Abstract
Purpose
To evaluate the efficacy and tolerability of adjunctive lacosamide (LCM) in patients with focal-onset seizures, with or without combined secondarily generalized seizures.
Methods
106 patients aged ≥ 16 years were recruited consecutively in this single-center prospective observational study. All patients received LCM as an add-on treatment on the basis of clinical judgement. Seizure frequency, adverse events (AEs) and retention rates were obtained at 3 and 6 months after LCM introduction.
Result
The overall response rates were 53.3 and 70.4% after 3 and 6 months, respectively, and the freedom of seizures at the same points was reached at 19 and 26.5%. The retention rates were 99.1% at the 3-month follow-up and 93.3% at the 6-month follow-up. The overall incidence of adverse events was 35.8%. The leading AEs were dizziness (16.98%) and sedation (6.6%).
Conclusions
Our study confirmed the efficacy and tolerability of adjunctive LCM in Chinese patients in real-life conditions. Based on our treatment experience, a universal maintenance dose of LCM would be needed in Chinese patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is one of the most common chronic diseases of the central nervous system, with an estimated prevalence of 0.5–1% [1]. In China, The prevalence of epilepsy is about 7.0 per 1000 [2]. Anti-seizure medication (ASM) therapy is the main treatment for epilepsy, but about 30% of patients still do not successfully respond to ASMs [3]. The International League Against Epilepsy (ILAE) defines drug-resistant epilepsy (DRE) as " failure of adequate trials of two tolerated and appropriately chosen and used AED schedules (whether as monotherapies or in combination) to achieve sustained seizure freedom [4]. Therefore, there is an urgent need to develop and apply newer ASMs with novel mechanisms of action.
Lacosamide, one of the latest anti-epileptic drugs, is a functionalized amino acid with the chemical name (R) -2-acetyl-n-benzyl-3-methoxyacrylamide, which was widely used in adult and childhood epilepsy [5,6,7,8,9,10]. They function by selectively enhancing the slow inactivation of voltage-gated sodium channels without affecting fast inactivation; in this way, they reduce the excitability of pathological neurons without affecting physiological neuronal function [11]. Meanwhile, it appears to bind to collapsin response mediator protein 2 (CRMP-2) involved in neurotrophic signaling. This is hypothesized to produce a neuroprotective effect preventing the formation of abnormal neuronal connections in the brain [12]. In addition, Ruffolo G et al. [13] have recently found that lacosamide also acts on the GABA receptor; this mechanism is related to its ability to prevent the evolution of status epilepticus.
Therefore, we conducted this prospective study to evaluate the efficacy and tolerability of LCM as an add-on therapy in patients with focal-onset seizures, with or without secondarily generalized seizures.
Methods
Subjects
Patients with focal-onset seizures (with or without secondarily generalized seizures) who visited Qilu Hospital of Shandong University from August 2020 to April 2021 were enrolled in this study. The study was performed in accordance with the Declaration of Helsinki. All subjects and their guardians (in the case of children) gave informed consent to participate. The inclusion criteria were: (a) age ≥ 16 years old; (b) diagnosed as focal-onset seizures [14, 15] (with or without secondarily generalized seizures) based on clinical presentations and EEG confirmation, according to International League Against Epilepsy classifications of seizures and epilepsy; (c) the patients have ≥ 1 seizures per month during the 3 months before inclusion; (d) seizures were not controlled with ≥ 1 ASM. The exclusion criteria: (a) psychogenic nonepileptic seizures; (b)status epilepticus; (c)primary generalized tonic–clonic seizures; (d) lactation or pregnancy; (e) alcohol or drug abuse; (f) psychiatric disease and severe diseases of other systems; patients were excluded if they had experienced these symptoms during the 3 months before inclusion.
Study design
This was a 6 month, single-center, prospective study evaluating the efficacy and safety of LCM. The following clinical data of the patients were collected: age, sex, etiology of epilepsy, age at onset, duration of epilepsy, previous ASMs, concomitant ASMs, seizure frequency (monthly seizure frequency during the 3 months before starting lacosamide treatment), seizure types (focal or combined secondarily generalized seizures). Enzyme-inducing ASMs (EIASMs) included carbamazepine, oxcarbazepine, phenobarbital, phenytoin. All patients enrolled were treated with LCM twice daily at morning time and bedtime, the initial dose was 50 mg each time, the maintenance dose was 100 mg each time after two weeks, all patients were used to the same dosing schedules. And there was no change in concomitant ASMs (neither changes in types of concomitant ASMs nor changes in doses of concomitant ASMs). Patients were followed up at 3 and 6 months after LCM add-on.
Outcome evaluation
Efficacy was assessed by measuring changes in seizure frequency at 3 and 6 months follow-up compared with baseline. The baseline was 3 months before the addition of LCM and the seizure frequency was based on the patients’ seizure diary. We classified patients into five categories: (1) seizure freedom, (2) reduction of seizure frequency ≥ 50%, (3) reduction of seizure frequency < 50%, (4) no change, (5) worsened (patients with increased seizure frequency). Patients who have achieved a reduction of more than 50% or seizure free were defined as responders (The criteria for patients with combined secondarily generalized seizures was to achieve a reduction in all seizure types).
Tolerability was evaluated by reported adverse events (AEs), LCM discontinuation and clinical laboratory tests (blood routine, blood sedimentation rate, blood glucose, blood lipid, liver and kidney function, blood electrolytes, and urine routine) at each follow-up. AEs were mainly based on directly reported by the patients and through specific questioning about the most known common AEs associated with LCM (no standardized AE questionnaire was used).
Adverse reactions are mainly manifested as dizziness, sedation, fatigue, memory loss, nausea, irritability, vision and gait instability. Those who cannot follow-up timely due to COVID-19 will be follow-up by telephone or WeChat.
Statistical analysis
All statistical analyses were performed using the statistical software SPSS version 23.0. For between-group comparisons, t Tests or the non-parametric Mann–Whitney U tests were used to compare continuous variables, while categorical variables were compared using Chi-squared tests or Fisher’s exact test. Retention rate was calculated by counting the number of patients taking lacosamide every 2 weeks using the Kaplan–Meier survival analysis. The threshold of statistical significance was p < 0.05.
Result
Subjects
We enrolled 111 patients, but five of them did not receive any dose of lacosamide (three patients refused to sign the informed consent, two patients worried about adverse events of LCM), so their data were not included in this study, we ultimately recruited 106 patients (47 females, 59 males). The mean age was 33.1 ± 13.7 years (range 16–71 years). Baseline population and clinical characteristics of the patients are shown in Table 1. The etiology was classified according to the International Anti-epilepsy Consortium, including genetic (n = 1), structural (n = 27), immunity (n = 2), metabolism (n = 3), infection (n = 14) and unknown etiology (n = 59). Among all patients enrolled in the study, 32(30.2%) had focal seizures and 74 (69.8%) had secondarily generalized seizures, and their monthly seizure frequency was 13.4 ± 22.
All patients were taking at least one ASM at the time of initiation of LCM, while the mean number of ASM was 1.65 ± 0.71 and the type of accompanying ASM is shown in Table 2. Valproate acid (VPA) is the most common concomitant ASM (73.58%), followed by levetiracetam (LEV)(33.96%), oxcarbazepine (OXC) (17.92%) and carbamazepine(CBZ)(16.04%). Meanwhile, concomitant ASMs were also classified as EIASMs and non-EIASMs (any other ASMs).
LCM dose and retention rate
The starting dose is 100 mg/d, and then increased to 200 mg/d two weeks later to reach a universally tolerated dose with good seizure control. The usual target dose is 400 mg/d, but the dose adjustment is determined by the physician based on the patients’ clinical response.
The retention rate at 3 months was 99.1%(105/106) because one discontinued due to a worsening in seizure frequency. The retention rate at 6 months was 93.3%(98/105) because two patients were lost to follow-up and five patients discontinued lacosamide. Of these five patients, due to AEs occurrence in two subjects, no change in seizure frequency in four patients and a worsening of seizure frequency in one patient.
Efficacy
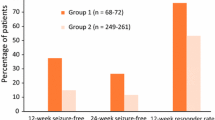
At 3 months, 105 patients were available for efficacy evaluations. The overall response rate (≥ 50% seizure reduction) at 3 months was 53.3% (56/105). In detail, seizure freedom was achieved in 19% (20/105), 39.0% (36/105) had a reduction ≥ 50%. 32(30.5%) had a reduction < 50%, 11 (10.5%) showed no change in seizure frequency, and 1(0.9%) out of 105 patients experienced a worsening in seizure frequency (Fig. 1).
At the 6 months follow-up, 98 patients were available for efficacy evaluations. The total response rate at 6 months was 70.4% (69/98), and 26.5% (26/98) became seizure-free, 43.9% (43/98) had a reduction ≥ 50% in seizure frequency. 23 (23.5%) had a reduction < 50% and 6(6.1%) showed no change in seizure frequency. Furthermore, none of the patient experienced a worsening of seizure frequency.
After the last follow-up, patients were divided into responders and non-responders, and comparisons of their demographic and related variables were shown in Table 3. There was no significant difference between responders and non-responders in age, sex, age of onset and so on. We found that patients with shorter epilepsy duration had a better response effect for lacosamide addition, compared with longer epilepsy duration (6.2 ± 5.4 vs 12.2 ± 12.0, p = 0.002). And, interestingly, patients with unknown etiology (56/98, 57.1%) and structural (25/98, 25.5%) appeared to respond better, although this result was not statistically significant.
Patients combined with secondarily generalized seizures had a higher response rate (48.0%, 47/98) (p = 0.168) and non-responders had higher baseline episodes than responders (p = 0.986) but were not statistically significant. In addition, there were no significant differences between responders and non-responders in the number of previous ASMs and concomitant ASMs (p = 0.136).
Patients concomitant with non-EIASM (77.4%, 48/62) responded higher than those with EIASM(58.3%,21/36) but not statistically significant(p = 0.05), and in concurrent ASM, VPA and LEV combined more frequently in responders than non-responders. In addition, the proportion of responders combining VPA and LCM was highest (36.2%, 25/69), followed by the LEV and LCM combination (13.0%, 9/69).
Safety
Overall, 38 (35.8%) out of the 106 patients experienced at least one adverse event during treatment with LCM (6-month follow-up), and a total of 51 adverse events were reported (Fig. 2). There were no significant differences in the daily LCM doses between patients experiencing adverse events and those without. Dizziness was the most common adverse reaction (16.98%, 18/106), followed by sedation (8.5%, 9/106) and fatigue (6.6%, 7/106). Memory loss (4.71%, 5/106), nausea (2.83%, 3/106), irritability (2.83%, 3/106), vision (1.87%, 2/106) and gait instability (1.87%, 2/106) were less frequently mentioned. In general, adverse events were mild to moderate and could be tolerated by most patients. Three (2.83%) stopped due to adverse events (some had more than one adverse event). Specifically, one patient withdrew from LCM treatment for dizziness and gait instability, one patient for lethargy, and one for memory loss.
We also observed some changes in laboratory examination, but most were within the normal range and had no clinical significance.
Discussion
Surgical treatment for epilepsy achieved seizure-free four times than medication [15]. However, a significant proportion of refractory patients are either ineligible for surgery or refuse surgery. In addition, approximately one-third of the patients had a persistent seizure episode after seizure surgery [16, 17]. Thus, medication remains the primary treatment for most patients with focal seizures. In patients with focal epilepsy, combination therapy is a more effective treatment regimen after the first AED failed due to lack of efficacy [18]. A large sample population study showed that combination medications treatments with different mechanisms of action showed greater efficacy compared to the same mechanism [19]. The mechanism of ASM should be considered when selecting the second ASM as a combination treatment. Combination therapy with the old enzyme-induced ASM may reduce the efficacy of other drugs [20]. The use of novel non-enzyme-induced ASM is easier to implement combination treatment [21]. And patients with shorter epilepsy duration had a better response effect for lacosamide addition, compared with longer epilepsy duration, this finding would encourage the early initiation of lacosamide. Since 2010, numerous studies have demonstrated the good clinical efficacy of LCM in patients with epilepsy [22,23,24,25], and this observational study evaluated the efficacy and safety of LCM as an add-on therapy for the treatment of patients with focal-onset seizures, with or without secondarily generalized seizures. In our population, we found a responder rate of 53.3% after 3 months and 70.4% after 6 months of LCM administration, with 19% and 26.5% of patients achieving seizure freedom at 3 and 6 months, respectively.
In combination therapy, common combination agents include multitarget ASMS, synaptic vesicle proteins 2A regulators, fast sodium channel blockers, benzodiazepines, etc. Lacosamide has ideal pharmacokinetics and pharmacodynamic properties, which was no need to consider clinical interaction [26]; however, in clinical practice, it has been found to have potential effects with other drugs. Serum concentrations were affected by enzyme inducers and age, and Tountopoulou M et al. [27] reported that lacosamide reduced blood concentrations of sodium valproate acid (VPA) and levetiracetam (LEV). The mechanism of this change is not completely understood. Markoula S et al. [28] reported that carbamazepine and sodium phenytoin may significantly reduce serum lacosamide concentrations through the induction of lysamine metabolism. Simona Lattanzi et al. [29] also reported that there was a statistically significant (p = 0.006) higher number of responders to BRV in patients who were receiving SCBs than in those receiving no sodium channel blockers (SCBs), and treatment discontinuation due to AEs was less common in patients treated with BRV and concomitant SCBs than in patients treated with BRV and no SCBs (8.8% vs. 14.6%; p = 0.038). The chemical structure of brivaracetam (BRV) is similar to levetiracetam (LEV).
The most common adverse events of LCM involve the nervous and gastrointestinal systems, including headache, vomiting, dizziness, nausea, fatigue, ataxia, abnormal vision abnormalities, dizziness, nystagmus, coordination problems and gait problems, with occasional reported drug rash or arrhythmias [30, 31]. Dose-related adverse events include dizziness, nausea, fatigue and vomiting; most are mild or moderate intensity, adverse reactions can be mitigated or disappeared by reducing the maintenance dose [32]. In this experiment, the adverse effects were mild and only 1 patient increased seizure frequency after the addition of LCM and stopped LCM use due to ataxia. These AEs subsided with dosage reduction and withdrawal without causing serious diseases. Moreover, it is worth mentioning that the occurrence of AEs cannot be attributed to a single addition of a new drug, but may also be caused by different combinations and the total drug load [33]. At each follow-up, we performed clinical laboratory tests on the patient, no patient was found to have abnormalities of liver and kidney function during the medication. Some patients had abnormalities in blood glucose and lipid, none were related to our study and they all were long-term chronic diseases in patients.
There are several limitations to our study. First, this was a single-center observational study that included only a limited number of patients. Therefore, randomized double-blind clinical trials on a larger number of patients are necessary for the future. Second, serum levels of LCM were not measured, we could not precisely assess the influence of enzyme inducers on plasma levels associated with seizure control and AEs. Third, due to some patients having 1 seizure per month during the 3 months before inclusion, in the 6 month follow-up time, if they did not show any epileptic seizures within 6 months, it is listed as seizure-free. The follow-up time is short, there may be some deviation, and a longer follow-up is needed for verification. Finally, as we did not use a standardized questionnaire for assessing AEs, the incidence of adverse events caused by LCM treatment may be inaccurate.
This study confirms the good efficacy and tolerance of LCM addition in the treatment of focal epilepsy. As the third generation of ASMs, LCM currently uses insufficient clinical data in China, which may extend the clinical indication of STP beyond DS. Controlled studies with larger samples are needed to confirm these results, and it is believed that future LCM may be a new option for the effective treatment of patients with focal seizures.
Conclusion
In conclusion, as a prospective real-life study in Chinese patients, our findings confirmed the good efficacy and tolerability of adjunctive LCM in patients with focal-onset seizures, with or without combined secondarily generalized seizures. The concomitant use of EIASMs did not appear to reduce the efficacy of LCM in seizure control. The combined application of valproic acid, levetiracetam and LCM may provide a better treatment option for patients, but further studies with long-term follow-up are necessary to confirm this result.
Data availability
All our data came from the epilepsy patient database of our institute, and all data were used with the informed consent of patients to ensure data availability.
References
Beghi E, Giussani G (2018) Aging and the epidemiology of epilepsy. Neuroepidemiology 51(3–4):216–223. https://doi.org/10.1159/000493484
Wang W, Wu J, Dai X et al (2008) Global campaign against epilepsy: assessment of a demonstration project in rural China. Bull World Health Organ 86(12):964–969. https://doi.org/10.2471/blt.07.047050
Dalic L, Cook MJ (2016) Managing drug-resistant epilepsy: challenges and solutions. Neuropsychiatr Dis Treat 12:2605–2616. https://doi.org/10.2147/NDT.S84852
Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Hauser WA, Mathern G et al (2010) Definition of drug resistant epilepsy: consensus proposal by the ad hoc task force of the ILAE commission on therapeutic strategies. Epilepsia 51(6):1069–1077
de Biase S, Nilo A, Bernardini A et al (2019) Timing use of novel anti-epileptic drugs: is earlier better? Expert Rev Neurother 19(10):945–954
Palleria C, Cozza G, Khengar R et al (2017) Safety profile of the newest antiepileptic drugs: a curated literature review. Curr Pharm Des 23(37):5606–5624
Abou-Khalil BW (2019) Update on antiepileptic drugs 2019. Continuum (Minneapolis, Minn) 25(2):508–536
Rosati A, Ilvento L, Rizzi R et al (2018) Long-term efficacy of add-on lacosamide treatment in children and adolescents with refractory epilepsies: a single-center observational study. Epilepsia 59(5):1004–1010
Ortiz de la Rosa JS, Ladino LD, Rodriguez PJ et al (2018) Efficacy of lacosamide in children and adolescents with drug-resistant epilepsy and refractory status epilepticus: a systematic review. Seizure. 56:34–40
Kwok CS, Johnson EL, Krauss GL (2017) Comparing safety and efficacy of “third-generation” antiepileptic drugs: long-term extension and post-marketing treatment. CNS Drugs 31(11):959–974
Rogawski MA, Tofighy A, White HS, Matagne A, Wolff C (2015) Current understandingof the mechanism of action of the antiepileptic drug lacosamide. Epilepsy Res 110:189–205
Wilson SM, Khanna R (2015) Specific binding of lacosamide to collapsin responsemediator protein 2 (CRMP2) and direct impairment of its canonical function:implications for the therapeutic potential of lacosamide. Mol Neurobio 51:599–609
Ruffolo G, Di Bonaventura C, Cifelli P, Roseti C et al (2018) A novel action of lacosamide on GABAA currents sets the ground for a synergic interaction with levetiracetam in treatment of epilepsy. Neurobiol Dis 115:59–68
Scheffer IE, Berkovic S, Capovilla G et al (2017) ILAE classification of the epilepsies: position paper of the ILAE commission for classification and terminology. Epilepsia 58(4):512–521. https://doi.org/10.1111/epi.13709
Fisher RS, Cross JH, French JA et al (2017) Operational classification of seizure types by the International league against epilepsy: position paper of the ILAE commission for classification and terminology. Epilepsia 58(4):522–530. https://doi.org/10.1111/epi.13670
Baud MO, Perneger T, Racz A, Pensel MC, Elger C, Rydenhag B et al (2018) European trends in epilepsy surgery. Neurology 91:96–106
Jobst BC, Cascino GD (2015) Resective epilepsy surgery for drug-resistant focal epilepsy: a review. JAMA 313(3):285–293
ChiX,LiR,HaoX,etal.Response to treatment schedule safter the firstanti epileptic drug failed.Epilepsia.2018;00:1–7.
Margolis JM, Chu BC, Wang ZJ et al (2014) Effectiveness of antiepileptic drug combination therapy for partial-onset seizures based on mechanisms of action. JAMA Neurol 71:985–993
Schmidt D, Schachter SC (2014) Drug treatment of epilepsy in adults. BMJ 348:254
Schmidt D (2009) Drug treatment of epilepsy:options and limitations. Epilepsy Behav 15:56–65
Heyman E, Lahat E, Levin N et al (2012) Preliminary efficacy and safetyof lacosamide in children with refractory epilepsy. Eur J PaediatrNeurol 16(1):15–19
Yorns WR, Khurana DS, Carvalho KS et al (2014) Efficacy of lacosamideas adjunctive therapy in children with refractory epilepsy. J ChildNeurol 29(1):23–27
Guilhoto LM, Loddenkemper T, Gooty VD et al (2011) Experience with lacosamide in a series of children with drug-resistant focal epilepsy. Pediatr Neurol 44(3):414–419
Rastogi RG, Ng Y (2012) Lacosamide in refractory mixed pediatricepilepsy: a prospective add-on study. J Child Neurol 27(4):492–495
Svendsen T, Brodtkorb E, Baftiu A et al (2017) Therapeutic drug monitoring of lacosamide in norway: focus on pharmacokinetic variability. Eff Tolerab Neurochem Res 42(7):2077–2083
Tountopoulou M et al (2017) Lacosamide lowers valproate and levetiracetam levels. Neuropediatrics 48(3):188–189
Markoula S, Teotonio R, Ratnaraj N et al (2014) Lacosamide serum concentrations in adult patients with epilepsy: the influence of gender, age, dose, and concomitant antiepileptic drugs. Ther Drug Monit 36:494–498
Lattanzi S, Canafoglia L, Canevini MP et al (2021) Adjunctive brivaracetam in focal epilepsy: real-world evidence from the brivaracetam add-on first italian network study (BRIVAFIRST). CNS Drugs 35(12):1289–1301
Shorvon S, Perucca E, Engel J Jr (2016) The Treatment of Epilepsy, 4th edn. John Wiley & Sons, UK
Lattanzi S, Cagnetti C, Foschi N et al (2015) Lacosamide monotherapy for partial onset seizures. Seizure. 27:71–74
Biton V, Gil-Nagel A, Isojarvi J et al (2015) Safety and tolerability of lacosamide as adjunctive therapy for adults with partial-onsetseizures: analysis of data pooled from three randomized, doubleblind, placebo-controlled clinical trials. Epilepsy Behav 52(2):119–127
Rohracher A, Kalss G, Leitinger M et al (2016) Two-year real-world experience with perampanel in patients with refractory focal epilepsy: Austrian data. Ther Adv Neurol Disord 9(6):445–453. https://doi.org/10.1177/1756285616661115
Acknowledgements
We sincerely thank the Institute of Epilepsy, Shandong University for their technical and financial assistance.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 81873786).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
The study was approved by the Medical Ethics Committee of Qilu Hospital of Shandong University, and all subjects gave informed consent before participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
**, Y., Zhang, R., Jiang, J. et al. Efficacy and tolerability of lacosamide as adjunctive therapy in patients with focal-onset seizures: an observational, prospective study. Acta Neurol Belg 123, 1081–1087 (2023). https://doi.org/10.1007/s13760-023-02236-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-023-02236-8