Abstract
Background and objective
Adrenal incidentalomas (AIs) are lesions larger than 1 cm that are incidentally detected in the adrenal glands. Chest computed tomography (CCT) is widely used in the first evaluation of patients with suspected coronavirus disease (COVID-19) that resulted in many incidental findings in the thorax and upper abdomen. In this study, we aimed to investigate the frequency of AI and their effects on the course and outcome of COVID-19 regardless of functional status.
Material and methods
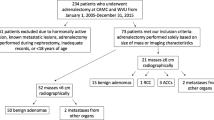
We included 2493 patients aged between 18 and 99 years and whose adrenal glands were clearly visible in CCT images. They were divided into two groups: those with AI (AI group) and without AI (Control group).
Results
AI was detected in 148 (5.93%) patients and 80 (54.1%) of them were male. There was no difference in sex distribution between the groups, but the median age of patients with AI was significantly higher than those without AI [54.5 (20–94 years) vs. 42 (18–99 years); p < 0.001)]. In addition, in the AI group, both hospitalizations due to COVID-19-related conditions (30.4 vs. 21.2%, p = 0.008) and the mortality rate experienced during this time was significantly higher (14.7 vs. 7%, p < 0.001) diseases. The AI group had a significantly higher comorbidity rate than the control group (61.5 vs. 41.9%, p < 0.001). The most common comorbid diseases were hypertension, cardiovascular diseases, diabetes mellitus, respiratory system diseases, and hyperlipidaemia. Advanced age and male gender in terms of mortality, advanced age and covid 19 positivity in terms of hospitalization were determined as significant risk factors.
Conclusions
The presence of AI may increase the morbidity and mortality rates associated with COVID-19, regardless of their functional status. Therefore, patients subjected to CCT imaging for COVID-19-related lung diseases should also be evaluated for AI. Careful follow-up of patients with COVID-19 and AI is necessary to monitor the progression of COVID-19.
Similar content being viewed by others
References
S. Umakanthan, P. Sahu, A.V. Ranade, M.M. Bukelo, J.S. Rao, L.F. Abrahao-Machado, S. Dahal, H. Kumar, D. Kv, Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad. Med. J. 96(1142), 753–758 (2020). https://doi.org/10.1136/postgradmedj-2020-138234
https://www.worldometers.info/coronavirus/ Last updated: January 24 2023, 21:12 GMT
H. Ejaz, A. Alsrhani, A. Zafar, H. Javed, K. Junaid, A.E. Abdalla, K.O.A. Abosalif, Z. Ahmed, S. Younas, COVID-19 and comorbidities: deleterious impact on infected patients. J. Infect. Public Health 13(12), 1833–1839 (2020). https://doi.org/10.1016/j.jiph.2020.07.014
A. Sanyaolu, C. Okorie, A. Marinkovic, et al., Comorbidity and its impact on patients with COVID-19. Compr. Clin. Med. 2(8), 1069–1076 (2020). https://doi.org/10.1007/s42399-020-00363-4
K.J. Clerkin, J.A. Fried, J. Raikhelkar, G. Sayer, J.M. Griffin, A. Masoumi, S.S. Jain, D. Burkhoff, D. Kumaraiah, L. Rabbani, A. Schwartz, N. Uriel, COVID-19 and cardiovascular disease. Circulation 141(20), 1648–1655 (2020). https://doi.org/10.1161/CIRCULATIONAHA.120.046941
Y.Y. Zheng, Y.T. Ma, J.Y. Zhang, X. **e, COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 17(5), 259–260 (2020). https://doi.org/10.1038/s41569-020-0360-5
M. Honardoost, L. Janani, R. Aghili, Z. Emami, M.E. Khamseh, The association between presence of comorbidities and COVID-19 severity: a systematic review and meta-analysis. Cerebrovasc. Dis. 50(2), 132–140 (2021). https://doi.org/10.1159/000513288
A. Gasmi, M. Peana, L. Pivina, S. Srinath, A. Gasmi Benahmed, Y. Semenova, A. Menzel, M. Dadar, G. Bjørklund, Interrelations between COVID-19 and other disorders. Clin. Immunol. 224, 108651 (2021). https://doi.org/10.1016/j.clim.2020.108651
Araujo-Castro et al. Predictors of tumour growth and autonomous cortisol secretion development during follow-up in non-functioning adrenal incidentalomas. J. Clin. Med. 10(23), 5509 (2021)
I. Bancos, A. Prete, Approach to the patient with adrenal incidentaloma. J. Clin. Endocrinol. Metab. 106(11), 3331–3353 (2021). https://doi.org/10.1210/clinem/dgab512
W.F. Young Jr, Clinical practice. The incidentally discovered adrenal mass. N. Engl. J. Med. 356(6), 601–10 (2007). https://doi.org/10.1056/NEJMcp065470
E. Kebebew, Adrenal Incidentaloma. N. Engl. J. Med. 384(16), 1542–1551 (2021). https://doi.org/10.1056/NEJMcp2031112
Y.S. Elhassan, et al., Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess: a systematic review and meta-analysis. Ann. Intern. Med. 171(2), 107–116 (2019). https://doi.org/10.7326/M18-3630
M. Barbot, M. Zilio, C. Scaroni, Cushing’s syndrome: overview of clinical presentation, diagnostic tools and complications. Best. Pract. Res. Clin. Endocrinol. Metab. 34(2), 101380 (2020). https://doi.org/10.1016/j.beem.2020.101380
L. Papanastasiou, K.I. Alexandraki, I.I. Androulakis, S. Fountoulakis, T. Kounadi, A. Markou, V. Tsiavos, C. Samara, T.G. Papaioannou, G. Piaditis, G. Kaltsas, Concomitant alterations of metabolic parameters, cardiovascular risk factors and altered cortisol secretion in patients with adrenal incidentalomas during prolonged follow-up. Clin. Endocrinol. 86(4), 488–498 (2017). https://doi.org/10.1111/cen.13294
C. Aresta, V. Favero, V. Morelli, L. Giovanelli, C. Parazzoli, A. Falchetti, F. Pugliese, L. Gennari, F. Vescini, A. Salcuni, A. Scillitani, L. Persani, I. Chiodini, Cardiovascular complications of mild autonomous cortisol secretion. Best. Pract. Res Clin. Endocrinol. Metab. 35(2), 101494 (2021). https://doi.org/10.1016/j.beem.2021
M. Araujo-Castro, C. Robles Lázaro, P. Parra Ramírez, M. Cuesta Hernández, M.A. Sampedro Núñez, M. Marazuela, Cardiometabolic profile of non-functioning and autonomous cortisol-secreting adrenal incidentalomas. Is the cardiometabolic risk similar or are there differences? Endocrine 66(3), 650–659 (2019). https://doi.org/10.1007/s12020-019-02066-w
M. Araujo-Castro, C. Mínguez Ojeda, M.N. Sánchez Ramírez, V. Gómez Dos Santos, E. Pascual-Corrrales, M. Fernández-Argüeso, Adrenalectomy improves blood pressure control in nonfunctioning adrenal incidentalomas and glycemic and lipid control in patients with autonomous cortisol secretion. Endocrine 78(1), 142–150 (2022). https://doi.org/10.1007/s12020-022-03120-w
Z. Ye, Y. Zhang, Y. Wang, Z. Huang, B. Song, Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur. Radio. 30(8), 4381–4389 (2020). https://doi.org/10.1007/s00330-020-06801-0
P.C. Jacobs, W.P. Mali, D.E. Grobbee, Y. van der Graaf, Prevalence of incidental findings in computed tomographic screening of the chest: a systematic review. J. Comput. Assist. Tomogr. 32(2), 214–21 (2008). https://doi.org/10.1097/RCT.0b013e3181585ff2
O. Anjum, H. Bleeker, R. Ohle, Computed tomography for suspected pulmonary embolism results in a large number of non-significant incidental findings and follow-up investigations. Emerg. Radio. 26(1), 29–35 (2019). https://doi.org/10.1007/s10140-018-1641-8
https://www.worldometers.info/coronavirus/country/turkey/ Last updated: January 25 2023, 21:59 GMT
https://www.worldometers.info/coronavirus/coronavirus-death-rate/
S. Salehi, A. Abedi, S. Balakrishnan, A. Gholamrezanezhad, Coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS) and common lexicon: a proposal based on the imaging data of 37 studies. Eur. Radio. 30(9), 4930–4942 (2020). https://doi.org/10.1007/s00330-020-06863-0
T.C. Kwee, R.M. Kwee, Chest CT in COVID-19: What the radiologist needs to know. radiographics 40(7), 1848–1865 (2020). https://doi.org/10.1148/rg.2020200159
M. Romeih, M.R. Mahrous, M. El Kassas, Incidental radiological findings suggestive of COVID-19 in asymptomatic patients. World J. Radio. 14(1), 1–12 (2022). https://doi.org/10.4329/wjr.v14.i1.1
H. Pavan, T.S. Garcia, F.S. Torres, F.F. Gazzoni, L. Folador, C.L.A. Ghezzi, Focal incidental upper abdominal findings on unenhanced chest computed tomography that do not require further imaging: a roadmap for the thoracic radiologist. Radio. Bras. 55(3), 173–180 (2022). https://doi.org/10.1590/0100-3984.2021.0106
E.J. Mortani Barbosa Jr, O. Osuntokun, Incidental findings in thoracic CTs performed in trauma patients: an underestimated problem. Eur. Radio. 29(12), 6772–6779 (2019). https://doi.org/10.1007/s00330-019-06313-6
J. Kim, K.H. Bae, Y.K. Choi, J.Y. Jeong, K.G. Park, J.G. Kim, I.K. Lee, Clinical characteristics for 348 patients with adrenal incidentaloma. Endocrinol. Metab. 28(1), 20–5 (2013). https://doi.org/10.3803/EnM.2013.28.1.20
M.J. Sangwaiya, G.W. Boland, C.G. Cronin, M.A. Blake, E.F. Halpern, P.F. Hahn, Incidental adrenal lesions: accuracy of characterization with contrast-enhanced washout multidetector CT–10-minute delayed imaging protocol revisited in a large patient cohort. Radiology 256(2), 504–10 (2010). https://doi.org/10.1148/radiol.10091386
J.J. Park, B.K. Park, C.K. Kim, Adrenal imaging for adenoma characterization: imaging features, diagnostic accuracies and differential diagnoses. Br. J. Radio. 89(1062), 20151018 (2016). https://doi.org/10.1259/bjr.20151018
G. Akkus, M. Evran, M. Sert, T. Tetiker, Adipocytokines in non-functional adrenal incidentalomas and relation with insulin resistance parameters. Endocr. Metab. Immune Disord. Drug Targets 19(3), 326–332 (2019). https://doi.org/10.2174/1871530318666181009112042
R. Emral, B.İ. Aydoğan, A.D. Köse, Ö. Demir, D. Çorapçıoğlu, Could a nonfunctional adrenal incidentaloma be a risk factor for increased carotid intima-media thickness and metabolic syndrome. Endocrinol. Diabetes Nutr. (Engl. Ed.) 66(7), 402–409 (2019). https://doi.org/10.1016/j.endinu.2019.01.007. English, Spanish
M. Araujo-Castro, Cardiometabolic profile and urinary metabolomic alterations in non-functioning adrenal incidentalomas: a review. Clin. Endocrinol. 97(6), 693–701 (2022). https://doi.org/10.1111/cen.14745
S. Yener, M. Baris, M. Secil, B. Akinci, A. Comlekci, S. Yesil, Is there an association between non-functioning adrenal adenoma and endothelial dysfunction? J. Endocrinol. Invest 34(4), 265–70 (2011). https://doi.org/10.1007/BF03347083
S. Yener, Metabolic and cardiovascular impact of non-functioning adrenal adenomas: a clinical dilemma. Eur. J. Intern. Med. 24(6), 520–4 (2013). https://doi.org/10.1016/j.ejim.2013.02.005
G. Di Dalmazi, V. Vicennati, S. Garelli, E. Casadio, E. Rinaldi, E. Giampalma, C. Mosconi, R. Golfieri, A. Paccapelo, U. Pagotto, R. Pasquali, Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: a 15-year retrospective study. Lancet Diabetes Endocrinol. 2(5), 396–405 (2014). https://doi.org/10.1016/S2213-8587(13)70211-0
Y. Chen, S.L. Klein, B.T. Garibaldi, H. Li, C. Wu, N.M. Osevala, T. Li, J.B. Margolick, G. Pawelec, S.X. Leng, Aging in COVID-19: vulnerability, immunity and intervention. Ageing Res. Rev. 65, 101205 (2021). https://doi.org/10.1016/j.arr.2020.101205
X. Fang, S. Li, H. Yu, P. Wang, Y. Zhang, Z. Chen, Y. Li, L. Cheng, W. Li, H. Jia, X. Ma, Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis. Aging 12(13), 12493–12503 (2020). https://doi.org/10.18632/aging.103579
J.J. Zhang, X. Dong, G.H. Liu, Y.D. Gao, Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin. Rev. Allergy Immunol. 64(1), 90–107 (2023). https://doi.org/10.1007/s12016-022-08921-5
D. Müller-Wieland, N. Marx, M. Dreher, K. Fritzen, O. Schnell, COVID-19 and cardiovascular comorbidities. Exp. Clin. Endocrinol. Diabetes 130(3), 178–189 (2022). https://doi.org/10.1055/a-1269-1405
M. Eidininkienė, J. Cesarskaja, S. Talačkaitė, V. Traškaitė-Juškevičienė, A. Macas, Co-existing diseases and COVID-19-a one way ticket? Int. J. Environ. Res. Public Health 19(8), 4738 (2022). https://doi.org/10.3390/ijerph19084738
S. Das, R.A. K, S.R. Birangal, A.N. Nikam, A. Pandey, S. Mutalik, A. Joseph, Role of comorbidities like diabetes on severe acute respiratory syndrome coronavirus 2: a review. Life Sci. 258, 118202 (2020). https://doi.org/10.1016/j.lfs.2020.118202
Acknowledgements
We commemorate with respect and gratitude our friend, Dr. Yavuz Durmuş, with whom we conducted this research and who died due to COVID-19. We thank the Turkish Society of Endocrinology and Metabolism Diseases for funding the language revision of this study.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
M.G. designed the study and wrote the main manuscript text. B.B.A. collected patient data and contributed to data analysis, and T.S. performed detailed examination of radiological images. S.K. reviewed the article and contributed to its writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests. No payment has been made to any of authors due to all researchers working in the same hospital and collaborated voluntary.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Metin Guclu, Bilal Burcak Aslan
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guclu, M., Aslan, B.B., Setayeshi, T. et al. Could the presence of adrenal incidentaloma negatively affect COVID 19 outcomes?. Endocrine 82, 406–413 (2023). https://doi.org/10.1007/s12020-023-03454-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03454-z