Abstract
Introduction
An expert panel of Canadian dermatologists was assembled to develop consensus statements regarding the current landscape of topical therapies for plaque psoriasis and the place in therapy of the recently approved fixed-dose combination halobetasol propionate (HP)/tazarotene (TAZ) lotion (HP/TAZ) in the treatment algorithm for plaque psoriasis.
Method
A modified nominal group technique, which combined both independent and group input from the expert panel, was used to develop the consensus statements. The expert panel completed surveys to elicit their independent views on the current landscape of topical therapies for plaque psoriasis in Canada. The first expert panel session was held to discuss the existing body of literature and develop draft consensus statements about topical therapies and the place in therapy of HP/TAZ. Independent feedback on the draft consensus statements was solicited from expert panel members prior to another expert panel session where the amended consensus statements were further discussed, edited and, finally, voted on.
Results
The expert panel reached consensus on 20 statements.
Conclusion
Expert panel members agreed, based on the existing body of literature, that there is a place in therapy for HP/TAZ to address several current unmet treatment needs of patients with plaque psoriasis. Studies have shown that HP/TAZ is an effective and safe first-line treatment for moderate-to-severe plaque psoriasis. Due to its cosmetically pleasing vehicle and once-daily administration, HP/TAZ may improve patient acceptance and treatment adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Additional and diverse treatment choices in plaque psoriasis should provide patients with more options, which can lead to better outcomes |
An expert panel of Canadian dermatologists was assembled to develop consensus statements on topical therapies and the role of halobetasol propionate/tazarotene (HP/TAZ) |
What was learned from the study? |
Through both independent reflection and group discussions, the expert panel identified the need for more first-line topical therapies for plaque psoriasis |
The consensus statements supported that first-line topical therapy with HP/TAZ addresses several current unmet needs |
Overall, the expert panel found HP/TAZ to be effective and safe for moderate-to-severe plaque psoriasis, offering a convenient treatment option that may improve patient acceptance and adherence |
Introduction
Plaque psoriasis (PsO) is a chronic inflammatory skin condition [1, 2]. Approximately 1–3% of Canadians have PsO [3, 4]. Several rating scales or measures have been developed and validated to measure and stratify PsO severity [5]. The total body surface area (BSA) involved is one of the most commonly used measures, with < 3% BSA involved considered to be mild, 3–10% BSA to be moderate, and > 10% to be severe [5]. Unfortunately, BSA does not reflect plaque characteristics or symptom severity. The Physician Global Assessment (PGA) is a severity rating scale that takes three plaque characteristics (erythema, induration, and scaling) into consideration. It is fairly simple to use in practice and has been used as a primary endpoint in clinical trials (therein referred to as the Investigator’s Global Assessment, or IGA) of PsO treatments [5].
Around 30% of patients are described as having moderate or severe disease [6]. Compared to the general population, individuals with PsO have a greater risk for anxiety and depression, higher mortality rate, and increased work productivity impairment with increasing disease severity [7,8,9]. Individuals with PsO also report work absenteeism rates of 15–19.4 days per year [7, 8, 10]. More than 80% of individuals with PsO feel their condition negatively impacts their quality of life (QoL) [11,12,13]. The disease burden extends into physical, emotional, and psychosocial well-being [1, 14, 15].
Only 13.6% of affected individuals are satisfied with their current treatment [16]. Patients cite lack of response, development of tachyphylaxis, and contraindications as reasons limiting treatment choices [14, 17]. Given the heterogeneity of patients with respect to PsO signs/symptoms, disease severity, and treatment preferences, additional and more diverse treatment choices should provide patients with more options, which are expected to lead to better outcomes. In most Canadian jurisdictions, a difference in accessibility to specialty care versus primary care exists and, therefore, easy-to-use, convenient treatment options may allow for more patients to be successfully treated.
Since PsO is a chronic disease, it usually requires ongoing, long-term management with topical, systemic, and/or light therapies [2]. All approved interventions aim to temper the dysregulated immune response. Common topical therapies include monotherapy or combination therapy with corticosteroids, keratolytics, retinoids, tar-based derivatives, vitamin D analogues, aryl hydrocarbon receptor modulators, and/or phosphodiesterase-4 inhibitors [18].
Corticosteroids, with their immunosuppressive, anti-inflammatory, anti-proliferative, and vasoconstrictive effects, remain widely used. Although potent-to-superpotent topical corticosteroids, such as halobetasol propionate 0.05% (HP), can be efficacious in the short-term, their use as monotherapy may be limited to a duration of 2 weeks as per the product monograph due to the risk of cutaneous adverse events (AEs), such as skin atrophy [19]. Retinoids, with their anti-inflammatory and anti-proliferative effects, can also be used. Tazarotene (TAZ) is the only topical retinoid currently approved for the treatment of PsO in Canada. However, monotherapy is limited by cutaneous AEs, such as local irritation [20].
Halobetasol propionate (HP) 0.01%/tazarotene (TAZ) 0.045% lotion (HP/TAZ; Duobrii™; Bausch Health, Canada Inc., Laval, QC, Canada) is a fixed-dose combination topical therapy consisting of a potent-to-superpotent corticosteroid (HP) and a retinoid (TAZ). Phase II and pivotal phase III clinical trials have demonstrated that HP/TAZ is effective and safe [15, 21,22,23,24]. While the individual use of HP and TAZ as monotherapies is well-established, evidence indicates that a combination of the two provides a synergistic, therapeutic benefit with reduced corticosteroid-induced atrophy and retinoid-associated local irritation [20, 25,26,27]. HP/TAZ combination therapy provides increased efficacy and safety compared to HP and TAZ monotherapies [21].
HP/TAZ, which is indicated in Canada for improving the signs and symptoms of PsO in adult patients with moderate-to-severe disease, received a notice of compliance from Health Canada in 2020 [28]. The purpose of this study is to gather clinician perspective, experience, and knowledge gained since the availability of HP/TAZ in Canada, by convening an expert panel of Canadian dermatologists to deliberate and develop consensus statements on the current topical therapy landscape for PsO in Canada and the place in therapy for HP/TAZ.
Methods
Nominal Group Technique
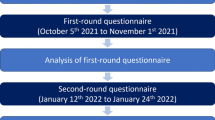
Consensus statements were developed through the modified nominal group technique (NGT). Briefly, this qualitative research approach established consensus in the presence of uncertainty by combining experts’ independent and group reflections [29]. This included the collection of their individual clinical opinions (via survey instrument) on the importance of different treatment outcomes; limitations of the efficacy and safety of currently available topical therapies; patient preferences around treatment characteristics; adherence; unmet needs; and how cost influences treatment. These results were collated, distributed to the expert panel members, and discussed as a group through structured face-to-face virtual sessions (Fig. 1).
Targeted Literature Reviews
An initial targeted literature review was performed by Medlior Health Outcomes Research Ltd. (Medlior; Calgary, AB, Canada), an independent research organization, to identify information related to the topical therapy landscape of PsO and the efficacy, safety, patient adherence/preference, and cost effectiveness of HP/TAZ. A total of 29 publications were identified. A summary of the literature review was provided as an evidence package to the expert panel.
Expert Panel Sessions and Consensus Statement Development
Based on their knowledge, expertise, and experience in PsO treatment and use of HP/TAZ in Canada, seven Canadian dermatologists were selected to participate in an expert panel (with 1 dermatologist serving as the Chair). The independent reflection activity of the modified NGT was facilitated by the distribution of a survey and literature review. Specifically, expert panel members used this material to formulate clinical opinions on the current topical therapy landscape for PsO in Canada. Discussions between the expert panel members with respect to the unmet needs, benefits, and limitations of PsO treatment options occurred during virtual face-to-face expert panel sessions. During the first expert panel session, all participants disclosed any conflict of interest; confirmed the objectives and process; reviewed the literature and survey findings; determined their definition of consensus—requiring six out of seven expert panel members to anonymously vote ‘agree’ or ‘strongly’ agree on a 5-point Likert scale; and discussed as well as composed consensus statements regarding the topical therapy landscape or the place in therapy for HP/TAZ.
Following the first expert panel session, the draft consensus statements were consolidated and circulated among expert panel members, allowing them to provide anonymous individual feedback. In the second expert panel session, the edited and refined draft consensus statements were further discussed and edited by the expert panel members. Finally, an anonymous vote (on 6 December 2021) was conducted allowing expert panel members to score the 20 consensus statements.
Statement of Ethics Compliance
This article is based on previously conducted studies and does not contain any new studies involving human participants or animals.
Results
Consensus Statements
Through independent reflection and group discussion, expert panel members composed 20 statements which all achieved consensus (see Tables 1 and 2 for detailed voting results) based on the current literature as well as their clinical opinions and professional experiences treating patients with PsO. The consensus statements were categorized into two main groups—those pertaining to the general topical therapy landscape (Table 1) and those pertaining specifically to HP/TAZ (Table 2)—with each of the two main groups further organized into four themes (unmet needs, efficacy, safety/limitations, and convenience/acceptability/accessibility).
Discussion
Consensus was achieved amongst expert panel members regarding the place in therapy of HP/TAZ as a unique, efficacious, safe, and convenient first-line treatment option for the management of moderate-to-severe PsO.
Unmet Needs
Plaque psoriasis often negatively impacts the QoL of individuals living with this condition and usually requires ongoing, long-term management [7, 8, 13]. Physical, emotional, and psychosocial aspects of the disease need to be addressed. Many patients with PsO are undertreated, dissatisfied with their treatment, and do not feel that their condition is controlled [11, 12, 16].
While topical corticosteroids have been widely used, long-term management with more potent agents remains challenging as the duration of use is limited to 2–4 weeks due to associated long-term safety concerns, such as skin atrophy [1, 5, 25]. Thus, in Canada, there is an unmet need for accessible, efficacious topical therapies that provide patients with the ability to safely control their disease over the long term [14, 17]. The expert panel unanimously agreed that since PsO is a chronic disease with no cure, there is a need for effective and safe topical therapies that can be used in the long term (Table 1). In addition to being a first-line therapy, the expert panel was also in agreement that HP/TAZ can be used as adjunctive treatment. Based on clinical opinion, they also reported that HP/TAZ may offer an additional treatment option for difficult-to-treat sites (e.g., palms, soles, and scalp [off-label]) (Table 2). Since HP/TAZ has no limits on treatment duration, although a maximum of 50 g per week should be used, this fixed-dose combination therapy addresses the need for a new long-term treatment option that can be used until disease control is achieved.
Safety/Limitations
The expert panel agreed that some current treatment options have limitations, including treatment duration or safety concerns (Table 1). For individual topical therapies, such as potent-to-superpotent corticosteroids (e.g., HP) and retinoids (e.g., TAZ), the primary safety concerns include skin atrophy and local irritation, respectively [1, 5, 20, 25, 30]. Combination formulations may combine complementary mechanisms of action, thus increasing efficacy and mitigating safety concerns for both active ingredients. The expert panel acknowledged the complimentary actions of the HP/TAZ combination, which has greater efficacy than the individual ingredients used alone, agreeing that HP enhances the tolerability of TAZ and TAZ reduces the atrophic potential of HP (Table 2).
The safety of HP/TAZ was demonstrated in the phase II and pivotal phase III clinical trials [15, 21,22,23, 31]. The most frequently reported treatment-emergent adverse event (TEAEs) were application-site reactions, such as dermatitis, pruritus, and pain [21, 23]. Importantly, HP/TAZ had fewer and less severe TEAEs than TAZ alone [21]. Reported AEs were mild-to-moderate in severity over the 12-week assessment period of the phase II and two pivotal phase III clinical trials, as well as during a 52-week phase III clinical trial [21,22,23]. These safety data were consistent with the known safety profiles of HP and TAZ; no new safety concerns were revealed during any of the studies [21,22,23].
One common clinical opinion among the expert panel members was that physicians and patients share a common treatment goal of minimizing AEs. Additionally, there was also agreement among the expert panel that HP/TAZ is generally well-tolerated, and while irritation may occur, it is typically mild in severity (Table 2). Yet in terms of other safety precautions, the expert panel reached consensus that HP/TAZ should not be applied to the face, intertriginous areas, and anogenital region, nor on sites affected by dermatitis/eczema (Table 2). They also agreed that HP/TAZ should not be used in women who are pregnant due to animal studies showing a risk for embryotoxic and teratogenic effects of corticosteroids and TAZ (Table 2).
Another theme from clinical practice was the desire to avoid AEs associated with long-term use of treatments. In a long-term 52-week open-label phase III clinical trial, extended exposure (up to 24 consecutive treatment weeks) did not lead to any added safety concerns [23]. TEAEs occurred primarily during the first 12 weeks and resolved during the course of the study; 22.8% of patients reported TEAEs between weeks 0 and 12, while only 3.7% of patients reported TEAEs between weeks 36 and 52. Skin atrophy was rare, occurring in only 0.7% of patients (N = 555) [23]. Thus, HP/TAZ meets the need for a topical therapy with few safety concerns that can be used as needed long-term.
Efficacy
In 2018, a national survey of Canadians living with moderate-to-severe PSO identified lack of efficacy as the most common cause of dissatisfaction with current treatment [13]. In another patient preference and satisfaction survey, nearly all patients with PsO stated that they would consider using new treatments [16]. The expert panel shared that, in their clinical experience, achieving clear or almost clear skin is a common treatment goal among physicians and patients. Rapid onset of action is important as it may motivate treatment adherence. Efficacious treatments which result in long-term disease control and treatment-free intervals are vital (Table 1). Therefore, they recommended HP/TAZ as an appropriate first-line topical therapy to reduce the signs of psoriasis (erythema, elevation/thickness, and scaling) and BSA, supporting treatment goals of achieving clear or almost clear skin (Table 2) and achieving disease control.
The efficacy of HP/TAZ was demonstrated in the phase II and pivotal phase III clinical trials [15, 21,22,23, 32]. In one phase II and two pivotal phase III clinical trials, HP/TAZ was consistently more effective than its monads or vehicle at achieving treatment success (defined as IGA score of ‘clear’ or ‘almost clear’ [IGA 0/1] with at least a 2-grade improvement from baseline), improving psoriasis signs (erythema, elevation/thickness, and scaling) as well as reducing BSA [15, 21, 22]. Notably, at week 8, 52.5% of patients in the HP/TAZ group had statistically significant superiority in terms of treatment success compared with 33.3% of patients in the HP group (p < 0.05), 18.6% of patients in the TAZ group (p < 0.001), and 9.7% of patients in the vehicle group (p < 0.001) [21]. In addition, HP/TAZ demonstrated statistically significant superiority over vehicle in reducing mean BSA at week 8 (37.6% vs. 3.1% reduction, respectively; p < 0.001) [22]. In the pivotal phase III clinical trials, Dermatology Life Quality Index (DLQI) scores showed improvement in disease-related quality of life for HP/TAZ-treated patients. Specifically, the DLQI score was reduced to a clinically relevant mean (standard deviation) of 4.1 (4.69) at week 8 and 4.6 (5.62) at 4-week post-treatment [compared to 8.2 (5.89) at baseline] [33].
The expert panel also noted that in clinical practice, HP/TAZ demonstrated a rapid onset of action with sustained improvement post-treatment (Table 2), similar to what was seen in published studies. In a phase II clinical trial, HP/TAZ demonstrated statistically significant superiority for treatment success over TAZ and vehicle, with numerical superiority over HP as early as week 2 [21, 34]. In the two pivotal phase III clinical trials, success rates were superior to placebo after 2 weeks and were maintained throughout a 4-week post-treatment period [22, 33, 35]. Further, an open-label, long-term phase III clinical trial demonstrated that, after the achievement of treatment success, over half of patients (55.3%) did not require retreatment for at least 4 weeks, over one quarter of patients (28.3%) did not require retreatment for at least 8 weeks, and nearly one-in-five patients (19.5%) for at least 12 weeks [23].
Convenience/Acceptability/Accessibility
Inconsistent treatment adherence hinders therapeutic success for patients with PsO [36, 37]. Factors that influence treatment adherence include patient satisfaction, cosmetic acceptability, and vehicle properties [36]. In addition, many patients prefer topical therapies over other routes of administration because they offer a sense of being in control of their PsO [16, 38]. The literature findings were echoed by expert panel members’ clinical opinions, which indicated that patients prefer a cosmetically acceptable vehicle with once-daily administration. The expert panel also reached consensus that patients often prefer topical therapies because they give them a sense of control and flexibility (Table 1).
Topical therapies with a once-daily regimen have been shown to nearly double treatment adherence rates when compared to a twice-daily regimen (82% vs. 44%, respectively; p < 0.001) [27, 39]. This evidence was endorsed by the expert panel’s consensus statements on convenience, with members agreeing that patients value a treatment that does not require frequent application (Table 1). They also accepted the premise that HP/TAZ is aesthetically pleasing, hydrating, easily spreadable, and rubs in quickly, with the fixed-dose, once-daily formulation possibly improving treatment adherence by simplifying treatment (Table 2).
A phase II clinical trial found that treatment compliance was 94.9% with the HP/TAZ cohort [21]. The HP/TAZ vehicle uses Prismatrex™ (Bausch Health, Canada Inc.) technology, which results in a non-greasy product designed to provide a more rapid and efficient delivery of active and moisturizing/hydrating ingredients into the skin. As a result, this optimized formulation improves delivery, maximizes therapeutic effects, increases skin moisturization/hydration, restores barrier function, and promotes patient acceptance [27, 32]. A patient perception evaluation found that between 93% and 100% of survey participants responded favorably to the characteristics of the HP/TAZ vehicle (e.g., moisturizing, hydrating, quick absorbing, and aesthetically pleasing) [27].
Finally, with one-fifth of patients having not seen a dermatologist in the past 5 years, localized PsO is often managed by primary care providers [13]. The expert panel agreed with this reality and further highlighted that easy access to topical therapies is needed to enhance disease treatment (Table 1).
Conclusion
Through both independent reflection and group discussions, an expert panel of seven Canadian dermatologists agreed that there is a need for additional first-line topical therapies for PsO. Using robust methods of consensus statement building based on a balanced review of the existing literature interpreted through expert clinical insight, the expert panel composed 20 consensus statements to represent sound guidance on how Canadian physicians currently providing care to patients with PsO can incorporate HP/TAZ appropriately into their treatment algorithms. Specifically, consensus statements supported the premise that first-line topical therapy with HP/TAZ addresses several unmet needs of patients with moderate-to-severe PsO. Furthermore, it was agreed that HP/TAZ is effective, safe, and cosmetically acceptable.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Papp K, Gulliver W, Lynde C, Poulin Y, Ashkenas J. Canadian guidelines for the management of plaque psoriasis: overview. J Cutan Med Surg. 2011;15(4):210–9. https://doi.org/10.2310/7750.2011.10066.
Hsu S, Papp KA, Lebwohl MG, et al. Consensus guidelines for the management of plaque psoriasis. Arch Dermatol. 2022;148(1):95–102. https://doi.org/10.1001/archdermatol.2011.1410.
Papp K, Valenzuela F, Poulin Y, Bernstein G, Wasel N. Epidemiology of moderate-to-severe plaque psoriasis in a Canadian surveyed population. J Cutan Med Surg. 2010;14(4):167–74. https://doi.org/10.2310/7750.2010.09066.
Papp KA, Gniadecki R, Beecker J, et al. Psoriasis prevalence and severity by expert elicitation. Dermatol Ther (Heidelb). 2021;11(3):1053–64. https://doi.org/10.1007/s13555-021-00518-8.
Elmets CA, Korman NJ, Prater F, et al. Joint AAD-NPF Guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J Am Acad Dermatol. 2020;84(2):432–70. https://doi.org/10.1016/j.jaad.2020.07.087.
Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker J. Psoriasis. Lancet. 2021;397(10281):1301–15. https://doi.org/10.1016/S0140-6736(20)32549-6.
Nicholas MN, Gooderham M. Psoriasis, depression, and suicidality. Skin Ther Lett. 2017;22(3):1–4.
Strober B, Greenberg JD, Karki C, et al. Impact of psoriasis severity on patient-reported clinical symptoms, health-related quality of life and work productivity among US patients: real-world data from the Corrona Psoriasis Registry. BMJ Open. 2019;9(4):e027535. https://doi.org/10.1136/bmjopen-2018-027535.
Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80(4):1073–113. https://doi.org/10.1016/j.jaad.2018.11.058.
Levy AR, Davie AM, Brazier NC, et al. Economic burden of moderate to severe plaque psoriasis in Canada. Int J Dermatol. 2012;51(12):1432–40. https://doi.org/10.1111/j.1365-4632.2011.05359.x.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation Surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–5. https://doi.org/10.1001/jamadermatol.2013.5264.
Feldman SR, Goffe BS, Rice G, et al. The challenge of managing psoriasis: Unmet medical needs and stakeholder perspectives. Am Health Drug Benefits. 2016;9(9):504–13.
Canadian Psoriasis Network. Psoriasis journey to stability. National report—Canadians’ journey living with psoriasis. 2018.:2–31. https://www.canadianpsoriasisnetwork.com/wp-content/uploads/2018/09/JTSFinal-r.pdf. Accessed
Kim WB, Jerome D, Yeung J. Diagnosis and management of psoriasis. Can Fam Physician. 2017;63:278–85.
Gold LS, Lebwohl MG, Sugarman JL, et al. Safety and efficacy of a fixed combination of halobetasol and tazarotene in the treatment of moderate-to-severe plaque psoriasis: results of 2 phase 3 randomized controlled trials. J Am Acad Dermatol. 2018;79(2):287–93. https://doi.org/10.1016/j.jaad.2018.03.040.
Green L, Armstrong A, Teller CF, Bell S, Lin T. Treatment of psoriasis: a survey on patient preference and satisfaction. Skin J Cut Med. 2020;4(1):S1–S1.
Segaert S, Calzavara-Pinton P, de la Cueva P, et al. Long-term topical management of psoriasis: the road ahead. J Dermatol Treat. 2020. https://doi.org/10.1080/09546634.2020.1729335.
Maliyar K, Fleming P, Ogunyemi B, Lynde C. A brief history of psoriasis management in Canada. J Cutan Med Surg. 2020;24(3):273–7. https://doi.org/10.1177/1203475420903682.
Uva L, Miguel D, Pinheiro C, et al. Mechanisms of action of topical corticosteroids in psoriasis. Int J Endocrinol. 2012;2012:561018. https://doi.org/10.1155/2012/561018.
Tanghetti E, Lebwohl M, Stein GL. Tazarotene revisited: safety and efficacy in plaque psoriasis and its emerging role in treatment strategy. J Drugs Dermatol. 2018;17(12):1280–7.
Sugarman JL, Stein Gold L, Lebwohl MG, Pariser DM, Alexander BJ, Pillai R. A phase 2, double-blind, randomized, vehicle controlled clinical study to assess the safety and efficacy of a halobetasol/tazarotene fixed combination in the treatment of plaque psoriasis. J Drugs Dermatol. 2017;16(3):197–204.
Sugarman JL, Weiss J, Tanghetti EA, et al. Safety and efficacy of a fixed combination halobetasol and tazarotene lotion in the treatment of moderate-to-severe plaque psoriasis: a pooled analysis of two phase 3 studies. J Drugs Dermatol. 2018;17(8):855–61.
Lebwohl MG, Stein Gold L, Papp K, et al. Long-term safety and efficacy of a fixed-combination halobetasol propionate 0.01%/tazarotene 0.045% lotion in moderate-to-severe plaque psoriasis: phase 3 open-label study. J Eur Acad Dermatol. 2021;35(5):1152–60. https://doi.org/10.1111/jdv.17113.
Ramachandran V, Bertus B, Bashyam AM, Feldman SR. Treating psoriasis with halobetasol propionate and tazarotene combination: a review of phase II and III clinical trials. Ann Pharmacother. 2020;54(9):872–8. https://doi.org/10.1177/1060028020910439.
PrULTRAVATE® halobetasol propionate cream 0.05% w/w, halobetasol propionate ointment 0.05% w/w halobetasol propionate lotion 0.01% w/w Product monograph including patient medication information. Bausch Health, Canada Inc. 2150 St-Elzear Blvd., West Laval, Quebec, H7L 4 A 8 Oct 7, 2020. https://bauschhealth.ca/wp-content/uploads/pdf/Ultravate%20PM-E-2020-10-07.pdf
Bhatia ND, Pariser DM, Kircik L, et al. Safety and efficacy of a halobetasol 0.01%/tazarotene 0.045% fixed combination lotion in the treatment of moderate-to-severe plaque psoriasis: a comparison with halobetasol propionate 0.05% cream. J Clin Aesthet Dermatol. 2018;11(11):15–9.
Tanghetti EA, Stein Gold L, Del Rosso JQ, Lin T, Angel A, Pillai R. Optimized formulation for topical application of a fixed combination halobetasol/tazarotene lotion using polymeric emulsion technology. J Dermatol Treat. 2019;32(4):391–8. https://doi.org/10.1080/09546634.2019.1668907.
PRDUOBRII™ halobetasol propionate and tazarotene lotion 0.01% w/w halobetasol propionate and 0.045% w/w tazarotene Product monograph including patient medication information Bausch Health, Canada Inc. 2150 St-Elzear Blvd., West Laval, Quebec, H7L 4A8 Canada. June 8, 2020. https://pdf.hres.ca/dpd_pm/00056991.PDF
Black N, Murphy M, Lam** D, et al. Consensus development methods: a review of best practice in creating clinical guidelines. J Health Serv Res Policy. 1999;4(4):236–48. https://doi.org/10.1177/135581969900400410.
Murphy G, Reich K. In touch with psoriasis: topical treatments and current guidelines. J Eur Acad Dermatol Venereol. 2011;25(Suppl. 4):3–8. https://doi.org/10.1111/j.1468-3083.2011.04059.x.
Lebwohl MG, Sugarman JL, Gold LS, et al. Long-term safety results from a phase 3 open-label study of a fixed combination halobetasol propionate 0.01% and tazarotene 0.045% lotion in moderate-to-severe plaque psoriasis. J Am Acad Dermatol. 2019;80(1):282–5. https://doi.org/10.1016/j.jaad.2018.09.002.
Lebwohl MG, Tanghetti EA, Stein Gold L, Del Rosso JQ, Gilyadov NK, Jacobson A. Fixed-combination halobetasol propionate and tazarotene in the treatment of psoriasis: narrative review of mechanisms of action and therapeutic benefits. Dermatol Ther. 2021;11(4):1157–74. https://doi.org/10.1007/s13555-021-00560-6.
Stein Gold L, Lain E, Green LJ, Lin T, Israel R. Halobetasol 0.01%/tazarotene 0.045% lotion in the treatment of moderate-to-severe plaque psoriasis: maintenance of therapeutic effect after cessation of therapy. J Drugs Dermatol. 2019;18(8):815–20. https://doi.org/10.1016/j.jaad.2019.06.277.
Stein Gold L, Kircik LH, Pariser D, et al. Rapid onset of action in patients with moderate-to-severe plaque psoriasis with halobetasol 0.01%/Tazarotene 0.045% fixed combination. J Drugs Dermatol. 2018;17(8):863–8.
Lebwohl MG, Stein Gold L, Del Rosso JQ, Green L, Jacobson A. Posttreatment maintenance of therapeutic effect with fixed-combination halobetasol propionate 0.01%/tazarotene 0.045% lotion for moderate-to-severe plaque psoriasis. J Dermatol Treat. 2021. https://doi.org/10.1080/09546634.2021.1914310.
Belinchón I, Rivera R, Blanch C, Comellas M, Lizán L. Adherence, satisfaction and preferences for treatment in patients with psoriasis in the European union: a systematic review of the literature. Patient Prefer Adher. 2016;10:2357–67. https://doi.org/10.2147/PPA.S117006.
Committee C. 2016 Addendum to the Canadian guidelines for the management of plaque psoriasis 2009. J Cutan Med and Surg. 2016;20(5):375–431. https://doi.org/10.1177/1203475416655705.
Vender R, Gooderham MJ, Guenther LC, et al. Canadian patients’ preferences in topical psoriasis care: Insights from the PROPEL surveys. J Cutan Med Surg. 2018;22(5):464–71. https://doi.org/10.1177/1203475418773736.
Zaghloul SS, Goodfield MJD. Objective assessment of compliance with psoriasis treatment. Arch Dermatol. 2004;140(4):408–14. https://doi.org/10.1001/archderm.140.4.408.
Acknowledgements
Medical Writing/Editorial Assistance
Suzanne McMullin, Erin Graves, and Jody Filkowski, all employees of Medlior Health Outcomes Research Ltd., are thanked for the contribution of their expertise and assistance throughout all aspects of the consensus statement development process. Jody Filkowski and Ki-Youn Kim, an independent contractor, each participated in the initial manuscript development. Support for the assistance was funded by Bausch Health, Canada Inc., Laval, QC, Canada.
Funding
This study and the Rapid Service Fee were funded by Bausch Health, Canada Inc., Laval, Quebec, Canada.
Author information
Authors and Affiliations
Contributions
All authors contributed to the expert panel, which included reviewing the literature, responding to surveys, participating in virtual meetings, discussing and voting on consensus statements, as well as reviewing and providing feedback on previous and final versions of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
L. Guenther is on the Speaker’s Bureau of, a consultant for, and/or has received grant/research support from Abbvie, Altana, Amgen, Aslan, Bausch Health, Boehringer Ingelheim, BMS, Celgene, Eli Lilly and Company, Galderma, GSK, Innovaderm, Janssen, Leo Pharma, Merck Frosst, Novartis, Pfizer, Sandoz, Sun Pharma, and UCB. I. Turchin has been advisor, consultant, speaker and/or investigator for Abbvie, Amgen, Arcutis, Aristea, Bausch Health, BMS, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Galderma, Incyte, Janssen, Kiniksa, LEO Pharma, Mallinckrodt, Novartis, Pfizer, Sanofi Genzyme, Sun Pharma, and UCB. R. Vender has received grants and/or research support from, is on the Speaker’s Bureau for, received honoraria from, and/or is a consultant for Abbvie, Actelion, Amgen, Aralez, Arcutis, Bausch Health, Boehringer Ingelheim, BMS, Celgene, Centocor, Cipher, Dermira, Dermavant, Galderma, GSK, Innovaderm, Janssen, Kabi-Care, Leo, Eli Lilly and Company, Meiji, Merck, Novartis, Palladin, Pfizer, Regeneron, Sandoz, Sun Pharma, Takeda, UCB, and Viatris-Mylan. L. Albrecht is on the Speaker’s Bureau of, a consultant for, and/or has received grant/research support or honoraria from Abbvie, Akros, Amgen, Arcutis, Avillion, Bausch Health/Valeant, Boehringer Ingelheim, BMS, Celgene, Centocor, Cutanea, Dermavant, Dermira, Eli Lilly and Company, Galderma, Glenmark, Hoffman-La Roche, Janssen, LEO Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Sanofi Genzyme, UCB, and Valeant/Bausch Health. C. Maari has received honoraria from Bausch Health, Canada Inc. H. Yanofsky has received honoraria from Bausch Health, Canada Inc. V.H. Prajapati has been an advisor, consultant, speaker, and/or investigator for AbbVie, Actelion, Amgen, AnaptysBio, Apogee Therapeutics, Aralez, Arcutis, Arena, Asana, Aspen, Bausch Health/Valeant, Boehringer Ingelheim, BMS, Celgene, Cipher, Concert, CorEvitas, Dermavant, Dermira, Eli Lilly and Company, Galderma, GSK, Homeocan, Incyte, Janssen, LEO Pharma, Medexus, Nimbus Lakshmi, Novartis, Organon, Pediapharm, Pfizer, RAPT Therapeutics, Regeneron, Reistone, Sanofi Genzyme, Sun Pharma, Takeda, Tribute, and UCB.
Ethical approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Additional information
Prior Presentation: This work has been previously presented as a poster at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 2023 Conference on 9 May 2023, in Boston, MA, USA.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Guenther, L., Turchin, I., Vender, R. et al. Canadian Expert Consensus on the Use of Halobetasol Propionate/Tazarotene Lotion for Plaque Psoriasis. Dermatol Ther (Heidelb) (2024). https://doi.org/10.1007/s13555-024-01204-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13555-024-01204-1