Abstract
Early identification of patients with a poorer prognosis in the Emergency Department (ED) is crucial for prompt treatment and resource allocation. We investigated the relationship between the Neutrophil to Lymphocyte Ratio (NLR) and 30-day mortality in elderly acute medical patients. Prospective single-center cohort study including consecutive patients admitted to the ED. Inclusion criteria were age > 65 years and medical condition as the cause of ED access. Exclusion criteria were patients admitted for traumatic injuries or non-traumatic surgical diseases. ROC analysis was used to set the best cut-off of the NLR for mortality. 953 patients were included and 142 (14.9%) died during follow-up. ROC analysis showed a good predictive value of the NLR with an AUC 0.70, 95%CI 0.67–0.73 (p < 0.001) and identified a NLR > 8 as the best cut-off. Patients with NLR > 8 had a more serious triage code (72.6% had a triage code ≤ 2) and an increased heart rate and body temperature. They more often presented with dyspnea, abdominal pain, falls and vomiting. They also were characterized by an increase in urea, creatinine, white blood cells, neutrophils, fibrinogen, D-dimer, glycemia, CRP, LDH and transaminases and by a decrease in eGFR, of lymphocytes and monocytes. Multivariable logistic regression analysis demonstrated that the NLR remained associated with mortality after adjustment for confounders (Odds ratio 2.563, 95%CI 1.595–4.118, p < 0.001). Patients with NLR > 8 showed a higher mortality rate. NLR is an easy and inexpensive tool that may be used for risk stratification in the ED. The results of this study need to be validated in larger external cohorts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In today’s healthcare landscape, one of the paramount challenges facing emergency departments (EDs) is the accurate risk stratification of elderly patients. As the population ages, EDs are witnessing a growing influx of older adults seeking medical attention, often presenting with complex and multifaceted health issues. Effectively assessing the risk associated with these patients is crucial, as it directly impacts clinical decision-making, resource allocation, and the overall quality of care provided [1,2,3]. In-hospital mortality for patients older than 65 was found to be between 8.2% and 22.8% when admitted for acute conditions [4,5,6].
Currently the risk stratification is performed through clinical scores that are specific for each disease (i.e., SOFA score, Ranson’s criteria), but general criteria that can help the clinician identify patients at high risk of death are lacking. As the rapid identification of high-risk patients is crucial for the early initiation of evidence-based life-saving treatment and management, new scores and biomarkers are being tested with this aim.
One of those is the neutrophil-to-lymphocyte ratio (NLR), which is a simple and inexpensive score calculated as a ratio between the neutrophil and lymphocyte counts. NLR is a biomarker that takes into account two faces of the immune system: the innate immune response, mainly due to neutrophils, and adaptive immunity, supported by lymphocytes [7, 8]. Several studies reported the prognostic value of NLR and its role as a marker of systemic inflammations in numerous pathologies such as chronic obstructive pulmonary disease (COPD), atrial fibrillation, coronary artery disease (CAD), sepsis, and acute pancreatitis [9,10,11,12,13,14,15,16,17,18,19,20,21]. Furthermore, the kinetic of this biomarker is really fast, NLR is thought to change within 6 h of the onset of physiologic stress, far earlier than other markers such as white cell count or C-reactive protein (CRP)[22].
Given those premises and the association with poor outcomes in different conditions, NLR could be useful in risk stratification of patients presenting to the ED with non-surgical conditions.
The aim of this study was to assess the value in the risk stratification of the NLR, its capability to predict all-cause mortality in patients presenting to the ED and establish a cut-off for elderly acute medical patients.
Methods
Study design and population
This was a single centre, prospective, observational study which included consecutive patients presenting to the ED of the Policlinico Universitario Umberto I in Rome between the 28th of April and the 28th of May 2022. Adult patients older than 65 years old presenting to the ED were enrolled after providing written informed consent. Patients presenting for a traumatic injury or non-traumatic surgical diseases and SARS-CoV-2 positive patients were excluded from the study. The study was carried out according to the principles of the Declaration of Helsinki and approved by the Sapienza University of Rome Ethics committee (Prot. 0405/2022). Reporting is in accordance with the STROBE statement. The authors designed the study, gathered, and analyzed the data anonymously, vouched for the data and analysis, wrote the manuscript, and decided to submit it for publication.
Relative NLR calculation
The relative neutrophil–lymphocyte ratio (NLR) was calculated as follows: (% neutrophil count, cells/μL)/(% lymphocyte count, cells/μL).
Routine clinical assessment
All patients underwent clinical assessment that included medical history, physical examination, standard blood tests, 12-lead electrocardiogram (ECG) and vital parameters at admission, everything was documented on the medical records. ED discharge diagnosis was prospectively documented. Management of patients was left to the discretion of the attending physician.
Triage and priority codes
At entry into the ED, patients are assigned a code with decremental priority ranging from 1 to 5 depending on their severity. In detail: Code 1: interruption or impairment of one or more vital functions with immediate access; Code 2: risk of impairment of vital functions. Condition with developmental risk or severe pain access within 15 min; Code 3: deferrable urgency stable condition without developmental risk with suffering and effect on the general state which usually requires complex services access within 60 min; Code 4: green minor urgency stable condition without developmental risk which usually requires simple single specialist diagnostic therapeutic services access within 120 min; Code 5: non-urgent problem not urgent or of minimum clinical relevance access within 240 min (source Italian Ministry of Health website: https://www.salute.gov.it/imgs/C_17_pubblicazioni_3145_allegato.pdf).
Follow-up and clinical endpoints
Information regarding death during follow-up were obtained from the patient’s hospital records and the national death registry. The primary endpoint was all-cause mortality at 30 days.
Statistical analysis
Continuous variables are presented as average and standard deviation (SD) or median and interquartile range [IQR] and compared using the student t- test or the Mann–Whitney U test as appropriate. Categorical variables are presented as count and percentages (%) and compared with the Pearson χ2 test or Fisher exact test, as appropriate.
The descriptive analysis was performed by comparing patients with a NLR below or above 8 and according to the vital status at 30 days. To calculate the odds ratio (OR) and its 95% confidence intervals (95% CI) for all-cause mortality at 30 days a univariable and multivariable logistic regression analysis was performed. In the multivariable model, we inserted significant variables from univariable regression analysis.
In detail, we inserted the following variables into the multivariable model: relative NLR > 8, female sex, age, SBP, shock, respiratory rate, swollen legs, atrial fibrillation (AF), altered mental status, active cancer, blood glucose, GOT/AST, hemoglobin, creatinine, LDH, and mean platelet volume (MPV). Other significant variables were not inserted if collinear (as an example total WBC, neutrophil or lymphocytes, CRP with NLR, dyspnoea with respiratory rate, insulin use with blood glucose).
We also built the receiver operating characteristic (ROC) curve with the value of the Youden index to test the predictive value of the NLR in the whole population and in the subgroup of women.
All hypothesis testing was two-tailed and P values of less than 0.05 were considered to indicate statistical significance without adjustments for multiple testing. Statistical analyses were performed using IBM SPSS 25 and MedCalc.
Results
Study population and characteristics
We included 1074 consecutive patients. Of these, 121 were excluded due to lack of personal data or for not having performed blood tests before discharge. Therefore, 953 patients remained available for analysis. Out of those, 267 (28%) had an NLR > 8.
The characteristics of the population, stratified by NLR values above or below 8, are shown in Table 1.
When admitted to the ED, patients with NLR > 8, compared to those with a NLR < 8, were older and characterized by a more serious triage code (only 1% had a triage code = 4, while 72.6% had a triage code ≤ 2) and by an increased heart rate and body temperature. They more often presented with dyspnea, abdominal pain, falls and vomiting. Regarding comorbidities, there were no significant differences between the two groups.
Patients with a NLR > 8 were more frequently on chronic therapy with diuretics; they are also characterized by an increase in urea, creatinine, white blood cells, neutrophils, fibrinogen, D-dimer, glycemia, CRP, lactate dehydrogenase (LDH) and by a decrease in the estimated glomerular filtration rate (eGFR), of lymphocytes and monocytes (Table 1).
Mortality
A total of 27 patients were lost during follow-up, therefore, the survival analysis was performed on a cohort of 926 patients. In total, 142 (15.3%) patients died in-hospital or during the 30-day follow-up. Those patients who died during the follow-up were characterized by a more severe triage code, they were older and presented with a higher respiratory rate. In terms of symptoms and signs, the occurrence of an adverse outcome was more often associated with shock, dyspnea, swollen legs, vertigo, altered mental status, vomiting and diarrhea at presentation (Table 2). In our cohort, COPD, atrial fibrillation, dementia and active cancer were the comorbidities more commonly found in those patients who died during follow-up. The remaining characteristics stratified by vital status are presented in Table 2.
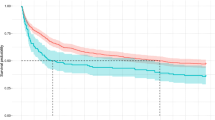
Association of NLR with mortality
In our cohort, the NLR as a continuous value reached an AUC of 0.70 (95%CI 0.67–0.73 p < 0.001) for the outcome of all-cause mortality at 30 days (on 926 patients for whom survival data were available) (Fig. 1).
This value was consistent in the group of women (n = 456, 71 deaths) with an AUC of 0.71, 95%CI 0.67–0.75 and a best cut-off of > 4.47. The optimal calculated cut-off for this variable in our cohort was 8.
To analyze the relationship between all-cause mortality and different predictors we built a logistic regression model. The OR of having a NLR > 8 was 2.563 (95%CI 1.595–4.118) with a p < 0.001. Another strong association with the outcome was found to be an altered mental status at presentation with an OR of 3.610 (95%CI 1.976–6.596). The results for the other predictors are shown in Table 3.
Discussion
In this analysis including almost 1000 patients, we have described the characteristics of elderly patients presenting to the ED for acute medical conditions according to their NLR at presentation. We found that NLR is an independent predictor of mortality during 30 days of follow-up. In particular, we found an optimized cut-off of NLR > 8 specific for acute medical patients aged > 65 years, which differs from previous studies. Patients admitted with a NLR > 8 had specific characteristics with a generally more severe disease presentation.
In our cohort, the mortality rate at 30 days was 15.3%. In the literature, we found very heterogeneous reports about short-term mortality in elderly patients admitted to the ED, ranging from 8 to 25% [2, 23, 24].
Byrne DG et al. found in a cohort of 23,114 patients that 25.8% were over the age of 75 years. For this group, the 30-day mortality was 20.7% compared with 4.5% for younger patients [25]. In these studies, the main symptoms associated with adverse outcomes were delirium, hypoxemia, unconsciousness at presentation, female sex, age [23, 24]. Our results are in line with those previous findings, showing that respiratory rate, altered mental status, and systolic blood pressure were associated with an increased risk of mortality.
Our main finding relies on the clinically useful predictive value of the NLR in acute elderly medical patients. We used an optimized cut-off for NLR > 8, providing an AUC of 0.70. This value is in line with many other clinical scores currently used in clinical practice [26, 27].
In our cohort, 28% of patients had a NLR > 8. These patients had more severe symptoms and signs at presentation. Patients with a NLR > 8 showed a 2.5-fold higher risk of dying during the follow-up.
Different cut-off values for the NLR have been proposed in recent publications, depending on the clinical setting and underlying pathology [8]. Regolo M. et al. showed that in-hospital mortality in COVID-19 patients is predicted by a NLR > 11.38 (AUC = 0.77, p < 0.001) [26].
In patients older than 80 years hospitalized a NLR on admission > 2.97 (sensitivity of 92.6% and specificity of 52.5%, AUC = 0.714, p = 0.001) was an independent predictor of all-cause 3-month mortality [27]. Similarly, in a cohort of more than 5000 hospitalized geriatric patients an NLR higher than 7.95 was associated with in-hospital mortality with an AUC of 0.707 (0.686–0.728) [28]. This is in line with our results, showing that the NLR could be useful in risk stratification for all-cause mortality in elderly patients presenting to the ED for medical conditions. Furthermore, a test that could quickly classify nearly 30% of such patients as low-risk of short term mortality could be an additional support to emergency physicians for a safe discharge.
This laboratory value can be obtained quickly as part of the laboratory routine and is inexpensive. Given the lack of systematic risk stratification strategies, the proposal of the simple NLR in the setting of the emergency may be particularly useful.
Another interesting finding is the association of MPV with mortality. This is in line with previous studies in literature. In fact, an increased MPV seems to correlate with higher mortality in patients suffering from myocardial infarction, critically ill patients and in septic patients [29,30,31]. This could reflect a systemic inflammatory response, as inflammation, endothelial dysfunction and thrombotic conditions may alter platelet size [32].
Some limitations should be considered when interpreting these findings. First, patients with traumatic injuries were excluded from this study, therefore, we cannot generalize our findings to those patients. Then, the value of NLR can be falsely increased in some patients. As described by Karakonstantis et al., factors such as age, exogenous steroid intake, endogenous sexual hormones, active hematological disorders, such as leukemia, cytotoxic or granulocyte colony-stimulating factor chemotherapies, and HIV can determine an increase of the NLR [33].
In conclusion, NLR is a simple tool that is associated with the severity of presentation and all-cause mortality; therefore, elderly patients with a NLR > 8 should be early identified as being at higher risk of adverse outcomes and promptly managed.
Data availability
The data that support the findings of this study are available from the authors but restrictions apply to the availability of these data and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from Ethical Committee.
References
Aminzadeh F, Dalziel WB (2002) Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 39:238–247. https://doi.org/10.1067/mem.2002.121523
Karamercan MA, Dündar DZ, Slagman A, Ergin M, Janssens KAC, Fabbri A, Bjornsen LP, Somodi S, Adam VN, Polyzogopoulou E, Demir HA, Laribi S, on behalf of the EGERS study investigators (2023) Epidemiology of geriatric patients presenting to emergency departments in Europe: EGERS study. Eur J Emerg Med 30:117–124. https://doi.org/10.1097/MEJ.0000000000000997
Valli G, Galati E, De Marco F, Bucci C, Fratini P, Cennamo E, Ancona C, Volpe N, Ruggieri MP (2021) In-hospital mortality in the emergency department: clinical and etiological differences between early and late deaths among patients awaiting admission. Clin Exp Emerg Med 8:325–332. https://doi.org/10.15441/ceem.21.020
Barba R, Martínez JM, Zapatero A, Plaza S, Losa JE, Canora J, Pérez A, De Casasola GG (2011) Mortality and complications in very old patients (90+) admitted to departments of internal medicine in Spain. Eur J Intern Med 22:49–52. https://doi.org/10.1016/j.ejim.2010.11.001
Ayaz T, Sahin SB, Sahin OZ, Bilir O, Rakıcı H (2014) Factors affecting mortality in elderly patients hospitalized for nonmalignant reasons. J Aging Res 2014:1–7. https://doi.org/10.1155/2014/584315
Socorro García A, De La Puente M, Perdomo B, López Pardo P, Baztán JJ (2015) Functional status and mortality at month and year in nonagenarians hospitalized due to acute medical illness. Eur J Intern Med 26:705–708. https://doi.org/10.1016/j.ejim.2015.08.007
Song M, Graubard BI, Rabkin CS, Engels EA (2021) Neutrophil-to-lymphocyte ratio and mortality in the United States general population. Sci Rep 11:464. https://doi.org/10.1038/s41598-020-79431-7
Buonacera A, Stancanelli B, Colaci M, Malatino L (2022) Neutrophil to lymphocyte ratio: an emerging marker of the relationships between the immune system and diseases. Int J Mol Sci 23:3636. https://doi.org/10.3390/ijms23073636
Teng F, Ye H, Xue T (2018) Predictive value of neutrophil to lymphocyte ratio in patients with acute exacerbation of chronic obstructive pulmonary disease. PLoS One 13:e0204377. https://doi.org/10.1371/journal.pone.0204377
Lu F-Y, Chen R, Li N, Sun X-W, Zhou M, Li Q-Y, Guo Y (2021) Neutrophil-to-lymphocyte ratio predicts clinical outcome of severe acute exacerbation of COPD in frequent exacerbators. Int J Chron Obstruct Pulmon Dis 16:341–349. https://doi.org/10.2147/COPD.S290422
El-Gazzar AG, Kamel MH, Elbahnasy OKM, El-Naggar ME-S (2020) Prognostic value of platelet and neutrophil to lymphocyte ratio in COPD patients. Expert Rev Respir Med 14:111–116. https://doi.org/10.1080/17476348.2019.1675517
Hao S, Yuan Y, Ye W, Fang X (2023) Association between neutrophil-lymphocyte ratio and all-cause mortality in critically ill patients with chronic obstructive pulmonary disease: a retrospective cohort study. Med Sci Monit https://doi.org/10.12659/MSM.938554
Gibson PH, Cuthbertson BH, Croal BL, Rae D, El-Shafei H, Gibson G, Jeffrey RR, Buchan KG, Hillis GS (2010) Usefulness of neutrophil/lymphocyte ratio as predictor of new-onset atrial fibrillation after coronary artery bypass grafting. Am J Cardiol 105:186–191. https://doi.org/10.1016/j.amjcard.2009.09.007
Shao Q, Chen K, Rha S-W, Lim H-E, Li G, Liu T (2015) Usefulness of neutrophil/lymphocyte ratio as a predictor of atrial fibrillation: a meta-analysis. Arch Med Res 46:199–206. https://doi.org/10.1016/j.arcmed.2015.03.011
Saliba W, Barnett-Griness O, Elias M, Rennert G (2015) Neutrophil to lymphocyte ratio and risk of a first episode of stroke in patients with atrial fibrillation: a cohort study. J Thromb Haemost 13:1971–1979. https://doi.org/10.1111/jth.13006
Wu S, Yang Y, Zhu J, Ren J, Wang J, Zhang H, Shao X (2021) Impact of baseline neutrophil-to-lymphocyte ratio on long-term prognosis in patients with atrial fibrillation. Angiology 72:819–828. https://doi.org/10.1177/00033197211000495
Huang Z, Fu Z, Huang W, Huang K (2020) Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: a meta-analysis. Am J Emerg Med 38:641–647. https://doi.org/10.1016/j.ajem.2019.10.023
Zhou H, Mei X, He X, Lan T, Guo S (2019) Severity stratification and prognostic prediction of patients with acute pancreatitis at early phase: A retrospective study. Medicine (Baltimore) 98:e15275. https://doi.org/10.1097/MD.0000000000015275
Cifci M, Halhalli HC (2020) The Relationship between neutrophil-lymphocyte and platelet-lymphocyte ratios with hospital stays and mortality in the emergency department. Cureus. https://doi.org/10.7759/cureus.12179
Li X, Ji Y, Kang J, Fang N (2018) Association between blood neutrophil-to-lymphocyte ratio and severity of coronary artery disease: Evidence from 17 observational studies involving 7017 cases. Medicine (Baltimore) 97:e12432. https://doi.org/10.1097/MD.0000000000012432
Sager HB, Koenig W (2021) Immune cell-based cardiovascular risk assessment: spotlight on the neutrophil–lymphocyte ratio. Eur Heart J 42:904–906. https://doi.org/10.1093/eurheartj/ehaa1104
Honda T, Uehara T, Matsumoto G, Arai S, Sugano M (2016) Neutrophil left shift and white blood cell count as markers of bacterial infection. Clin Chim Acta 457:46–53. https://doi.org/10.1016/j.cca.2016.03.017
Morales Erazo A, Cardona Arango D (2017) Factores pronósticos de mortalidad temprana en ancianos ingresados en un servicio de urgencias. Rev Esp Geriatría Gerontol 52:257–260. https://doi.org/10.1016/j.regg.2017.05.004
Olsson H, Karlson BW, Herlitz J, Karlsson T, Hellberg J, Prytz M, Sernert N, Ekerstad N (2022) Predictors of short- and long-term mortality in critically ill, older adults admitted to the emergency department: an observational study. BMC Emerg Med 22:15. https://doi.org/10.1186/s12873-022-00571-2
Byrne DG, Chung SL, Bennett K, Silke B (2010) Age and outcome in acute emergency medical admissions. Age Ageing 39:694–698. https://doi.org/10.1093/ageing/afq114
Regolo M, Vaccaro M, Sorce A, Stancanelli B, Colaci M, Natoli G, Russo M, Alessandria I, Motta M, Santangelo N, Fiorito L, Giarrusso O, Giangreco F, Arena A, Noto P, Ciampi C, Carpinteri G, Malatino L (2022) Neutrophil-to-lymphocyte ratio (NLR) is a promising predictor of mortality and admission to intensive care unit of COVID-19 patients. J Clin Med 11:2235. https://doi.org/10.3390/jcm11082235
Sun X, Luo L, Zhao X, Ye P, Du R (2017) The neutrophil-to-lymphocyte ratio on admission is a good predictor for all-cause mortality in hypertensive patients over 80 years of age. BMC Cardiovasc Disord 17:167. https://doi.org/10.1186/s12872-017-0595-1
Di Rosa M, Sabbatinelli J, Soraci L, Corsonello A, Bonfigli AR, Cherubini A, Sarzani R, Antonicelli R, Pelliccioni G, Galeazzi R, Marchegiani F, Iuorio S, Colombo D, Burattini M, Lattanzio F, Olivieri F (2023) Neutrophil-to-lymphocyte ratio (NLR) predicts mortality in hospitalized geriatric patients independent of the admission diagnosis: a multicenter prospective cohort study. J Transl Med 21:835. https://doi.org/10.1186/s12967-023-04717-z
Wang J, Ma X, Si X, Wu M, Han W (2023) Mean platelet volume and the association with all-cause mortality and cardiovascular mortality among incident peritoneal dialysis patients. BMC Cardiovasc Disord 23:543. https://doi.org/10.1186/s12872-023-03551-x
Zampieri FG, Ranzani OT, Sabatoski V, De Souza HP, Barbeiro H, Da Neto LMC, Park M, Da Silva FP (2014) An increase in mean platelet volume after admission is associated with higher mortality in critically ill patients. Ann Intensive Care 4:20. https://doi.org/10.1186/s13613-014-0020-1
Vélez-Páez JL, Legua P, Vélez-Páez P, Irigoyen E, Andrade H, Jara A, López F, Pérez-Galarza J, Baldeón L (2022) Mean platelet volume and mean platelet volume to platelet count ratio as predictors of severity and mortality in sepsis. PLoS One 17:e0262356. https://doi.org/10.1371/journal.pone.0262356
Yuri Gasparyan A, Ayvazyan L, Mikhailidis PD, Kitas G (2011) Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des 17:47–58. https://doi.org/10.2174/138161211795049804
Karakonstantis S, Kalemaki D, Tzagkarakis E, Lydakis C (2018) Pitfalls in studies of eosinopenia and neutrophil-to-lymphocyte count ratio. Infect Dis 50:163–174. https://doi.org/10.1080/23744235.2017.1388537
Acknowledgements
We are indebted to the patients who participated in the study and to the emergency department staff for their most valuable efforts. ROMA-ED (Research On Medical patients Admitted to the Emergency Department) Investigators to be listed as contributors: Sara Cerretti, Elisa Fante, Fabrizio Urso, Enrico Baldini, Laura Zinnamosca, Maria Alessandroni, Grazia Loiudice, Chiara Boccardo, Enrico Petrillo, Giada Della Grotta, Leonardo Magrini, Marina Colzi, Cristiana Gianni, Federica Biamonte, Antonio Concistrè, Antonella Ponzio, Cristiana Franchi, Cristiano Marinelli, Tecla Pecci, Flavia Fabi, Giona Roma, Alessandra Massi, Alina Diaczenko, Mauro Casagrande. Valentina Di Manno, Maria Civita Cedrone, Rosaria Berardi, Lorenzo Vantaggio, Andrea Corrao, Katia Fazi, Anna Criniti, Carla Lubrano, Maria Santulli, Antonio Angeloni, Emiliano Lorusso, Simona Giglio.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. This work was supported by research grants from Sapienza University of Rome (Number AR12218169611EB8).
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Daniele Pastori and Gioacchino Galardo. The first draft of the manuscript was written by Gioacchino Galardo and Luca Crisanti, all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors designed the study, gathered and analyzed the data, vouched for the data and analysis, wrote the paper, and decided to publish. Drs. Pastori, Galardo, and Pugliese had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The manuscript and its contents have not been published previously and are not being considered for publication elsewhere in whole or in part in any language, including publicly accessible websites or e-print servers. All other authors declare that they have no conflict of interest with this study.
Ethical approval
The study was carried out according to the principles of the Declaration of Helsinki and approved by the Sapienza University of Rome Ethics committee (Prot. 0405/2022).
Informed consent
Written informed consent was obtained from the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Research on Medical patients admitted to the Emergency Department (ROMA-ED) investigators list are listed in Acknowledgements section.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Galardo, G., Crisanti, L., Gentile, A. et al. Neutrophil to lymphocyte ratio (NLR) and short-term mortality risk in elderly acute medical patients admitted to a University Hospital Emergency Department. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03683-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03683-8