Abstract
Purpose
Although the concept of extrapancreatic extension (EPEx) was removed in the eighth edition of the American Joint Committee on Cancer pancreatic cancer staging system, several studies have supported the prognostic significance of EPEx. This study aimed to investigate the significance of EPEx in pancreatic ductal adenocarcinoma (PDAC) using the National Cancer Database (NCDB).
Methods
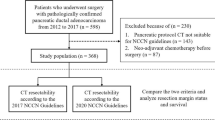
Data of patients who underwent resection for PDAC between 2006 and 2016 were extracted and analyzed from the NCDB. Cases arising from premalignant lesions, those with metastases, and those treated with neoadjuvant therapy were excluded.
Results
Among 37,634 patients, the median overall survival was 23 months and the 5-year survival rate was 22.7%. The EPEx prevalence was the lowest for T1 stage (63.2%) and increased with each T-stage (T2:83.4%, T3:85.8%). The overall survival was better in EPEx-negative patients than in EPEx-positive patients (median 33.7 vs. 21.5 months; p<0.001). When the T-stages were stratified by EPEx, EPEx-positive patients showed worse survival in all T-stages than EPEx-negative patients. Survival was comparable between T1 EPEx-positive and T2 or T3 EPEx-negative patients (p=0.088 and p=0.178, respectively). Furthermore, T2 and T3 EPEx-negative patients had similar survival to each other (p=0.877), and distinctly superior survival compared to T2 and T3 EPEx-positive patients (p<0.001).
Conclusions
EPEx was an important prognostic factor in the overall cohort and in differentiating between T stages. This study strongly suggests that staging systems should reinstate EPEx and apply it to all T-stages, especially in T1, where EPEx was absent in 36% of patients.




Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Shi S, Hua J, Liang C, Meng Q, Liang D, Xu J et al. Proposed Modification of the 8th Edition of the AJCC Staging System for Pancreatic Ductal Adenocarcinoma. Ann Surg. 2019;269(5):944-50.
Kwon W, He J, Higuchi R, Son D, Lee SY, Kim J et al. Multinational validation of the American Joint Committee on Cancer 8th edition pancreatic cancer staging system in a pancreas head cancer cohort. J Hepatobiliary Pancreat Sci. 2018;25(9):418-27.
van Roessel S, Kasumova GG, Verheij J, Najarian RM, Maggino L, de Pastena M et al. International Validation of the Eighth Edition of the American Joint Committee on Cancer (AJCC) TNM Staging System in Patients With Resected Pancreatic Cancer. JAMA Surg. 2018;153(12):e183617.
Saka B, Balci S, Basturk O, Bagci P, Postlewait LM, Maithel S et al. Pancreatic Ductal Adenocarcinoma is Spread to the Peripancreatic Soft Tissue in the Majority of Resected Cases, Rendering the AJCC T-Stage Protocol (7th Edition) Inapplicable and Insignificant: A Size-Based Staging System (pT1: ≤2, pT2: >2-≤4, pT3: >4 cm) is More Valid and Clinically Relevant. Ann Surg Oncol. 2016;23(6):2010-8.
Kwon W, Park T, He J, Higuchi R, Son D, Lee SY et al. Is the New T1 Category as Defined in the Eighth Edition of the AJCC Pancreatic Cancer Staging System an Improvement? J Gastrointest Surg. 2020;24(2):262-9.
Öztürk SK, Erden E. Do the Well Known Prognostic Parameters in Pancreatic Ductal Adenocarcinoma Really Reflect Survival? Turk Patoloji Derg. 2018;34(2):127-33.
Jamieson NB, Foulis AK, Oien KA, Dickson EJ, Imrie CW, Carter R et al. Peripancreatic fat invasion is an independent predictor of poor outcome following pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. J Gastrointest Surg. 2011;15(3):512-24.
Mitsunaga S, Hasebe T, Kinoshita T, Konishi M, Takahashi S, Gotohda N et al. Detail histologic analysis of nerve plexus invasion in invasive ductal carcinoma of the pancreas and its prognostic impact. Am J Surg Pathol. 2007;31(11):1636-44.
Patel BN, Giacomini C, Jeffrey RB, Willmann JK, Olcott E. Three-dimensional volume-rendered multidetector CT imaging of the posterior inferior pancreaticoduodenal artery: its anatomy and role in diagnosing extrapancreatic perineural invasion. Cancer Imaging. 2013;13(4):580-90.
Patel BN, Olcott E, Jeffrey RB. Extrapancreatic perineural invasion in pancreatic adenocarcinoma. Abdominal Radiology. 2018;43(2):323-31.
Müller PC, Frey MC, Ruzza CM, Nickel F, Jost C, Gwerder C et al. Neoadjuvant Chemotherapy in Pancreatic Cancer: An Appraisal of the Current High-Level Evidence. Pharmacology. 2021;106(3-4):143-53.
Versteijne E, Vogel JA, Besselink MG, Busch ORC, Wilmink JW, Daams JG et al. Meta-analysis comparing upfront surgery with neoadjuvant treatment in patients with resectable or borderline resectable pancreatic cancer. Br J Surg. 2018;105(8):946-58.
Nakata K, Ohuchida K, Aishima S, Sadakari Y, Kayashima T, Miyasaka Y et al. Invasive carcinoma derived from intestinal-type intraductal papillary mucinous neoplasm is associated with minimal invasion, colloid carcinoma, and less invasive behavior, leading to a better prognosis. Pancreas. 2011;40(4):581-7.
Aronsson L, Bengtsson A, Torén W, Andersson R, Ansari D. Intraductal papillary mucinous carcinoma versus pancreatic ductal adenocarcinoma: A systematic review and meta-analysis. Int J Surg. 2019;71:91-9.
Mas L, Lupinacci RM, Cros J, Bachet JB, Coulet F, Svrcek M. Intraductal papillary mucinous carcinoma versus conventional pancreatic ductal adenocarcinoma: A comprehensive review of clinical-pathological features, outcomes, and molecular insights. Int J Mol Sci. 2021;22(13):6756.
Allen PJ, Kuk D, Castillo CF, Basturk O, Wolfgang CL, Cameron JL et al. Multi-institutional Validation Study of the American Joint Commission on Cancer (8th Edition) Changes for T and N Staging in Patients With Pancreatic Adenocarcinoma. Ann Surg. 2017;265(1):185-91.
Kamarajah SK, Burns WR, Frankel TL, Cho CS, Nathan H. Validation of the American Joint Commission on Cancer (AJCC) 8th Edition Staging System for Patients with Pancreatic Adenocarcinoma: A Surveillance, Epidemiology and End Results (SEER) Analysis. Ann Surg Oncol. 2017;24(7):2023-30.
Mohanty S, Bilimoria KY. Comparing national cancer registries: The National Cancer Data Base (NCDB) and the Surveillance, Epidemiology, and End Results (SEER) program. J Surg Oncol. 2014;109(7):629-30.
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B et al. Using the National Cancer Database for Outcomes Research: A Review. JAMA Oncol. 2017;3(12):1722-8.
Nakao A, Harada A, Nonami T, Kaneko T, Takagi H. Clinical significance of carcinoma invasion of the extrapancreatic nerve plexus in pancreatic cancer. Pancreas. 1996;12(4):357-61.
Park H, An S, Eo S-H, Song K-B, Park J-h, Kim K-p et al. Survival effect of tumor size and extrapancreatic extension in surgically resected pancreatic cancer: proposal for improved T classification. Human Pathology. 2014;45(11):2341-6.
Kim JH, Eun HW, Kim KW, Lee JY, Lee JM, Han JK et al. Diagnostic performance of MDCT for predicting important prognostic factors in pancreatic cancer. Pancreas. 2013;42(8):1316-22.
Mochizuki K, Gabata T, Kozaka K, Hattori Y, Zen Y, Kitagawa H et al. MDCT findings of extrapancreatic nerve plexus invasion by pancreas head carcinoma: correlation with en bloc pathological specimens and diagnostic accuracy. Eur Radiol. 2010;20(7):1757-67.
Toshima F, Inoue D, Yoshida K, Izumozaki A, Yoneda N, Minehiro K et al. CT-diagnosed extra-pancreatic extension of pancreatic ductal adenocarcinoma is a more reliable prognostic factor for survival than pathology-diagnosed extension. Eur Radiol. 2022;32(1):22-33.
Williams M, Affolter K. Pancreatoduodenectomy: Perspectives on a Standardized Grossing Protocol for the Practicing Pathologist. AJSP: Reviews & Reports. 2020;25(4):168-73.
van Roessel S, Soer EC, van Dieren S, Koens L, van Velthuysen MLF, Doukas M et al. Axial slicing versus bivalving in the pathological examination of pancreatoduodenectomy specimens (APOLLO): a multicentre randomized controlled trial. HPB. 2021;23(9):1349-59.
Soer EC, Verbeke CS. Gross Evaluation and Histopathology. In: Søreide K, Stättner S, editors. Textbook of Pancreatic Cancer: Principles and Practice of Surgical Oncology. Cham: Springer International Publishing; 2021. p. 519-30.
Soer E, Brosens L, van de Vijver M, Dijk F, van Velthuysen ML, Farina-Sarasqueta A et al. Dilemmas for the pathologist in the oncologic assessment of pancreatoduodenectomy specimens : An overview of different grossing approaches and the relevance of the histopathological characteristics in the oncologic assessment of pancreatoduodenectomy specimens. Virchows Arch. 2018;472(4):533-43.
Grillo F, Ferro J, Vanoli A, Delfanti S, Pitto F, Peñuela L et al. Comparison of pathology sampling protocols for pancreatoduodenectomy specimens. Virchows Archiv. 2020;476(5):735-44.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 33.6 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, M., Thomas, A.S., Lee, S.Y. et al. Reconsidering the absence of extrapancreatic extension in T staging for pancreatic adenocarcinoma in the AJCC (8th ed) Staging Manual using the National Cancer Database. J Gastrointest Surg 27, 2484–2492 (2023). https://doi.org/10.1007/s11605-023-05850-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05850-2