Abstract
Air pollution may increase the risk of hypertension (HTN) by increasing oxidative stress and inflammation, and reducing sodium excretion. Potassium intake may reduce the risk of HTN through sodium excretion and reduce inflammation and oxidative stress. This study is aimed at investigating the association between air pollutants and HTN and whether these associations differ based on the potassium intake data of Korean adults from the 2012–2016 Korean National Health and Nutrition Examination Survey (KNHANES). This cross-sectional study used data from KNHANES (2012–2016) combined with annual air pollutant data from the Ministry of Environment using administrative units. We included 15,373 adults who responded to the semi-food frequency questionnaire. Associations between ambient PM10, SO2, NO2, CO, and O3 with HTN according to potassium intake were assessed using the survey logistic regression model for complex samples analysis. After adjusting for potential covariates such as, age, sex, education level, smoking status, family income, alcohol consumption, body mass index (BMI), exercise status, and survey year, as the air pollutant score considering the five air pollutants increased (severe air pollution), the prevalence of HTN increased in a dose-dependent manner (p for trend < 0.001). Meanwhile, in the adults with higher potassium intake and who were exposed to lowest levels of air pollutants score (score = 0), the ORs of HTN were significantly lower (OR = 0.56, 95% CI: 0.32–0.97). In conclusion, our study suggests that exposure to air pollutants may increase the prevalence of HTN among Korean adults. However, high potassium intake may help prevent HTN caused by air pollutants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mean levels of air pollutants such as particulate matter (PM)2.5, PM10, nitrogen dioxide (NO2), and carbon monoxide (CO) were significantly reduced due to social distancing restrictions after the COVID-19 outbreak in Korea (Ju et al. 2021). However, the levels of PM2.5, PM10, and NO2 in Korea are still higher than the WHO (2021) air pollution guidelines (5 μg/m3 for PM2.5, 15 μg/m3 for PM10, and 10 ppb for NO2) (World Health Organization 2021). Several studies have reported that exposure to air pollution may cause oxidative stress by increasing the secretion of various pro-oxidative cytokines and can trigger systemic inflammation (Li et al. 2017; Sanidas et al. 2017). This leads to endothelial dysfunction, autonomic nervous system imbalance, vasoconstriction, and consequently, elevated blood pressure (BP) (Sanidas et al. 2017). In particular, PM exposure increases blood pressure (BP) due to abnormal DNA methylation (Bellavia et al. 2013) and reduces sodium excretion (Tsai et al. 2012).
According to the 2020 Korea National Health and Nutrition Examination Survey (KNHANES), among Korean adults aged ≥ 19 years, the prevalence of hypertension (HTN) was 28.1% in men and 16.8% in women (Korea Disease Control and Prevention Agency, KDCA 2020). HTN significantly increases the risk of cardiovascular, kidney, and other diseases (World Health Organization 2021).
Potassium is a major intracellular mineral that maintains total body fluid volume and acid and electrolyte balance through the Na/K ATPase pump. It is also involved in nerve transmission, muscle contraction, and kidney function (Stone et al. 2016). In Korea, the sufficient intake of potassium for adults is 3500 mg/day. However, the proportion of those over 19 years of age who consume less than the sufficient intake is very high, ranging from 58.4 to 88.6% in each age group (The Korean Nutrition Society 2020). This is probably due to the increased consumption of processed foods and the decreased consumption of vegetables and fruits. A systematic review and meta-analysis suggested that increased potassium intake reduces BP in adults with HTN (Aburto et al. 2013). Potassium is known to have antihypertensive effects by decreasing intravascular volume of sodium by increasing its excretion in the urine and is involved in endothelial-dependent vasodilation (Weaver 2013). In addition, sufficient potassium in the body reduces inflammation and oxidative stress (Stone et al. 2016). Therefore, we hypothesized that the prevalence of HTN would increase when the exposure to each air pollutant and the air pollutants score considering five air pollutants were high, whereas potassium intake would prevent it.
Therefore, our study investigated the association between each air pollutant and HTN and the air pollutant score considering five air pollutants in a representative Korean population using the data from the 2012–2016 KNHANES after linking atmospheric monitoring data. In addition, we investigated whether these associations differ according to the potassium intake.
Methods
Study population
KNHANES is an ongoing series of nationwide surveys conducted by the KDCA. KNHANES started in 1998 and has been conducted annually since 2007, and the rolling sampling survey method was applied to become a representative probability sample for Korea. To evaluate the health and nutritional status of Koreans, the statistical data were mainly composed of health interviews, health examinations, and nutrition. Health interviews and health examinations were conducted at the mobile examination center, and the nutrition surveys were conducted via household visits. Our study used data from KNHANES (KDCA 2012-2016a), which collected the usual dietary intake using a semi-food frequency questionnaire (FFQ). In total, 17,552 participants were included in this study. We excluded participants without BP-related variables (n = 1,722) and those whose air pollution data were unavailable based on their residential addresses (n = 85). For statistical analyses, we sequentially excluded participants with missing information on family income (n = 67), education level (n = 164), smoking status (n = 33), exercise status (n = 2), and abnormalities in energy intake (< 500 kcal/day or > 5000 kcal/day; n = 105). Thus, 15,373 participants were included in the final analysis.
Hypertension
Trained nurses measured BP using a mercury sphygmomanometer (Baumanometer Wall Unit 33, W. A. BAUM, Copiague, NY, USA) with a suitably sized cuff for the participant’s arm after the participant sat for at least 5 min to stabilize BP (KNHANES V ~ VII). Before BP measurement, the participants were instructed to sit with their backs on the backrest so that their spines were straight to sit in a stable and comfortable posture. BP was measured three times, and the mean blood pressure of the second and third measured values was used to analyze systolic BP (SBP) and diastolic BP (DBP). HTN was defined as SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, or the use of antihypertensive medication.
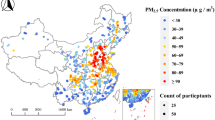
Ambient air pollution
We used atmospheric monitoring data for 24 h concentrations of ambient air pollutants between 2012 and 2016 from the Ministry of Environment (https://www.airkorea.or.kr). As of 2016, 264 air pollution monitoring networks have been installed in 82 units (city or county; administrative area units) in Korea. Ambient PM10, sulfur dioxide (SO2), NO2, CO, and ozone (O3) concentrations were measured using β-ray absorption, pulse ultraviolet (UV) fluorescence, chemiluminescence, non-dispersive infrared, and UV photometry, respectively (National Institute of Environmental Research 2020). For this study, we assigned the annual means of ambient PM10, SO2, NO2, CO, and O3 concentrations to each participant based on their residential addresses and computed them for the administrative divisions. For the cutoffs of PM10 and NO2, we followed the Korea Air Quality Standards (annual PM10 ≤ 50 μg/m3 and annual NO2 ≤ 30 ppb). As CO and O3 are not established in annual air quality standards, and all the levels of SO2 were lower than the annual standard (20 ppb), we used the median concentrations as cutoffs for SO2 (≤ 4.5 ppb), CO (≤ 549.1 ppb), and O3 (≤ 24.7 ppb). For the air pollutant score, 1 point was given for levels of above the cutoff value and 0 point was given for levels equal or below the cutoff value, and the sum of each pollutant was calculated. These scores were summed, and air pollution was considered severe when the score was high.
Dietary factors
The FFQ, consisting of 112 foods/dishes, included queries on the average frequency of intake over the past year and included nine intake frequency categories: three times a day, twice a day, once a day, 5–6 times a week, 2–4 times a week, once a week, 2–3 times a month, once a month, and never or seldom (Yun et al. 2013). The average intake of each food/dish was divided into three or four items using a general unit for each food or dish (e.g., bowls, plates, or pieces). To calculate the calorie and nutrient contents for each item, the frequency of intake was converted to frequency of intake per day, and the intake was calculated by getting the ratio of the intake standard. The FFQ used in this study has acceptable reproducibility and validity as a tool that reflects the nutrient intake of Koreans (Kim et al. 2015, Yum and Lee 2016). Energy-adjusted potassium intake was adjusted for the total energy intake using the residual method (Willett et al. 1997).
Other covariates
Our analysis considered the following covariates: age, sex, education level, smoking status, family income, alcohol consumption, body mass index (BMI), exercise status, and survey year. Education level was categorized into three levels: less than middle school graduate, high school graduate, and college degree or higher. Smoking status was categorized into three groups: never, former, and current. Alcohol consumption was categorized into five groups: never, past, ≤ 1 time/month, 2–4 times/month, and ≥ 2 times/week. BMI was categorized into three groups according to the Asia–Pacific classification (Pan and Yeh 2008): underweight & normal (< 23 kg/m2), overweight (23–24.99 kg/m2), and obese (≥ 25 kg/m2). The survey year (the subject’s examination year) was adjusted as a continuous variable. Family income was categorized into four groups: low, middle-low, middle-high, and high. Exercise status was divided into a group that did not exercise at all (no) and a group that exercised for more than one day (yes) by asking whether they performed strength training for one week.
Statistical analysis
Statistical data analysis was performed using SAS survey procedures (version 9.4; SAS Institute Inc.) to account for the complex sampling, multi-stage study design, and weights of KNHANES. As we used combined data from five years of continuous KNHANES (KDCA 2012-2016b), we computed five-year survey weights to account for oversampling, survey non-response, and post-stratification according to the Analytic Manual of KDCA. General characteristics were described as weighted mean and standard error (SE) for continuous variables and weighted percentage of categorical variables. The survey t-test for continuous variables and the Rao–Scott chi-square test for categorical variables were used to test the differences in participant characteristics. We used survey logistic regression models to evaluate the association of ambient PM10, SO2, NO2, CO, and O3 (high and low levels, and air pollutant score), and potassium intake with HTN. In addition, we estimated the odds ratio (OR) for HTN per interquartile range (IQR) change (5.7 μg/m3 for PM10, 1.3 ppb for SO2, 10.6 ppb for NO2, 94.1 ppb for CO, and 6.3 ppb for O3) for each air pollutant with 95% confidence interval (CI). Finally, the association between air pollutants score and HTN was stratified according to the potassium intake.
Results
General characteristics
Table 1 presents the general characteristics of the study participants according to their HTN status. Adults with HTN were significantly more likely to be older, have a higher proportion of males, have lower education levels and family income, consume alcohol frequently, and have a higher proportion of obese or current and former smokers compared to adults without HTN.
Association of HTN with air pollutants and potassium intake
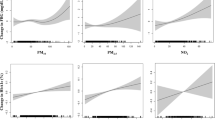
Table 2 shows the ORs for HTN according to air pollutants and potassium intake. For the IQR change of each air pollutant concentration, the ORs for HTN were 1.11 (95% CI: 1.03–1.19) by IQR change in PM10 (5.7 μg/m3), 1.12 (95% CI: 1.05–1.21) by IQR change in NO2 (10.6 ppb), 1.14 (95% CI: 1.05–1.25) by IQR change in CO (94.1 ppb), and 0.87 (95% CI: 0.80–0.95) by IQR change in O3 (6.3 ppb).
For the high versus low levels of each air pollutant, in adults who were exposed to high levels, the ORs for HTN were 1.15 (95% CI: 1.01–1.30) in PM10, 1.17 (95% CI: 1.05–1.31) in SO2, 1.16 (95% CI: 1.01–1.33) in NO2, 1.17 (95% CI: 1.05–1.32) in CO, and 0.87 (95% CI: 0.77–0.98) in O3, compared to adults who were exposed to low levels.
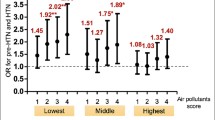
As the air pollutant score considering the five air pollutants increased (severe air pollution), the prevalence of HTN increased in a dose-dependent manner (p for trend < 0.001). Meanwhile, the highest tertile of potassium intake showed a lower prevalence of HTN than the lowest tertile of potassium intake (OR = 0.86, 95% CI: 0.75–0.99, p for trend = 0.037).
Association between HTN and air pollutants by potassium intake
Table 3 shows the ORs of air pollutants for HTN according to potassium intake. For high versus low levels of air pollutants according to potassium intake, even in adults who were exposed to high levels of PM10 and SO2, the ORs of HTN were significantly lower in those who consumed higher potassium (OR = 0.74, 95% CI: 0.58–0.95 for PM10; OR = 0.83, 95% CI: 0.70–0.98 for SO2). In addition, the ORs for HTN were significantly lower in adults exposed to low levels of PM10, SO2, NO2, and CO, and a higher intake of potassium than those in adults exposed to high levels of these air pollutants and a lower intake of potassium (OR = 0.73, 95% CI: 0.59–0.90 for PM10; OR = 0.74, 95% CI: 0.60–0.92 for SO2, OR = 0.73, 95% CI: 0.58–0.92 for NO2, OR = 0.75, 95% CI: 0.62–0.92 for CO).
Association between HTN and air pollutant score by potassium intake
Table 4 shows the ORs of air pollutants score for HTN according to potassium intake. In adults with higher potassium intake and who were exposed to lowest levels of air pollutants score, the ORs of HTN were significantly lower (OR = 0.56, 95% CI: 0.32–0.97) compared to adults with lower potassium intake and who were exposed to highest levels of air pollutants.
Discussion
In this study, we found that high exposure to PM10, NO2, SO2, and CO was significantly associated with a higher prevalence of HTN than that by low exposure to each air pollutant. As the air pollutant score increased (exposure to severe air pollution), the prevalence of HTN also increased in a dose-dependent manner. Additionally, in adults with higher intake potassium and who were exposed to lowest levels of air pollutants score (score = 0), the prevalence of HTN was significantly lower compared to those who consumed lower potassium and exposed to higher levels of air pollutants score (score = 4).
According to KNHANES 2020, among Korean adults aged ≥ 19 years, the prevalence of HTN was 28.1% in men and 16.8% in women (KDCA 2020). Kim et al. (2021) reported that the prevalence of HTN significantly increased over the years along with other chronic diseases such as diabetes, hypercholesterolemia, and obesity (Kim et al. 2021). Proper management is crucial because uncontrolled high BP causes numerous complications such as heart attack, stroke, heart failure, renal failure, and dementia (Ramirez and Sullivan 2018).
In 2018, Yang and colleagues included 100 studies in their meta-analysis and reported positive association of short-term exposure to PM10, PM2.5, SO2, and NO2 with HTN (Yang et al. 2018). Another meta-analysis by Cai et al. pooled data from 17 studies and reported positive association of short-term exposure to SO2, and PM10, and long-term exposure to PM10 and NO2 (Cai et al. 2012). Long-term exposure to PM2.5 increases BP by impairing renal D1 receptor-mediated sodium excretion through upregulation of G protein-coupled receptor kinase type 4 expression as shown in an experimental model (Lu et al. 2018). Third, other air pollutants, O3 may affect BP by intracellular oxidative stress (Paffett et al. 2015), and exposure to SO2, NO2, and PM2.5 may increase the inflammatory response (Ljungman et al. 2009; Panasevich et al. 2009) and endothelial dysfunction (Zhang et al. 2016). Indeed, Xu et al. reported that short-term exposure to gaseous air pollutants such as O3, NO2, and SO2 is associated with increased levels of circulating inflammatory biomarkers such as CRP and TNF-α (Xu et al. 2022). Therefore, when these air pollutants are high, there may be a negative synergistic effect of increasing BP. Our study found that as the air pollutant score increased (exposure to severe air pollution), the prevalence of HTN increased in a dose-dependent manner. However, exposure to O3 alone reduced the prevalence of HTN. Similar to our study, Ju et al. reported that exposure to O3 reduced the prevalence of age-related macular degeneration in middle-aged and older adults (Ju et al. 2022). They suggested that this result may be due to low-level exposure to O3 concentrations (range of annual O3, 19–40 ppb) in Korean adults. Although no significant association between O3 levels and HTN was found in a meta-analysis (Yang et al. 2018), a study in China with a relatively high concentration of O3 reported that interquartile range increase in O3 exposure was associated with HTN (OR = 1.48, 95% CI: 1.20–1.83) (Zhang et al. 2020); thus, further studies considering short-term or long-term exposure and exposure concentrations of O3 are needed.
Several studies have reported that dietary patterns, including antioxidant nutrient (Xu et al. 2021) and vitamin intake (Péter et al. 2015), are effective in reducing the risk of HTN induced by air pollution. This may be because antioxidant nutrients stabilize reactive free radicals and serve as the first line of defense against reactive free radical attack (Milisav et al. 2018).
Potassium is an essential mineral that maintains total body fluid volume and acid and electrolyte balance and is involved in nerve transmission, muscle contraction, and kidney function (Stone et al. 2016). In addition, potassium has antihypertensive effects due to decreased intravascular volume through increased excretion of sodium in the urine and is involved in endothelial-dependent vasodilation through the Na/K ATPase pump (Weaver 2013). A systematic review and meta-analysis suggested that increased potassium intake reduces BP in adults with HTN (Aburto et al. 2013).
In our study, adults with higher potassium intake and who were exposed to lowest levels of air pollutants score, the prevalence of HTN was significantly lower compared to those with lowest potassium intake and who were exposed to highest levels of air pollutants score. This may be because, as mentioned above, air pollution increases oxidative stress and inflammation and reduces sodium excretion; whereas, sufficient potassium in the body reduces inflammation and oxidative stress and promotes sodium excretion (Stone et al. 2016). In addition, potassium intake may help reduce blood pressure and improve vascular outcomes through the following mechanisms: modulation of baroreceptor sensitivity, reduced sensitivity to catecholamine, improved insulin sensitivity, and reduction of sympathetic activity and renin production (Houston 2011; Penton et al. 2015). However, a dose–response meta-analysis of randomized controlled trials reported that both low and high potassium intake may increase BP levels (Filippini et al. 2020). They suggested that increased potassium intake may help reduce BP in most populations, whereas high potassium intake may not be beneficial in participants, such as those taking BP medications or having a high baseline potassium intake or low sodium intake. Therefore, when ingesting in the form of potassium supplement, it is necessary to ensure proper intake in consideration of the participants’ characteristics.
According to the 2020 Dietary Reference Intakes for Koreans, the sufficient intake of potassium for adults is 3,500 mg/day. However, the proportion of those over 19 years of age who consume less than the sufficient intake is very high, ranging from 58.4 to 88.6% in each age group (The Korean Nutrition Society 2020). In addition, although vegetables including oriental melon (675 mg/150 g), spinach (553 mg/70 g), tomatoes (375 mg/150 g), potatoes (469 mg/140 g), and legumes (361 mg/20 g) contain high amounts of potassium per serving size, the main sources of potassium intake by Koreans are kimchi (125 mg/40 g), pork (195 mg/60 g), and white rice (80 mg/90 g) (The Korean Nutrition Society 2020). Therefore, Koreans with HTN need to increase their potassium intake by consuming fruits and vegetables rather than foods with high sodium content or red meat.
This study has several strengths. First, we combined KNHANES data from 2012 to 2016, a representative sample of the general population in Korea, and data on the five major air pollutants from the Ministry of Environment. Second, we found an association between HTN and air pollution, and these associations differed with potassium intake, which has not been identified in Korea. Third, our study scored and analyzed the cutoff values for air pollutants to consider all high air pollutant exposures. Fourth, we confirmed the results of the adjustment for sodium intake interacting with potassium, and the results after adjusting for sodium intake were similar to the results before adjusting for sodium intake (data not shown). However, this study has some limitations. First, our study had a cross-sectional design which does not allow for a causal interpretation between air pollutant exposure and HTN. This is because our results did not reflect past exposure to air pollutants as there was no information on the change of residence of the participants. Second, we used the annual mean of each pollutant computed for wider units (administrative divisions). However, in a previous study (Ju et al. 2022) that presented air pollution concentrations in a wider unit (administrative divisions) and a smaller unit (local/town), there was no difference in the results according to the two units of investigation of air pollutants.
In conclusion, our study suggests that exposure to air pollutants may increase the prevalence of HTN in Korean adults. However, a high potassium intake may help prevent HTN caused by air pollutants. In addition, policy efforts to reduce the concentration of air pollution at the national level will be needed for public health.
Data availability
The data used in this study are freely available from the following sources: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do.
References
Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP (2013) Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 346:f1378. https://doi.org/10.1136/bmj.f1378
Bellavia A, Urch B, Speck M, Brook RD, Scott JA, Albetti B, Behbod B, North M, Valeri L, Bertazzi PA, Silverman F, Gold D, Baccarelli AA (2013) DNA hypomethylation, ambient particulate matter, and increased blood pressure: findings from controlled human exposure experiments. J Am Heart Assoc 2:e000212. https://doi.org/10.1161/JAHA.113.000212
Cai Y, Zhang B, Ke W, Feng B, Lin H, **ao J, Zeng W, Li X, Tao J, Yang Z, Ma W, Liu T (2016) Associations of short-term and long-term exposure to ambient air pollutants with hypertension: a systematic review and meta-analysis. Hypertension 68:62–70. https://doi.org/10.1161/HYPERTENSIONAHA.116.07218.10.1111/joim.13467
de Bont J, Jaganathan S, Dahlquist M, Persson Å, Stafoggia M, Ljungman P (2022) Ambient air pollution and cardiovascular diseases: an umbrella review of systematic reviews and meta-analyses. J Intern Med 291:779–800
Filippini T, Naska A, Kasdagli MI, Torres D, Lopes C, Carvalho C, Moreira P, Malavolti M, Orsini N, Whelton PK, Vinceti M (2020) Potassium intake and blood pressure: a dose-response meta-analysis of randomized controlled trials. J Am Heart Assoc 9:e015719. https://doi.org/10.1161/JAHA.119.015719
Houston MC (2011) The importance of potassium in managing hypertension. Curr Hypertens Rep 13:309–317. https://doi.org/10.1007/s11906-011-0197-8
Ju MJ, Oh J, Choi YH (2021) Changes in air pollution levels after COVID-19 outbreak in Korea. Sci Total Environ 750:141521. https://doi.org/10.1016/j.scitotenv.2020.141521
Ju MJ, Kim J, Park SK, Kim DH, Choi YH (2022) Long-term exposure to ambient air pollutants and age-related macular degeneration in middle-aged and older adults. Environ Res 204:111953. https://doi.org/10.1016/j.envres.2021.111953
Kim DW, Song S, Lee JE, Oh K, Shim J, Kweon S, Paik HY, Joung H (2015) Reproducibility and validity of an FFQ developed for the Korea National Health and Nutrition Examination Survey (KNHANES). Public Health Nutr 18:1369–1377. https://doi.org/10.1017/S1368980014001712
Kim KN, Kim JH, Jung K, Hong YC (2016) Associations of air pollution exposure with blood pressure and heart rate variability are modified by oxidative stress genes: a repeated-measures panel among elderly urban residents. Environ Health 15:47. https://doi.org/10.1186/s12940-016-0130-3
Kim KI, Ji E, Choi JY, Kim SW, Ahn S, Kim CH (2021) Ten-year trends of hypertension treatment and control rate in Korea. Sci Rep 11:6966. https://doi.org/10.1038/s41598-021-86199-x
KDCA (2012-2016a) Korea health statistics: Korea National Health and Nutrition Examination Survey (KNHANES V~ VII). https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do. Accessed 16 May 2022
KDCA (2012-2016b) Medical examination guideline: Korea National Health and Nutrition Examination Survey (KNHANES V~ VII). https://knhanes.kdca.go.kr/knhanes/sub04/sub04_02_02.do?classType=4. Accessed 1 Feb 2023
KDCA (2020) Korea Health Statistics: Korea National Health and Nutrition Examination Survey 2020. https://knhanes.kdca.go.kr/knhanes/sub04/sub04_04_01.do. Accessed 26 Aug 2022
Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, Chen J, Hao K, Kinney PL, Chen H, Kan H (2017) Particulate matter exposure and stress hormone levels: a randomized, double-blind, crossover trial of air purification. Circulation 136:618–627. https://doi.org/10.1161/CIRCULATIONAHA.116.026796
Ljungman P, Bellander T, Schneider A, Breitner S, Forastiere F, Hampel R, Illig T, Jacquemin B, Katsouyanni K, von Klot S, Koenig W, Lanki T, Nyberg F, Pekkanen J, Pistelli R, Pitsavos C, Rosenqvist M, Sunyer J, Peters A (2009) Modification of the interleukin-6 response to air pollution by interleukin-6 and fibrinogen polymorphisms. Environ Health Perspect 117:1373–1379. https://doi.org/10.1289/ehp.0800370
Lu X, Ye Z, Zheng S, Ren H, Zeng J, Wang X, Jose PA, Chen K, Zeng C (2018) Long-term exposure of fine particulate matter causes hypertension by impaired renal D(1) receptor-mediated sodium excretion via upregulation of G protein-coupled receptor kinase type 4 expression in Sprague-Dawley rats. J Am Heart Assoc 7. https://doi.org/10.1161/JAHA.117.007185
Milisav I, Ribarič S, Poljsak B (2018) Antioxidant vitamins and ageing. Subcell Biochem 90:1–23. https://doi.org/10.1007/978-981-13-2835-0_1
National Institute of Environmental Research (2020) Annual report of air quality in Korea 2020. www.airkorea.or.kr/web/detailViewDown?pMENU_NO=125. Accessed 15 Jun 2022
Paffett ML, Zychowski KE, Sheppard L, Robertson S, Weaver JM, Lucas SN, Campen MJ (2015) Ozone inhalation impairs coronary artery dilation via intracellular oxidative stress: evidence for serum-borne factors as drivers of systemic toxicity. Toxicol Sci 146:244–253. https://doi.org/10.1093/toxsci/kfv093
Pan WH, Yeh WT (2008) How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: an extension of Asian-Pacific recommendations. Asia Pac J Clin Nutr 17:370–374
Panasevich S, Leander K, Rosenlund M, Ljungman P, Bellander T, de Faire U, Pershagen G, Nyberg F (2009) Associations of long- and short-term air pollution exposure with markers of inflammation and coagulation in a population sample. Occup Environ Med 66:747–753. https://doi.org/10.1136/oem.2008.043471
Penton D, Czogalla J, Loffing J (2015) Dietary potassium and the renal control of salt balance and blood pressure. Pflugers Arch 467:513–530. https://doi.org/10.1007/s00424-014-1673-1
Péter S, Holguin F, Wood LG, Clougherty JE, Raederstorff D, Antal M, Weber P, Eggersdorfer M (2015) Nutritional solutions to reduce risks of negative health impacts of air pollution. Nutrients 7:10398–10416. https://doi.org/10.3390/nu7125539
Ramirez LA, Sullivan JC (2018) Sex differences in hypertension: where we have been and where we are going. Am J Hypertens 31:1247–1254. https://doi.org/10.1093/ajh/hpy148
Sanidas E, Papadopoulos DP, Grassos H, Velliou M, Tsioufis K, Barbetseas J, Papademetriou V (2017) Air pollution and arterial hypertension. A new risk factor is in the air. J Am Soc Hypertens 11:709–715. https://doi.org/10.1016/j.jash.2017.09.008
Stone MS, Martyn L, Weaver CM (2016) Potassium intake, bioavailability, hypertension, and glucose control. Nutrients 8. https://doi.org/10.3390/nu8070444
The Korean Nutrition Society (2020) Dietary reference intakes for Koreans 2020 Ministry of Health and Welfare: Sejong https://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&CONT_SEQ=362385. Accessed 11 Nov 2022
Tsai DH, Riediker M, Wuerzner G, Maillard M, Marques-Vidal P, Paccaud F, Vollenweider P, Burnier M, Bochud M (2012) Short-term increase in particulate matter blunts nocturnal blood pressure dip** and daytime urinary sodium excretion. Hypertension 60:1061–1069. https://doi.org/10.1161/HYPERTENSIONAHA.112.195370
Weaver CM (2013) Potassium and health. Adv Nutr 4:368s–377s. https://doi.org/10.3945/an.112.003533
World Health Organization (2021) WHO global air quality guidelines. Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: World Health Organization; 2021
Willett WC, Howe GR, Kushi LH (1997) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65:1220S-1228S. https://doi.org/10.1093/ajcn/65.4.1220S. (discussion 1229S-1231S)
World Health Oragnization (2021) Hypertension www.who.int/news-room/fact-sheets/detail/hypertension Acessed 16 June 2022
Xu H, Guo B, Qian W, Ciren Z, Guo W, Zeng Q, Mao D, **ao X, Wu J, Wang X, Wei J, Chen G, Li S, Guo Y, Meng Q, Zhao X (2021) Dietary pattern and long-term effects of particulate matter on blood pressure: a large cross-sectional study in Chinese adults. Hypertension 78:184–194. https://doi.org/10.1161/HYPERTENSIONAHA.121.17205
Xu Z, Wang W, Liu Q, Li Z, Lei L, Ren L, Deng F, Guo X, Wu S (2022) Association between gaseous air pollutants and biomarkers of systemic inflammation: a systematic review and meta-analysis. Environ Pollut 292:118336. https://doi.org/10.1016/j.envpol.2021.118336
Yang BY, Qian Z, Howard SW, Vaughn MG, Fan SJ, Liu KK, Dong GH (2018) Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ Pollut 235:576–588. https://doi.org/10.1016/j.envpol.2018.01.001
Yum J, Lee S (2016) Development and evaluation of a dish-based semiquantitative food frequency questionnaire for Korean adolescents. Nutr Res Pract 10:433–441. https://doi.org/10.4162/nrp.2016.10.4.433
Yun SH, Shim JS, Kweon S, Oh K (2013) Development of a food frequency questionnaire for the Korea National Health and Nutrition Examination Survey: data from the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV). Korean J Nutr 46:186–196. https://doi.org/10.4163/kjn.2013.46.2.186
Zhang Y, Ji X, Ku T, Sang N (2016) Inflammatory response and endothelial dysfunction in the hearts of mice co-exposed to SO(2), NO(2), and PM(2.5). Environ Toxicol 31:1996–2005. https://doi.org/10.1002/tox.22200
Zhang J, Cai L, Gui Z, Wang S, Zeng X, Lai L, Lv Y, Tan K, Wang H, Huang C, Chen Y (2020) Air pollution-associated blood pressure may be modified by diet among children in Guangzhou, China. J Hypertens 38:2215–2222. https://doi.org/10.1097/HJH.0000000000002521
Acknowledgements
This study analyzed data provided by the Korea National Health and Nutrition Examination Survey 2012–2016. This research was supported by Gangneung-Wonju National University.
Author information
Authors and Affiliations
Contributions
JHK and HJK conceived and designed the study. JHK analyzed the data and drafted the manuscript. HJK reviewed and edited the manuscript. HJK supervised the study. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical standards
KNHANES (2012-2016) were conducted by the KDCA and all participants provided written informed consent. All survey protocols were approved by the Institutional Review Board of KDCA (approval numbers: 2012-01EXP-01-2C, 2013-07CON-03-4C and 2013-12EXP-03-5C).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kwak, J.H., Kim, H.J. Alleviating air pollutant-associated hypertension by potassium intake in Korean adults: a cross-sectional study from the 2012–2016 Korea National Health and Nutrition Examination Survey. Environ Sci Pollut Res 30, 73881–73889 (2023). https://doi.org/10.1007/s11356-023-27216-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-27216-6