Abstract
Introduction
Determination of circulating prostate specific antigen (PSA) is commonly used in the diagnosis and treatment monitoring of prostate cancer [1]. Presently, PSA testing is performed in centralized laboratories, which is associated with prolonged time between venipuncture and the PSA value being available. In this prospective study, we present a new and rapid test system for the quantitative determination of PSA levels from finger-stick blood.
Methods
The Claros1® analyzer is a rapid microfluidics-based point-of-care system for quantitative PSA analysis from 10-µl finger-stick blood that requires only 10 min for testing. Total PSA concentrations by the Claros system in 100 consecutive asymptomatic men (median age 57 years, range 44–81 years) were compared with two commercially available, commonly used PSA assays (Abbott and Elecsys by Roche) performed by a reference laboratory.
Results
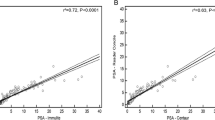
Eighty-six percent of finger-stick blood-borne probes from 100 men were evaluable for PSA testing by the Claros1® analyzer system. In 13/14 cases the expiry date of the microfluid cassettes of the Claros system was exceeded and one blood puncture was performed inadequately. The correlations between the Claros results and OPKO–Abbott and OPKO–Roche assay results were high, with R2 values of 0.982 and 0.985, respectively. The R2 value for the Roche–Abbott correlation was 0.991 with a slope value of 1.160. Prostate cancer was diagnosed in seven cases, with a median PSA of 1.8 ng/ml in the Claros group compared to 1.75 ng/ml and 2.1 ng/ml in the Abbott and Roche groups, respectively.
Conclusion
The Claros1® PSA assay combines the advantages of rapid, accurate detection with a low required sample volume, allowing the analysis to be performed using finger-stick blood. Provided that further analysis proves the reproducibility of the test, it may help to reduce the number of office visits, thus decreasing costs to the health care system.

Similar content being viewed by others
References
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics. CA Cancer J Clin. 2014;64:9–29.
Catalona WJ, et al. Comparison of digital rectal examination and serum prostate specific antigen in the early detection of prostate cancer: results of a multicenter clinical trial of 6,630 men. J Urol. 1994;151:1283–90.
Welch HG, Gorski DH, Albertsen PC. Trends in metastatic breast and prostate cancer–lessons in cancer dynamics. N Engl J Med. 2015;373:1685–7.
Cooperberg MR, Lubeck DP, Meng MV, Mehta SS, Carroll PR. The changing face of low-risk prostate cancer: trends in clinical presentation and primary management. J Clin Oncol. 2004;22:2141–9.
Fossati N, et al. Impact of stage migration and practice changes on high-risk prostate cancer: results from patients treated with radical prostatectomy over the last two decades. BJU Int. 2015;22:24. https://doi.org/10.1111/bju.13125.
Schröder FH, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360:1320–8.
Fitzpatrick JM, Banu E, Oudard S. Prostate-specific antigen kinetics in localized and advanced prostate cancer. BJU Int. 2009;103:578–87.
Scattoni V, et al. Diagnosis of local recurrence after radical prostatectomy. BJU Int. 2004;93:680–8.
Wilson DH, et al. Fifth-generation digital immunoassay for prostate-specific antigen by single molecule array technology. Clin Chem. 2011;57:1712–21.
Lepor H, et al. Clinical evaluation of a novel method for the measurement of prostate-specific antigen, AccuPSA(TM), as a predictor of 5-year biochemical recurrence-free survival after radical prostatectomy: results of a pilot study. BJU Int. 2012;109:1770–5.
Okada H, Hosokawa K, Maeda M. Power-free microchip immunoassay of PSA in human serum for point-of-care testing. Anal Sci. 2011;27:237–41.
Lin YY, et al. A nanoparticle label/immunochromatographic electrochemical biosensor for rapid and sensitive detection of prostate-specific antigen. Biosens Bioelectron. 2008;23:1659–65.
Kim DJ, et al. Organic electrochemical transistor based immunosensor for prostate specific antigen (PSA) detection using gold nanoparticles for signal amplification. Biosens Bioelectron. 2010;25:2477–82.
Adel Ahmed H, Azzazy HME. Power-free chip enzyme immunoassay for detection of prostate specific antigen (PSA) in serum. Biosens Bioelectron. 2013;49:478–84.
Karim O, et al. Point-of-care PSA testing: an evaluation of PSAwatch. Prostate Cancer Prostatic Dis. 2007;10:270–3.
Dok An C, et al. Evaluation of a rapid qualitative prostate specific antigen assay, the One Step PSA(TM) test. Cancer Lett. 2001;162(2):135–9.
Jung K, et al. Rapid detection of elevated prostate-specific antigen levels in blood: performance of various membrane strip tests compared. Urology 1999;53(1):155–60.
Lein M, et al. Rapid screening of PSA: evaluation of an immunochemical membrane strip test. Clin Chem. 1995;41(10):1545–7.
Madersbacher S, et al. Validation of a 10-minute dipstick test for serum prostate-specific antigen. Eur Urol. 1996;30(4):446–50.
Berg W, et al. Possibility of improving the acceptance rateof early detection testing for prostate cancerwith a one-step test for prostate-specific antigen in whole blood. Urol Int. 1999;63(2):102–6.
Fernandez-Sanchez C, et al. One-step immunostrip test for the simultaneous detection of free and total prostate specific antigen in serum. J Immunol Methods 2005;307(1–2):1–12.
Miano R, et al. Evaluation of a new, rapid, qualitative, one-step PSA Test for prostate cancer screening: the PSA RapidScreen test. Prostate Cancer Prostatic Dis. 2005;8(3):219–23.
Wu CC, et al. Evaluation of a rapid quantitative determination method of PSA concentration with gold immunochromatographic strips. BMC Urol. 2015;15:109.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study or publication of this article. The article processing charges were funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Agnieszka Maj-Hes, Sabina Sevcenco, Tibor Szarvas, and Gero Kramer have nothing to disclose.
Compliance with Ethics Guidelines
All procedures performed in this study involving human participants were in accordance with the ethical committee of the Medical University of Vienna and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Data Availability
The manuscript has no associated data or the data will not be deposited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7613810.
Rights and permissions
About this article
Cite this article
Maj-Hes, A., Sevcenco, S., Szarvas, T. et al. Claros System: A Rapid Microfluidics-Based Point-of-Care System for Quantitative Prostate Specific Antigen Analysis from Finger-Stick Blood. Adv Ther 36, 916–922 (2019). https://doi.org/10.1007/s12325-019-0888-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-019-0888-0