Abstract
Background
Known predictors of adverse outcomes in patients with moderate-severe TBI (msTBI) explain only a relatively small proportion of patient-related outcomes. The frequency and impact of intensive care unit complications (ICU-COMPL) on msTBI-associated outcomes are poorly understood.
Methods
In 213 consecutive msTBI patients admitted to a Level I Trauma Center neuro trauma ICU, twenty-eight ICU-COMPL (21 medical and 7 neurological) were prospectively collected and adjudicated by group consensus, using pre-defined criteria. We determined frequencies, and explored associations of ICU-COMPL and hospital discharge outcomes using multivariable logistic regression.
Results
The average age of the study sample was 53 years, and the median presenting Glasgow Coma Scale and Injury Severity Scores were 5 and 27, respectively. Hyperglycemia (79 %), fever (62 %), systemic inflammatory response syndrome (60 %), and hypotension requiring vasopressors (42 %) were the four most common medical ICU-COMPL. Herniation (39 %), intracranial rebleed (39 %), and brain edema requiring osmotherapy (37 %) were the three most common neurological ICU-COMPL. After adjusting for admission variables, duration of ventilation, and ICU length-of-stay, patients with brain edema (OR 5.8; 95 % CI 2, 16.7) had a significantly increased odds for dying during hospitalization whereas patients with hospital-acquired urinary tract infection (UTI) had a decreased odds (OR 0.05; 95 % CI 0.005, 0.6). Sensitivity analysis revealed that UTI occurred later, suggesting a non-causal association with survival. Brain herniation (OR 15.7; 95 % CI 2.6, 95.4) was associated with an unfavorable functional status (GOS 1–3).
Conclusion
ICU-COMPL are very common after msTBI, have a considerable impact on short-term outcomes, and should be considered in the prognostication of these high risk patients. Survival associations of time-dependent complications warrant cautious interpretation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Large epidemiological studies of the International Mission for Prognosis and Analysis of Clinical Trials in Traumatic Brain Injury (IMPACT) have identified and validated important early predictors of adverse outcomes in patients with moderate-severe traumatic brain injury (msTBI) [1–3]. These predictors, including advanced age, lower Glasgow Coma Scale (GCS) motor score, pupillary reactivity, pre-admission hypotension and hypoxia, and head computed tomography (CT) appearance, however, have two key shortcomings: they only explain about one-third of the variability in patient-related outcomes, and they are solely based on hospital admission characteristics. Inasmuch, they fail to account for the often prolonged hospital and intensive care unit (ICU) course that the majority of these critically ill patients undergo if they do not succumb to their injuries early.
To our knowledge, a limited number of retrospective studies have examined the frequency of medical ICU complications in patients with TBI and their impact on short-term outcomes [4, 5]. At present, the frequencies of specific, pre-defined ICU complications in prospectively enrolled patients hospitalized with msTBI, and their impact on patient-centered outcomes in addition to IMPACT admission predictors, are not known. This information has important implications for the enhanced care of patients with msTBI since many ICU complications may be preventable or at least treatable. In addition, more accurate outcome prediction models, including data from admission and the ICU and hospital stay, would be useful to physicians and families of affected patients to guide clinical decision-making about the extent and goals of care in these critically ill patients.
The objectives of this observational study were to determine the frequencies of pre-specified medical and neurological ICU complications in a contemporary cohort of patients hospitalized with msTBI, and explore the impact of these clinical complications on in-hospital mortality and functional outcome at the time of hospital discharge.
Materials and Methods
Patient Population
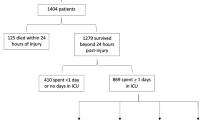
Two-hundred and seventeen patients with msTBI (enrollment GCS ≤12) admitted to the University of Massachusetts (UMASS), Neurological-Trauma-Intensive Care Unit (NTICU) between November, 2009 and November, 2012 were enrolled in the Outcome Prognostication in Traumatic Brain Injury (OPTIMISM) Study. This study was approved by the UMASS institutional review board. In order to optimize our complex data collection and consent process and assess the feasibility of these procedures, we did not obtain written informed consent from the first 47 patients and also included mild TBI, who were excluded from the present analysis. After a several months optimization process and “run-in” phase, we excluded patients with mild TBI and added long-term follow-up to the study plan. In all subsequent patients, written consent was obtained from either the patient or their surrogate for further follow-up. For the present analyzes, and to show feasibility of this observational study, outcomes at the time of hospital discharge were examined because not all enrolled patients had completed their post-discharge follow-up assessments in this ongoing study. The diagnosis of TBI was based on the history and mechanism of injury. In addition, study eligibility required the absence of a non-traumatic brain lesion on admission non-contrast computed tomography (CT), which was reviewed by a neuroradiologist per clinical routine, and by three board-certified neurointensivists during weekly data review as described below. After excluding four patients with hypoxic-ischemic injury due to hanging or drowning, the final study sample comprised 213 patients. Enrollment GCS was assessed with great care based on the recommendations by the IMPACT investigators [2].
We recorded the GCS within the first 24 h as close to the trauma as possible post-resuscitation, off sedation, and after intoxication by alcohol or illicit drugs had worn off. If patients were extubated quickly within the first 24 h, GCS was recorded immediately post extubation. In patients who deteriorated early due to enlarging hematomas or brain edema, we recorded the post-resuscitation GCS after this neurological deterioration in the first 24 h. Patients were excluded if their enrollment GCS was ≥13.
Clinical Management
All msTBI patients hospitalized at UMASS, including those with multi-organ injuries, are routinely admitted to the NTICU. All patients receive 0.9 % normal saline at a dose of 1 mL/kg h, and are managed according to the Brain Trauma Foundation (BTF) guidelines [6]. Routine intracranial pressure (ICP) monitoring is performed with an intraparenchymal probe, or an extraventricular drain, depending on the treating neurosurgeon’s preference. Intracranial hypertension and acute symptomatic intracranial mass effect are treated with repeated intravenous boluses of 20 % mannitol (1 g/kg) or 23.5 % hypertonic saline (15–30 mL per dose) and a stepwise sedation protocol with sedation to the highest necessary Richmond Agitation Sedation Scale goal ≤0 to achieve ICP control of 20 mmHg or less, using propofol (5–50 mcg/kg min), or midazolam (1–40 mg/h) infusions in combination with fentanyl (25–400 mcg/kg h) infusions. If an acute symptomatic intracranial mass is amenable to surgery, a craniotomy, with or without a craniectomy, is performed based on clinical indications and the neurosurgeon’s preference. Cerebral perfusion pressure (CPP) is supported with the use of vasospressor infusions (phenylephrine or norepinephrine) to achieve a goal CPP of ≥60 mmHg. No routine autoregulation testing is performed. However, if a simultaneous increase in the ICP and mean arterial pressure (MAP) is noted in patients on vasopressors, abnormal autoregulation is assumed, leading to a more tightly regulated MAP goal to prevent the iatrogenic elevation of ICP. Severe hyponatremia (serum sodium ≤134 mmol/L) is treated with fludrocortisone 0.2–0.4 mg twice daily in addition to continuous hypertonic saline (1.5 or 3 %) to achieve normal serum sodium values (140 mmol/L or higher) and prevent exacerbation of brain edema. Intubated patients are ventilated with a low tidal volume strategy according to the Acute Respiratory Distress Syndrome Network (ARDS-net) protocol (6–8 mL/kg ideal body weight) without permissive hypercapnia [7]. An institution-wide ICU insulin protocol calls for the initiation of a continuous insulin infusion when patients have two consecutive glucose readings >7.8 mmol/L (140 mg/dL) at any point during the ICU stay to control blood glucose levels to 4.4–7.8 mmol/L (80–140 mg/dL).
To minimize the risk of ventilator-associated pneumonia (VAP) or aspiration pneumonia, all patients have the head of their bed elevated at 30°. Ventilated patients are routinely treated with oral chlorhexidine gluconate to prevent VAP, and with famotidine or a proton-pump-inhibitor to prevent stress ulcers. In the absence of contraindications (e.g., enlarging hemorrhagic brain lesion or high risk organ hemorrhage), deep venous thrombosis prophylaxis with subcutaneous enoxaparin twice daily, or unfractionated heparin three times daily, is initiated within the first 24 h of hospital admission. Otherwise, the same treatment regimen is started within the first 72 h, or, if contraindications persist, an inferior vena cava filter is placed. Possible discontinuation of central venous and arterial line access and indwelling urinary catheters is reviewed daily to minimize the risk of infections.
All best practices are reviewed and documented daily during NTICU rounds using a standardized checklist. Fever (axillary temperature ≥ 38.3 °C) is treated aggressively with the institution of enteral or rectal acetaminophen 975 mg every 6 h and ibuprofen 600 mg every 6 h in the absence of contraindications. If fever persists or recurs, ventilated patients are started on induced normothermia for a target core body temperature of 37 °C using cooling blankets (Blanketrol III®, Cincinnati SubZero, Cincinnati, OH), ice-cold saline infusions [8] and ice-packs. Shivering is treated aggressively using a staged protocol which included buspirone, enteral or intravenous (IV) magnesium (Mg) for goal Mg levels of 2–4.5 mg/dL, sedation with midazolam, propofol, fentanyl, with addition of clonidine, dexmedetomidine, and/or IV dantrolene for refractory shivering. Patients are transfused for hemoglobin levels ≤7 mg/dL [9] unless they have ongoing hemorrhage or an acute myocardial infarction, with a hemoglobin goal of 9–10 mg/dL for the latter. Patient care is provided by the neurocritical care team, including a full-time board-certified attending neurointensivist, with 24/7 team coverage, as well as the trauma team. These teams are in direct communication about the patient’s management plan. Neurosurgery provides consultations on an as-needed basis for procedural interventions.
Clinical Variables
The mechanisms underlying the trauma, and out-of-hospital data including initial GCS, pupillary reactivity, and physiologic data, were obtained from the emergency medical services report. If the patient was initially transported to an outside hospital, this information was extracted from the outside hospital record, and the outside hospital head CT was reviewed. The UMASS emergency department (ED) trauma assessment data was recorded, including GCS, pupillary reactivity, physiological data, and head CT findings. Hypoxia was defined as oxygen saturation levels of ≤89 %. Hypotension was defined as a systolic blood pressure ≤89 mmHg. For hypotension, hypoxia and pupillary reactivity, the worst finding either in the field, outside the hospital, or in the UMASS ED were used for data analysis. Injury Severity Score (ISS) was calculated by the trauma attending. Patients were followed throughout their ICU stay. A total of 28 pre-specified medical and neurological ICU complications (Tables 1, 2) were prospectively recorded and adjudicated during weekly research meetings between the three neurointensivists and the research nurse. The initial head CT was reviewed weekly, graded, and adjudicated by this group according to the Marshall CT grading scale [10]. Study data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at the University of Massachusetts Medical School, using a secure, web-based data entry tool [11].
Outcome Assessment
At the time of hospital discharge, written notes by physical and occupational therapy, physiatry, nursing, and attending physicians were reviewed by a study team member and patients were retrospectively categorized according to the Glasgow Outcome Scale (GOS) [12]. Our principle study outcomes were dichotomized into death (GOS 1) and survival (GOS 2–5), as well as into unfavorable (GOS 1–3) and favorable (GOS 4, 5) neurological status.
Statistical Analysis
Univariate analyzes were performed using Chi square or Fisher’s exact test for categorical variables, two-tailed t test of normally distributed continuous variables, and Wilcoxon–Mann–Whitney test for non-normally distributed continuous or ordinal variables. We categorized the occurrence of deep vein thrombosis and pulmonary embolism into venous thromboembolism (VTE). Missing data were only encountered for pupillary reactivity. Missing pupillary reactivity was treated as “both pupils react”, as we assumed that an abnormal neurological examination was more likely to be documented by the trauma and neurosurgical team. A verbal GCS score of “T” (intubated patients) was transformed to “1” to allow statistical analysis of GCS as a continuous variable. Significant predictors of hospital mortality or unfavorable functional outcomes in our univariate analyzes were entered in a stepwise, forward logistic regression model, in the order of their frequency of occurrence, after adjusting for baseline differences and known predictors of poor outcome in msTBI: patient’s age, GCS, pupillary reactivity, Marshall CT classification, length of mechanical ventilation (days), ICU length-of-stay (ICU LOS; days), and trauma cause. We created separate models for medical, neurological, and combined medical–neurological complications and their associations with our principal study outcomes (mortality and unfavorable outcome [GOS 1–3]). We restricted the total number of variables to eight in the separate models, and nine in the combined clinical complications model. Addition of the ISS to the models to adjust for other bodily injuries was considered, but omitted in the main analysis since there were no between group differences in the baseline ISS and because we were restricted in the number of variables we could control for in the regression models. In a sensitivity analysis, we explored differences in the direction and strength of the associations with mortality and unfavorable hospital outcome in the final models by adding the ISS. The limit for entry and removal of variables in the stepwise regression model was p < 0.05. A-priori we decided to analyze medical and neurological complications and their associations with patient outcomes separately before combining them. This was done because we hypothesized that certain neurological complications may have stronger associations with patient outcomes than medical complications. Weaker, but potentially important associations of medical complications with outcome could be missed if we aggregated these complications. Firth bias-correction was used in the univariate analysis to handle those variables which displayed quasi-complete separation due to low occurrence rates in our study sample [13]. This approach uses a penalized likelihood estimation (as opposed to the usual unconditional logistic regression method), and allows the calculation of an odds ratio and accompanying 95 % confidence intervals. It is considered the ideal approach to complete or quasi-complete separation problems in logistic regression [13]. Complications with a total occurrence of <15 were excluded from the final models to ensure model stability. Finally, to determine the relative contributions of the individual predictors of mortality and poor functional outcome, we compared reductions in the Nagelkerke (R 2) value of the entire model after individual removal of each predictor. All tests were two-tailed, and p values <0.05 were considered to be statistically significant. Data analyzes were performed using commercially available software SAS® 9.3 (SAS Institute Inc., Cary, NC).
Results
Study Sample Characteristics
Baseline characteristics of the study sample are shown in Table 1. The average age of study patients was 53 years, 70 % were men, and the majority (76 %) had a severe TBI. The average ICU LOS was 10.4 days.
Frequency of Medical and Neurological ICU Complications
Ninety-five percent (202/213) of study patients developed at least one medical ICU complication, while 70 % (149/213) developed at least one neurological ICU complication. After combining both medical and neurological complications, 96 % (205/213) of the study population experienced at least one ICU complication during their index hospitalization.
The frequencies of the medical and neurological ICU complications examined are shown in Figs. 1 and 2. Hyperglycemia was the most frequent medical ICU complication (79 %) followed by fever (62 %), systemic inflammatory response syndrome (SIRS; 60 %), and hypotension requiring vasopressors (42 %). Among the neurological complications examined, brain herniation (39 %) was the most common neurological ICU complication, followed by rebleeding (39 %) and brain edema requiring osmotherapy (37 %). ICP crisis was the most common complication among those with an ICP monitor (62 % of 62 patients with ICP monitor).
Magnitude and Predictors of Adverse Hospital Outcomes
In-hospital mortality was 35 % (74/213), and 23 % (49/213) of our study population died within the first 48 h of hospital admission. Causes of death were documented in 97 % (72/74) of patients, and included withdrawal of the ventilator in 76 % (56/74), brain death in 15 % (11/74), and cardiac arrest in the ICU in 7 % (5/74). Eighty-three percent (177/213) of study patients experienced an unfavorable outcome (GOS 1–3). Among the 139 survivors at the time of hospital discharge, 4 % (9/213) were classified as being in a persistent vegetative (GOS 2), 44 % (94/213) as severely disabled (GOS 3), 15 % (32/213) as moderately disabled (GOS 4), and 2 % (4/213) as having a good recovery (GOS 5).
The proportion of patients who experienced at least one medical ICU complication was higher in those with unfavorable functional status (GOS 1–3) at hospital discharge (98 %; 173/177) than among those with a favorable functional outcome (81 %, 29/36; p < 0.001), but was equally high in those who died (99 %, 73/74) compared to those who lived (93 %, 129/139; p = 0.1). The proportion of patients with at least one neurological ICU complication was higher in those with an unfavorable functional outcome (77 %, 136/177) compared to those with a favorable functional outcome at hospital discharge (36 %, 13/36; p < 0.001), and was also higher in patients who died in the hospital (92 %, 68/74) compared to those who survived (58 %, 81/139; p < 0.001).
Tables 2 and 3 show the results of the univariate analyzes of factors associated with hospital mortality and unfavorable functional status. Hyperglycemia and hypotension requiring vasopressors were associated with increased odds for mortality and unfavorable functional outcome, while cardiac arrest and disseminated intravascular coagulation were only associated with mortality, but not unfavorable functional outcome. Fever, as well as the infectious complications pneumonia, VAP, hospital-acquired urinary tract infections (UTIs), and sepsis appeared to be associated with improved survival of the index hospitalization, without association with unfavorable outcome (GOS 1–3). SIRS showed an association with improved survival, as well as with poor functional outcome. The univariate analysis of the neurological complications showed that brain herniation and edema were associated with both increased odds for mortality and unfavorable functional outcome at discharge (Table 3). Ischemic stroke and ICP crisis (in those with ICP monitor) were associated with increased discharge mortality, but not unfavorable functional outcome.
Multivariable logistic regression, adjusting for known admission predictors of poor outcome and baseline differences between our respective comparison groups, showed that, among the medical ICU complications examined, UTI was associated with a higher odds for surviving the index hospitalization (Table 4). In the multivariable adjusted model predicting an unfavorable functional outcome (GOS 1–3), hypotension requiring vasopressors was identified as a significant predictor of an unfavorable outcome (Table 4).
Among the neurological complications examined, brain edema was significantly associated with increased hospital mortality, while herniation was associated with an unfavorable functional status (GOS 1–3) after adjusting for other factors of prognostic importance (Table 4).
After combining both medical and neurological ICU complications, brain edema remained independently associated with an increased odds of dying during hospitalization, while UTI remained associated with a higher odds of surviving the acute hospitalization. The combined multivariable adjusted logistic regression model identified only brain herniation as a predictor of an unfavorable discharge outcome (Table 4).
We performed a sensitivity analysis adding ISS to the final separate medical and neurological ICU complications and combined models, and found no significant or clinically meaningful differences in the direction or strength of the associations with our principal study outcomes.
There were no interactions between any of the significant predictors of our two primary study outcomes in any of the final regression models. All models showed increasingly larger R 2 coefficients (improved explanation of the variability of outcome) by adding medical, neurological, and combined medical–neurological ICU complications, respectively, to the baseline variables (Table 4).
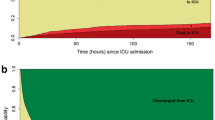
The additional relative contribution of the individual predictors to the explained variance of outcome in the final combined ICU complication models is shown in Fig. 3. In the mortality model, brain edema and UTI contributed to the explained variance to a higher degree than GCS and pupillary reactivity, and to a similar degree as the Marshall CT scale. In the unfavorable outcome (GOS 1–3) model, brain herniation contributed to a high degree to the explained variance, second only to age which contributed only slightly more (Fig. 3).
Relative contribution of individual predictors to the explained variance (Nagelkerke R 2) of mortality or unfavorable outcome (GOS 1–3) in the final, combined (medical and neurological) ICU complication model. To determine the relative contributions of the individual predictors, we compared reductions in the Nagelkerke R 2 value of the entire model after individual removal of each predictor. The individual R 2 reductions are shown in the bar graphs for each model. Gray bars represent the baseline variables adjusted for in each model. Black bars represent the significant ICU complications in both models
Since patients who died or were discharged from the hospital during the first 48 h of admission may have a different set of predictive factors, or were not hospitalized for a long enough duration to examine the development and impact of selected medical and neurological complications, we carried out a sensitivity analysis, excluding patients who were discharged or died <48 h after admission, leaving 164 patients available for analysis. Of these, 37 patients died and 127 survived their acute hospitalization, while 134 patients remained in the unfavorable status group; these numbers were insufficient to perform a meaningful regression analysis for predictors of in-hospital mortality or an unfavorable functional outcome. In carrying out a univariate analysis, some clinical complications developed at a lower frequency than in the overall study cohort (hypotension requiring vasopressors, anemia, cardiac arrest, acute liver failure, brain herniation, brain edema, and ischemic stroke) while others showed either a higher frequency or no change (Tables 2, 3). The univariate analysis of the clinical complications examined revealed no significant changes in magnitude or statistical significance from the univariate analysis in the entire cohort, with the exception that sepsis (OR 0.4; 95 % CI 0.2–1), VAP (OR 0.3; 95 % CI 0.1–1), hypotension requiring vasopressors (OR 0.6; 95 % CI 0.3–1.2), SIRS (OR 0.8; 95 % CI 0.4–1.8), and pneumonia (OR 0.6; 95 % CI 0.3–1.2) were no longer significant univariate predictors of survival. In contrast, UTI remained associated with increased in-hospital survival even after excluding early hospital discharges and deaths (OR 0.2; 95 % CI 0.04–0.7).
We performed an additional post hoc sensitivity analysis using the motor GCS only in our predictive models of non-neurological, neurological, and combined ICU complications; this was done because the IMPACT score was derived and validated using the motor GCS and not the full GCS due to the unreliability of the verbal GCS in intubated patients [1]. The multivariable regression forward-selection models and the final models revealed no changes in the type, direction, or magnitude of the predictors by substituting our total GCS with the motor GCS.
Discussion
The results of this study in a contemporary cohort of patients hospitalized with msTBI at a Level I Trauma Center demonstrate that medical and neurological ICU complications are very common in these critically ill patients admitted to an NTICU. Our data also suggests that, at least for adverse short-term hospital outcomes, ICU complications appear to contribute in a varying, but generally similar or even higher degree than some of the well-established known predictors of adverse outcomes after msTBI such as GCS, Marshall CT grading scale, and pupillary reactivity. This finding is important since the only widely validated and currently available msTBI outcome prognostication scale, the IMPACT score, includes only hospital admission variables [1, 14]. This present analysis did not assess whether ICU complications may also explain long-term functional or cognitive outcomes after msTBI.
In the present cohort, brain edema was associated with an increased risk of dying during hospitalization while UTI appeared to be associated with improved survival after adjusting for other known admission predictors of outcome, duration of ventilation, and ICU LOS. These adjustments are necessary and important because many ICU complications may develop only after an extended ICU stay or prolonged ventilation, while others might be early complications. Our study findings, however, have to be interpreted with great caution given the small sample size and other possible confounders.
Predictors of an unfavorable discharge status (GOS 1–3) in our adjusted models of medical and neurological ICU complications included hypotension requiring vasopressors, and herniation, while only brain herniation remained associated with unfavorable functional status in the combined clinical complication models.
Our study expands upon the relatively limited medical literature on non-neurological and neurological complications and their influence on short-term outcomes in patients hospitalized with msTBI. A recent review published by investigators from the IMPACT study reinforces that the inpatient clinical course of patients with msTBI has been inadequately studied [15].
A retrospective study examining the frequency of extracranial complications in 613 patients with severe head trauma analyzed data from the Traumatic Coma Data Bank over the period 1983–1988, found that pneumonia, shock of at least 30 min duration during the hospital course, coagulopathy, and sepsis contributed to an unfavorable outcome of GOS 1–3, documented as the “last recorded” with a follow-up time of 5 days to more than 3 years [5]. In addition to the retrospective design of this investigation, limitations of this study included the quality of the data on ICU complications, which had neither been validated nor reviewed by intensivists, the use of pre-resuscitation GCS, and the highly variable follow-up time which was not controlled for in the analysis. A more recent study in 209 patients who presented with severe TBI over a 3-year period beginning in 2000 suggested that non-neurologic organ failure, as measured by the maximum modified multiple organ dysfunction score (MODS) in the ICU, may contribute to a large proportion of all deaths after severe TBI, but specific complications were not identified [16]. A recent study in 683 adult neurotrauma patients admitted to the Royal Perth ICU, the poly-trauma ICU of Western Australia’s designated major trauma center, between 1994 and 2002, of whom 636 (93.1 %) also had extracranial injuries, found that extracranial injuries significantly influenced 6-month mortality after neurotrauma and suggested that adjustment for the severity of extracranial trauma using the ISS should be undertaken for any TBI outcome models [17]. This important prognosticator was not adjusted for in the two previously mentioned studies [5, 16]. Furthermore, the latter study also emphasized that the source data for the IMPACT prediction model was largely derived from clinical trials of TBI with patients with isolated head trauma and low rates of extracranial injuries [17]. In actual clinical practice, however, msTBI patients commonly present with poly-trauma, reinforcing the importance of adjusting for ICU complications, and possibly ISS, to improve the calibration of outcome prediction models. In our study, we did not adjust for ISS in our main outcome models. This was because there were no differences in the ISS between our respective comparison groups and because we were restricted in the number of variables we could control for in our multivariable regression models. Our sensitivity analysis adjusting for ISS did not reveal any statistically significant or clinically meaningful differences in the direction or strength of the associations with our principal study outcomes.
Hospital-acquired infections were associated with increased short-term survival in our study. Even after adjustment for several important factors associated with outcome, including ICU LOS, hospital-acquired UTI remained associated with increased short-term survival. This counterintuitive finding may have been due to the inclusion of early deaths (<48 h of admission) and their relatively high proportion in over half (49/74) of the deaths in our study, and because hospital-acquired infections, including UTI, commonly do not develop until several days into the hospital course. This is confirmed by our sensitivity analysis in which we excluded early (<48 h after admission) discharges and deaths; the total number of hospital-acquired infections remained unchanged or decreased minimally with a relative increase in the frequencies. In this restricted cohort, the univariate analysis revealed that SIRS, pneumonia, VAP, and sepsis were no longer significantly associated with survival, while UTI remained predictive of survival (OR 0.2; 95 % CI 0.04–0.7). Although we adjusted for ICU LOS in our multivariable analysis in the non-restricted cohort of 213 patients, we may not have adequately controlled for other factors, such as the notion that the longer patients live after admission, the more likely they are to survive overall, but also with an elevated odds of develo** an infectious complication, such as a hospital-acquired UTI.
The literature does not provide ample information about UTI rates in msTBI. A single-center retrospective study of infections in 258 patients with TBI undergoing neurosurgery between 1999 and 2005 in Europe revealed a 7 % incidence of UTI [18], while our frequency was 13 %. The associations between UTI on discharge and long-term outcomes were not examined in this study. More than three quarters of the sample in this study were men compared to 70 % of our study cohort, possibly explaining the increased UTI frequency in our patients. In this study, longer intra-hospital stay before the neurosurgical procedure was associated with UTI, among other infections [18]. An additional reason for our increased UTI frequency might have been a relatively higher urinary catheter rate in our patients, a known risk factor for hospital-acquired UTI [19]. Indeed, our institutional skin protection guidelines prohibit diaper use in immobilized patients, which may possibly result in a longer duration of indwelling urinary catheters.
Hypotension requiring vasopressors occurred in two of every five patients in our study and was associated with an unfavorable functional status, but not mortality. Sepsis, including septic shock, was not associated with any of our assessed outcomes. Inasmuch, hypotension is unlikely a marker of septic shock, but possibly a marker of neurogenic or hypovolemic shock, which have previously been associated with increased mortality in patients with TBI [20].
Hyperglycemia (defined as >7.8 mmol/L [140 mg/dL]) occurred as the most frequent non-neurological complication in our cohort. This target may seem low, but was chosen because our institutional protocol called for the initiation of an insulin infusion in order to reduce the magnitude of higher serum glucose levels in our patient population. Hyperglycemia has been associated with worse outcomes in other neurocritically ill patient groups, including those with aneurysmal subarachnoid hemorrhage [21], ischemic stroke [22–24], symptomatic hemorrhagic conversion after ischemic stroke [25], and TBI [26–28]. Concern has been raised over intensive glucose control in TBI (target range 4.4–6.1 mmol/L [80–110 mg/dL]), as several studies have suggested that intensive insulin therapy may result in reductions in brain glucose and elevation of biomarkers indicative of intracerebral cellular distress [29, 30]. Moreover, intensive glycemic control may not improve outcomes after TBI with a trend towards decreased survival at 21 days [31]. Although we do not practice intensive glucose control because of its associations with cerebral metabolic distress [29, 30] and allow serum glucose values up to 7.8 mmol/L (140 mg/dL), we cannot disprove the fact that the allowed range in our insulin protocol may have caused increased levels of cerebral metabolic distress and worse patient-related outcomes.
Among the neurological complications examined, brain edema requiring osmotherapy occurred in 37 % of patients and was strongly associated with increased hospital mortality, while herniation, noted in 39 % of all patients, was strongly associated with unfavorable functional outcome, but not mortality. This finding persisted, even after adjusting for the presence of hyponatremia or brain edema requiring osmotherapy in a different sensitivity analysis. Several reasons may exist for these findings. Herniation is a potentially reversible process when intervened upon early (i.e., bolus mannitol or hypertonic saline, or by neurosurgical intervention), which in turn may prevent death, but may still lead to significant disability at discharge. We did not collect information on different types of herniation, such as uncal versus tonsillar versus subfalcine, which may have a differential influence on mortality. In contrast, brain edema requiring osmotherapy may be a marker of particularly severe brain injury, which is not as easily reversible.
The sensitivity analysis after excluding early discharges and deaths within 48 h revealed several interesting findings. The relative frequencies after the exclusion of early discharges and deaths were increased in many, decreased in some, and unchanged in others. This observation provides important clues about the timing of the occurrence of these ICU complications during the ICU course. Complications with a decreased frequency after exclusion of early discharges and deaths indicate that they occur more often during this early time period, while complications with an increased frequency occur more frequently later in the hospital course. Complications with unchanged frequencies appear to be time-independent.
Study Strengths and Limitations
Important, unique strengths of our study include the prospective collection of strictly pre-defined ICU complications, the weekly critical review of these data by three board-certified neurointensivists, and centralized data adjudication.
Several limitations exist in our study, however, which must be kept in mind in the interpretation of our study results. Overall, the mortality rate in our study was high (35 %) and may have been due to older age in our cohort, but this is in line with the mortality rates reported in large, randomized-controlled trials and other cohort studies involving msTBI (26–36 %) [4, 14, 32, 33]. Only a small proportion of patients (17 %) had a GOS of 4 (able to live independently) or 5 (good recovery, able to return to work or school) at hospital discharge. This is not surprising given that our cohort was severely injured with a median presenting GCS of 5 and ISS of 27, and recovery from msTBI is often protracted requiring extensive rehabilitation. Therefore, ideally msTBI outcomes should be assessed for several months after injury. For the present analysis, long-term outcomes beyond hospital discharge were not available. Although we are now collecting these outcomes as part of the OPTIMISM study, many patients had not reached their long-term outcome assessment time points, resulting in insufficient power at the time of this analysis.
By assigning the value “1” to the verbal GCS in intubated patients, our GCS may have been skewed towards the lower end. However, we minimized possible GCS misclassification by assigning the enrollment GCS after resuscitation, after sedation and intoxication had worn off, and after possible extubation in the first 24 h. Cases with an enrollment GCS ≥13 were excluded from the study.
Other study limitations include limited generalizability due to the single-center design. Multi-modality monitoring was not performed, which may have provided important additional information on secondary brain injury in the context of systemic ICU complications. However, multi-modality monitoring is available only at a small number of academic neurological ICUs due to the high personnel and equipment costs. Therefore, our data more likely resembles that of a standard NTICU, and may be more generalizable. A small proportion of non-surviving msTBI patients received ICP monitoring (27 %), indicating that these patients were deemed unsalvageable. This may have confounded the association of ICP crisis with mortality or unfavorable hospital discharge outcome in our cohort. An additional limitation lies in the fact that many ICU complications may be iatrogenic, and their frequency may have been influenced by our ICU management practices. Finally, a larger and more homogeneous study cohort would have increased the stability of our point estimates as well as our power to identify additional complications that contribute to poor outcome and identify subgroups at varying risk for both medical and neurological complications and unfavorable patient outcomes. Since this study was an exploratory analysis of our data, we plan to perform multivariable adjustments in sub-cohorts in the future as the OPTIMISM study enrolls more patients.
In conclusion, our data show that the OPTIMISM study is feasible and that ICU complications are very common in patients with msTBI. In this exploratory analysis, we identified several potentially modifiable predictors of adverse outcome after msTBI, which contribute significantly to the variability in the outcome observed. Inclusion of ICU complications when prognosticating msTBI outcomes to families should be considered in patient and family discussions. Data from the OPTIMISM study, once validated in larger cohorts, may provide the basis upon which intervention trials targeting the prevention or treatment of these complications could be undertaken to evaluate whether important short as well as long-term patient-related outcomes can be improved.
References
Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5:e165.
Marmarou A, Lu J, Butcher I, et al. Prognostic value of the Glasgow Coma Scale and pupil reactivity in traumatic brain injury assessed pre-hospital and on enrollment: an IMPACT analysis. J Neurotrauma. 2007;24:270–80.
Roozenbeek B, Lingsma HF, Lecky FE, et al. Prediction of outcome after moderate and severe traumatic brain injury: external validation of the International Mission on Prognosis and Analysis of Clinical Trials (IMPACT) and Corticoid Randomisation After Significant Head injury (CRASH) prognostic models. Crit Care Med. 2012;40:1609–17.
Corral L, Javierre CF, Ventura JL, Marcos P, Herrero JI, Manez R. Impact of non-neurological complications in severe traumatic brain injury outcome. Crit Care. 2012;16:R44.
Piek J, Chesnut RM, Marshall LF, et al. Extracranial complications of severe head injury. J Neurosurg. 1992;77:901–7.
BrainTraumaFoundation. Guidelines for the management of severe traumatic brain injury. J Neurotrauma 2007;24(Suppl 1):S1–106.
ARDSNetwork. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–8.
Polderman KH, Rijnsburger ER, Peerdeman SM, Girbes AR. Induction of hypothermia in patients with various types of neurologic injury with use of large volumes of ice-cold intravenous fluid. Crit Care Med. 2005;33:2744–51.
Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–17.
Marshall LF, Marshall SB, Klauber MR, et al. The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma. 1992;9(Suppl 1):S287–92.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4.
Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21:2409–19.
Murray GD, Butcher I, McHugh GS, et al. Multivariable prognostic analysis in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:329–37.
Lingsma HF, Roozenbeek B, Steyerberg EW, Murray GD, Maas AI. Early prognosis in traumatic brain injury: from prophecies to predictions. Lancet Neurol. 2010;9:543–54.
Zygun DA, Kortbeek JB, Fick GH, Laupland KB, Doig CJ. Non-neurologic organ dysfunction in severe traumatic brain injury. Crit Care Med. 2005;33:654–60.
Ho KM, Burrell M, Rao S. Extracranial injuries are important in determining mortality of neurotrauma. Crit Care Med. 2010;38:1562–8.
Kourbeti IS, Papadakis JA, Neophytou C, et al. Infections in patients with traumatic brain injury who undergo neurosurgery. Br J Neurosurg. 2011;25:9–15.
King C, Garcia Alvarez L, Holmes A, Moore L, Galletly T, Aylin P. Risk factors for healthcare-associated urinary tract infection and their applications in surveillance using hospital administrative data: a systematic review. J Hosp Infect. 2012;82:219–26.
Siegel JH. The effect of associated injuries, blood loss, and oxygen debt on death and disability in blunt traumatic brain injury: the need for early physiologic predictors of severity. J Neurotrauma. 1995;12:579–90.
Wartenberg KE, Schmidt JM, Claassen J, et al. Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med. 2006;34:617–23.; quiz 24.
Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–32.
Fuentes B, Ortega-Casarrubios MA, Sanjose B, et al. Persistent hyperglycemia >155 mg/dL in acute ischemic stroke patients: how well are we correcting it? Implications for outcome. Stroke. 2010;41:2362–5.
Leigh R, Zaidat OO, Suri MF, et al. Predictors of hyperacute clinical worsening in ischemic stroke patients receiving thrombolytic therapy. Stroke. 2004;35:1903–7.
Kase CS, Furlan AJ, Wechsler LR, et al. Cerebral hemorrhage after intra-arterial thrombolysis for ischemic stroke: the PROACT II trial. Neurology. 2001;57:1603–10.
Melo JR, Di Rocco F, Blanot S, et al. Acute hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. Acta Neurochir (Wien). 2010;152:1559–65.
Jeremitsky E, Omert LA, Dunham CM, Wilberger J, Rodriguez A. The impact of hyperglycemia on patients with severe brain injury. J Trauma. 2005;58:47–50.
Salim A, Hadjizacharia P, Dubose J, et al. Persistent hyperglycemia in severe traumatic brain injury: an independent predictor of outcome. Am Surg. 2009;75:25–9.
Vespa P, Boonyaputthikul R, McArthur DL, et al. Intensive insulin therapy reduces microdialysis glucose values without altering glucose utilization or improving the lactate/pyruvate ratio after traumatic brain injury. Crit Care Med. 2006;34:850–6.
Vespa P, McArthur DL, Stein N, et al. Tight glycemic control increases metabolic distress in traumatic brain injury: a randomized controlled within-subjects trial. Crit Care Med. 2012;40:1923–9.
Meier R, Bechir M, Ludwig S, et al. Differential temporal profile of lowered blood glucose levels (3.5 to 6.5 mmol/l versus 5 to 8 mmol/l) in patients with severe traumatic brain injury. Crit Care. 2008;12:R98.
Edwards P, Arango M, Balica L, et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet. 2005;365:1957–9.
Yuan F, Ding J, Chen H, et al. Predicting outcomes after traumatic brain injury: the development and validation of prognostic models based on admission characteristics. J Trauma Acute Care Surg. 2012;73:137–45.
Acknowledgments
We appreciate the statistical advice from Bruce Barton, Ph.D., Research Professor of Biostatistics and Health Services Research, Department of Quantitative Health Sciences, University of Massachusetts Medical School, Worcester, MA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muehlschlegel, S., Carandang, R., Ouillette, C. et al. Frequency and Impact of Intensive Care Unit Complications on Moderate-Severe Traumatic Brain Injury: Early Results of the Outcome Prognostication in Traumatic Brain Injury (OPTIMISM) Study. Neurocrit Care 18, 318–331 (2013). https://doi.org/10.1007/s12028-013-9817-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-013-9817-2