Abstract
Objectives
Preliminary research on self-compassion as a target for reducing forms of bias is promising, yet healthcare provider self-compassion has not yet been explored in relationship to weight bias. Healthcare providers commonly endorse weight stigma and bias, contributing to health disparities for patients with “obesity.” The current study explores the feasibility of the self-compassion loving kindness meditation (LKM) as a brief intervention that reduces weight bias in nursing students.
Method
Participants (189 nursing students) were randomly assigned to the LKM condition or body scan control condition before engaging in an implicit bias task and answering self-report measures of internalization of the thin ideal, weight bias, positive attitudes towards people with “obesity,” positive emotions, self-compassion, cognitive flexibility, and compassionate care.
Results
Statistically significant differences in self-compassion, cognitive flexibility, weight bias, and compassionate care failed to be found between the groups. Participants in the LKM condition endorsed significantly higher levels of positive emotionality compared to the control condition. Higher levels of self-compassion were related to lower levels of weight bias for participants in both conditions. Multiple linear regression analyses revealed that internalization of the thin ideal and self-compassion accounted for 19.2% of the variance in positive attitudes towards people with “obesity.”
Conclusions
This study suggests the importance of examining self- and other-compassion in the context of weight stigma. Its findings exemplify the complexity of weight stigma and the need to further explore the mechanisms to be targeted to effectively reduce healthcare professionals’ bias.
Pre-registration
This study is not preregistered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
While several definitions of self-compassion exist in the literature, Neff (2003) posits that self-compassion is composed of three elements, including self-kindness (i.e., kindness towards ourselves, particularly when we fail), common humanity (i.e., recognition that suffering is a shared experience), and mindfulness (i.e., non-judgmentally observing our current emotional and cognitive state). Neff (2003) further explains that these three elements can be further understood in contrast to their opposing principles, which are self-judgment (self-kindness), isolation (common humanity), and overidentification (mindfulness). Self-compassion research has expanded greatly in the last decade, with over 100 empirical studies examining how a positive, affirmative, non-judgmental attitude towards oneself enhances mental and physical health (e.g., Chio et al., 2021; Ferrari et al., 2019). More specifically, moderate to large effect sizes have been found between self-compassion and outcomes such as overall global health, sleep, depression, anxiety, and psychopathology (e.g., Kılıç et al., 2021; MacBeth & Gumley, 2012; Phillips & Hine, 2021). Consequently, increasing attention has been drawn towards the feasibility and efficacy of self-compassion interventions for a variety of intra- and interpersonal outcomes.
Brief self-compassion interventions have demonstrated significant improvement in psychological well-being in adults with and without previous meditation experience (Baer et al., 2012). Furthermore, higher levels of self-compassion have been found to be related to more perspective-taking, compassion for humanity, empathic concern, and altruism in adults (Neff & Pommier, 2013). Positive, significant effects of a self-compassion intervention (i.e., the loving kindness meditation) on one’s compassion towards the self and others as compared to a control condition (i.e., sitting quietly) also have been demonstrated (Polizzi et al., 2022). Recent literature is starting to evince the efficacy of self-compassion interventions for improving interpersonal relationships (i.e., compassionate care), including between healthcare providers and their patients (Rao & Kemper, 2017). Furthermore, preliminary research suggests the feasibility of these interventions for specifically addressing and reducing racial bias (Stell & Farsides, 2016). Self-compassion interventions, therefore, may be a viable route for addressing bias-related concerns in the patient-provider relationship and improving compassionate care for patients.
One type of bias that has received increasing attention in the literature is weight stigma, which is defined as the “social devaluation and denigration of people perceived to carry excess weight” (Tomiyama, 2014, p. 8). The detrimental impact of weight stigma on the well-being of people with higher weight has been well established, including associations with poorer self-esteem, overall health, body esteem, and social support, as well as increased loneliness, depression, and anxiety for individuals with “overweight” or “obesity” (Phelan et al., 2015). Furthermore, experiences of weight stigma are related to negative co** behaviors in people with higher weight, such as emotional eating, negative self-talk, social isolation, and avoidance of exercising in public (Carels et al., 2018; Lewis et al., 2011). Research also has demonstrated that exposure to weight-stigmatizing situations is associated with shifts in self-perception of one’s ability to control eating, self-reported health, and risk for being subjected to stigma (Hunger & Major, 2015; Major et al., 2014). These negative psychological outcomes together with negative co** behaviors may contribute to the ongoing struggle with weight, further contributing to poorer overall well-being for people with higher weight (Carels et al., 2018; Sikorski et al., 2015).
Unfortunately, healthcare providers of individuals with higher weight are one of the most common sources of weight stigma (Puhl & Brownell, 2006). It is estimated that between 65 and 98% of healthcare professional trainees hold stigmatizing beliefs about patients with “overweight” or “obesity” (Blanton et al., 2016; Puhl et al., 2014; Swift et al., 2013), and these beliefs have been found to be associated with differential care for these patients (e.g., attributing all health issues to weight; Gudzune et al., 2014). Consequently, some patients with “obesity” would rather avoid medical appointments altogether rather than receive the services and care they need in order to avoid stigma from their healthcare provider (e.g., Alberga et al., 2019). Therefore, it is essential to identify ways to address the perpetuation of weight stigma in patient-provider relationships so that patients can safely and comfortably engage in this important aspect of their overall care. In the current study, “higher weight” will be used to describe individuals who have been diagnosed with “overweight” or “obesity” in the medical setting as an attempt to not further perpetuate the stigma associated with this terminology. However, research studies that have utilized the language of “overweight” and “obesity” will be cited as such in order to accurately communicate their findings, although the problematic nature of this language is recognized.
Several factors have been found to be associated with weight stigma in healthcare providers, such as beliefs about the etiology of “obesity,” level of empathy for patients, and perceptions of control over “obesity” (Cohen & Persky, 2019; Jung et al., 2015; Khan et al., 2018; Phelan et al., 2015). As such, research has begun to explore the role of psychoeducational interventions that target beliefs about the etiology of “obesity” and perceptions of control over “obesity” for mitigating weight bias in healthcare providers (e.g., Diedrichs & Barlow, 2011). While results indicated some improvement in weight stigma from these interventions, there is a need for interventions that address the complex, multi-faceted nature of this stigma.
Inducing empathy and promoting perspective taking may be favorable methods to reduce weight bias given the use of these strategies to reduce other forms of bias (e.g., HIV-related bias in the LGBT+ community; Gloor & Puhl, 2016). Furthermore, people who have greater empathy for individuals with higher weight are less likely to demonstrate weight stigma (Khan et al., 2018). Additionally, induction of positive, other-regarding emotions (Griskevicius et al., 2010) and cognitive flexibility (i.e., the ability to react flexibly in unexpected situations or changing environments; Moore & Malinowski, 2009) have been found to be related to shifts in cognitive processing that are associated with decreased implicit bias. Therefore, interventions aimed at increasing empathy, positive other-regarding emotions, and cognitive flexibility could result in the reduction of implicit weight bias. Since prior research has demonstrated the relationship between self-compassion and empathy, positive emotions, and cognitive flexibility (Moore & Malinowski, 2009; Seppala et al., 2014; Shahabi et al., 2019), the potential for self-compassion interventions for mitigating bias is promising.
Societal messages related to “ideal” body types also influence one’s perception of higher weight. The thin ideal represents the societal definition of an attractive female body as slim and having little body fat. Internalization of the thin ideal is the “extent to which an individual cognitively ‘buys into’ socially defined ideals of attractiveness and engages in behaviors designed to produce an approximation of these ideals” (Thompson & Stice, 2001, p. 181). This internalization has been found to be related to body dissatisfaction, dieting, and negative affect, further contributing to disordered eating behaviors (Dondzilo et al., 2019; Low et al., 2003). While the negative impact of this internalization on physical and emotional well-being is well established, there is a lack of literature exploring the impact of this internalization on one’s perspectives of others with higher weight. Therefore, there is a need for research exploring the influence of this internalization on the efficacy of interventions aimed to mitigate weight stigma.
One empirically supported intervention that has promise for improving the patient-provider relationship is the loving kindness meditation (LKM). The LKM has been found to be associated with improved positive emotions, confidence in providing compassionate care, social connectedness, and empathy (Rao & Kemper, 2017; Seppala et al., 2014), all of which relate to the patient-provider relationship. Furthermore, the LKM may be a viable option for reducing bias by increasing cognitive flexibility, resulting in individuals not relying on stereotypes or faulty thinking when engaging with patients’ minoritized identities (e.g., Shahabi et al., 2019). Notably, the LKM is not self-compassion alone, but rather one of many avenues for increasing self-compassion.
The current study aimed to explore the efficacy of the LKM for reducing weight bias in nursing students, specifically, by increasing self-compassion, positive, other-focused emotions, and cognitive flexibility, in order to improve compassionate, affirmative care. Nurses make up the largest proportion of healthcare providers in the USA, and nurses are at the forefront of healthcare for patients with higher weight. Consistent with the literature on weight bias in healthcare providers broadly, nurses also endorse these biases (Garcia, 2012). Given the potential challenge of inducing changes in weight bias, we also aimed to improve compassionate care through the LKM separate from a shift in weight bias.
Method
Participants
Participants were recruited through the National Student Nurses’ Association, Inc. (NSNA) listserv. This NSNA is a national non-profit organization with over 60,000 pre-RN (registered nurse) students enrolled in associate, baccalaureate, and diploma nursing programs. To be included in the current study, participants must have been at least 18 years old, proficient in reading, listening, and writing English, enrolled part-time or full-time in a nursing training program, and have access to a desktop or laptop computer with audio and/or speakers. Participants who completed the survey were entered in a raffle to win 1 of 10 US$15 electronic gift cards.
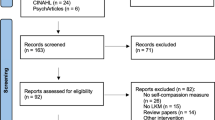
In addition to excluding 176 participants who prematurely terminated the survey, one participant also was excluded from the study due to questionable validity check responses as well as excessive speed on the IAT (Fig. 1). The final sample included 189 participants, and select demographic information is included in Table 1. Participants were randomly assigned to condition, with 80 participants in the intervention condition and 109 participants in the control condition.
Procedure
A brief description of the study, inclusion criteria, risks and benefits, compensation, secure Qualtrics survey link, and contact information were sent via email to the NSNA listserv. After participants clicked on the survey link, they were directed to the informed consent page. Those who provided consent were directed to the demographic questionnaire and the Sociocultural Attitudes Towards Appearance Questionnaire – 4 (SATAQ-4) Thin/Low Body Fat subscale. Next, participants were randomly assigned to the loving kindness meditation or body scan meditation using the Qualtrics randomization function.
Both meditations began with an introduction for participants to sit comfortably, close their eyes, relax, and take several deep breaths. The LKM consisted of a 10-min guided meditation recorded by the first author. The script for the LKM was adapted from Kristin Neff’s loving kindness meditation (2020) and adjusted to match the methodology of Stell and Farsides (2016). Participants were directed to repeat loving kindness phrases (e.g., “May you have health,” “May you be happy,” “May you be well.”) to themselves, someone they care deeply for, and someone they have neutral feelings towards. Similar to Stell and Farsides (2016), in the final round of loving kindness phrases, participants were instructed to open their eyes. They were presented with a photograph of a woman with higher weight and then prompted to direct loving kindness phrases to this person (e.g., health, happiness, wellness).
Instead of having an inactive control group, mindfulness meditation was used to specifically explore the utility of the compassion component of the LKM for reducing weight bias. The mindfulness meditation consisted of a 10-min body scan guided meditation that was adapted from an online audio-recording (Yvonne, 2016). Participants were directed to scan their bodies, starting at their toes and moving to the crown of their heads. They were directed to notice specific parts of their body as they sit in a chair. To keep this condition as similar as possible to the intervention condition, participants were instructed to open their eyes at the end of the body scan meditation. They were presented with a photograph of a woman with a higher weight and then prompted to pay attention to the physical features of the woman’s face.
Several methods were utilized to confirm that participants engaged in the meditations. First, participants were not shown the “Next” button until adequate time had passed for them to listen to the meditation. Additionally, participants were screened out of the meditation if they spent more than 20 minutes on the meditation page. They were asked to list at least one loving kindness phrase they repeated (i.e., LKM condition) or to describe the place in their body where they noticed the most tension (i.e., body scan control condition). Finally, all participants were asked an open-ended question about how they felt in their bodies following the meditation.
Following completion of the meditation, participants completed the weight Implicit Association Test (IAT) within Qualtrics, which was created using the ShinyApp online platform. IAT blocks were randomized so that they were not presented in the same order for all participants (Carpenter et al., 2019). Participants then completed the post-measures in the following order: Modified Differential Emotions Scale (mDES), Cognitive Flexibility Inventory (CFI), Self-Compassion Scale – Short Form (SCS-SF), Compassion Competence Scale (CCS), Attitudes Towards Obese Persons (ATOP), and demographic questions. At least one validity check was interspersed throughout the post-measures.
Measures
Demographic Variables
Participants were asked various demographic questions including their age, racial/ethnic identity, gender identity, sexual orientation, highest level of education, current degree program, year in the program, enrollment status, approximate number of hours of clinical experience, intention for pursuing a career in a nursing specialty area, body size, and previous meditation experience.
Internalization of the Thin Ideal
Internalization of the thin ideal was measured using the Thin/Low Body Fat subscale of the Sociocultural Attitudes Towards Appearance Questionnaire – 4 (SATAQ-4; Schaefer et al., 2015). The SATAQ-4 is intended to measure the sociocultural factors that influence appearance ideals. The Thin/Low Body Fat subscale of the SATAQ-4 consists of five items for which participants indicate their level of agreement using a 5-point Likert scale (e.g., “I want my body to look very thin.”). Higher total scores on the Thin/Low Body Fat subscale indicate higher levels of internalization of the thin ideal (i.e., a thin figure with little body fat). Scores for the Thin/Low Body Fat subscale have demonstrated adequate internal consistency (α = 0.87), and prior validation studies have indicated convergent and construct validity (Schaefer et al., 2015). In the current study, Cronbach’s α was 0.78 and McDonald’s ω was 0.80.
Weight Bias
Participants’ weight bias was assessed using the weight Implicit Association Test (IAT; Greenwald et al., 1998). Broadly, the IAT measures the strength of relationships between concepts and evaluations or stereotypes (Project Implicit, 2011). Participants were first asked to sort images of people with lower weight and people with higher weight based on the associated categories (i.e., fat people, thin people). They were then asked to sort positively and negatively valenced words (e.g., athletic, clumsy) based on the associated categories (i.e., good, bad). Finally, the first two conditions were combined so that participants must sort images and positively and negatively valenced words based on the combined categories (e.g., fat people/good, thin people/bad). Participants were presented with blocks of stimuli using both pairings of the categories. The IAT is based on the assumption that sorting is easier when participants are doing so in a manner that is consistent with their implicit mental associations. Raw data was inputted into the iatgen software to calculate a D-score for each participant to represent their level of weight bias. A D-score of zero indicated no bias, a positive D-score indicated a preference for people with lower weight, and a negative D-score indicated a preference for people with higher weight (Carpenter et al., 2019). Scores on the IAT demonstrated adequate internal consistency (α = 0.81) as well as convergent and discriminant validity in initial validation studies (Nosek & Smyth, 2007).
Positive Emotions
The Modified Differential Emotions Scale (mDES; Fredrickson et al., 2003) was used to assess levels of positive emotions. The Positive Emotions subscale was utilized for the current study. Per the methodology used in previous research exploring the role of the LKM in reducing racial bias (Stell & Farsides, 2016), the directions for the scale were modified to direct participants to focus on their emotional experience during the meditation (i.e., “During the meditation exercise, I felt [positive emotion].”). Participants indicated their agreement with each statement on a 5-point Likert scale. The Positive Emotions subscale was separated into positive, other-regarding and positive, non-other-regarding emotions per the methodology of Stell and Farsides (2016). Positive, other-regarding emotions include gratitude, elevation, love, and awe, and scores on these items have demonstrated adequate internal consistency (α = 0.92). Positive, non-other-regarding emotions include amusement, buoyancy, hope, curiosity, happiness, pride, and contentment, and scores on these items have also demonstrated adequate internal consistency (α = 0.85; Stell & Farsides, 2016). Total scores were calculated for both positive, other-regarding and positive, non-other-regarding emotions. Higher total scores were indicative of greater positive emotionality during the meditations. In the current study, both scales demonstrated acceptable inter-item consistency and reliability (positive, other-regarding emotions: α = 0.86, ω = 0.87; positive, non-other-regarding emotions: α = 0.84, ω = 0.85).
Cognitive Flexibility
The Cognitive Flexibility Inventory (CFI; Dennis & Vander Wal, 2010) was used to assess participants’ cognitive flexibility. The CFI consists of 20 items rated on a 7-point Likert scale to measure three components of cognitive flexibility: “(1) the tendency to perceive difficult situations as controllable, (2) the ability to perceive multiple alternative explanations for life occurrences and human behavior, and (3) the ability to generate multiple alternative solutions to difficult situations” (Dennis & Vanderwal, 2010; p. 241). The Control subscale measures the first aspect of cognitive flexibility (i.e., perceiving situations as controllable; “I often look at situations from different viewpoints.”) and the Alternatives subscale measures the latter two aspects of cognitive flexibility (i.e., ability to both perceive and generate multiple explanations for difficult situations; “I consider multiple options before making a decision.”). Lower total scores on the CFI as well as the Alternatives and Control subscales are indicative of greater cognitive rigidity whereas higher scores are indicative of greater cognitive flexibility. Scores on the CFI have demonstrated strong internal consistency (α = 0.90–0.91) and high 7-week test-retest reliability (r = 0.81), as well as convergent, construct, and concurrent validity in an undergraduate population from a Midwestern university (Dennis & Vander Wal, 2010). Cronbach’s a in the current study were 0.84 (Control subscale), 0.87 (Alternatives subscale), and 0.86 (total score). McDonald’s ω in the current study were 0.86 (Control subscale), 0.87 (Alternatives subscale), and 0.83 (total score).
Self-Compassion
Self-compassion was assessed using the Self-Compassion Scale – Short Form (SCS-SF; Raes et al., 2011). The SCS-SF consists of 12 items rated on a 5-point Likert scale that assess an individual’s sense of common humanity (e.g., “I try to see my failings as part of the human condition.”), mindfulness (e.g., “When something painful happens I try to take a balanced view of the situation.”), and self-kindness (e.g., “I try to be understanding and patient towards those aspects of my personality I don’t like.”). Higher total mean scores on the SCS-SF indicate higher levels of self-compassion. Scores on the SCS-SF have demonstrated adequate internal consistency (α ≥ 0.86; Raes et al., 2011). Furthermore, the SCS-SF is strongly correlated with the full Self-Compassion Scale (r ≥ 0.97), which has demonstrated predictive validity for well-being, convergent validity with a single-item measure of self-compassion, discriminant validity with social desirability and self-criticism, and construct validity for perceived competence, fear of failure, and body appreciation (Neff, 2016; Neff & Tóth-Király, 2022). In the current study, both Cronbach’s α and McDonald’s ω were 0.83.
Compassionate Care
Compassionate care was measured using the Compassion Competence Scale (CCS; Lee & Seomun, 2016). The CCS consists of 17 questions for which participants indicated their level of agreement using a 5-point Likert scale (e.g., “I am careful in my speech and behaviors so as to avoid hurting my patient’s feelings.”). Higher average scores on the CCS indicate higher levels of compassionate care. The scale has demonstrated face validity, content validity, and convergent validity, and scores on the scale have demonstrated adequate internal consistency (α = 0.91) and adequate 2-week test-retest reliability (r = 0.80; Lee & Seomun, 2016). Both Cronbach’s α and McDonald’s ω were 0.86 in the current study.
Attitudes Towards “Obesity”
Participants’ positive attitudes towards people with “obesity” were assessed using the Attitudes Toward Obese Persons scale (ATOP; Allison et al., 1991). The scale included 20 items assessing the degree to which participants agree with statements about people with “obesity” using a 6-point Likert scale (e.g., “Obese people are often less aggressive than nonobese people.” and “Obese people should not expect to lead normal lives.”). Total scores were calculated, and higher scores reflected positive attitudes towards people with “obesity.” In initial validation studies, the scores for the ATOP demonstrated excellent internal consistency (α = 0.81 for graduate students, 0.80 for undergraduate students, and 0.84 for members of the National Association to Advance Fat Acceptance) and construct and discriminant validity (Allison et al., 1991). In the current study, both Cronbach’s α and McDonald’s ω were 0.85.
Data Analyses
All data were analyzed using SPSS Version 27.0 software. Demographic data was examined using chi-square tests to assess baseline differences between control and intervention groups. Pearson’s bivariate correlations were computed for all continuous study variables. A one-way analysis of variance (ANOVA) was used to assess the effect of treatment on study variables. Statistical assumptions of ANOVA were assessed using recommendations by Gamst et al. (2008), and assumptions were met for testing for independence, normality, and homogeneity of variance. Therefore, a one-way ANOVA was used without adjustment. A multiple linear regression was calculated to predict participants’ attitudes towards people with “obesity,” specifically for the intervention condition. Statistical assumptions of multiple linear regression were assessed using recommendations by Tabachnick and Fidell (2013), and assumptions of independence of residuals, normality, linearity, and homoscedasticity were met. Therefore, a multiple linear regression was used without adjustment.
Results
Participants (n = 189) had a mean age of 29.77 (SD = 10.39) and the majority identified as White (75.1%), women (95.8%), and straight (88.4%). Most participants were enrolled full-time (86.8%) in a Bachelor of Science in Nursing program (73.5%) and identified as smaller-bodied (38.1%). Furthermore, most participants reported having previous meditation experience (75.1%).
Pearson’s bivariate correlations revealed a statistically significant, positive correlation between self-compassion and positive attitudes towards people with “obesity” for participants in the intervention (r = 0.36, p < 0.01) and control conditions (r = 0.27, p < 0.01). Descriptive statistics for study variables by condition can be found in Table 2. A one-way ANOVA was used to examine the baseline differences between the intervention and control groups with regard to study variables, and results indicated a statistically significant difference between the groups on the SATAQ-4, F(1, 187) = 3.90, p = 0.05, ηp2 = 0.02, with higher levels of internalization of the thin ideal for the intervention group (M = 16.67, SD = 3.97) compared to the control group (M = 15.43, SD = 4.48) at baseline (Table 3). A one-variable chi-square test did not indicate statistically significant differences between groups for prior meditation experience (c2 = 0.09, p = 0.76).
A one-way ANOVA was used to examine the differences between the intervention and control groups for self-compassion, compassionate care, weight bias, positive attitudes towards people with “obesity,” positive emotionality, and cognitive flexibility (Table 3). A statistically significant effect of treatment was found for the Positive, Other-Regarding Emotions subscale of the mDES, F(1, 187) = 27.40, p < 0.001, ηp2 = 0.13, with greater levels of positive, other-regarding emotions for the intervention group (M = 9.48, SD = 3.41) compared to the control group (M = 6.61, SD = 3.92). Additionally, a statistically significant effect of treatment was found on the Positive, Non-Other-Regarding Emotions subscale of the mDES, F(1, 187) = 15.47, p < 0.001, ηp2 = 0.08. The intervention group demonstrated significantly higher levels of positive, non-other-regarding emotions (M = 14.83, SD = 4.98) compared to the control group (M = 6.61, SD = 3.92). Statistically significant differences were not found between groups for self-compassion [F(1, 187) = 0.01, p = 0.91], compassionate care [F(1, 187) = 0.01, p = 0.93], weight bias [F(1, 186) = 0.83, p = 0.36], positive attitudes towards people with “obesity” [F(1, 187) = 0.78, p = 0.38], or cognitive flexibility [F(1, 187) = 0.35, p = 0.56].
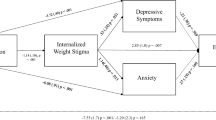
Post hoc analyses were conducted to better understand constructs that predict attitudes towards people with “obesity” for the intervention group to inform future studies. The model fit was significant for attitudes towards people with “obesity,” F (2, 79) = 9.13, p < 0.001 (Table 4). Both self-compassion (b* = 0.62, p = 0.01) and internalization of the thin ideal (b* = −0.99, p = 0.02) predicted attitudes towards people with “obesity.” According to these results, participants in the intervention condition with higher levels of self-compassion reported more positive attitudes towards people with “obesity.” Additionally, participants in the intervention condition with lower levels of internalization of the thin ideal reported more positive attitudes towards people with “obesity.” Together, these variables predicted 19.2% of the variance in attitudes towards people with “obesity” for participants in the intervention condition.
Discussion
This study aimed to explore the feasibility of the LKM for reducing weight bias in nursing students by increasing self-compassion, positive, other-focused emotions, and cognitive flexibility. Prior research indicates that LKM has promise for improving the patient-provider relationship given its association with improved positive emotions, confidence in providing compassionate care, social connectedness, and empathy (Rao & Kemper, 2017; Seppala et al., 2014). Furthermore, preliminary evidence suggests the feasibility of this intervention for decreasing implicit racial bias (Stell & Farsides, 2016). Based on literature searches using multiple databases (e.g., PsychInfo, Google Scholar) and including multiple languages (i.e., not excluding languages in the search options), this study is the first to examine the use of the LKM for reducing weight bias in healthcare providers.
Findings supported the hypothesis that participants in the LKM intervention condition would demonstrate significantly higher positive emotions compared to participants in the meditation control condition. Our findings align with prior research demonstrating the utility of the LKM for increasing positive emotions and address prior limitations by demonstrating the effectiveness of the LKM as compared to an active control group (Zeng et al., 2015). As a result, our findings provide preliminary evidence that the LKM may be more effective than mindfulness meditations alone for increasing positive emotionality. These findings also indicate that the LKM increases positive emotionality towards the self as well as others, which is an important consideration for addressing issues within the patient-provider relationship. The unique components of the LKM (i.e., guiding listeners to send love, kindness, and compassion towards the self and others) appear to be the active ingredients for increasing positive emotionality rather than mindfulness alone. Given the plethora of research indicating concerns with provider well-being and burnout (e.g., Shanafelt et al., 2012), it is necessary to identify interventions that can support providers on intrapersonal and interpersonal levels, such as the LKM.
Notably, both self-compassion and internalization of the thin ideal were found to be significant predictors of positive attitudes towards people with “obesity”. Prior research has demonstrated that a strong preference for thin bodies is strongly associated with one’s own internalization of the thin ideal, dietary restraint, and body dissatisfaction (Dondzilo et al., 2019). Also, the relationship between self-compassion and one’s own body appreciation, body acceptance, and lower disordered eating has been established (Slater et al., 2017; Tylka et al., 2015). However, there is a paucity of research examining the impact of self-compassion and internalization of the thin ideal on one’s perception of others’ bodies. The current study provides preliminary evidence for the impact of one’s own intrapersonal challenges related to weight/body size and self-compassion on attitudes towards people with “obesity,” which may be an important consideration for future weight bias interventions.
Incongruent with our hypotheses, statistically significant differences were not found between conditions for self-compassion, weight bias, positive attitudes towards people with “obesity”, cognitive flexibility, or compassionate care. Specifically for weight bias, it was hypothesized that the LKM would effectively target the cognitive and emotional processes of weight stigma to reduce this bias in nursing students given that psychoeducation-based interventions have been only somewhat effective in addressing weight bias in pre-service health students (Diedrichs & Barlow, 2011). These insignificant results suggest that the one-time, 10-minute intervention was not robust enough to elicit significant differences in these outcome variables for participants in the intervention condition as compared to the control condition, particularly given the complexity and social acceptability of weight stigma (Puhl & Heuer, 2010). Furthermore, baseline data was not collected to avoid priming participants to the purpose of the study and risking practice effects. However, we are unable to assess if there were baseline differences between groups and/or changes due to the intervention that could further explain these findings.
Limitations and Future Directions
There are several limitations in data collection methods that should be considered for future studies. In addition to post-intervention-only measures, the lack of longitudinal data is a limitation of the current study. Results may have been susceptible to demand characteristics, suggesting that additional data points post-intervention (e.g., 1–2 months later) would be helpful for ascertaining if providers continue to maintain compassion towards the self and others. This longitudinal data could also demonstrate the need (or lack thereof) for ongoing practice of the LKM to maintain effects. Additionally, the current study is susceptible to the common methods bias due to data being collected through the same survey using similar response methods. The relationships that were found between constructs, consequently, could be spurious correlations rather than true correlations (Podsakoff et al., 2012).
Participant demographics and global health status are additional limitations of the current study. The current sample included more White individuals and fewer men compared to estimates of the national nursing student population. Approximately 12% of nursing students identify as men and 67.8% as White (compared to 3.7% and 75.1% in the current sample, respectively; American Association of Colleges of Nursing, 2017, 2020). Therefore, the generalization of our results to the larger population should be done with caution. Finally, it is important to acknowledge that this study was conducted during the COVID-19 pandemic, which has important implications for the focus on weight stigma. Given increased reports of COVID-19 and obesity in the media, stigmatizing attitudes towards people with “obesity” likely have been reinforced. For instance, media reports have highlighted the negative, inaccurate messages that people with higher weight are responsible for their weight and a burden to the healthcare system (Flint, 2020). As a result, participants in the current study may have endorsed higher levels of weight stigma than they would have prior to the pandemic. These elevated weight bias scores could have impacted the efficacy of the intervention, requiring a more intensive intervention to effectively mitigate their weight stigma.
While we did not find a significant effect of the LKM on weight bias, future studies should continue to explore this relationship with a few potential changes to the study design. Increasing the duration and frequency of the intervention may better address the mechanisms by which bias could be reduced. Perhaps repeated, daily exposures of the brief LKM (e.g., Galante et al., 2016) could result in longer-lasting, significant changes in the mechanisms by which LKM reduces weight bias. On the other hand, longer exposures at less frequent intervals, such as one, 1.5- to 2-hr session weekly for 8 weeks may also be efficacious. Additionally, increased duration and frequency together with psychoeducation about weight bias and the multitude of factors that contribute to weight may be a more effective combination for addressing the multi-faceted nature of weight stigma. Finally, to better understand how the LKM functions to reduce bias, it is recommended that studies incorporate a self-compassion intervention, mindfulness intervention, and inactive control group (e.g., waitlist control or a silent, unguided reflection).
Based on the findings of the current study, there are important implications for research on healthcare provider training. Given we found that higher levels of self-compassion were associated with lower levels of weight bias and higher levels of compassionate care, research exploring the addition of self-compassion interventions to training programs may be important. Nursing students may benefit from regularly practicing self-compassion throughout training to build a compassionate stance towards the self and others. Ideally, future studies could explore incorporating this practice early and throughout training in order to promote long-term behaviors that improve provider well-being and, therefore, the patient-provider relationship (e.g., Rao & Kemper, 2017; Seppala et al., 2014). Potential interventions could include weekly self-compassion didactics and experiential activities that specifically incorporate marginalized patient populations (e.g., patients with higher weight). By intentionally drawing the connection between this practice and patient care, nursing students may be better able to mitigate their biases and provide empathic, patient-centered care to patients with higher weight. Without this intentional connection, the interventions may not be as effective. Furthermore, while the current study specifically explored the utility of the LKM, this is only one of several interventions that could be utilized to increase self-compassion. Alternative interventions, such as affectionate breathing or a self-compassion break, could be considered (Neff, 2023).
Considering the work of Sinclair et al. (2016), future studies may also benefit from incorporating patient and family perceptions of compassionate care since their voices have been largely excluded from the literature. These additional data points will help researchers identify the clinical impact of these interventions on patients’ experiences with their healthcare providers as it pertains to weight stigma. Also, this information will help corroborate healthcare providers’ self-report of the quality of care they provide, which may also be an important consideration to address if discrepancies exist.
In conclusion, the current study highlighted the complexity of weight stigma, as well as the potential roles of self-compassion, positive emotionality, and cognitive flexibility in promoting compassionate care towards patients with “obesity.” Given that we found statistically significant differences between groups for positive emotionality, it appears that mindfulness alone is not enough to elicit changes in this area, and the “active ingredient” in self-compassion interventions may be necessary to increase positive emotionality. Because statistically significant differences in self-compassion, cognitive flexibility, weight bias, and compassionate care were not found between the groups, a one-time, 10-min LKM may not be robust enough to elicit changes in these constructs. Therefore, there is a need to further explore the mechanisms that must be targeted to effectively reduce bias. This study offers a new direction for weight bias research by targeting one’s compassion towards the self as well as others.
References
Alberga, A. S., Edache, I. Y., Forhan, M., & Russell-Mayhew, S. (2019). Weight bias and health care utilization: A sco** review. Primary Health Care Research & Development, 20, e116. https://doi.org/10.1017/S1463423619000227
Allison, D. B., Basile, V. C., & Yuker, H. E. (1991). The measurement of attitudes toward and beliefs about obese persons. International Journal of Eating Disorders, 10(5), 599–607. https://doi.org/10.1002/1098-108X(199109)10:53.0.CO;2-%23
American Association of Colleges of Nursing (2017). The changing landscape: Nursing student diversity on the rise. https://www.aacnnursing.org/Portals/42/Diversity/Student-Diversity.pdf
American Association of Colleges of Nursing (2020). 2019-2020 race & ethnicity of students enrolled in nursing programs. https://www.aacnnursing.org/Portals/42/News/Surveys-Data/EthnicityTbl.pdf
Baer, R. A., Lykins, E. L. B., & Peters, J. R. (2012). Mindfulness and self-compassion as predictors of psychological wellbeing in long-term meditators and matched nonmeditators. The Journal of Positive Psychology, 7(3), 230–238. https://doi.org/10.1080/17439760.2012.674548
Blanton, C., Brooks, J. K., & McKnight, L. (2016). Weight bias in university health professions students. Journal of Allied Health, 45(3), 212–218. https://doi.org/10.7899/JCE-17-15
Carels, R. A., Hlavka, R., Selensky, J. C., Solar, C., Rossi, J., & Caroline Miller, J. (2018). A daily diary study of internalised weight bias and its psychological, eating and exercise correlates. Psychology & Health, 34(3), 306–320. https://doi.org/10.1080/08870446.2018.1525491
Carpenter, T. P., Pogacar, R., Pullig, C., Kouril, M., Aguilar, S., LaBouff, J., Isenberg, N., & Chakroff, A. (2019). Survey-software implicit association tests: A methodological and empirical analysis. Behavior Research Methods, 51(5), 2194–2208. https://doi.org/10.3758/s13428-019-01293-3
Chio, F. H., Mak, W. W., & Ben, C. L. (2021). Meta-analytic review on the differential effects of self-compassion components on well-being and psychological distress: The moderating role of dialecticism on self-compassion. Clinical Psychology Review, 85, 101986. https://doi.org/10.1016/j.cpr.2021.101986
Cohen, R. W., & Persky, S. (2019). Influence of weight etiology information and trainee characteristics on physician-trainees’ clinical and interpersonal communication. Patient Education and Counseling, 102(9), 1644–1649. https://doi.org/10.1016/j.pec.2019.04.011
Dennis, J. P., & Vander Wal, J. S. (2010). The cognitive flexibility inventory: Instrument development and estimates of reliability and validity. Cognitive Therapy and Research, 34(3), 241–253. https://doi.org/10.1007/s10608-009-9276-4
Diedrichs, P. C., & Barlow, F. K. (2011). How to lose weight bias fast! Evaluating a brief anti-weight bias intervention. British Journal of Health Psychology, 16(4), 846–861. https://doi.org/10.1111/j.2044-8287.2011.02022.x
Dondzilo, L., Rieger, E., Jayawardena, N., & Bell, J. (2019). Drive for thinness versus fear of fat: Approach and avoidance motivation regarding thin and non-thin images in women. Cognitive Therapy and Research, 43(3), 585–593. https://doi.org/10.1007/s10608-018-9989-3
Ferrari, M., Hunt, C., Harrysunker, A., Abbott, M. J., Beath, A. P., & Einstein, D. A. (2019). Self-compassion interventions and psychosocial outcomes: A meta-analysis of RCTs. Mindfulness, 10(8), 1455–1473. https://doi.org/10.1007/s12671-019-01134-6
Flint, S. W. (2020). Stigmatizing media portrayal of obesity during the coronavirus (COVID-19) pandemic. Frontiers in Psychology, 11, 2124. https://doi.org/10.3389/fpsyg.2020.02124
Fredrickson, B. L., Tugade, M. M., Waugh, C. E., & Larkin, G. R. (2003). What good are positive emotions in crisis? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychology, 84(2), 365–376. https://doi.org/10.1037/0022-3514.84.2.365
Galante, J., Bekkers, M., Mitchell, C., & Gallacher, J. (2016). Loving-kindness meditation effects on well-being and altruism: A mixed-methods online RCT. Applied Psychology: Health and Well-Being, 8(3), 322–350. https://doi.org/10.1111/aphw.12074
Gamst, G., Meyers, S., & Guarino, A. J. (2008). Analysis of variance designs. Cambridge University Press.
Garcia, J. T. (2012). Assessing weight bias in nurses toward obese patients and its effect on quality of care [Unpublished doctoral dissertation]. University of Florida.
Gloor, J. L., & Puhl, R. M. (2016). Empathy and perspective-taking: Examination and comparison of strategies to reduce weight stigma. Stigma and Health, 1(4), 269. https://doi.org/10.1037/sah0000030
Greenwald, A. G., McGhee, D. E., & Schwartz, J. L. (1998). Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology, 74(6), 1464–1480. https://doi.org/10.1037//0022-3514.74.6.1464
Griskevicius, V., Shiota, M. N., & Neufeld, S. L. (2010). Influence of different positive emotions on persuasion processing: A functional evolutionary approach. Emotion, 10(2), 190–206. https://doi.org/10.1037/a0018421
Gudzune, K. A., Bennett, W. L., Cooper, L. A., Clark, J. M., & Bleich, S. N. (2014). Prior doctor shop** resulting from differential treatment correlates with differences in current patient-provider relationships. Obesity, 22(9), 1952–1955. https://doi.org/10.1002/oby.20808
Hunger, J. M., & Major, B. (2015). Weight stigma mediates the association between BMI and self-reported health. Health Psychology, 34(2), 172. https://doi.org/10.1037/hea0000106
Jung, F. U. C. E., Luck-Sikorski, C., Wiemers, N., & Riedel-Heller, S. G. (2015). Dietitians and nutritionists: Stigma in the context of obesity. A systematic review. PLoS ONE, 10(10), e014076. https://doi.org/10.1317/journal.pone.0140276
Khan, S. S., Tarrant, M., Weston, D., Shah, P., & Farrow, C. (2018). Can raising awareness about the psychological causes of obesity reduce obesity stigma? Health Communication, 33(5), 585–592. https://doi.org/10.1080/10410236.2017.1283566
Kılıç, A., Hudson, J., McCracken, L. M., Ruparelia, R., Fawson, S., & Hughes, L. D. (2021). A systematic review of the effectiveness of self-compassion-related interventions for individuals with chronic physical health conditions. Behavior Therapy, 52(3), 607–625. https://doi.org/10.1016/j.beth.2020.08.001
Lee, Y., & Seomun, G. (2016). Development and validation of an instrument to measure nurses’ compassion competence. Applied Nursing Research, 30, 76–82. https://doi.org/10.1016/j.apnr.2015.09.007
Lewis, S., Thomas, S. L., Blood, R. W., Castle, D. J., Hyde, J., & Komesaroff, P. A. (2011). How do obese individuals perceive and respond to the different types of obesity stigma that they encounter in their daily lives? A qualitative study. Social Science & Medicine, 73(9), 1349–1356. https://doi.org/10.1016/j.socscimed.2011.08.021
Low, K. G., Charanasomboon, S., Brown, C., Hiltunen, G., Long, K., Reinhalter, K., & Jones, H. (2003). Internalization of the thin ideal, weight and body image concerns. Social Behavior and Personality, 31(1), 81–89. https://doi.org/10.2224/sbp.2003.31.1.81
MacBeth, A., & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32(6), 545–552. https://doi.org/10.1016/j.cpr.2012.06.003
Major, B., Hunger, J. M., Bunyan, D. P., & Miller, C. T. (2014). The ironic effects of weight stigma. Journal of Experimental Social Psychology, 51, 74–80. https://doi.org/10.1014/j.jesp.2013.11.009
Moore, A., & Malinowski, P. (2009). Meditation, mindfulness and cognitive flexibility. Consciousness and Cognition, 18(1), 176–186. https://doi.org/10.1016/j.concog.2008.12.008
Neff, K. (2020). Loving-kindness meditation [Speech audio recording]. Self-compassion. https://self-compassion.org/wp-content/uploads/2016/11/LKM_cleaned.mp3
Neff, K. (2023). Self-compassion guided practices and exercises. Self-Compassion. https://self-compassion.org/category/exercises/
Neff, K. D. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–102. https://doi.org/10.1080/15298860309032
Neff, K. D. (2016). The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness, 7(1), 264–274. https://doi.org/10.1007/s12671-015-0479-3
Neff, K. D., & Pommier, E. (2013). The relationship between self-compassion and other-focused concern among college undergraduates, community adults, and practicing meditators. Self and Identity, 12(2), 160–176. https://doi.org/10.1080/15298868.2011.649546
Neff, K. D., & Tóth-Király, I. (2022). Self-compassion scale (SCS). In Medvedev O. N., Krägeloh C. U., Siegert R. J., Singh N. N. (Eds.), Handbook of assessment in mindfulness research. Springer. https://doi.org/10.1007/978-3-030-77644-2_36-1
Nosek, B. A., & Smyth, F. L. (2007). A multitrait-multimethod validation of the implicit association test. Experimental Psychology, 54(1), 14–29. https://doi.org/10.1027/1618-3169.54.1.14
Phelan, S. M., Burgess, D. J., Puhl, R., Dyrbye, L. N., Dovidio, J. F., Yeazel, M., & van Ryn, M. (2015). The adverse effect of weight stigma on the well-being of medical students with overweight or obesity: Findings from a national survey. Journal of General Internal Medicine, 30(9), 1251–1258. https://doi.org/10.1007/s11606-015-3266-x
Phillips, W. J., & Hine, D. W. (2021). Self-compassion, physical health, and health behaviour: A meta-analysis. Health Psychology Review, 15(1), 113–139. https://doi.org/10.1080/17437199.2019.1705872
Podsakoff, P. M., MacKenzie, S. B., & Podsakoff, N. P. (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569. https://doi.org/10.1146/annurev-psych-120710-100452
Polizzi, C. P., Baltman, J., & Lynn, S. J. (2022). Brief meditation interventions: Mindfulness, implementation instructions, and lovingkindness. Psychology of Consciousness: Theory, Research, and Practice, 9(4), 366–378. https://doi.org/10.1037//cns0000194
Project Implicit (2011). About the IAT. https://implicit.harvard.edu/implicit/iatdetails.html
Puhl, R. M., & Brownell, K. D. (2006). Confronting and co** with weight stigma: An investigation of overweight and obese adults. Obesity, 14(10), 1802–1815. https://doi.org/10.1038/oby.2006.208
Puhl, R. M., & Heuer, C. A. (2010). Obesity stigma: Important considerations for public health. American Journal of Public Health, 100(6), 1019–1028. https://doi.org/10.2105/AJPH.2009.159491
Puhl, R. M., Luedicke, J., & Grilo, C. M. (2014). Obesity bias in training: Attitudes, beliefs, and observations among advanced trainees in professional health disciplines. Obesity, 22(4), 1008–1015. https://doi.org/10.1002/oby.20637
Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology & Psychotherapy, 18(3), 250–255. https://doi.org/10.1002/cpp.702
Rao, N., & Kemper, K. J. (2017). Online training in specific meditation practices improves gratitude, well-being, self-compassion, and confidence in providing compassionate care among health professionals. Journal of Evidence-Based Complementary & Alternative Medicine, 22(2), 237–241. https://doi.org/10.1177/2156587216642102
Schaefer, L. M., Burke, N. L., Thompson, J. K., Dedrick, R. F., Heinberg, L. J., Calogero, R. M., Bardone-Cone, A. M., Higgins, M. K., Frederick, D. A., Kelly, M., Anderson, D. A., Schaumberg, K., Nerini, A., Stefanile, C., Dittmar, H., Clark, E., Adams, Z., Macwana, S., Klump, K. L.,..., & Swami, V. (2015). Development and validation of the Sociocultural Attitudes Towards Appearance Questionnaire-4 (SATAQ-4). Psychological Assessment, 27(1), 54. https://doi.org/10.1037/a0037917
Seppala, E. M., Hutcherson, C. A., Nguyen, D. T., Doty, J. R., & Gross, J. J. (2014). Loving-kindness meditation: A tool to improve healthcare provider compassion, resilience, and patient care. Journal of Compassionate Health Care, 1(1), 5. https://doi.org/10.1186/s40639-014-005-9
Shahabi, B., Shahabi, R., & Foroozandeh, E. (2019). Analysis of the self-compassion and cognitive flexibility with marital compatibility in parents of children with autism spectrum disorder. International Journal of Developmental Disabilities, 66(4), 282–288. https://doi.org/10.1080/20473869.2019.1573000
Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D., West, C. P., Sloan, J., & Oreskovich, M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377. https://doi.org/10.1001/archinternmed.2012.3199
Sikorski, C., Luppa, M., Luck, T., & Riedel-Heller, S. G. (2015). Weight stigma ‘gets under the skin’—Evidence for an adapted psychological mediation framework—A systematic review. Obesity, 23(2), 266–276. https://doi.org/10.1002/oby.20952
Sinclair, S., Norris, J. M., McConnell, S. J., Chochinov, H. M., Hack, T. F., Hagen, N. A., & Bouchal, S. R. (2016). Compassion: A sco** review of the healthcare literature. BMC Palliative Care, 15, 6. https://doi.org/10.1186/s12904-016-0080-0
Slater, A., Varsani, N., & Diedrichs, P. C. (2017). #fitspo or #loveyourself? The impact of fitspiration and self-compassion instagram images on women’s body image, self-compassion, and mood. Body Image, 22, 87–96. https://doi.org/10.1016/j.bodyim.2017.06.004
Stell, A., & Farsides, T. (2016). Brief loving-kindness meditation reduces racial bias, mediated by positive other-regarding emotions. Motivation & Emotion, 40(1), 140–147. https://doi.org/10.1007/s11031-015-9514-x
Swift, J. A., Hanlon, S., El-Redy, L., Puhl, R. M., & Glazebrook, C. (2013). Weight bias among UK trainee dietitians, doctors, nurses and nutritionists. Journal of Human Nutrition and Dietetics, 26(4), 395–402. https://doi.org/10.1111/jhn.12019
Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics (6th ed.). Pearson.
Thompson, J. K., & Stice, E. (2001). Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Current Directions in Psychological Science, 10(5), 181–183. https://doi.org/10.1111/1467-8721.00144
Tomiyama, A. J. (2014). Weight stigma is stressful. A review of evidence for the cyclic obesity/weight-based stigma model. Appetite, 82, 8–15. https://doi.org/10.1016/j.appet.2014.06.108
Tylka, T. L., Russell, H. L., & Neal, A. A. (2015). Self-compassion as a moderator of thinness-related pressures’ associations with thin-ideal internalization and disordered eating. Eating Behaviors, 17, 23–26. https://doi.org/10.1016/j.eatbeh.2014.12.009
Yvonne (2016). Body scan [Speech audio recording]. Intro to Mindfulness & Meditation 4 Week Course. https://soundcloud.com/mindfulness-works/sets/intro-to-mindfulness
Zeng, X., Chiu, C. P. K., Wang, R., Oei, T. P. S., & Leung, F. Y. K. (2015). The effect of loving-kindness meditation on positive emotions: A meta-analytic review. Frontiers in Psychology, 6, 1693. https://doi.org/10.3389/fpsyg.2015.01693
Author information
Authors and Affiliations
Contributions
Ellen Joseph: literature review, conceptualization, methodology, data analysis, interpretation, writing.
Trisha Raque: conceptualization, supervision, reviewing, editing.
Corresponding author
Ethics declarations
Ethics Approval
This research was approved by the Institutional Review Board at the University of Denver and was performed in accordance with ethical standards for research with human participants.
Informed Consent
All participants included in the current study provided informed consent immediately after clicking the survey link. Any participants who failed to complete the informed consent or declined were excluded from the study.
Conflict of Interest
The authors have no conflicts of interests to declare that are relevant to the content of this article. Partial funding support was received through the College of Education Student Association (COESA) at the University of Denver for a student dissertation scholarship.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joseph, E.C., Raque, T.L. Feasibility of a Loving Kindness Intervention for Mitigating Weight Stigma in Nursing Students: A Focus on Self-Compassion. Mindfulness 14, 841–853 (2023). https://doi.org/10.1007/s12671-023-02094-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02094-8