Abstract
Background
Proximal Roux-en-Y gastric bypass is commonly used to manage obesity, performed using laparoscopic or robot-assisted minimally invasive surgery. As the prevalence of robotic bariatric surgery increases, further data is required to justify its use.
Methods
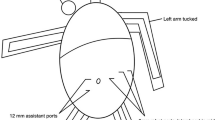
This was a large, retrospective analysis of prospectively recorded data for Roux-en-Y gastric bypass (RYGB) procedures performed using laparoscopic (LRYGB) or robotic (RRYGB; da Vinci ** system, Intuitive Surgical Sàrl) surgery between January 2016 and March 2019. The surgical techniques did not differ apart from different trocar placements. Data collected included patient characteristics before and after RYGB, operative outcomes and complications.
Results
In total, 114 RRYGB and 108 LRYGB primary surgeries were performed. There were no significant differences between the groups, apart from a significantly shorter duration of surgery (116.9 vs. 128.9 min, respectively), lower C-reactive protein values at days 1 (31.1 vs. 44.1 mg/l) and 2 (50.3 vs. 77.8 mg/l) after the intervention, and overall complication rate (4.4 vs. 12.0%, Clavien-Dindo classification II-V) with RRYGB compared with LRYGB. There was a lower hemoglobin value in the postoperative course after RRYGB (12.1 vs. 12.6 g/dl, day 2).
Conclusions
In our experience, robotic RYGB has proven to be safe and efficient, with a shorter duration of surgery and lower rate of complications than laparoscopic RYGB. RRYGB is easier to learn and seems safer in less experienced centers. Increasing experience with the robotic system can reduce the duration of surgery over time. Further studies with higher evidence level are necessary to confirm our results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal Roux-en-Y gastric bypass is the most frequently performed bariatric procedure in Europe [1, 2] and is a standard procedure in the surgical treatment of obesity, particularly in the presence of type 2 diabetes or gastroesophageal reflux disease [1, 3]. The laparoscopic technique [4] is well-established and clearly superior to the open procedure [5]. The operation is safe with low complication rates but technically challenging with a relatively flat learning curve of at least 100 [6] to 500 [7] procedures. In the expectation of overcoming the limitations of laparoscopy and shortening the learning curve [8], the surgical robot was implemented in bariatric surgery.
In 1998, a bariatric operation using a surgical robot was performed for the first time for the implantation of a gastric band [9]. The first robot-assisted Roux-en-Y gastric bypass (RRYGB) followed in 2001 [10]. Since then, various studies have shown that RRYGB is safe and efficient but requires longer operating times and higher costs than laparoscopic RYGB (LRYGB) [11, 12]. Other studies reported lower complication rates, a lower number of revision procedures, and a steeper learning curve with RRYGB [8, 13,14,15,16,17], although some studies reported higher complication rates [18,19,20]. Meta-analyses have confirmed the lower incidence of complications, longer surgery times, and higher costs associated with RRYGB but criticized the relatively low quality of the existing studies and the lack of large randomized controlled trials [21, 22]. US registry data indicate the increasing prevalence of RRYGB, which comprised 5.8% (n = 2282) of all RYGB procedures in 2016 (versus 39,425 LRYGB procedures), with comparable complication rates but longer surgery time (138 min) versus LRYGB (108 min) [23]. Despite the increase, it remains controversial whether the use of the robot in bariatric surgery is justified.
We present the largest German series of RRYGB procedures using the da Vinci **, trocars, and instruments of €2000 [35]. With our current reduction in operative times with RRYGB and the corresponding deduction of a minimum of 30 min × €15/min, we assume additional costs of approx. €1500 per RRYGB case. It remains questionable whether these costs are economically profitable by avoiding complications, which has been postulated [14]. It also remains questionable whether advertising effects will recoup the economic costs, which has also been suggested [16]. To reduce costs effectively, an interdisciplinary setting with the highest possible utilization of the system is required, to minimize the high maintenance costs [36].
A possible weakness of the present paper lies in the selection type and in the temporal divergence of the two groups. While laparoscopic procedures were mainly performed between 2016 and 2017, most of the robotic operations took place around 2018. The cohorts are largely comparable. The differences observed in EOSS tended to favor the LRYGB group. The operations were performed by various surgeons, all of whom already had bariatric experience. At the beginning of the study, most of the bariatric surgeons involved were still within the learning curve of an LRYGB as a possible explanation for increased complication rates and operative times. Thus, the conclusions of this paper are valid for bariatric surgeons with limited laparoscopic RYGB experience. The experience with the da Vinci system was limited to bariatric procedures with the Si system before da Vinci ** was introduced. The entire learning curve with the ** System can be found in the robotic group. While the latter would benefit the laparoscopic cohort, the overall experience with the procedure gained in laparoscopic RYGB would favor the robotic cohort. The strength of the study lies in the comparable surgical techniques using linear stapler anastomoses. The study provides a detailed picture with a complete 30-day follow-up rate.
Conclusion
In our experience, robotic RYGB has proven to be safe and efficient. In case of still limited expertise with laparoscopic RYGB procedures, using a robotic system may result in lower complication rates and shorter operative times than laparoscopic RYGB. Whether the benefits outweigh the additional costs required for RRYGB remains to be evaluated. Further studies with higher evidence level are necessary to confirm our results.
References
Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey 2016: primary, Endoluminal, and Revisional procedures. Obes Surg. 2018;28:3783–94.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO global registry report 2018. Obes Surg. 2018;29(3):782–95.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724.
Wittgrove AC, Clark GWTL. Laparoscopic gastric bypass, Roux-en-Y: Preliminary report of five cases. Obes Surg. 1994 Nov;4(4):353–7.
Banka G, Woodard G, Hernandez-Boussard T, et al. Laparoscopic vs open gastric bypass surgery: differences in patient demographics, safety, and outcomes. Arch Surg. 2012;147:550–6.
Schauer P, Ikramuddin S, Hamad G, et al. The learning curve for laparoscopic Roux-en-Y gastric bypass is 100 cases. Surg Endosc. 2003;17:212–5.
Doumouras AG, Saleh F, Anvari S, et al. Mastery in bariatric surgery: the long-term surgeon learning curve of roux-en-Y gastric bypass. Ann Surg. 2018;267:489–94.
Sanchez BR, Mohr CJ, Morton JM, et al. Comparison of totally robotic laparoscopic roux-en-Y gastric bypass and traditional laparoscopic roux-en-Y gastric bypass. Surg Obes Relat Dis. 2005;1(6):549–54.
Cadiere GB, Himpens J, Vertruyen M, et al. The World’s first obesity surgery performed by a surgeon at a distance. Obes Surg. 1999;9:206–9.
Horgan S, Vanuno D. Robots in laparoscopic surgery. J Laparoendosc Adv Surg Tech. 2001;11:415–9.
Ahmad A, Carleton JD, Ahmad ZF, et al. Laparoscopic versus robotic-assisted roux-en-Y gastric bypass: a retrospective, single-center study of early perioperative outcomes at a community hospital. Surg Endosc. 2016;30:3792–6.
Scozzari G, Rebecchi F, Millo P, et al. Robot-assisted gastrojejunal anastomosis does not improve the results of the laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2011;25:597–603.
Buchs NC, Morel P, Azagury DE, et al. Laparoscopic versus robotic Roux-en-Y gastric bypass: lessons and long-term follow-up learned from a large prospective monocentric study. Obes Surg. 2014;24:2031–9.
Hagen ME, Pugin F, Chassot G, et al. Reducing cost of surgery by avoiding complications: the model of robotic Roux-en-Y gastric bypass. Obes Surg. 2012;22:52–61.
Stefanidis D, Bailey SB, Kuwada T, et al. Robotic gastric bypass may lead to fewer complications compared with laparoscopy. Surg Endosc. 2018;32:610–6.
Senellart P, Saint-Jalmes G, Mfam W-S, et al. Laparoscopic versus full robotic roux-en-Y gastric bypass: retrospective, single-center study of the feasibility and short-term results. J Robot Surg. 2019;
Cahais J, Lupinacci RM, Oberlin O, et al. Less morbidity with robot-assisted gastric bypass surgery than with laparoscopic surgery? Obes Surg. 2019;29:519–25.
Benizri EI, Renaud M, Reibel N, et al. Perioperative outcomes after totally robotic gastric bypass: a prospective nonrandomized controlled study. Am J Surg. 2013;206:145–51.
Moon RC, Gutierrez JC, Royall NA, et al. Robotic Roux-en-Y gastric bypass, is it safer than laparoscopic bypass? Obes Surg. 2016;26:1016–20.
Celio AC, Kasten KR, Schwoerer A, et al. Perioperative safety of laparoscopic versus robotic gastric bypass: a propensity matched analysis of early experience. Surg Obes Relat Dis. 2017;13:1847–52.
Economopoulos KP, Theocharidis V, McKenzie TJ, et al. Robotic vs. laparoscopic Roux-en-Y gastric bypass: a systematic review and meta-analysis. Obes Surg. 2015;25:2180–9.
Li K, Zou J, Tang J, et al. Robotic versus laparoscopic bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2016;26:3031–44.
Lundberg PW, Wolfe S, Seaone J, et al. Robotic gastric bypass is getting better: first results from the metabolic and bariatric surgery accreditation and quality improvement program. Surg Obes Relat Dis. 2018;14:1240–5.
Beckmann JH, Aselmann H, Egberts JH, et al. Roboterassistierter vs. laparoskopischer Magenbypass. Der Chir. 2018;89:612–20.
Beckmann JH, Kersebaum J, von Schönfels W, Becker T, Schafmayer C, Egberts JH, et al. Use of barbed sutures in robotic bariatric bypass surgery: a single-center case series. BMC Surg. BMC Surg; 2019;19:97.
Sharma AM, Kushner RF. A proposed clinical staging system for obesity. Int J Obes. 2009;33:289–95.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications. Ann Surg. 2004;240:205–13.
Sebastian R, Howell MH, Chang K-H, et al. Robot-assisted versus laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a propensity score-matched comparative analysis using the 2015–2016 MBSAQIP database. Surg Endosc. 2018;33(5):1600–12.
Sharma G, Strong AT, Tu C, et al. Robotic platform for gastric bypass is associated with more resource utilization: an analysis of MBSAQIP dataset. Surg Obes Relat Dis. 2018;14:304–10.
Papasavas P, Seip RL, Stone A, et al. Robot-assisted sleeve gastrectomy and roux-en-y gastric bypass: results from the metabolic and bariatric surgery accreditation and quality improvement program data registry. Surg Obes Relat Dis. 2019;15:1281–90.
Giordano S, Salminen P, Biancari F, et al. Linear stapler technique may be safer than circular in gastrojejunal anastomosis for laparoscopic Roux-en-Y gastric bypass: a meta-analysis of comparative studies. Obes Surg. 2011;21:1958–64.
Abellán I, López V, Lujan J, et al. Stapling versus hand suture for gastroenteric anastomosis in Roux-en-Y gastric bypass: a randomized clinical trial. Obes Surg. 2015;25:1796–801.
Rogula T, Koprivanac M, Janik M, et al. Does robotic Roux-en-Y gastric bypass provide outcome advantages over standard laparoscopic approaches? Obes Surg. 2018;28:2589–96.
Gutierrez M, Ditto R, Roy S. Systematic review of operative outcomes of robotic surgical procedures performed with endoscopic linear staplers or robotic staplers. J Robot Surg. 2019;13:9–21.
Beckmann JH, Becker T, Schafmayer C. Roboter-assistierte bariatrische Chirurgie in Deutschland. CHAZ. 2019;20:294–8.
Egberts J-HH, Beham A, Ghadimi M. Aufbau eines Roboterprogramms. Zentralblatt fur Chir - Zeitschrift fur Allg Visz und Gefasschirurgie. 2016;141:143–4.
Acknowledgments
The manuscript was edited by Deborah Nock (Medical WriteAway, Norwich, UK).
Funding
Open Access funding provided by Projekt DEAL. The robotic procedures were performed on the da Vinci® ** Surgical System, provided by Intuitive Surgical Sàrl for the purpose of clinical research to the Department of General, Visceral, Thoracic, Transplantation, and Pediatric Surgery, Kurt-Semm Center for Laparoscopic and Robotic Assisted Surgery, University Hospital Schleswig Holstein, Campus Kiel. The services of the medical writer were funded by Intuitive Surgical Sàrl. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
JHB, WvS, and CS are active as speakers for Johnson & Johnson Medical. JHB, TT, CS, JHE, and TB received grants for training with the da Vinci ** Surgical System through Intuitive Surgical Sàrl. JHB and JHE work as proctors for Intuitive Surgical Sàrl. TB received the da Vinci® ** Surgical System from Intuitive Surgical Sàrl for the purpose of clinical research. CS has a consulting contract with B. Braun, Melsungen AG. AB, JNK, ASM, and ML state that there is no conflict of interest. We declare that we have no further competing interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed written consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(PDF 494 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beckmann, J.H., Bernsmeier, A., Kersebaum, JN. et al. The Impact of Robotics in Learning Roux-en-Y Gastric Bypass: a Retrospective Analysis of 214 Laparoscopic and Robotic Procedures. OBES SURG 30, 2403–2410 (2020). https://doi.org/10.1007/s11695-020-04508-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04508-1