Abstract
Purpose
The purpose of this mini review is to describe metabolomics in cerebrospinal fluid (CSF) and its potential in aneurysmal subarachnoid hemorrhage (aSAH). In brain injury, patients’ micro dialysis enables detecting biochemical change in brain tissue. Indicators for ischemia were detected such as lactate, pyruvate, glucose, and glutamate. In aSAH patients, the pathophysiology and the factor for poor outcome are not completely understood yet. Routine use of biomarkers in CSF, particularly in aSAH patients, is still lacking.
Methods
This mini review was performed on the role of metabolomics alterations after aneurysmal subarachnoid hemorrhage.
Results
We identified five clinical studies that addressed metabolomics in patients with aneurysmal subarachnoid hemorrhage.
Conclusion
There is increasing evidence suggesting that biomarkers can give insight in the pathogenesis and can serve as an outcome predictor. In this mini review, we present a brief overview of metabolomics profiling in neuroscience and wish to discuss the predictive and therapeutic value in aSAH patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Regardless of the extensive experimental and clinical research efforts, aneurysmal subarachnoid hemorrhage (aSAH) remains a devastating disease, frequently striking patients in a fairly young age without any warning signs. Half of patients with aSAH are younger than 55 years old. Most survivors remain significantly impaired in their daily lives [1]. Post-hemorrhagic pathophysiological mechanisms are multifactorial and complex and factors predicting poor outcome or delayed cerebral ischemia (DCI) are not completely understood. Thus, the incorporation of innovative research strategies is pivotal. The advent of metabolomic approaches allows the simultaneous, large-scale screening of numerous metabolites in a biological sample. A major benefit of metabolomic research is novel metabolites that may be discovered and associated with a disease process for the first time, without the demand for an existing hypothesis. Despite considerable success in brain research, to date, metabolomics has hardly been applied for studying SAH-related changes in CSF [3, 4].
In this mini review, we present a brief overview of CSF metabolomics profiling in neuroscience and discuss its potential predictive and therapeutic value in aSAH patients.
Cerebrospinal fluid metabolome
Apart from numerous vital functions of CSF such as hydromechanical cerebral protection and salubrious homeostasis of the brain, specific CSF conditions may mirror pertinent alterations offering an in-depth insight into the cerebral metabolite production rates and its disorders for instance aSAH. Metabolomics methods have identified appreciable number of biomarkers for cerebral diseases including their progression [3, 5,6,7].
Metabolites are small molecules (< 1500 Da) in various body fluids which can influence cell response locally and systemically, possibly reflecting a disease progression [8]. Metabolites can be activated under specific conditions or can change during a disease progress or depending on drug interactions [4, 9]. The term “metabolome” is derived from the term metabolism and refers to a set of molecules within a biological sample (e.g., cerebrospinal fluid) [10]. In other words, metabolomics describes the systematic analysis of metabolites [11, 12].
In 2008, a very first systematic analysis of the human cerebrospinal fluid metabolome demonstrated that 41–70 CSF compounds can be detected with nuclear magnetic resonance spectroscopy (NMR), gas chromatography–mass spectrometry (GC–MS) or Fourier transform mass spectrometry coupled with liquid chromatography (LC–FTMS). The authors of the study also described that CSF is a metabolically diverse fluid with 33 different compound categories. Of note, CSF is rich in amino acids, sugars, and inorganic salts [5].
Nowadays, metabolomic approaches are used in several neurological diseases to particularize diagnosis, prognosis, and monitor treatments. Metabolomics has been applied in many degenerative disorders. For instance, various metabolites are being routinely used in diagnostics and treatment for Alzheimer´s disease, amyotrophic lateral sclerosis, epilepsy, Parkinson’s disease, multiple sclerosis, and stroke [11].
CSF metabolomics in aneurysmal subarachnoid hemorrhage
In respect of aSAH, established or clinically verified biomarkers are still lacking or are not yet used routinely in clinical practice. Discovery of novel specific indicators for, i.e., DCI and poor clinical outcome is urgently needed. However, to our best knowledge, there are only three recent studies dealing with metabolomics profiling of CSF after aSAH.
In a 2017 European study, Sokół et al. revealed that in their liquid chromatography–mass spectrometry/mass spectrometry (LC–MS/MS) of 49 CSF samples from 23 patients analyzing 33 amino acids and related compounds, 27 of them were significantly elevated within the first 3 days after aSAH. The investigation showed that the patterns differ between poor and good outcome. In particular, during early brain injury (EBI) after aSAH, concentration of nine amino acids was significantly higher in patients with poor outcome compared to those with good outcome: taurine, aspartic acid, citrulline, glutamic acid, gamma-amino-butyric acid, 3-methyl-histidine, ornithine, cystathionine, and isoleucine. On day 5 post-SAH, glutamic acid was the only amino acid that significantly increased. Interestingly, higher levels of excitatory amino acids (i.e., glutamic acid, aspartic acid, and 2-amino-adipic acid) appear to predict a poor outcome [13]. Similar findings were described in an American study in the same year. Of 97 metabolites identified with known chemical structures, 16 metabolites, primarily free amino acids, significantly changed their concentration with time. Of these, six metabolites (i.e., 2-hydroxyglutarate, tryptophan, glycine, proline, isoleucine, and alanine) strongly correlated with Glasgow Outcome Score (GOS) of patients at 1-year post-SAH [14]. Importantly, none of these metabolites correlated with vasospasm.
The first prospective study analyzed endogenous metabolites in patients with ruptured intracranial aneurysms and aSAH Fisher Grade III and IV compared to patients with elective aneurysms. CSF samples were consecutively collected before aneurysm treatment (the time point of EVD placement), intraoperatively, 6 h later, and daily thereafter for 10 days. The study showed that amino acids, biogenic amines, and acylcarnitine levels continuously increased over the time starting as early as 6 h after aSAH onset. Taurine concentration, however, was initially elevated directly after onset and started decreasing after only 6 h. Other analyzed metabolites such as hydroxysphingomyelins, lysophosphatidylcholines, and sphingomyelins showed temporarily increased levels immediately after aSAH with an ensuing decrease to CSF concentrations within the first 6 h that are comparable with the non-hemorrhagic CSF. The study presented significant consecutive alterations of various metabolites in the longitudinal course of aSAH. There was a peak of structural amino acids as early as within the first 6 h after aneurysm treatment. However, the authors concluded that further evaluation of CSF metabolites and compounds and their time-dependent alterations may elucidate pathophysiological processes after aSAH, potentially providing new predictive biomarkers related to aSAH-specific parameters and outcomes [16].
A Chinese study published in 2018 showed data of 40 subarachnoid hemorrhage patients and the control group of 6 patients. Neurological outcome was evaluated 12 months after discharge. Interestingly, the group showed that there is no significant variation among CSF metabolome in subarachnoid hemorrhage patients with different fisher scales (amount and distribution of blood). However, sub-analysis showed that pyruvate metabolism was altered in subarachnoid hemorrhage patients, especially in those with a high Hunt–Hess scale (clinical condition). Pyruvate level is associated with WFNS (focal motor deficit) grading scale above III. In retrospect, patients with unfavorable outcome had significantly altered amino acid metabolism and lipid biosynthesis [17].
The work of an American group which was published in 2020 aimed to identify the leading CSF metabolites associated with poor outcome, as determined by the modified Rankin Scale (mRS) at discharge and at 90 days after discharge. The authors used 81 CSF samples. Through orthogonal partial least squares-discriminant analysis, symmetric dimethylarginine (SDMA), dimethylguanidine valeric acid (DMGV), and ornithine were detected as the markers associated with poor outcome [18].
All five aforementioned clinical studies dealing with CSF metabolomics after aSAH provide a first very interesting finding of various metabolites that can be instrumental in further innovative research strategies.
Discussion
In summary, metabolomics of post-hemorrhagic CSF provides a unique signature of multifactorial pathophysiologic processes in the brain after aSAH. A published study in 2005 described metabolomics as a systematic study of unique chemical fingerprints that specific cellular processes leave behind that provides dynamic information [15]. While still in its infancy, we shall perceive the promising potential and possible future application of CSF metabolomics post-aSAH for clinical practice. All, Ho et al., Sokół et al., Lu et al., Koch et al., and Li et al. showed, in their clinical observational studies, several metabolites linked to aSAH and its outcomes. All authors concurred in significantly elevated levels of several amino acids in post-aSAH CSF time courses. So far, only these five clinical studies with a small number of patients are available in the literature (Supplementary Table 1). It can be discussed that the studies might have been underpowered. In our opinion, further thorough systematic evaluation of all identified CSF metabolites and compounds alongside with their time-dependent longitudinal alterations may be very helpful to possibly clarify pathophysiological processes after aSAH, with a potential of discovering new clinically relevant biomarkers related to aSAH-specific events.
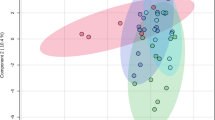
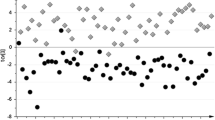
Several significant altered compounds in those studies are found in the cerebral glucose metabolism (Fig. 1). Further, metabolites as excitatory amino acids in the neurotransmitter formation and structural amine levels were changed after aSAH (Fig. 2).
Future metabolomics profiling in both untargeted and targeted ways in aSAH patients should allow acquiring further insights into the global cerebral endogenous metabolism after aSAH with in-depth monitoring of pertinent metabolomic changes, and therefore potential identification of aSAH-specific biomarkers.
Data availability
Availability of Data and Material not applicable.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- SAH:
-
Subarachnoid hemorrhage
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- GABA:
-
Gamma-aminobutyric acid
- DCI:
-
Delayed cerebral ischemia
- NMR:
-
Nuclear magnetic resonance
- GC–MS:
-
Gas chromatography–mass spectrometry
- LC–FTMS:
-
Fourier transform mass spectrometry coupled with liquid chromatography
- EBI:
-
Early brain injury
- GOS:
-
Glasgow Outcome Score
References
Etminan NCH, Hackenberg K, de Rooij NK, Vergouwen MDI, Rinkel GJE, Algra A (2019) Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol 76(5):588–597
Vasilopoulou CG, Margarity M, Klapa MI (2016) Metabolomic analysis in brain research: opportunities and challenges. Front Physiol 7:183
Fonteh AN, Harrington RJ, Huhmer AF, Biringer RG, Riggins JN, Harrington MG (2006) Identification of disease markers in human cerebrospinal fluid using lipidomic and proteomic methods. Dis Markers 22(1–2):39–64
Rashad SSD, Yamazaki T, Matsumoto Y, Tomioka Y, Saito R, Uruno A, Niizuma K, Yamamoto M, Tominaga T (2020) Metabolic basis of neuronal vulnerability to ischemia; an in vivo untargeted metabolomics approach. Sci Rep 10(1):6507
Wishart DS, Lewis MJ, Morrissey JA et al (2008) The human cerebrospinal fluid metabolome. J Chromatogr B Anal Technol Biomed Life Sci 871(2):164–173
Toczyłowska B, Chalimoniuk M, Wodowska M, Mayzner-Zawadzk E (2006) Changes in concentration of cerebrospinal fluid components in patients with traumatic brain injury. Brain Res 1104(1):183–189
Kaddurah-Daouk R, Krishnan KR (2009) Metabolomics: a global biochemical approach to the study of central nervous system diseases. Neuropsychopharmacology 34(1):173–186
Goodacre RVS, Dunn WB, Harrigan GG, Kell DB (2004) Metabolomics by numbers: acquiring and understanding global metabolite data. Trends Biotechnol 22(5):245–252
Monteiro MS, Carvalho M, Bastos ML, de Guedes Pinho P (2013) Metabolomics analysis for biomarker discovery: advances and challenges. Curr Med Chem 20(2):257–271
Wishart DS (2007) Current progress in computational metabolomics. Brief Bioinform 8(5):279–293
Donatti ACA, Godoi AB, da Rosa DC, Lopes-Cendes I (2020) Circulating metabolites as potential biomarkers for neurological disorders-metabolites in neurological disorders. Metabolites 10(10):389
Vasilopoulou CG, Margarity M, Klapa MI (2016) Metabolomic analysis in brain research metabolomic analysis in brain research: opportunities and challenges. Front Physiol 7:183
Sokół B, Urbaniak B, Wąsik N, Plewa S, Klupczyńska A, Jankowski R, Więckowska B, Juszkat R, Kokot Z (2017) Amino acids in cerebrospinal fluid of patients with aneurysmal subarachnoid haemorrhage: an observational study. Front Neurol 8:438
DE Lu A, Winkler E, Grant R, Eid T, Bulsara K (2017) Cerebrospinal fluid untargeted metabolomic profiling of aneurysmal subarachnoid hemorrhage: an exploratory study. Br J Neurosurg 32(6):637–641
Daviss B (2005) Growing poains for metabolomics. Scientist 19:25–28
Ho W, Goerke AS, Glodny B, Oberacher H, Helbok R, Thome C, Petr O. Time Course of Metabolomic Alterations in CSF after aneurysmal Subarachnoid Hemorrhage. Frontiers in neurology. 2020
Li Y, Wang R, Xu M, **g X, Sun R, Na S, Liu T, Ding X, Sun C, Ge W (2019) Aneurysmal subarachnoid hemorrhage onset alters pyruvate metabolism in poor-grade patients and clinical outcome depends on more: a cerebrospinal fluid metabolomic study. ACS Chem Neurosci 10(3):1660–1667
Koch M, Acharjee A, Ament Z, Schleicher R, Bevers M, Stapleton C, Patei A, Kimberly T. Machine Learning-driven metabolomic evaluation of cerebrospinal fluid: insights into poor outcomes after aneurysmal subarachnoid hemorrhage.
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Franziska A. Schmidt, conflict of interest: none, disclosure of funding: none; Wing Mann Ho, conflict of interest: none, disclosure of funding: none; Ondra Petr, conflict of interest: none, disclosure of funding: none; Claudius Thomé, conflict of interest: none, disclosure of funding: none.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ho, W.M., Schmidt, F.A., Thomé, C. et al. CSF metabolomics alterations after aneurysmal subarachnoid hemorrhage: what do we know?. Acta Neurol Belg 123, 2111–2114 (2023). https://doi.org/10.1007/s13760-023-02266-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-023-02266-2