Abstract
The dynamic behavior of osseointegrated implants can be used for the non-invasive evaluation of the condition of the bone-implant-interface (BII). The Advanced System for Implant Stability Testing (ASIST) is a vibration measurement system that relies on an impact technique and an analytical model to compute the interface stiffness and the ASIST stability coefficient (\(ASC\)). The objective of this work is to develop a finite element (FE) model capable of capturing the dynamic behaviour of the bone-anchored hearing aid under the ASIST loading condition. The model was validated with previously collected in vitro and in vivo data which were compared to the model’s acceleration responses and \(ASC\) scores. Similar acceleration responses were obtained, and the maximum absolute differences in \(ASC\) scores between the FE model and the in vitro and in vivo data were 1.15% and 5.48% respectively. The model was then used to show the existence of a relationship between the rod’s acceleration response and the BII stress field. Finally, the model was used to interpret the factors that affect the stiffness parameters of the ASIST analytical model. The interface stiffness and the system’s dynamic properties were more influenced (\(p<0.05\)) by the BII material and friction coefficient compared to the implant geometry.
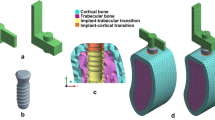
Graphical abstract
In this work, a finite element model of the bone anchored hearing aid was used to simulate the dynamic behaviour of the bone-implant system under the ASIST’s loading conditions. The model was first validated with previously collected experimental and clinical results. The validated model was then used to study the relationship between the impact rod’s acceleration response and the response at the bone implant interface. Finally, the model was used to formulate a better understanding on the influencing factors on the interface stiffness.










Similar content being viewed by others
Abbreviations
- ASIST:
-
Advanced System for Implant Stability Testing
- BII:
-
Bone implant interface
- FE:
-
Finite element
- OI:
-
Osseointegrated implant
References
Brånemark R, Brånemark PI, Rydevik B, Myers RR (2001) Osseointegration in skeletal reconstruction and rehabilitation: a review. J Rehabil Res Dev 38(2):175–181
Gao X, Fraulob M, Haïat G (2019) Biomechanical behaviours of the bone–implant interface: a review. JRSocInterface 16:20190259. https://doi.org/10.1098/rsif.2019.0259
Zanetti EM, Pascoletti G, Cali M, Bignardi C, Franceschini G (2018) Clinical assessment of dental implant stability during follow-up: what is actually measured, and perspectives. Biosensors 8(68). https://doi.org/10.3390/bios8030068
Mathieu V, Vayron R, Richard G, Lambert G, Naili S, Meningaud JP et al (2014) Biomechanical determinants of the stability of dental implants: influence of the bone-implant interface properties. J Biomech 47(1):3–13. https://doi.org/10.1016/j.jbiomech.2013.09.021
Pattijn V, Van Lierde C, Van Der Perre G, Naert I, Vander SJ (2006) The resonance frequencies and mode shapes of dental implants: rigid body behaviour versus bending behaviour A numerical approach. J Biomech 39(5):939–947. https://doi.org/10.1016/j.jbiomech.2005.01.035
Westover L, Faulkner G, Hodgetts W, Raboud D (2016) Advanced System for Implant Stability Testing (ASIST). J Biomech. 49:3651–9. https://doi.org/10.1016/j.jbiomech.2016.09.043
Westover L, Faulkner G, Hodgetts W, Raboud D (2018) Comparison of implant stability measurement devices for bone-anchored hearing aid systems. J Prosthet Dent. 119(1):178–84. https://doi.org/10.1016/j.prosdent.2017.02.021
Mohamed M, Pisavadia H, Westover L (2021) A finite element model for evaluating the effectiveness of the Advanced System for Implant Stability Testing (ASIST). J Biomech 124. https://doi.org/10.1016/j.jbiomech.2021.110570
Zanetti EM, Ciaramella S, Calì M, Pascoletti G, Martorelli M, Asero R et al (2018) Modal analysis for implant stability assessment: sensitivity of this methodology for different implant designs. Dent Mater 34(8):1235–45. https://doi.org/10.1016/j.dental.2018.05.016
AsgharzadehShirazi H, Ayatollahi MR, Asnafi A (2017) To reduce the maximum stress and the stress shielding effect around a dental implant–bone interface using radial functionally graded biomaterials. Comput Methods Biomech Biomed Engin. 20(7):750–9. https://doi.org/10.1080/10255842.2017.1299142
Gümrükçü Z, Korkmaz YT (2018) Influence of implant number, length, and tilting degree on stress distribution in atrophic maxilla: a finite element study. Med Biol Eng Comput 56(6):979–989. https://doi.org/10.1007/s11517-017-1737-4
Hernandez-Rodriguez MAL, Contreras-Hernandez GR, Juarez-Hernandez A, Beltran-Ramirez B, Garcia-Sanchez E (2015) Failure analysis in a dental implant. Eng Fail Anal. 57:236–42. https://doi.org/10.1016/j.engfailanal.2015.07.035
Muraru L, Van Lierde C, Naert I, Vander Sloten J, Jaecques SVN (2009) Three-dimensional finite element models based on in vivo microfocus computed tomography: elimination of metal artefacts in a small laboratory animal model by registration with artefact-free reference images. Adv Eng Softw 40(11):1207–10. https://doi.org/10.1016/j.advengsoft.2009.06.002
Zhuang HB, Pan MCH, Chen JZ, Wu JW, Chen CS (2014) A noncontact detection technique for interfacial bone defects and osseointegration assessment surrounding dental implants. Meas J Int Meas Confed 55:335–342. https://doi.org/10.1016/j.measurement.2014.05.039
Lamalfa E, Rizzo P (2015) Modeling the electromechanical impedance technique for the assessment of dental implant stability. J Biomech. 48(10):1713–20. https://doi.org/10.1016/j.jbiomech.2015.05.020
Zhai M, Li B, Li D (2017) Effects on the torsional vibration behavior in the investigation of dental implant osseointegration using resonance frequency analysis: a numerical approach. Med Biol Eng Comput 55(9):1649–1658. https://doi.org/10.1007/s11517-017-1612-3
Vayron R, Nguyen VH, Bosc R, Naili S, Haïat G (2015) Finite element simulation of ultrasonic wave propagation in a dental implant for biomechanical stability assessment. Biomech Model Mechanobiol. 14(5):1021–32. https://doi.org/10.1007/s10237-015-0651-7
Westover L, Faulkner G, Hodgetts W, Kamal F, Lou E, Raboud D (2018) Longitudinal evaluation of bone-anchored hearing aid implant stability using the Advanced System for Implant Stability Testing (ASIST). Otol Neurotol 39:e489–e495. https://doi.org/10.1097/MAO.0000000000001815
Engineering Toolbox. Metals and Alloys-Densities [Internet]. 2004. Available from: https://www.engineeringtoolbox.com/metal-alloys-densities-d_50.html
Swain R. Development and modelling of an impact test to determine the bone implant interface properties of osseointegrated implants. University of Alberta; 2006.
Rahmoun J, Auperrin A, Delille R, Naceur H, Drazetic P (2014) Characterization and micromechanical modeling of the human cranial bone elastic properties. Mech Res Commun. 60:7–14. https://doi.org/10.1016/j.mechrescom.2014.04.001
Peterson J, Dechow PC (2003) Material properties of the human cranial vault and zygoma. Anat Rec - Part A Discov Mol Cell Evol Biol 274(1):785–797. https://doi.org/10.1002/ar.a.10096
Delille R, Lesueur D, Potier P, Drazetic P, Markiewicz E (2007) Experimental study of the bone behaviour of the human skull bone for the development of a physical head model. Int J Crashworthiness 12(2):101–108
Swain R, Faulkner G, Raboud D, Wolfaardt J (2008) An improved impact technique for monitoring percutaneous implant integrity. Int J Oral Maxillofac Implants 23(2):263–269
Smith M (2009) ABAQUS/Standard user’s manual, Version 6.9. United States: Dassault Systemes Simulia Corp
Polycarpou AA (2005) Measurement and modeling of normal contact stiffness and contact dam** at the Meso. 127(February):52–60
Westover L (2016) Evaluating of the interface mechanical properties of craniofacial implants and natural teeth through development of the Advanced System for Implant Stability Testing (ASIST). University of Alberta
Al-Jetaily S, Al-dosari AAF (2011) Assessment of Osstell™ and Periotest® systems in measuring dental implant stability (in vitro study). Saudi Dent J 23(1):17–21. https://doi.org/10.1016/j.sdentj.2010.09.003
K.Chopra A (2012) Dynamics of structures theory and applications to earthquake engineering. Fourth. Prentice Hall, 347–392 p
Adeeb S. Introduction to solid mechanics and finite element analysis [Internet]. 2021. Available from: http://sameradeeb.srv.ualberta.ca
Lee JHC, Ondruschka B, Falland-Cheung L, Scholze M, Hammer N, Tong DC et al (2019) An investigation on the correlation between the mechanical properties of human skull bone, its geometry, microarchitectural properties, and water content. J Healthc Eng 2019. https://doi.org/10.1155/2019/6515797
Pammer D (2019) Evaluation of postoperative dental implant primary stability using 3D finite element analysis. Comput Methods Biomech Biomed Engin. 22(3):280–7. https://doi.org/10.1080/10255842.2018.1552682
Foghsgaard S, Caye-Thomasen P (2014) A new wide-diameter bone-anchored hearing implantvprospective 1-year data on complications, implant stability, and survival. Otol Neurotol 35(7):1238–1241
Moreira A, Rosa J, Freitas F, Francisco H, Luís H, Caramês J (2021) Influence of implant design, length, diameter, and anatomic region on implant stability: a randomized clinical trial. Rev Port Estomatol Med Dentária e Cir Maxilofac 61(1). https://doi.org/10.24873/j.rpemd.2021.01.816
Nelissen RC, den Besten CA, Mylanus EAM, Hol MKS (2016) Stability, survival, and tolerability of a 4.5-mm-wide bone-anchored hearing implant: 6-month data from a randomized controlled clinical trial. Eur Arch Oto-Rhino-Laryngology 273(1):105–11. https://doi.org/10.1007/s00405-015-3593-
Funding
This research was supported by Glenrose Rehabilitation Research Innovation and Technology (GRRIT), Mathematics of Information Technology and Complex Systems (Mitacs), and the Natural Sciences and Engineering Research Council of Canada (NSERC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1 Mesh independence
Appendix 2 Complete ANOVA analysis
Tables 7, 8, 9, 10, 11, 12 and 13
Rights and permissions
About this article
Cite this article
Mohamed, M., Westover, L. Evaluating the dynamic behaviour of bone anchored hearing aids using a finite element model and its applications to implant stability assessment. Med Biol Eng Comput 60, 2779–2795 (2022). https://doi.org/10.1007/s11517-022-02607-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02607-y