Neurosci. 2013;33(39):15324–32.
Gottfried JA. Smell: central nervous processing. Adv Otorhinolaryngol. 2006;63:44–69. https://doi.org/10.1159/000093750.
Lundström JN, Boesveldt S, Albrecht J. Central processing of the chemical senses: an overview. ACS Chem Neurosci. 2011;2:5–16.
Huart C, Collet S, Rombaux P. Chemosensory pathways: from periphery to cortex. B-ENT. 2009;5(S1):3–9.
Small DM. Taste representation in the human insula. Brain Struct Funct. 2010;214:551–61.
Lötsch J, Hähner A, Gossrau G, et al. Smell of pain: intersection of nociception and olfaction. Pain. 2016;157(10):2152–7.
Low LA, Fitzgerald M. Acute pain and a motivational pathway in adult rats: influence of early life pain experience. PLoS One. 2012;7(3):e34316.
Small DM, Apkarian AV. Increased taste intensity perception exhibited by patients with chronic back pain. Pain. 2006;120(1–2):124–30.
Todd AJ. Neuronal circuitry for pain processing in the dorsal horn. Nat Rev Neurosci. 2010;11:823–36.
Zald DH, Pardo JV. Emotion, olfaction, and the human amygdala: Amygdala activation during aversive olfactory stimulation. Proc Natl Acad Sci USA. 1997;94(8):4119–24.
Stein BE, Meredith MA. Multisensory integration. Neural and behavioural solutions for dealing with stimuli from different sensory modalities. Ann N Y Acad Sci. 1990;608(1):51–70.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Marchand S, Arsenault P. Odors modulate pain perception: a gender-specific effect. Physiol Behav. 2002;76:251–6.
Villemure C, Slotnick BM, Bushnell MC. Effects of odors on pain perception: deciphering the roles of emotion and attention. Pain. 2003;106:101–8.
Gedney JJ, Glover TL, Fillingim RB. Sensory and affective pain discrimination after inhalation of essential oils. Psychosom Med. 2004;66:599–606.
Aou S, Mizuno M, Matsunaga Y, Kubo K, Li X, Hatanaka A. Green odor reduces pain sensation and fatigue-like responses without affecting sensorimotor function. Chem Senses. 2005;30(Suppl 1):i262–3.
Martin GN. The effect of exposure to odor on the perception of pain. Psychosom Med. 2006;68:613–6.
Villemure C, Wassimi S, Bennett GJ, Shir Y, Bushnell MC. Unpleasant odors increase pain processing in a patient with neuropathic pain: Psychophysical and fMRI investigation. Pain. 2006;120:213–20.
Prescott J, Wilkie J. Pain tolerance selectively increased by a sweet-smelling odor. Psychol Sci. 2007;18(4):308–11.
Villemure C, Bushnell MC. Mood influences supraspinal pain processing separately from attention. J Neurosci. 2009;29(3):705–15.
Toet A, Smeets MAM, van Dijk E, Dijkstra D, van den Reijen L. Effects of pleasant ambient fragrances on dental fear: comparing apples and oranges. Chem Percept. 2010;3:18–189.
Renner B, Schreiber K. Olfactory and trigeminal interaction of menthol and nicotine in humans. Exp Brain Res. 2012;219:13–26.
Bartolo M, Serrao M, Gamgebeli Z, et al. Modulation of the human nociceptive flexion reflex by pleasant and unpleasant odors. Pain. 2013;154(10):2054–9.
Masaoka Y, Takayama M, Yajima H, Kawase A, Takakura N, Homma I. Analgesia is enhanced by providing information regarding good outcomes associated with an odor: placebo effects in aromatherapy? Evid Based Complement Altern Med. 2013;921802.
Bagheri-Nesami M, Espahbodi F, Nikkhah A, Shorofi SA, Charati JY. The effects of lavender aromatherapy on pain following needle insertion into a fistula in hemodialysis patients. Complement Ther Clin Pract. 2014;20:1–4.
Kaviani M, Azima S, Alavi N, Tabaei MH. The effect of lavender aromatherapy on pain perception and intrapartum outome in primiparous women. Br J Midwifery. 2014;22(2):125–8.
Riello M, Cecchini MP, Zanini A, Di Chiappari M, Tinazzi M, Fiorio M. Perception of phasic pain is modulated by smell and taste. Eur J Pain. 2019;23(10):1790–800.
Gossrau G, Baum D, Koch T, Sabatowski R, Hummel T, Haehner A. Exposure to odors increases pain threshold in chronic low back pain patients. Pain Med. 2020;21(10):2546–51.
Cecchini MP, Riello M, Sandri A, Zanini A, Fiorio M, Tinazzi M. Smell and taste dissociations in the modulation of tonic pain perception induced by a capsaicin cream application. Eur J Pain. 2020;00:1–10.
Mercer ME, Holder MD. Antinociceptive effects of palatable sweet ingesta on human responsivity to pressure pain. Physiol Behav. 1997;61(2):311–8.
Lewkowski MD, Ditto B, Roussos M, Young SN. Sweet taste and blood pressure-related analgesia. Pain. 2003;106:181–6.
Pepino MY, Mennella JA. Sucrose-induced analgesia is related to sweet preferences in children but not adults. Pain. 2005;119:210–8.
Lewkowski MD, Young SN, Ghosh S, Ditto B. Effects of opioid blockade on the modulation of pain and mood by sweet taste and blood pressure in young adults. Pain. 2008;135:75–81.
Kakeda T, Ito M, Matsui T, Ishikawa T. The evidence for sweet substance-induced analgesia in adult human. Pain Res. 2008;23:159–66.
Eggleston K, White TL, Sheehe PR. Adding coca to sucrose: the effect on cold pain tolerance. Chem Senses. 2010;35:269–77.
Kakeda T, Ogino Y, Moriya F, Saito S. Sweet-induced analgesia: an fMRI study. NeuroReport. 2010;21(6):427–31.
Kakeda T, Ishikawa T. Gender differences in pain modulation by a sweet stimulus in adults: a randomized study. Nurs Health Sci. 2011;13:34–40.
Hirsch AR, Ziad A, Kim AY, Lail NS, Sharma S. Pilot study: alleviation of pain in Burning Mouth Syndrome with topical sucralose. Headache. 2011;51(3):444–6.
Horjales-Araujo E, Finnerup NB, Jensen TS, Svensson P. Differential effect of visual and gustatory stimuli on experimental jaw muscle pain. Eur J Pain. 2013;17:811–9.
Priya SA, Savitri S, Shobha CN, Neelam D. Correlation of pain sensitivity and sweet taste in healthy male adults. Natl J Physiol Pharm Pharmacol. 2015;5(1):25–7.
Mooney ER, Davies AJ, Pickering AE. Sweet taste does not modulate pain perception in adult humans. Wellcome Open Res. 2020;5:43.
Duan G, Wu Z, Duan Z, et al. Effects of spicy stimulation and spicy-food consumption on human pain sensitivity: a healthy volunteer study. J Pain. 2020;21:848–57.
Moore PA, Duncan GH, Scott DS, Gregg JM, Ghia JN. The submaximal effort tourniquet test: its use in evaluating experimental and chronic pain. Pain. 1979;6:375–82.
Story MG, Cruz-Orengo L. Feel the burn: the linked sensations of temperature and pain come from family of membrane proteins that can tell neurons to fire when heated or hot-peppered. Am Sci. 2007;95(4):326–33.
van Amerongen G, de Boer MW, Groeneveld GJ, Hay JL. A literature review on the pharmacological sensitivity of human evoked hyperalgesia pain models. Br J Clin Pharmacol. 2016;82(4):903–22.
O’Neill J, Brock C, Olesen AE, Andresen T, Nilsson M, Dickenson AH. Unravelling the mystery of capsaicin: a tool to understand and treat pain. Pharmacol Rev. 2012;64(4):939–71.
Valeriani M, Arendt-Nielsen L, Le Pera D, et al. Short-term plastic changes of the human nociceptive system following acute pain induced by capsaicin. Clin Neurophysiol. 2003;114(10):1879–90.
Valeriani M, Tinazzi M, Le Pera D, et al. Inhibitory effect of capsaicin evoked trigeminal pain on warmth sensation and warmth evoked potentials. Exp Brain Res. 2005;160:29–37.
Hummel T, Kaehling C, Grosse F. Automated assessment of intranasal trigeminal function. Rhinology. 2016;54:27–31.
Antonini A, Tinazzi M, Abbruzzese G, et al. Pain in Parkinson disease: facts and uncertainties. Eur J Neurol. 2018;25(7):917-e69.
Rainville P. Brain mechanisms of pain affect and pain modulation. Curr Opin Neurobiol. 2002;12(2):195–204.
Oertel BG, Lötsch J. Clinical pharmacology of analgesics assessed with human experimental pain models: bridging basic and clinical research. Br J Pharmacol. 2013;168:534–53.
Croy I, Symmank A, Schellong J, et al. Olfaction as a marker for depression in humans. J Affect Disord. 2014;160:80–6.
Croy I, Springborn M, Lötsch J, Johnston ANB, Hummel T. Agreeable smellers and sensitive neurotics—correlations among personality traits and sensory thresholds. PLoS ONE. 2011;6(4):e18701.
Lehrner J, Marwinski G, Lehr S, Johren P, Deecke L. Ambient odors of orange and lavender reduce anxiety and improve mood in a dental office. Physiol Behav. 2005;86:92–5.
Jahangeer A, Mellier D, Caston J. Influence of olfactory stimulation on nociceptive behaviour in mice. Physiol Behav. 1997;62(2):359–66.
Nakama-Kitamura M. The distinctive significance of analgesic drugs and olfactory stimulants on learned pain in mice. Brain Res. 2014;1588:104–12.
Lötsch J, Oertel BG, Felden L, et al. Central encoding of the strength of intranasal chemosensory trigeminal stimuli in a human experimental pain setting. Hum Brain Mapp. 2020;41:5240–54.
Bhattacharjee M, Bhatia R, Mathur R. Gender specificity of sucrose induced analgesia in human adults. Indian J Physiol Pharmacol. 2007;51(4):410–4.
Perkins M, de Bruyne M, Giummarra MJ. A pain in the bud? Implications of cross-modal sensitivity for pain experience. Atten Percept Psychophys. 2016;78:2348–56.
Breslin PAS. An evolutionary perspective on food and human taste. Curr Biol. 2013;23(9):R409–18.
Cecchini MP, Fasano A, Boschi F, Osculati F, Tinazzi M. Taste in Parkinson’s disease. J Neurol. 2015;262:806–13.
Auvray M, Spence C. The multisensory perception of flavor. Conscious Cogn. 2008;17(3):1016–31.
Aroke EN, Powell-Roach KL, Jaime-Lara RB, et al. Taste the pain: the role of TRP channels in pain and taste perception. Int J Mol Sci. 2020;21:5929.
Green BG, Schullery MT. Stimulation of bitterness by capsaicin and menthol: differences between lingual areas innervated by the glossopharyngeal and chorda tympani nerves. Chem Senses. 2003;28:45–55.
Just T, Pau HW, Steiner S, Hummel T. Assessment of oral trigeminal sensitivity in humans. Eur Arch Otorhinolaryngol. 2007;264:545–51.
Lim J, Green BG. The psychophysical relationship between bitter taste and burning sensation: evidence of qualitative similarity. Chem Senses. 2007;32:31–9.
Schöbel N, Kyereme J, Minovi A, Dazert S, Bartoshuk L, Hatt H. Sweet taste and chorda tympani transection alter capsaicin-induced lingual pain perception in adult human subjects. Physiol Behav. 2012;107:368–73.
Green BG, McAuliffe BL. Menthol desensitization of capsaicin irritation: evidence of a short-term anti-nociceptive effect. Physiol Behav. 2000;68:631–9.
Dessirier JM, O’Mahony M, Carstens E. Oral irritant properties of menthol sensitizing and desensitizing effects of repeated application and cross-desensitization to nicotine. Physiol Behav. 2001;73:25–36.
Foo H, Mason P. Sensory suppression during feeding. Proc Natl Acad Sci USA. 2005;102(46):16865–9.
Foo H, Crabtree K, Thrasher A, Mason P. Eating is a protected behavior even in the face of persistent pain in male rats. Physiol Behav. 2009;97(3–4):426–9.
Foo H, Mason P. Analgesia accompanying food consumption requires ingestion of hedonic foods. J Neurosci. 2009;29(41):13053–62.
Bastian B, Jetten J, Hornsey M. Gustatory pleasure and pain. The offset of acute physical pain enhances responsiveness to taste. Appetite. 2014;72:150–5.
Wolff M, Vann SD. The cognitive thalamus as a gateway to mental representations. J Neurosci. 2019;39(19):3–14.
Mizera L, Gossrau G, Hummel T, Haehner A. Effects of analgesics on olfactory function and the perception of intranasal trigeminal stimuli. Eur J Pain. 2017;21:92–100.
Hara T, Hirayama M, Mizutani Y, et al. Impaired pain processing in Parkinson’s disease and its relative association with the sense of smell. Parkinsonism Relat Disord. 2013;19:43–6.
Haehner A, Hummel T, Heinritz W, et al. Mutation in Nav1.7 causes high olfactory sensitivity. Eur J Pain. 2018;22:1767–73.
Heimann D, Lötsch J, Hummel T, Doehring A, Oertel BG. Linkage between increased nociception and olfaction via a SCN9A haplotype. PLoS One. 2013;8(7):e68654.
Ahn H, Black JA, Zhao P, Tyrrell L, Waxman SG, Dib-Hajj SD. Na(v)1.7 is the predominant sodium channel in rodent olfactory sensory neurons. Mol Pain. 2011;7:32.
Weiss J, Pyrski M, Jacobi E, et al. Loss-of-function mutations in sodium channel Na(v)1.7 cause anosmia. Nature. 2011;472:186–90.
Zufall F, Pyrski M, Weiss J, Leinders-Zufall T. Link between pain and olfaction in an inherited sodium channelopathy. Arch Neurol. 2012;69(9):1119–23.
Sasannejad P, Saeedi M, Shoeibi A, Gorji A, Abbasi M, Foroughipour M. Lavender essential oil in the treatment of migraine headache: a placebo-controlled clinical trial. Eur Neurol. 2012;67:288–91.
Roussos AP, Hirsch AR. Alliaceous migraines. Headache. 2014;54(2):378–82.
Aktürk T, Tanık N, Serin Hİ, Saçmacı H, İnan LE. Olfactory bulb atrophy in migraine patients. Neurol Sci. 2019;40:127–32.
Stankewitz A, May A. Increased limbic and brainstem activity during migraine attacks following olfactory stimulation. Neurology. 2011;77:476–82.
Tsai S-S, Wang H-H, Chou F-H. The effects of aromatherapy on postpartum women: a systematic review. J Nurs Res. 2020;28(3):e96.
Lakhan SE, Sheafer H, Tepper D. The effectiveness of aromatherapy in reducing pain: a systematic review and meta-analysis. Pain Res Treat. 2016;2016:8158693. https://doi.org/10.1155/2016/8158693.
Dimitriou V, Mavridou P, Manataki A, Damigos D. The use of aromatherapy for postoperative pain management: a systematic review of randomized controlled trials. J Perianesth Nurs. 2017;32(6):530–41.
De Clifford-Faugere G, Lavallée A, Khadra C, Ballard A, Colson S, Aita M. Systematic review and meta-analysis of olfactive stimulation interventions to manage procedural pain in preterm and full-term neonates. Int J Nurs Stud. 2020;110:103697.
Zhang S, Su F, Li J, Chen W. The analgesic effects of maternal milk odor on newborns: a meta-analysis. Breastfeed Med. 2018;13(5):327–34.
Braud A, Descroix V, Ungeheuer M-N, Rougeot C, Boucher Y. Taste function assessed by electrogustometry in burning mouth syndrome: a case–control study. Oral Dis. 2017;23:395–402.
Formaker BK, Frank ME. Taste function in patients with oral burning. Chem Senses. 2000;25:575–81.
Imura H, Shimada M, Yamazaki Y, Sugimoto K. Characteristic changes of saliva and taste in burning mouth syndrome patients. J Oral Pathol Med. 2016;45:231–6.
Just T, Steiner S, Pau HW. Oral pain perception and taste in Burning Mouth Syndrome. J Oral Pathol Med. 2010;39:22–7.
Siviero M, Teixeira MJ, de Siqueira JTT, Siqueira SRDT. Somesthetic, gustatory, olfactory function and salivary flow in patients with neuropathic trigeminal pain. Oral Dis. 2010;16:482–7.
Grushka M, Sessle BJ, Howley TP. Psychophysical evidence of taste dysfunction in burning mouth syndrome. Chem Senses. 1986;11(4):485–98.
Nagler RM, Hershkovich O. Sialochemical and gustatory analysis in patients with oral sensory complaints. J Pain. 2004;5(1):56–63.
Sinding C, Gransjoen AM, Schlumberger G, Grushka M, Frasnelli J, Singh PB. Grey matter changes of the pain matrix in patients with burning mouth syndrome. Eur J Neurosci. 2016;43:997–1005.
Bartoshuk LM, Catalanotto F, Hoffman H, Logan H, Snyder DJ. Taste damage (otitis media, tonsillectomy and head and neck cancer), oral sensations and BMI. Physiol Behav. 2012;107:516–26.
Cecchini MP, Cardobi N, Sbarbati A, Monaco S, Tinazzi M, Tamburin S. Post-traumatic taste disorders: a case series. J Neurol. 2018;265:836–44.
Boucher Y, Berteretche MV, Farhang F, Arvy MP, Azerad J, Faurion A. Taste deficits related to dental deafferentiation: an electrogustometric study in humans. Eur J Oral Sci. 2006;114:456–64.
Faurion A. Sensory interactions through neural pathways. Physiol Behav. 2006;89:44–6.
Harrison D, Larocque C, Bueno M, et al. Sweet solutions to reduce procedural pain in neonates: a meta-analysis. Pediatrics. 2017;139(1):e20160955.
Stevens B, Yamada J, Ohlsson A, Haliburton S, Shorkey A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database of Syst Rev. 2016;7:CD001069.
Huang R-R, **e R-H, Wen SW, Chen S-L, She Q, Liu Y-N, Harrison D. Sweet solutions for analgesia in neonates in China: a systematic review and meta-analysis. Can J Nurs Res. 2019;51(2):116–27.
Hatfield LA, Murphy N, Karp K, Polomano RC. A systematic review of behavioural and environmental interventions for procedural pain management in preterm infants. J Pediatr Nurs. 2019;44:22–30.
Olsson E, Pettersson M, Eriksson M, Ohlin A. Oral sweet solution to prevent pain during neonatal hip examination: a randomized controlled trial. Acta Paediatr. 2019;108(4):626–9.
Ghaderi F, Ahmadbeigi M, Vossoughi M, Sardarian A. The efficacy of administrating a sweet-tasting solution for reducing the pain related to dental injections in children: a randomized controlled trial. Int J Paediatr Dent. 2020;00:1–7.
Acknowledgements
We wish to thank K. Britsch for his assistance in proof-reading the manuscript.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee is funded by the University of Verona.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Angela Sandri, Maria Paola Cecchini, Marianna Riello, Alice Zanini, Riccardo Nocini, Mirta Fiorio, Michele Tinazzi have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies performed by any of the authors and involving human participants or animals.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Angela Sandri, Maria Paola Cecchini, Mirta Fiorio and Michele Tinazzi are equally contributed in this work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sandri, A., Cecchini, M.P., Riello, M. et al. Pain, Smell, and Taste in Adults: A Narrative Review of Multisensory Perception and Interaction. Pain Ther 10, 245–268 (2021). https://doi.org/10.1007/s40122-021-00247-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-021-00247-y