Abstract
Oral anticoagulants (OACs) are recommended for patients with atrial fibrillation (AFib) having CHA2DS2-VASc score ≥ 2. However, the benefits of OAC initiation in patients with AFib and cancer at different levels of CHA2DS2-VASc is unknown. We included patients with new AFib diagnosis and a record of cancer (breast, prostate, or lung) from the 2012–2019 Surveillance, Epidemiology, and End Results (SEER)-Medicare database (n = 39,915). Risks of stroke and bleeding were compared between 5 treatment strategies: (1) initiated OAC when CHA2DS2-VASc ≥ 1 (n = 6008), (2) CHA2DS2-VASc ≥ 2 (n = 8694), (3) CHA2DS2-VASc ≥ 4 (n = 20,286), (4) CHA2DS2-VASc ≥ 6 (n = 30,944), and (5) never initiated OAC (reference group, n = 33,907). Confounders were adjusted using inverse probability weighting through cloning-censoring-weighting approach. Weighted pooled logistic regressions were used to estimate treatment effect [hazard ratios (HRs) and 95% confidence interval (95% CIs)]. We found that only patients who initiated OACs at CHA2DS2-VASc ≥ 6 had lower risk of stroke compared without OAC initiation (HR 0.64, 95% CI 0.54–0.75). All 4 active treatment strategies had reduced risk of bleeding compared to non-initiators, with OAC initiation at CHA2DS2-VASc ≥ 6 being the most beneficial strategy (HR = 0.49, 95% CI 0.44–0.55). In patients with lung cancer or regional/metastatic cancer, OAC initiation at any CHA2DS2-VASc level increased risk of stroke and did not reduce risk of bleeding (except for Regimen 4). In conclusion, among cancer patients with new AFib diagnosis, OAC initiation at higher risk of stroke (CHA2DS2-VASc score ≥ 6) is more beneficial in preventing ischemic stroke and bleeding. Patients with advanced cancer or low life-expectancy may initiate OACs when CHA2DS2-VASc score ≥ 6.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States (US), 2.7–6.1 million people were affected by atrial fibrillation (AFib) annually and it is projected to reach 12 million by 2050 [1]. AFib is associated with more than 454,000 hospitalizations and 158,000 deaths each year [2,3,4,−4]. Among patients with cancer, AFib was also associated with higher burden of adverse outcomes, such as ischemic stroke, venous thromboembolism (VTE), bleeding, and death compared with AFib patients without cancer [5,6,7,−8].
Although the benefit of oral anticoagulants (OACs) in patients with AFib has been well established [9], the current management of patients with AFib and cancer regarding OAC treatments remains suboptimal due to insufficient evidence [10]. Among patients with AFib and cancer, OAC initiation was associated with a slightly reduced risk of adverse event (ischemic stroke and intracranial bleeding) compared with non-users [11]. However, recent studies found only half of patients with AFib and cancer initiated OAC, much less than those without cancer [11,12,13,14]. One of the major challenges is to determine the appropriate time when patients with AFib and cancer should start OACs to maximize the benefit of stroke prevention while minimizing the risk of bleeding. In general, OAC initiation is recommended for AFib patients with a CHA2DS2-VASc score ≥ 2, a composite stroke risk score of congestive heart failure, hypertension, age, diabetes mellitus, prior stroke, transient ischemic attack, thromboembolism, vascular disease and sex category [9, 15]. However, such threshold has not been explored in patients with AFib and cancer. For example, when patient with existing cancer is newly diagnosed with AFib with low risk of ischemic stroke (i.e., CHA2DS2-VASc < 2), whether this patient should start the treatment immediately or wait until they reach a higher risk of ischemic stroke (i.e., CHA2DS2-VASc ≥ 4 or CHA2DS2-VASc ≥ 6). In some patient groups, anticoagulation is withheld because of a perceived unfavorable risk-benefit ratio [16]. Since patients with AFib and cancer are at higher risk of stroke and bleeding [5, 6], initiating OAC at low risk may be beneficial in stroke prevention, but may result in increased risk of bleeding. On the other hand, late OAC initiation may prevent risk of bleeding but increase risk of stroke in these patients. Although recent studies found that patients with AFib and cancer who had CHA2DS2-VASc ≥ 4 were more likely to receive OACs compared to patients with lower risk of stroke [17], the benefit of this treatment strategy has never been explored. Determining the benefit of initiating OACs at different levels of risk of stroke is critically important to optimize the management of patients with AFib and cancer.
In this study, we assessed and compared benefits of multiple OAC initiation treatment strategies at different thresholds of risk of stroke among newly diagnosed AFib patients with cancer using the target trial framework. The target trial framework is the application of design principles from randomized controlled trials (RCTs) to the analysis of observational data to improve the quality of observational epidemiology when a comparator trial is not yet available or feasible [18].
Materials and methods
Study design and data source
We used the target trial framework and STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) checklist to conduct and report a retrospective cohort study using the SEER registry linked to the Medicare database (cancer sites: breast, prostate, and lung) from 2011–2019 [19, 20]. The SEER registry contains patient demographics, primary tumor site, tumor characteristics, and cancer stage at diagnosis, treatment, and follow-up of cancer patients across the US [21]. The Medicare data add to SEER data health care services utilization (medical claims, procedures, and prescriptions) [22]. Table 1 summarizes the protocol for target trial and emulation procedure. The study design and study timeline are illustrated by Figure S1.
Study sample and eligibility criteria
Study sample
We included individuals aged ≥ 66, newly diagnosed non-valvular atrial fibrillation (NVAF) between January 1, 2012 and December 31, 2019, defined as any International Classification of Disease-9th Revision-Clinical Modification (ICD-9-CM) codes 427.31 or 427.32 or any International Classification of Disease-10th Revision-Clinical Modification (ICD-10-CM) codes I48.xx in any position on one Medicare inpatient claim or on two outpatient claims at least 7 days but < 1 year apart [23]. We retained patients with breast, lung, or prostate cancer—the most common cancer types with AFib—from the SEER file at any time before the initial AFib diagnosis (ICD-O-3 codes C50.0-C50.9 for breast; C34.0, C34.1, C34.2, C34.3, C34.8, C34.9, C33.9 for lung; C61.9 for prostate cancer). Patients were required to continuously enroll in Medicare part A, B, D, and without Medicare Advantage or Health Maintenance Organization (HMO) for at least 12 months before initial NVAF diagnosis.
Exclusion criteria
We adapted exclusion criteria from clinical trials [24, 25]. In addition, patients were excluded if they had any other indication than NVAF, contraindication to OACs or had the event of interest shortly before cohort entry: (1) any OAC use during the 12 months baseline period, (2) presence of valvular diseases, repair, or replacement, venous thromboembolism, or joint replacement during the 12 months baseline period, (3) any stroke within 14 days before first NVAF diagnosis, (4) major surgery (i.e., hip fracture, cardiac surgery) or critical bleeding within 30 days before first NVAF diagnosis, (5) renal impairment stage 5 or end-stage renal diseases during the 12 months baseline period. All ICD codes for identification of these conditions can be found in Table S1, Supplementary materials.
Treatment strategies and assignments
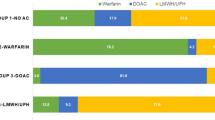
In the hypothetical target trial, eligible individuals were randomly assigned to one of the following 5 treatment strategies: (Regimen 1) initiated OAC when CHA2DS2-VASc ≥ 1, (Regimen 2) initiated OAC when CHA2DS2-VASc ≥ 2, (Regimen 3) initiated OAC when CHA2DS2-VASc ≥ 4, (Regimen 4) initiated OAC when CHA2DS2-VASc ≥ 6, and (Regimen 5) never initiated OAC (reference group). In the emulation of target trial, cloning, censoring, and weighting approach were used to mimic the randomization [26]. OAC prescriptions (including warfarin and dabigatran, apixaban, rivaroxaban, edoxaban) were identified from Medicare Part D Prescription Drug Event (PDE) files using national drug code (NDC)) [27]. CHA2DS2-VASc scores were computed from Medicare claims during12 months before AFib diagnosis and monthly during follow-up, based on a composite of conditions including congestive heart failure (1 point), hypertension (1), age ≥ 75 (2 point), diabetes mellitus (1 point), prior stroke, TIA, or thromboembolism (2 point), vascular disease (e.g. peripheral artery disease, myocardial infarction, aortic plaque) (1 point), age 65–74 years (1 point), and sex category (1 point) [15].
Follow-up
The follow-up started at the initial NVAF diagnosis (index date) and ended at the occurrence of a study outcome, the end of administrative censoring (12 months after baseline), death (all-cause deaths from the SEER and Medicare files via the variables of “Date of Death Flag”), loss to follow-up (the earliest of 30 days after the end of continuous Medicare Part A, B, or D enrollment or enrollment in an HMO), or December 31, 2019, whichever came first.
Outcomes
The outcomes of interest were ischemic stroke and major bleeding. We defined major bleeding and ischemic stroke using validated algorithms defined by ICD-9-CM and ICD-10-CM codes in the primary diagnosis from Medicare medical claims files [28, 29, 30].
Covariates
Covariates selected from prior literature were adjusted in the analysis [24, 28, 31]. Time-fixed baseline covariates were extracted within 12-month period prior to first AFib diagnosis, including: demographics (index age, sex, race/ethnicity, calendar year, geographical region, urbanicity), socioeconomic factors (household median income, percentage of household with education level below high school, and Medicaid eligibility), comorbidity risk scores (CHA2DS2-VASc, HAS-BLED, and Comorbidity Scores SEER-Medicare version 2021 by NCI) [32], individual comorbidities (asthma/chronic obstructive pulmonary disease, hematological disorders, dementia, depression, thrombocytopenia, acute kidney disease (AKD), peptic ulcer disease), cancer characteristics (time from cancer diagnosis to the onset of AFib, cancer type, cancer stage, tumor grade, active cancer status [28, 31]), cancer treatment (radiation, and cancer-directed surgery, and potentially interacting antineoplastic agents), and medication history (angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, calcium channel blockers, beta blockers, antiarrhythmic medications, diuretics, statin, pump proton inhibitors, and serotonin reuptake inhibitors). Socioeconomic factors such as household income and education level are available at the aggregate area level. If patients had more than one type of cancer before AFib diagnosis, we retained the most recent cancer diagnosis. Cancer treatments were obtained from diagnosis codes or procedures codes within 30 days before AFib diagnosis [33]. Due to high proportion of missing values, other cancer characteristics such as number of regional nodes examined, tumor size, TMN classification, and other cancer-type specific characteristics (i.e., hormone receptor status (HR) and human epidermal growth factor receptor 2 (HER2) for breast cancer or histologic type for lung cancer) were used for descriptive purpose but not adjusted in the models [34]. The following time-varying covariates were extracted monthly after AFib onset, including CHA2DS2-VASc score, HAS-BLED score, thrombocytopenia, AKD, radiation, cancer-directed surgery, and use of potentially interacting treatment with OACs. These variables may change over time and has an impact on outcomes and the OAC prescription in each month [35, 36]. All diagnosis codes, drug codes, and procedure codes for covariate ascertainment were described in Table S1, Supplementary materials. We used multiple imputation algorithms (fully conditional specification with logistic regression for categorical variables and predictive mean matching for continuous variables) to impute missing values (urbanicity, cancer summary stage, percentage of residents living below poverty, and percentage of non-high school graduates—Table S2, Supplementary Materials) [37].
Causal contrast
We computed the observational analog of per-protocol (PP) effects because cloning-censoring-weighting approach was used [38]. Those who were not compliant to their assigned treatment regimes were censored during follow-up.
Statistical analysis
Descriptive statistics such as mean and standard deviation (SD) for continuous variables, frequency count and percentage for categorical variables were used to describe the study sample. We quantified the incidence rates of ischemic stroke and major bleeding for each treatment strategy. In the main analysis, cloning-censoring-weighting procedure was used to estimate the treatment effect of 5 treatment strategies [26, 38]. Briefly, we created 5 copies for each individual’s person-time data, then assigned each copy to 5 treatment strategies. At baseline, replicates with baseline CHA2DS2-VASc score that did not comply with their assigned strategy were removed from the dataset. Next, replicates whose data were no longer consistent with their assigned strategy during follow-up were censored. To adjust for potential confounding during follow-up, unstabilized time-varying censoring weights were used. Cumulative weights at each time points due to protocol violation are the product of inverse probability of weights for treatment initiation (IPTWs) and inverse probability of censoring weights (IPCWs) due to loss to follow-up (See Technical Appendix). Total weights were truncated at 99th percentile to avoid extreme weights. To estimate the treatment effects for 5 strategies, we fitted a weighted pooled logistic regression estimated by generalized estimating equations (GEEs) with robust variance estimators. We obtained summary hazard ratios (HRs) with 95% confidence interval (95% CIs) and created weighted survival curves comparing four active treatment strategies with the reference strategy. Statistical analyses were conducted using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA).
Subgroup analyses and sensitivity analyses
We conducted the following subgroup analyses: cancer type (breast, lung, prostate), cancer status at baseline (active, history), cancer stage (in situ, local, regional, and distant), and tumor grade (I, II, and III). In addition, a series of sensitivity analyses were conducted. First, we extended follow-up time to 36 months to explore long-term outcomes for each treatment strategies. Second, since metastatic cancer patients were removed from randomized control trials due to their short live expectancy, we excluded them in this sensitivity analysis [24, 25]. Third, we removed individuals with thrombocytopenia at baseline, since these patients are at elevated risk of bleeding and may not eligible for OAC initiation [39, 40]. Fourth, we further truncated weights at 95th percentile to test the robustness of the treatment effects to the presence of extreme weights [59]. Using stabilized variance may reduce the variance and avoid extreme weights, but the stabilization procedures might not valid for cloning-censoring-weighting approach like our study [60]. However, the results remain robust in the sensitivity analysis after we truncated the weights to 95th percentile. Sixth, our findings may not be generalizable beyond the target population in this study (i.e., patients with newly diagnosed cancer on existing AFib, other cancer types, or non-Medicare populations). Future studies are warranted to investigate the benefits and risks of OACs among patients with other advanced cancer such as hematological cancers due to higher risk of stroke and bleeding in this population [61, 62].
Although our study emulated a hypothetical target trial and adopted components (i.e., inclusion/exclusion criteria, outcomes, and follow-up) from prior RCTs [24, 25], several components were not perfectly mimicked. Specifically, RCTs removed patients platelet count < 90,000/µL, systolic blood pressure ≥ 180 mmHg or diastolic blood pressure ≥ 100 mmHg, or creatinine clearance less than 30 mL/min at the screening visit [24, 25]. However, these lab values were not available in SEER-Medicare data. We therefore replaced these conditions with the presence of thrombocytopenia or severe renal impairments. In addition, several components were defined by clinicians’ assessment in RCTs, such as AFib definition by an electrocardiogram (ECG) document or congestive heart left failure with ventricular ejection fraction ≤ 35% [24, 25]. Moreover, therapeutic responses and adverse events were monitored with international normalized ratio (INR) and liver-function tests, which are not available in our emulation [24, 25]. Although non-randomization component has been criticized as the main source of bias in observational studies, it was not proven as the primary cause of inconsistency between observational and RCTs. Successful emulation without randomization has been conducted to benchmark the estimates from observational studies to RCTs and vice versa, especially during the COVID pandemic when the need of RCTs could not be met due to time constraint [63,64,65]. In this study, randomization was assumed using a cloning-censoring-weighting approach and the adjustment of measured time-varying confounding during follow-up [26]. It is also necessary to highlight that misspecification of time zero has been found as the major source of failure in obtaining valid causal effects in observational studies [19, 20]. In our study, we specified time zero by aligning the time when all inclusion and exclusion criteria met, start of treatment strategies, and follow-up. Such practice removed immortal time bias and prevalent user bias from our analysis [19, 20].
Our study has many strengths. Using the target trial emulation framework to design the study and the cloning–censoring–weighting approach, we explicitly designed a trial to answer a causal question. We included patients with newly AFib diagnosis and followed them after AFib diagnosis to remove survival bias. In addition, we further adjusted for important confounders such as cancer characteristics by the linkage between Medicare administrative claims data and the SEER registry. We pre-specified a wide range of subgroup analyses and sensitivity analyses to confirm the robustness of the main analysis. Our findings are expected to help clinicians’ decision making in optimizing OAC initiation and individualizing their decisions based on patient’s cancer characteristics.
Conclusion
Among cancer patients with new AFib diagnosis, OAC initiation at higher risk of stroke (CHA2DS2-VASc score ≥ 6) may be more beneficial in preventing ischemic stroke and bleeding. Patients with advanced cancer status or low life-expectancy may initiate OACs when CHA2DS2-VASc score ≥ 6.
References
Patel NJ, Deshmukh A, Pant S et al (2014) Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation 129(23):2371–2379
Benjamin EJ, Muntner P, Alonso A et al (2019) Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 139(10):e56–e528
Centers for Disease Control and Prevention - National Center for Health Statistics (2019) About multiple cause of death, 1999–2019. https://wonder.cdc.gov/mcd-icd10.html. Accessed 14 Oct 2021
Chung MK, Eckhardt LL, Chen LY et al (2020) Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the American Heart Association. Circulation 141(16):e750–e772
Timp JF, Braekkan SK, Versteeg HH, Cannegieter SC (2013) Epidemiology of cancer-associated venous thrombosis. Blood 122(10):1712–1723
Prandoni P, Lensing AWA, Piccioli A et al (2002) Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 100(10):3484–3488
Melloni C, Shrader P, Carver J et al (2017) Management and outcomes of patients with atrial fibrillation and a history of cancer: the ORBIT-AF registry. Eur Heart J Qual Care Clin Outcomes 3(3):192–197
Fanola CL, Ruff CT, Murphy SA et al (2018) Efficacy and safety of edoxaban in patients with active malignancy and atrial fibrillation: analysis of the ENGAGE AF-TIMI 48 trial. J Am Heart Assoc 7(16):e008987
Joglar JA, Chung MK, Armbruster AL et al (2024) 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation 149(1):e1–e156
Sorigue M, Miljkovic MD (2019) Atrial fibrillation and stroke risk in patients with cancer: a primer for oncologists. J Oncol Pract 15(12):641–650
Atterman A, Friberg L, Asplund K, Engdahl J (2020) Net benefit of oral anticoagulants in patients with atrial fibrillation and active cancer: a nationwide cohort study. EP Europace 22(1):58–65
Fradley MG, Ellenberg K, Alomar M et al (2020) Patterns of anticoagulation use in patients with cancer with atrial fibrillation and/or atrial flutter. JACC Cardio Oncol 2(5):747–754
Malavasi VL, Fantecchi E, Gianolio L et al (2019) Atrial fibrillation in patients with active malignancy and use of anticoagulants: under-prescription but no adverse impact on all-cause mortality. Eur J Intern Med 59:27–33
O’Neal WT, Claxton JS, Sandesara PB et al (2018) Provider specialty, anticoagulation, and stroke risk in patients with atrial fibrillation and cancer. J Am Coll Cardiol 72(16):1913–1922
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137(2):263–272
Seelig J, Pisters R, Hemels ME, Huisman MV, Ten Cate H, Alings M (2019) When to withhold oral anticoagulation in atrial fibrillation - an overview of frequent clinical discussion topics. Vasc Health Risk Manag 15:399–408
Ardeshirrouhanifard S, An H, Goyal RK et al (2022) Use of oral anticoagulants among individuals with cancer and atrial fibrillation in the United States, 2010–2016. Pharmacother J Hum Pharmacol Drug Ther 42(5):375–386
Labrecque JA, Swanson SA (2017) Target trial emulation: teaching epidemiology and beyond. Eur J Epidemiol 32(6):473–475
Hernán MA, Robins JM (2016) Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol 183(8):758–764
Hernán MA, Sauer BC, Hernández-Díaz S, Platt R, Shrier I (2016) Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol 79:70–75
National Cancer Institute (2021) Overview of the surveillance, epidemiology, and end results (SEER) Program. https://seer.cancer.gov/about/overview.html. Accessed 27 Dec 2021
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF (2002) Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care 40(8 Suppl):Iv–3
Jensen PN, Johnson K, Floyd J, Heckbert SR, Carnahan R, Dublin S (2012) A systematic review of validated methods for identifying atrial fibrillation using administrative data. Pharmacoepidemiol Drug Saf 21(Suppl 1):141–147
Connolly SJ, Ezekowitz MD, Yusuf S et al (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361(12):1139–1151
Patel MR, Mahaffey KW, Garg J et al (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365(10):883–891
Hernán MA (2018) How to estimate the effect of treatment duration on survival outcomes using observational data. BMJ 360:k182–k182
Garg RK, Glazer NL, Wiggins KL et al (2011) Ascertainment of warfarin and aspirin use by medical record review compared with automated pharmacy data. Pharmacoepidemiol Drug Saf 20(3):313–316
Deitelzweig S, Keshishian AV, Zhang Y et al (2021) Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients with active Cancer. JACC Cardio Oncol 3(3):411–424
Thigpen JL, Dillon C, Forster KB et al (2015) Validity of international classification of disease codes to identify ischemic stroke and intracranial hemorrhage among individuals with associated diagnosis of atrial fibrillation. Circ Cardiovasc Qual Outcomes 8(1):8–14
Cunningham A, Stein CM, Chung CP, Daugherty JR, Smalley WE, Ray WA (2011) An automated database case definition for serious bleeding related to oral anticoagulant use. Pharmacoepidemiol Drug Saf 20(6):560–566
Shah S, Norby FL, Datta YH et al (2018) Comparative effectiveness of direct oral anticoagulants and warfarin in patients with cancer and atrial fibrillation. Blood Adv 2(3):200–209
National Cancer Institute. Division of Cancer Control and Population Sciences (DCCPS) (2023) NCI comorbidity index overview. https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.html. Accessed 10 Jan 2023
The Surveillance E (2023) Published, and end results (SEER) program,. observational research in oncology toolbox. https://seer.cancer.gov/oncologytoolbox/. Accessed 15 Feb 2023
Doll KM, Rademaker A, Sosa JA (2018) Practical guide to surgical data sets: surveillance, epidemiology, and end results (SEER) database. JAMA Surg 153(6):588–589
Iyengar V, Patell R, Ren S et al (2022) Bleeding risk in atrial fibrillation and thrombocytopenia: a propensity matched Cohort study. Blood 140(Supplement 1):345–346
Yeh YH, Chan YH, Chen SW et al (2022) Oral anticoagulant use for patients with atrial fibrillation with concomitant anemia and/or thrombocytopenia. Am J Med 135(8):e248–e256
Liu Y, De A (2015) Multiple imputation by fully conditional specification for dealing with missing data in a large epidemiologic study. Int J Stat Med Res 4(3):287–295
Cain LE, Saag MS, Petersen M et al (2016) Using observational data to emulate a randomized trial of dynamic treatment-switching strategies: an application to antiretroviral therapy. Int J Epidemiol 45(6):2038–2049
Park J, Cha MJ, Choi YJ et al (2019) Prognostic efficacy of platelet count in patients with nonvalvular atrial fibrillation. Heart Rhythm 16(2):197–203
Pastori D, Antonucci E, Violi F et al (2019) Thrombocytopenia and mortality risk in patients with atrial fibrillation: an analysis from the start registry. J Am Heart Association 8(21):e012596
**ao Y, Moodie EE, Abrahamowicz M (2013) Comparison of approaches to weight truncation for marginal structural Cox models. Epidemiol Methods 2(1):1–20
Chesnaye NC, Stel VS, Tripepi G et al (2022) An introduction to inverse probability of treatment weighting in observational research. Clin Kidney J 15(1):14–20
Leader A, Mendelson Cohen N, Afek S et al (2023) Arterial thromboembolism in patients with AF and CHA2DS2-VASc score 0–2 with and without Cancer. JACC Cardio Oncol 5(2):174–185
López-Fernández T (2023) CHA(2)DS(2)-VASc score in cardio-oncology: sharpening the rules. JACC Cardio Oncol 5(2):186–188
Yoshida K, Solomon DH, Kim SC (2015) Active-comparator design and new-user design in observational studies. Nat Rev Rheumatol 11(7):437–441
Duchesneau ED, Jackson BE, Webster-Clark M et al (2022) The timing, the treatment, the question: comparison of epidemiologic approaches to minimize Immortal Time bias in real-world data using a surgical oncology example. Cancer Epidemiol Biomarkers Prev 31(11):2079–2086
Pereira J, Phan T (2004) Management of bleeding in patients with advanced cancer. Oncologist 9(5):561–570
Navi BB, Reiner AS, Kamel H et al (2017) Risk of arterial thromboembolism in patients with Cancer. J Am Coll Cardiol 70(8):926–938
D’Souza M, Carlson N, Fosbøl E et al (2018) CHA2DS2-VASc score and risk of thromboembolism and bleeding in patients with atrial fibrillation and recent cancer. Eur J Prev Cardiol 25(6):651–658
Raposeiras-Roubin S, Abu-Assi E, Marchán A et al (2022) Validation of embolic and bleeding risk scores in patients with atrial fibrillation and cancer. Am J Cardiol 180:44–51
Matetic A, Mohamed MO, Essien UR et al (2023) Association between cancer, CHA2DS2VASc risk, and in-hospital ischaemic stroke in patients hospitalized for atrial fibrillation. Eur Heart J Qual Care Clin Outcomes 9(8):749–757
Bungo B, Chaudhury P, Arustamyan M et al (2022) Better prediction of stroke in atrial fibrillation with incorporation of cancer in CHA(2)DS(2)VASC score: CCHA(2)DS(2)VASC score. Int J Cardiol Heart Vasc 41:101072
January CT, Wann LS, Calkins H et al (2019) 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation 140(2):e125–e151
Lyon AR, López-Fernández T, Couch LS et al (2022) 2022 ESC guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J 43(41):4229–4361
Boriani G, Lee G, Parrini I et al (2021) Anticoagulation in patients with atrial fibrillation and active cancer: an international survey on patient management. Eur J Prev Cardiol 28(6):611–621
National Cancer Institute. Division of Cancer Control and Population Sciences (2023) Measures that are limited or not available in the data. https://healthcaredelivery.cancer.gov/seermedicare/considerations/measures.html. Accessed 13 June 2023
Cereda A, Lucreziotti S, Franchina AG et al (2023) Systematic review and meta-analysis of oral anticoagulant therapy in atrial fibrillation cancer patients. Cancers. https://doi.org/10.3390/cancers15092574
Mehta HB, An H, Ardeshirrouhanifard S, Raji MA, Alexander GC, Segal JB (2022) Comparative effectiveness and safety of direct oral anticoagulants versus warfarin among adults with cancer and atrial fibrillation. Circ Cardiovasc Qual Outcomes 15(12):e008951
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 34(28):3661–3679
Cain LE, Robins JM, Lanoy E, Logan R, Costagliola D, Hernán MA (2010) When to start treatment? A systematic approach to the comparison of dynamic regimes using observational data. Int J Biostat 6(2):18
Adelborg K, Corraini P, Darvalics B et al (2019) Risk of thromboembolic and bleeding outcomes following hematological cancers: a Danish population-based cohort study. J Thromb Haemost 17(8):1305–1318
Del Prete C, Kim T, Lansigan F, Shatzel J, Friedman H (2018) The epidemiology and clinical associations of stroke in patients with acute myeloid leukemia: a review of 10,972 admissions from the 2012 National Inpatient Sample. Clin Lymphoma Myeloma Leuk 18(1):74-77e71
Dagan N, Barda N, Kepten E et al (2021) BNT162b2 mRNA Covid-19 vaccine in a Nationwide Mass Vaccination setting. N Engl J Med 384(15):1412–1423
Gupta S, Wang W, Hayek SS et al (2021) Association between early treatment with tocilizumab and mortality among critically ill patients with COVID-19. JAMA Intern Med 181(1):41–51
Cho K, Keithly SC, Kurgansky KE et al (2021) Early convalescent plasma therapy and mortality among US veterans hospitalized with nonsevere COVID-19: an observational analysis emulating a target trial. J Infect Dis 224(6):967–975
Acknowledgements
This study used the linked the SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Centers for Medicare & Medicaid Services, Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database. The collection of cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Sect. 103885; Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries, under cooperative agreement 1NU58DP007156; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201800032I awarded to the University of California, San Francisco, contract HHSN261201800015I awarded to the University of Southern California, and contract HHSN261201800009I awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and do not necessarily reflect the opinions of the State of California, Department of Public Health, the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
BT: Conceptualization; Data curation; Formal analysis; Methodology; Writing—original draft. BF: Methodology; Validation; Writing—review and editing. EC: Methodology; Validation; Writing—review and editing. JZ: Methodology; Validation; Writing—review and editing. LH: Methodology; Validation; Writing—review and editing. JQ: Conceptualization; Methodology; Supervision; Validation; Writing—review and editing
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to report for all authors.
Ethical approval
The study was granted exemption by the Auburn University institutional review board (IRB) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Truong, B., Hornsby, L., Fox, B. et al. Benefit and risk of oral anticoagulant initiation strategies in patients with atrial fibrillation and cancer: a target trial emulation using the SEER-Medicare database. J Thromb Thrombolysis 57, 638–649 (2024). https://doi.org/10.1007/s11239-024-02958-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-024-02958-3