Abstract
Background
Communication of the benefits and harms of blood pressure lowering strategy is crucial for shared decision-making.
Objectives
To quantify the effect of intensive versus standard systolic blood pressure lowering in terms of the number of event-free days
Design
Post hoc analysis of the Systolic Blood Pressure Intervention Trial
Participants
A total of 9361 adults 50 years or older without diabetes or stroke who had a systolic blood pressure of 130–180 mmHg and elevated cardiovascular risk
Interventions
Intensive (systolic blood pressure goal <120 mmHg) versus standard blood pressure lowering (<140 mmHg)
Main Measures
Days free of major adverse cardiovascular events (MACE), serious adverse events (SAE), and monitored adverse events (hypotension, syncope, bradycardia, electrolyte abnormalities, injurious falls, or acute kidney injury) over a median follow-up of 3.33 years
Key Results
The intensive treatment group gained 14.7 more MACE-free days over 4 years (difference, 14.7 [95% confidence interval: 5.1, 24.4] days) than the standard treatment group. The benefit of the intensive treatment varied by cognitive function (normal: difference, 40.7 [13.0, 68.4] days; moderate-to-severe impairment: difference, −15.0 [−56.5, 26.4] days; p-for-interaction=0.009) and self-rated health (excellent: difference, −22.7 [−51.5, 6.1] days; poor: difference, 156.1 [31.1, 281.2] days; p-for-interaction=0.001). The mean overall SAE-free days were not significantly different between the treatments (difference, −14.8 [−35.3, 5.7] days). However, the intensive treatment group had 28.5 fewer monitored adverse event–free days than the standard treatment group (difference, −28.5 [−40.3, −16.7] days), with significant variations by frailty status (non-frail: difference, 38.8 [8.4, 69.2] days; frail: difference, −15.5 [−46.6, 15.7] days) and self-rated health (excellent: difference, −12.9 [−45.5, 19.7] days; poor: difference, 180.6 [72.9, 288.4] days; p-for-interaction <0.001).
Conclusions
Over 4 years, intensive systolic blood pressure lowering provides, on average, 14.7 more MACE-free days than standard treatment, without any difference in SAE-free days. Whether this time-based effect summary improves shared decision-making remains to be elucidated.
Trial Registration
ClinicalTrials.gov Registration: NCT01206062
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The final report of Systolic Blood Pressure Intervention Trial (SPRINT) showed that an intensive systolic blood pressure lowering decreased the rate of major adverse cardiovascular events (MACE) and all-cause mortality compared with a standard treatment by 27% over a median follow-up of 3.33 years in non-diabetic patients at elevated risk for cardiovascular disease (CVD).1 Conventional effect measures that are familiar to trialists and researchers, such as hazard ratios (HR) and the number needed to treat (NNT), may not be intuitive to clinicians and patients.2, 3 Relative measures tend to exaggerate the effect size,4 thereby influencing treatment decisions.2
Recently, restricted mean survival time (RMST) was proposed as an alternative effect measure for clinical studies.5,6,7,8,9,10,11,12 The RMST is an average event-free time up to a pre-specified time point and, heuristically, it is the area under the Kaplan-Meier survival curve up to that point. Although RMST shares the same limitations as HR and NNT that it provides population average treatment effect for the study duration, it is an absolute measure, thus contains more information than relative measures like HR. It also gives an intuitive way to communicate treatment effect as a gain or loss in event-free time.13,14,15,16 While there is no definitive evidence on how an RMST-based summary influences treatment decisions compared to the conventional effect measures, a recent survey suggests that RMST information might reduce decisional conflict and influence treatment choice in older adults with limited life expectancies.17
The RMST analysis has been applied to publicly available SPRINT data to quantify the benefits and harms of intensive blood pressure lowering.18, 19 The current analysis expands the previous reports by applying RMST methods to the final SPRINT data and identifying baseline prognostic factors that moderate the effect of the intensive treatment to find subgroups that were more likely to benefit and least likely to harm from the intensive treatment.
METHODS
Study Design, Population, and Interventions
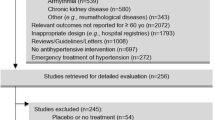
The design, conduct, and main results of SPRINT have been reported previously (ClinicalTrials.gov Registration: NCT01206062).1, 20,21,22 The SPRINT protocol was approved by the institutional review board at each participating site and all participants provided written informed consent. This post hoc analysis was approved by Advarra/Hebrew SeniorLife institutional review board. Briefly, participants were 9361 adults 50 years or older who had a systolic blood pressure of 130 to 180 mmHg and elevated cardiovascular risk, defined as one or more of the following risk factors: history of clinical or subclinical CVD other than stroke, estimated glomerular filtration rate of 20–59 mL/min/1.73 m2 using the 4-variable Modification of Diet in Renal Disease equation,23 10-year CVD risk ≥ 15% calculated using the Framingham Risk Score, or age ≥ 75 years. Individuals with diabetes or prior stroke were excluded. Eligible participants were randomized to an intensive systolic blood pressure lowering treatment (goal <120 mmHg) or standard treatment (goal <140 mmHg) (see CONSORT diagram in Supplementary Figure 1). After a recommendation by the trial’s Data and Safety Monitoring Board, the SPRINT intervention was stopped on August 20, 2015, by the trial sponsor (National Heart, Lung, and Blood Institute), based on significantly reduced rates of CVD events and death in the intensive treatment group after a median follow-up of 3.33 years.
Measurements
Demographic characteristics, medical history, and laboratory tests were collected at baseline. Chronic kidney disease (CKD) was defined as estimated glomerular filtration rate <60 mL/min/1.73 m2. A comorbidity burden was measured as a count of 30 medical and 6 mental conditions.24 Montreal Cognitive Assessment (MoCA) (range: 0–30 points; higher scores indicate better cognitive function) was performed. Participants were classified into normal, mild impairment, or moderate-to-severe impairment according to the race/ethnicity and educational level (Supplementary Table 1).25 A 36-item deficit-accumulation frailty index (range: 0–1; higher scores indicate greater frailty) was calculated as a proportion of abnormalities from baseline assessment of health status, comorbidities, physical function, cognitive function, and laboratory tests.26 Participants were classified into non-frail (frailty index ≤ 0.10), pre-frail (>0.10 to ≤ 0.21), or frail (>0.21) as previously defined.22 Self-reported general health was collected as excellent, very good, good, fair, and poor.
Efficacy and Safety Outcomes
The efficacy outcome was a composite MACE that consisted of myocardial infarction, acute coronary syndrome, stroke, acute decompensated heart failure, or cardiovascular death. These events were adjudicated by a committee blinded to treatment assignment. The safety outcome was composite serious adverse events (SAE), which were defined as events that were fatal or life-threatening, resulted in clinically significant or persistent disability, required a prolonged hospitalization, or were judged by the investigators as clinically significant harms that might require medical or surgical intervention. We also assessed monitored adverse events of interest (hypotension, syncope, bradycardia, electrolyte abnormalities, injurious falls, or acute kidney injury). Definitions of individual events are provided in Supplementary Table 2.
Statistical Analysis
The analysis was conducted according to the intention-to-treat principle. We estimated 4-year RMST difference (days) and 95% confidence interval (CI) between the intensive and standard treatments for the composite MACE, composite SAE, and monitored adverse events that occurred up to August 20, 2015. Because these events were likely to have different severities, we interpreted with a caveat that a difference in MACE-free days might not be clinically comparable to the same difference in SAE-free or monitored adverse event–free days. To identify baseline characteristics that were associated with a greater RMST difference (i.e., greater benefit or safety of the intensive treatment over the standard treatment), we examined treatment interaction by pre-specified subgroups defined by age (≥ 75 years versus <75 years), sex, race (Black versus non-Black), history of CVD, and CKD. We also considered treatment interactions by frailty status, cognitive function, and self-rated general health, which were not pre-specified subgroups in SPRINT. For each of these grou**s and for each outcome, we first used RMST regression to model RMST as a function of treatment group, the given pre-specified and exploratory baseline characteristics, and the corresponding 2-way interactions. Based on these results, only the interaction terms that were statistically significant at a 5% level were retained for the respective multivariable regression model. The variables that were retained in the final model for MACE are treatment, age, gender, race, CVD history, CKD, frailty status, cognitive function, self-rated general health, interaction between treatment and cognitive function, and interaction between treatment and self-rated general health. The variables that were retained in the final model for SAE are treatment, age, gender, race, CVD history, CKD, frailty status, cognitive function, and self-rated general health. No interaction terms were included, as none was statistically significant in 2-way analyses with treatment. The model for monitored adverse events included the same main effect terms, as well as interaction between treatment and frailty and between treatment and self-rated general health. As a comparison to RMST analysis, we also fit Cox proportional hazards regression to analyze the composite MACE, composite SAE, and monitored adverse events. Analyses were performed using SAS software (version 9.4; SAS Institute Inc.) and a 2-sided p value <0.05 was considered statistically significant.
RESULTS
Characteristics of Study Population
The study population included individuals with a mean (standard deviation [SD]) age of 67.9 (9.4) years, 35.6% women, and 68.5% non-Black race (Table 1). Clinical CVD was prevalent in 20.1% and CKD in 28.3%. Most participants reported excellent (8.0%), very good (34.6%), or good (42.7%) general health, while 14.3% reported fair or poor health. The mean (SD) frailty index was 0.18 (0.08), with 30.5% with a frailty index >0.21. The mean (SD) MoCA score was 22.8 (4.3) points and 10.0% showed moderate-to-severe cognitive impairment.
RMST Analysis Versus Cox Proportional Hazards Regression Analysis
Over 4 years, the intensive treatment group had, on average, 14.7 (95% CI: 5.1, 24.4) additional MACE-free days than the standard treatment group (Fig. 1A). The HR (95% CI) was 0.74 (0.63, 0.87), which indicates a 26% reduction in the hazard rate of MACE with the intensive treatment. The SAE-free days did not differ significantly between the treatment groups (−14.8 [95% CI: −35.3, 5.7] days without SAE) (Fig. 1B). The corresponding HR (95% CI) for SAE was 1.03 (0.97, 1.11). However, those treated with the intensive strategy for 4 years had, on average, 28.5 (95% CI: 16.7, 40.3) more days with the monitored adverse events than those treated with the standard strategy (Fig. 1C). The HR (95% CI) for the monitored adverse events was 1.32 (1.16, 1.51), indicating a 32% increase with the intensive treatment.
Baseline Characteristics Associated with Cardiovascular Event–Free Time
The difference in the 4-year mean MACE-free time between the treatment groups varied by baseline cognitive function (normal: 19.9 [95% CI, 7.3, 32.6] days; mild impairment: 21.8 [6.2, 37.4] days; moderate-to-severe impairment: −38.8 [−74.5, −3.2] days; p-for-interaction=0.007) and by self-reported general health (excellent: −5.7 [−34.2, 22.8] days; very good: 10.3 [−4.8, 25.3] days; good: 31.8 [16.5, 47.0] days; fair: −27.6 [−57.7, 2.5] days; poor: 165.3 [38.9, 291.7] days; p-for-interaction <0.001) (Supplementary Table 3). There was little variation by age, sex, race, clinical CVD, CKD, or frailty status. The HRs for the intensive versus standard treatments were generally consistent with RMST results, except that the benefit of the intensive treatment attenuated with increasing frailty on the HR scale (HR [95% CI]: for non-frail, 0.37 [0.19, 0.72]; pre-frail, 0.66 [0.52, 0.85]; and frail, 0.87 [0.70, 1.08]; p-for-interaction=0.010), whereas RMST difference did not vary significantly by frailty status (non-frail: 20.4 [7.3, 33.6]; pre-frail: 15.5 [3.2, 27.9]; frail: 11.4 [−10.9, 33.7]; p-for-interaction=0.76).
A multivariable regression confirmed that RMST difference between the treatment groups varies by cognitive function and self-reported general health (Table 2). The intensive treatment provides greater MACE-free days for those with normal or mild cognitive impairment than those with moderate-to-severe impairment and for those who rated their health status poor than those who rated their health otherwise.
Baseline Characteristics Associated with Adverse Event–Free Time
There was no statistically significant variation in the difference in the 4-year mean SAE-free time or HRs by baseline characteristics (Supplementary Table 4). None of the interaction terms was statistically significant in a multivariable regression. However, the 4-year mean monitored adverse event–free time varied significantly by frailty status (non-frail: −5.4 [95% CI, −23.5, 12.7] days; pre-frail: −19.6 [−35.2, −3.9] days; frail: −56.7 [−82.3, −31.1] days; p-for-interaction=0.006) and by self-reported general health (excellent: 3.0 [−28.4, 34.3] days; very good: −15.8 [−34.3, 2.8] days; good: −49.1 [−67.6, −30.6] days; fair: −28.1 [−66.5, 10.4] days; poor: 143.4 [40.5, 246.3] days; p-for-interaction <0.001) (Supplementary Table 5). There was little variation by age, sex, race, clinical CVD, CKD, or cognitive function. The HRs for the intensive versus standard treatments showed a statistically significant interaction by self-rated general health (HR [95% CI] for excellent: 0.83 [0.47, 1.45]; very good: 1.26 [0.99, 1.59]; good: 1.63 [1.33, 2.01]; fair: 1.13 [0.84, 1.52]; poor: 0.20 [0.05, 0.91]; p-for-interaction=0.007), but not by frailty status (non-frail: 1.18 [0.74, 1.88]; pre-frail: 1.25 [1.03, 1.52]; frail: 1.42 [1.17, 1.73]; p-for-interaction=0.59).
Frailty and self-reported general health had statistically significant interactions with the treatment in a multivariable model (Table 3). The intensive treatment seemed to provide greater monitored adverse event–free days than the standard treatment for non-frail participants than frail participants and for those with poor self-rated health than those who rated their health otherwise.
DISCUSSION
In this post hoc analysis of SPRINT, we found that an intensive systolic blood pressure lowering adds an average of 14.7 days free of MACE compared with a standard treatment over 4 years. The mean SAE-free time was similar between the treatment groups, but the mean monitored event–free time was 28.5 days shorter in the intensive treatment group. Because the monitored adverse events are not comparable in severity with MACE and often reversible,27 these results do not undermine the benefit of the intensive treatment. Moreover, the intensive treatment seems to be more beneficial (i.e., more MACE-free days) among participants with no or mild cognitive impairment and among those with poor self-rated health.
For older adults, the 2017 American College of Cardiology/American Heart Association blood pressure guideline recommends shared decision-making.28 The guideline mainly discusses the effects of intensive blood pressure lowering in terms of relative risk reduction.28 A ratio measure can exaggerate the treatment effect when the absolute risk is low.2 It does not effectively quantify the magnitude of the benefits and harms that can be achieved in a specific time window, which may be relevant to older adults who need to consider treatment burden and their remaining life expectancy.29 The NNT at a specific point in time is often used, but it ignores cumulative incidence profiles up to that time point. This measure may be difficult for lay persons to understand.2
Our analysis illustrates that RMST provides a time-based summary of treatment effect that complements (rather than replaces) the conventional effect measures. However, there are important caveats in interpreting our RMST results. The RMST difference is affected by the event rates of the population, the treatment effect, and the choice of time window. The RMST analysis shares the same limitations as HR and NNT that it is a valid measure of treatment effect for the study duration. Because it represents group averages, it does not tell us about the heterogeneity of treatment effect among individuals with different characteristics or with variable adherence. The 14.7-day gain in MACE-free days over 4 years in our study may seem modest. Nonetheless, this magnitude of benefit is consistent with well-accepted interventions over a similar time frame in patients with elevated CVD risk, such as empagliflozin (17 days),10 liraglutide (19 days),10 pravastatin (19 days),12 and sacubitril/valsartan (24 days).15 Our results should not undermine potential long-term benefit (a modeling study suggests that up to 3 years of life can be gained30) or prevention of cognitive impairment and dementia.31
Moreover, there is no definitive evidence that an RMST-based summary improves treatment decision-making. In an online panel survey of 200 older adults with hypertension, there was no overall difference in decisional conflict scale and the choice of the blood pressure lowering strategy between the groups presented with RMST-based versus conventional effect summary information.17 However, among those with limited life expectancy, the RMST group tended to report lower decisional conflict (conventional versus RMST-based: 31.6 versus 26.1 in a 100-point scale [high scores indicate high conflict]) and lower preference for the intensive treatment (conventional versus RMST-based: 20% versus 5%). Although these differences were not statistically significant, RMST information might influence treatment choice in certain groups of older adults. This warrants further investigation.
Our study expands previous RMST analysis of SPRINT data18, 19 by analyzing the final adjudicated event data1 and identifying subgroups defined by cognitive function, self-rated general health, and frailty that were more likely to benefit or to be harmed from the intensive strategy. The lack of benefit of an intensive treatment for individuals with cognitive impairment has been reported in a recent analysis restricted to the SPRINT participants 80 years or older32 and a post hoc analysis of the Action to Control Cardiovascular Risk in Diabetes Blood Pressure trial.33 We found that the intensive treatment made little difference in MACE-free, SAE-free, and monitored event–free days for individuals who rated their health excellent, whereas the intensive treatment resulted in an immediate and larger gain in MACE-free and monitored event–free days for those with poor self-rated general health. Given the subjective nature of self-rated general health, lack of a clear pattern in the effect estimates with self-rated health, and a small number of participants with poor self-rated health (n=100), the reasons for and clinical importance of the observed variation in treatment effect remain unclear. A previous analysis of SPRINT showed that the occurrence of MACE and SAE is highly correlated.34 We speculate that the benefit of the intensive treatment might take longer to emerge in those with excellent health than in those with poor health and at high risk for MACE and SAE. A longer follow-up study may be needed to examine the effect of the intensive treatment in people in excellent health. Our subgroup findings on self-rated health should be confirmed in future research.
Another noteworthy finding is that the effect of the intensive treatment on MACE-free days seems consistent across frailty status. Post hoc analyses of the SPRINT participants 75 years or older22 and the Hypertension in the Very Elderly Trial35 have shown similar HRs across frailty status. Although the intensive strategy was associated with more days with the monitored adverse events than standard strategy for those with frailty, these events are known side effects of blood pressure lowering that can be managed with medication adjustment or a brief hospitalization. It is reassuring that the mean SAE-free days were similar between the treatment strategies across frailty status. In addition, considering that the SPRINT participants were ambulatory community-dwelling older adults, frail participants were probably at the milder end of the frailty spectrum.36 Therefore, the results may not generalize to older adults who are non-ambulatory or residing in a nursing facility.
Our results should be interpreted within the limitations of a post hoc analysis. First, although the baseline characteristics selected for the interaction analysis were pre-specified in SPRINT, we considered additional variables, such as frailty status, cognitive function, and self-reported general health, which were not pre-specified. Second, the time window for RMST estimation should be pre-specified at the design stage such that a clinically meaningful treatment effect can be observed. We chose 4 years based on a post hoc examination of event times (few events beyond 4 years) and the largest follow-up time in the dataset. A simulation study showed that an empirical choice of the time window like our approach can provide valid inference.37 Last, while MACE, SAE, and monitored adverse events are undesirable events of clinical interest, days gained or lost due to different events are not comparable. These trade-offs should be interpreted with consideration of patients’ perceptions and preferences about different events.
CONCLUSIONS
In middle-aged and older adults with hypertension and elevated CVD risk, the beneficial effect of the intensive blood pressure lowering over the standard treatment can be translated to an average gain of 14.7 days free of MACE over 4 years. Although the overall SAE-free days were similar between the treatment groups, the intensive strategy was associated with 28.5 additional days lost due to monitored adverse events. Whether an RMST-based summary can improve shared decision-making about blood pressure–lowering treatments remains to be elucidated.
References
Group SR, Lewis CE, Fine LJ, et al. Final Report of a Trial of Intensive Versus Standard Blood-Pressure Control. N Engl J Med. 2021;384(20):1921-1930. https://doi.org/10.1056/NEJMoa1901281
Zipkin DA, Umscheid CA, Keating NL, et al. Evidence-Based Risk Communication: a Systematic Review. Ann Intern Med. 2014;161(4):270-280. https://doi.org/10.7326/M14-0295
Hernan MA. The Hazards of Hazard Ratios. Epidemiology. 2010;21(1):13-15. https://doi.org/10.1097/EDE.0b013e3181c1ea43
Trinquart L, Jacot J, Conner SC, Porcher R. Comparison of Treatment Effects Measured by the Hazard Ratio and by the Ratio of Restricted Mean Survival Times in Oncology Randomized Controlled Trials. J Clin Oncol. 2016;34(15):1813-1819. https://doi.org/10.1200/JCO.2015.64.2488
Royston P, Parmar MK. The Use of Restricted Mean Survival Time to Estimate the Treatment Effect in Randomized Clinical Trials When the Proportional Hazards Assumption Is in Doubt. Stat Med. 2011;30(19):2409-2421. https://doi.org/10.1002/sim.4274
Royston P, Parmar MK. Restricted Mean Survival Time: an Alternative to the Hazard Ratio for the Design and Analysis of Randomized Trials with a Time-to-Event Outcome. BMC Med Res Methodol. 2013;13:152. https://doi.org/10.1186/1471-2288-13-152
Uno H, Claggett B, Tian L, et al. Moving Beyond the Hazard Ratio in Quantifying the Between-Group Difference in Survival Analysis. J Clin Oncol. 2014;32(22):2380-2385. https://doi.org/10.1200/JCO.2014.55.2208
Uno H, Wittes J, Fu H, et al. Alternatives to Hazard Ratios for Comparing the Efficacy or Safety of Therapies in Noninferiority Studies. Ann Intern Med. 2015;163(2):127-134. https://doi.org/10.7326/M14-1741
Tian L, Zhao L, Wei LJ. Predicting the Restricted Mean Event Time with the Subject’s Baseline Covariates in Survival Analysis. Biostatistics. 2014;15(2):222-233. https://doi.org/10.1093/biostatistics/kxt050
Kloecker DE, Davies MJ, Khunti K, Zaccardi F. Uses and Limitations of the Restricted Mean Survival Time: Illustrative Examples From Cardiovascular Outcomes and Mortality Trials in Type 2 Diabetes. Ann Intern Med. 2020. https://doi.org/10.7326/M19-3286
Guimaraes HP, Lopes RD, de Barros ESPGM, et al. Rivaroxaban in Patients with Atrial Fibrillation and a Bioprosthetic Mitral Valve. N Engl J Med. 2020;383(22):2117-2126. https://doi.org/10.1056/NEJMoa2029603
Orkaby AR, Rich MW, Sun R, Lux E, Wei LJ, Kim DH. Pravastatin for Primary Prevention in Older Adults: Restricted Mean Survival Time Analysis. J Am Geriatr Soc. 2018;66(10):1987-1991. https://doi.org/10.1111/jgs.15509
Kim DH, Uno H, Wei LJ. Restricted Mean Survival Time as a Measure to Interpret Clinical Trial Results. JAMA Cardiol. 2017;2(11):1179-1180. https://doi.org/10.1001/jamacardio.2017.2922
McCaw ZR, Orkaby AR, Wei LJ, Kim DH, Rich MW. Applying Evidence-Based Medicine to Shared Decision Making: Value of Restricted Mean Survival Time. Am J Med. 2019;132(1):13-15. https://doi.org/10.1016/j.amjmed.2018.07.026
Perego C, Sbolli M, Specchia C, et al. Utility of Restricted Mean Survival Time Analysis for Heart Failure Clinical Trial Evaluation and Interpretation. JACC Heart Fail. 2020;8(12):973-983. https://doi.org/10.1016/j.jchf.2020.07.005
Leifer ES, Mentz RJ. Patient-Centered Measures of Treatment Benefit. JACC Heart Fail. 2020;8(12):996-998. https://doi.org/10.1016/j.jchf.2020.09.003
Kim DH, Shi SM, Carroll D, Najafzadeh M, Wei LJ. Restricted Mean Survival Time Versus Conventional Measures for Treatment Decision-making. J Am Geriatr Soc. 2021. https://doi.org/10.1111/jgs.17195
Krishnaswami A, Peterson ED, Kim DH, Goyal P, Rich MW. Efficacy and Safety of Intensive Blood Pressure Therapy Using Restricted Mean Survival Time-Insights from the SPRINT Trial. Am J Med. 2020. https://doi.org/10.1016/j.amjmed.2019.12.050
Stensrud MJ, Aalen JM, Aalen OO, Valberg M. Limitations of Hazard Ratios in Clinical Trials. Eur Heart J. 2019;40(17):1378-1383. https://doi.org/10.1093/eurheartj/ehy770
Ambrosius WT, Sink KM, Foy CG, et al. The Design and Rationale of a Multicenter Clinical Trial Comparing Two Strategies for Control of Systolic Blood Pressure: the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Trials. 2014;11(5):532-546. https://doi.org/10.1177/1740774514537404
SPRINT Research Group. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103-2116. https://doi.org/10.1056/NEJMoa1511939
Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs Standard Blood Pressure Control and Cardiovascular Disease Outcomes in Adults Aged >/=75 Years: A Randomized Clinical Trial. JAMA. 2016. https://doi.org/10.1001/jama.2016.7050
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A More Accurate Method to Estimate Glomerular Filtration Rate from Serum Creatinine: A New Prediction Equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461-470. https://doi.org/10.7326/0003-4819-130-6-199903160-00002
Selim AJ, Fincke G, Ren XS, et al. Comorbidity Assessments Based on Patient Report: Results from the Veterans Health Study. J Ambul Care Manage. 2004;27(3):281-295. https://doi.org/10.1097/00004479-200407000-00011
Milani SA, Marsiske M, Cottler LB, Chen X, Striley CW. Optimal Cutoffs for the Montreal Cognitive Assessment Vary by Race and Ethnicity. Alzheimers Dement (Amst). 2018;10:773-781. https://doi.org/10.1016/j.dadm.2018.09.003
Pajewski NM, Williamson JD, Applegate WB, et al. Characterizing Frailty Status in the Systolic Blood Pressure Intervention Trial. J Gerontol A Biol Sci Med Sci. 2016;71(5):649-655. https://doi.org/10.1093/gerona/glv228
Rocco MV, Sink KM, Lovato LC, et al. Effects of Intensive Blood Pressure Treatment on Acute Kidney Injury Events in the Systolic Blood Pressure Intervention Trial (SPRINT). Am J Kidney Dis. 2018;71(3):352-361. https://doi.org/10.1053/j.ajkd.2017.08.021
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. https://doi.org/10.1016/j.jacc.2017.11.006
Guiding Principles for the Care of Older Adults with Multimorbidity: an Approach for Clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc. 2012;60(10):E1-E25. https://doi.org/10.1111/j.1532-5415.2012.04188.x
Vaduganathan M, Claggett BL, Juraschek SP, Solomon SD. Assessment of Long-term Benefit of Intensive Blood Pressure Control on Residual Life Span: Secondary Analysis of the Systolic Blood Pressure Intervention Trial (SPRINT). JAMA Cardiol. 2020;5(5):576-581. https://doi.org/10.1001/jamacardio.2019.6192
Hughes D, Judge C, Murphy R, et al. Association of Blood Pressure Lowering With Incident Dementia or Cognitive Impairment: a Systematic Review and Meta-analysis. JAMA. 2020;323(19):1934-1944. https://doi.org/10.1001/jama.2020.4249
Pajewski NM, Berlowitz DR, Bress AP, et al. Intensive vs Standard Blood Pressure Control in Adults 80 Years or Older: a Secondary Analysis of the Systolic Blood Pressure Intervention Trial. J Am Geriatr Soc. 2020;68(3):496-504. https://doi.org/10.1111/jgs.16272
Shi S, Gouskova N, Najafzadeh M, Wei LJ, Kim DH. Intensive Versus Standard Blood Pressure Control in Type 2 Diabetes: a Restricted Mean Survival Time Analysis of a Randomised Controlled Trial. BMJ Open. 2021;11(9):e050335. https://doi.org/10.1136/bmjopen-2021-050335
Botchway A, Buhnerkempe MG, Prakash V, Al-Akchar M, Adekola B, Flack JM. Serious Adverse Events Cluster in Participants Experiencing the Primary Composite Cardiovascular Endpoint: a Post Hoc Analysis of the SPRINT Trial. Am J Hypertens. 2020;33(6):528-533. https://doi.org/10.1093/ajh/hpaa010
Warwick J, Falaschetti E, Rockwood K, et al. No Evidence that Frailty Modifies the Positive Impact of Antihypertensive Treatment in Very Elderly People: an Investigation of the Impact of Frailty Upon Treatment Effect in the HYpertension in the Very Elderly Trial (HYVET) Study, a Double-Blind, Placebo-Controlled Study of Antihypertensives in People with Hypertension Aged 80 and Over. BMC Med. 2015;13:78. https://doi.org/10.1186/s12916-015-0328-1
Kim DH. Intensive vs Standard Blood Pressure Control for Older Adults. JAMA. 2016;316(18):1921. https://doi.org/10.1001/jama.2016.14909
Tian L, ** H, Uno H, et al. On the Empirical Choice of the Time Window for Restricted Mean Survival Time. Biometrics. 2020. https://doi.org/10.1111/biom.13237
Acknowledgements
We thank the patients who participated in the Systolic Blood Pressure Intervention Trial (SPRINT) for their important contributions. For a full list of contributors to SPRINT, please visit www.sprinttrial.org.
Dr. Dae Hyun Kim affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained. Dr. Curtis Tatsuoka had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
The SPRINT is funded with federal funds from the National Institutes of Health (NIH), including the National Heart, Lung, and Blood Institute (NHLBI), the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the National Institute on Aging (NIA), and the National Institute of Neurological Disorders and Stroke (NINDS), under Contract Numbers HHSN268200900040C, HHSN268200900046C, HHSN268200900047C, HHSN268200900048C, and HHSN268200900049C, and Inter-Agency Agreement Number A-HL-13-002-001. It was supported in part with resources and use of facilities through the Department of Veterans Affairs. The SPRINT investigators acknowledge the contribution of study medications (azilsartan and azilsartan combined with chlorthalidone) from Takeda Pharmaceuticals International, Inc. We also acknowledge the support from the following Clinical and Translational Science Awards funded by the National Center for Advancing Translational Sciences (NCATS): CWRU: UL1TR000439, OSU: UL1RR025755, U Penn: UL1RR024134& UL1TR000003, Boston: UL1RR025771, Stanford: UL1TR000093, Tufts: UL1RR025752, UL1TR000073 & UL1TR001064, University of Illinois: UL1TR000050, University of Pittsburgh: UL1TR000005, UT Southwestern: 9U54TR000017-06, University of Utah: UL1TR000105-05, Vanderbilt University: UL1 TR000445, George Washington University: UL1TR000075, University of CA, Davis: UL1 TR000002, University of Florida: UL1 TR000064, University of Michigan: UL1TR000433, Tulane University: P30GM103337 COBRE Award NIGMS, Wake Forest University: UL1TR001420. This analysis was also supported by grant R21AG060227 from NIA. All components of the SPRINT study protocol were designed and implemented by the investigators. The investigative team collected, analyzed, and interpreted the data. All aspects of manuscript writing and revision were carried out by the coauthors. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, the US Department of Veterans Affairs, or the United States Government. For a full list of contributors to SPRINT, please see the supplementary acknowledgement list: https://www.sprinttrial.org/public/dspScience.cfm.
Author information
Authors and Affiliations
Contributions
Conception and design: D.H. Kim, M. Odden, L.J. Wei
Analysis and interpretation of the data: All authors
Drafting of the article: D.H. Kim
Critical revision of the article for important intellectual content: All authors
Final approval of the article: All authors
Provision of study materials or patients: J.T. Wright
Statistical expertise: C. Tatsuoka, Z. Chen, L.J. Wei
Obtaining of funding: D.H. Kim
Administrative, technical, or logistic support: D.H. Kim
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 187 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, D.H., Tatsuoka, C., Chen, Z. et al. Intensive Versus Standard Blood Pressure Lowering and Days Free of Cardiovascular Events and Serious Adverse Events: a Post Hoc Analysis of Systolic Blood Pressure Intervention Trial. J GEN INTERN MED 37, 3797–3804 (2022). https://doi.org/10.1007/s11606-022-07753-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07753-5