Abstract
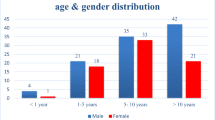
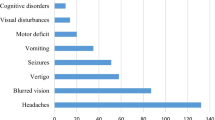
The central and peripheral nervous system cancers are the second most common cancers among the paediatric population (0–14 years). The non-specific symptoms seen in its clinical presentation make the diagnosis of these tumours extremely challenging among children compared to adults. This research study was therefore done to study the socio-demographic profile, clinical features, and management practices among paediatric patients with intracranial tumours. This was a cross-sectional medical record-based study done among 31 children aged < 18 years diagnosed with primary intracranial tumours. Data were recorded using a semi-structured proforma. The median age at diagnosis of tumours among the patients was 7(4, 15) years. Majority of them were males 17(54.8%). Medulloblastoma was the common tumour 12(38.7%). 18(58.1%) tumours originated from the infratentorial region. The most common infratentorial tumour was medulloblastoma, while the most common supratentorial tumour was meningioma. The most common site of involvement was the brainstem 11(35.5%). Majority of the tumours were presently in Stage III/IV 20(64.5%). The most common symptom was vomiting 18(58.1%). 23(74.2%) patients were managed using chemotherapy and among them the most used drug was Temozolomide 7(30.4%). Medulloblastoma was present more among patients who were diagnosed at the age ≤ 5 years (p = 0.022). Tumours involving the cerebellum were more among females (p = 0.0118). Headache was present more among patients who were diagnosed with tumours at the age > 5 years compared to the age ≤ 5 years (p = 0.0119). From the findings of this study, it can be concluded that majority of the patients were males. Medulloblastoma was the most common tumour. Close to two-third of the tumours were in Stage III/IV. The most common symptom reported was vomiting. The most used drug for treatment was Temozolomide.
Similar content being viewed by others
Data Availability
The SPSS spread sheet containing the research data is available with the corresponding author.
References
Sathishkumar K, Chaturvedi M, Das P, Stephen S, Mathur P (2022) Cancer incidence estimates for 2022 & projection for 2025: Result from National Cancer Registry Programme, India. Indian J Med Res 156:598–607
Trivedi PP, Goel DK, Mehta SP, Jetly DH (2019) An epidemiological study of paediatric central nervous system (CNS) tumours in Gujarat cancer research institute, Ahmedabad. Indian J Pathol Oncol 6:642–646
Dwivedi R, Sudhapriya P, Padmavathi P, Sharma V, Rameshchandra VV, Prasad BCM et al (2019) Epidemiological analysis of central nervous system tumors in pediatric patients from a tertiary care centre in India. Int J Contemp Pediatr 6:2697–2703
Curtin SC, Minino AM, Anderson RN (2016) Declines in Cancer Death Rates Among Children and Adolescents in the United States, 1999–2014. NCHS Data Brief 257:1–8
Alias H, Morthy SK, Zakaria SZS, Muda Z, Tamil AM (2020) Behavioral outcome among survivors of childhood brain tumor: a case control study. BMC Pediatr 20:53
Stanic D, Grujicic D, Pekmezovic T, Bokun J, Popovic-Vukovic M, Janic D et al (2021) Clinical profile, treatment and outcome of pediatric brain tumors in Serbia in a 10-year period: A national referral institution experience. PLoS ONE 6:e0259095
Walker D, Hamilton W, Walter FM, Watts C (2013) Strategies to accelerate diagnosis of primary brain tumours at the primary-secondary care interface in children and adults. CNS Oncol 2:447–462
Gandhi S, Meena A, Harsh A, Choudhary S, Meena SK, Dhayal S (2022) A Cross Sectional Study of Clinical and Histopathological Spectrum of Pediatric Brain Tumours. Saudi J Pathol Microbiol 7:186–192
Madhavan R, Kannabiran BP, Nithya AM, Kani J, Balasubramaniam P, Shanmugakumar S (2016) Pediatric brain tumors: An analysis of 5 years of data from a tertiary cancer care center, India. Indian J Cancer 53:562–565
Govindan A, Parambil RM, Alapatt JP (2018) Pediatric intracranial tumors over a 5-year period in a tertiary care center of North Kerala, India: A retrospective analysis. Asian J Neurosurg 13:1112–1117
Suresh SG, Srinivasan A, Scott JX, Rao SM, Chidambaram B, Chandrasekar S (2017) Profile and outcome of pediatric brain tumors – Experience from a tertiary care pediatric oncology unit in South India. J Pediatr Neurosci 12:237–244
Kim HI, Lim H, Moon A (2018) Sex differences in cancer: epidemiology, genetics and therapy. Biomol Ther (Seoul) 26:335–342
Bhat S, Yadav SP, Suri V, Patir R, Kurkure P, Kellie S et al (2011) Management of childhood brain tumors: consensus report by the Pediatric Hematology Oncology (PHO) Chapter of Indian Academy of Pediatrics (IAP). Indian J Pediatr 78:1510–1519
Jaiswal J, Shastry AH, Ramesh A, Chickabasaviah YT, Arimappamagan A, Santosh V (2016) Spectrum of primary intracranial tumors at a tertiary care neurological institute: A hospital-based brain tumor registry. Neurol India 64:494–501
American Cancer Society. Radiation Therapy for Brain and Spinal Cord Tumors in Children (2023) https://www.cancer.org/cancer/types/brain-spinal-cord-tumors-children/treating/radiation-therapy.html. Accessed 6 June 2023
Albright AL, Sposto R, Holmes E, Zeltzer PM, Finlay JL, Wisoff JH et al (2000) Correlation of neurosurgical subspecialization with outcomes in children with malignant brain tumors. Neurosurgery 47:879–885 (discussion 885-887)
Dana-Farber Cancer Institute. What Are the Differences Between Adult and Childhood Brain Tumors? (2017) Available from: https://blog.dana-farber.org/insight/2015/05/what-are-the-differences-between-adult-and-childhood-brain-tumors/#:~:text=Childhood%20brain%20tumors%20are%20less,a%20brain%20tumor%20will%20survive. Accessed 6 December 2022
Mostoufi-Moab S, Grimberg A (2010) Pediatric brain tumor treatment: growth consequences and their management. Pediatr Endocrinol Rev 8:6–17
Acknowledgements
We thank the Medical Superintendent of Kasturba Medical College Hospital, Attavar, Mangalore for permitting us to access the medical records of paediatric patients with primary intracranial tumours.
Funding
None.
Author information
Authors and Affiliations
Contributions
NJ: guarantor of this research work, concept, literature search, tool preparation, data analysis, manuscript preparation, revising the work critically for important intellectual content.
RSR: literature search, data interpretation, manuscript editing, revising the work critically for important intellectual content.
PARS: literature search, data collection, manuscript editing, revising the work critically for important intellectual content.
L: literature search, data collection, manuscript editing, revising the work critically for important intellectual content.
AR: literature search, data collection, manuscript editing, revising the work critically for important intellectual content.
VG: literature search, data collection, manuscript editing, revising the work critically for important intellectual content.
This manuscript has been read and approved by all the authors.
Corresponding author
Ethics declarations
Ethical Approval
Permission to conduct this study was taken from the Institutional Ethics Committee dated 18th March 2021. The protocol number was IEC KMC MLR 11–19/123.
Informed Consent to Participate
Not applicable as it is a record-based study.
Consent to Publish
Not applicable as it is a record-based study.
Competing Interests
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joseph, N., SR, R., Sagar, P.A.R. et al. Clinico-Demographic Profile of Paediatric Patients with Primary Intracranial Tumours in South India. Indian J Surg Oncol (2024). https://doi.org/10.1007/s13193-024-01988-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13193-024-01988-w