Abstract
The aim of this study is to clarify whether health-care inequality in Japan widens during a depression, even though Japan has a universal health-care system. To this end, we investigate the time-series fluctuations in health-care expenditure inequalities in Japan for the period 2008–2017, which includes the period during which the global financial crisis affected Japan. We construct an economy-wide inequality index comparing the actual health-care expenditure at various income levels (low, middle and high) against the estimated health-care needs. The findings of the study are as follows. First, the rich (the top 20% income class) spend far more than their estimated needs on health care, whereas the poor (bottom 20%) spend far less. Second, during the global financial crisis, health-care inequality especially among the working generation became greater in Japan, mainly because not only the low-income class but also the middle-income class (the bottom 30–60%) was unable to pay for health care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The Japanese health-care system provides universal coverage through compulsory public health insurance. The system provides treatments and drugs at relatively low, centrally controlled rates (Ikegami et al. 2011, Murray 2011). Patients do not make out-of-pocket payments beyond monthly upper limits, which are predetermined based on income and age. While patients usually pay 30% of reimbursement prices, a reduced co-payment rate of 10% or 20% is available for low-income patients aged 70 years and above. Lower insurance premiums are applied to those with low incomes, including retired persons aged 60 years and above based on the ability-to-pay principle in Japan’s public health insurance system. With the multiplicity of the health-care system, the main goal of Japan’s universal coverage is equitable health care. However, severe economic depression can lead to an unequal distribution of health care, with low-income patients unable to pay for it. In this study, we measure health-care inequality in Japan in the 2008–2017 period, which includes the global financial crisis.
We develop a method based on Van Doorslaer et al. (2000) to measure the difference between actual health-care utilization and the estimated health-care needs for each income level. Thus, we develop an economy-wide health-care inequality index. Related studies that employ similar methods are Van Doorslaer et al. (1997, 2004, 2006) for OECD countries, Morris et al. (2005) for England, Allin et al. (2010) for Canada and Ohkusa and Honda (2003) and Watanabe and Hashimoto (2012) for Japan.
The contributions of this paper are twofold. First, we employ more detailed Japanese data than the previous studies (Ohkusa and Honda (2003), and Watanabe and Hashimoto (2012)). Our data source, the Japan Household Panel Survey (JHPS), is a yearly survey that includes health-care expenditure and is more comprehensive than the data sources used in previous studies. Second, we analyse the relationship between economic depression and health-care inequality. Because our sample period includes the global financial crisis, we can demonstrate how the business cycle affects health-care inequality under a universal health-care system. This has been an open question in the existing literature (Fujita et al. 2016, Fukuda et al. 2007, Hanibuchi et al. 2016, Hiyoshi et al. 2014, Kanchanachitra and Tangcharoensathien 2017, Kondo et al. 2008, Macinko et al. 2003, Nakaya & Ito 2020, Sarah et al. 2015, and Xu 2013).
2 Materials and Methods
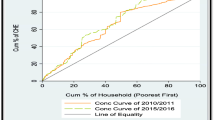
For the empirical method, we follow Van Doorslaer et al. (2000). Ohkusa and Honda (2003) and Watanabe and Hashimoto (2012) also apply this method using Japanese data. They calculate the inequality index based on two concentration curves: health-care utilization LM(R) and estimated health-care needs LN(R), where R denotes the cumulative proportion of the population ranked by income (or assets for the elderly). The two curves are represented in Fig. 1, where the horizontal line is R and the vertical line is the cumulative proportion of health-care expenditure. An important finding of this study is that LM(R) is below the diagonal line and LN(R) is above it, which indicates that the poor (rich) have low (high) health-care utilization despite high (low) needs (Van Doorslaer et al., 2004).
The health-care utilization concentration index is calculated as:
This measures two times the area between LM(R) and the diagonal line. The health-care needs concentration index is calculated as:
This measures two times the area between LN(R) and the diagonal line.
The measure of inequality compares the difference between LM and LN. If LM = LN for all R, then no inequality exists because all patients receive the same amount of health care as their estimated needs. However, if the poor spend below their needs and the rich spend above theirs, then the LM(R) curve is located below the diagonal line, whereas the LN(R) curve is located above it, increasing the difference between LM and LN. Therefore, the inequality index HIWV is defined as twice the area between the two curves, calculated as:
Thus, the larger the HIWV, the more severe the health-care inequality.
The inequality index HIWV can be constructed by a simple method (Van Doorslaer et al. (2000)) using data on the health-care utilization and needs of each person. In our analysis, health-care utilization is measured by the actual health-care expenditures and needs using our regressions. First, the data on actual health-care expenditure are taken from the JHPS, which reports the health-care expenditure (out-of-pocket expenditure) of each family head and his/her partner. Second, the health-care needs are estimated by regressions on the data, with the health-care expenditure as the dependent variable. The independent variables are sex, age, a cross-term for sex and age, the frequency of smoking, the frequency of drinking, self-assessment of health, experienced symptoms and the experience of medical treatment and hospitalization. The variables used are explained in Table 1.
Tables 2 and 3 show the descriptive statistics of the variables used for age 20–59 and over 60, respectively. We use a fixed-effect estimator on the panel data. The fitted value (prediction value) is regarded as the health-care needs of each person in each year. Based on the health-care expenditure and needs data, we can draw LN(R) and LM(R) curves for each year.
For the regression, we divide the samples into two categories: those aged 20–59 years, and those aged over 60 years. This is because of possible differences in co-payment rates and insurance premiums between the two age groups, as the elderly (over 60 years) are offered more generous, reduced co-payment rates and lower insurance premiums, as mentioned above. R denotes the cumulative proportion of the population ranked by income for the younger group (20–59 years), whereas it denotes the cumulative proportion of the population ranked by assets for those over 60 years, as this group includes many retired people.
We use JHPS surveys for 2009 (6911 households) to JHPS 2018 (3044 households). Our sample period is 2008–2017, during which the global financial crisis affected Japan while its health-care system did not greatly change. The JHPS contains data on households’ income, asset, consumption, work, assets, health and environment. It also includes individual data (for the household head and his/her partner), including income, asset, health and work. One important advantage of the JHPS is that it reports individuals’ health-care expenditure. By using data on health-care expenditure, we can capture the health-care utilization and needs more accurately.
3 Results
First, the results of the regression for health-care needs (i.e., LN(R) curve) are shown in Tables 4 and 5. For individuals aged 20–59 years, self-assessment of health, the frequency of smoking, the frequency of drinking and medical treatment/hospitalized are significant variables that determine health-care needs. For those over 60 years, self-assessment of health, drinking, felt reluctant to meet other people and medical treatment/hospitalized are significant. The fitted values of the regression give the LN(R) curves. Next, the health-care utilization LM(R) is constructed based on actual health-care expenditure data.
Given the LN(R) curve and LM(R) curve for those aged 20–59 years, we take the difference between the two curves and depict it in Fig. 2. The horizontal line is R (the cumulative proportion of population ranked by income), and the vertical line is the difference between the two concentration curves in Fig. 1. In Fig. 2, if the slope of the graph is downward at a certain income level, it indicates that health-care needs are higher than the actual health-care expenditure at that income level compared with the other income levels. Conversely, if the slope of the graph is upward at a certain income level, it means that health-care needs do not exceed the actual health-care expenditure at that income level by as much as they do at other income levels, or that the health-care needs are less than the actual health-care expenditure at that income level. If the slope is at its most negative at a certain income level, this implies that needs exceed expenditure largely at the income level compared with all other income levels. Note that the bottom of the U-shaped graph does not have this meaning. By construction, the value of the graph starts and ends with zero because both LM(R) and LN(R) are concentration curves and they take the same values at each end, as described in Fig. 1. Figure 3 describes the same relationship for those over 60 years.
Regarding Figs. 2 and 3, we make four observations. First, the graphs are approximately U-shaped for many years of our sample period. Many of the graphs tend to decrease until they reach the middle-income/asset level and then start increasing thereafter. This indicates that health-care needs tend to exceed actual health-care expenditures below the middle-income/asset level, whereas this is not the case above the middle-income/asset level. It follows that in Japan, despite the universal health-care system, the poor generally spend less than their needs, whereas this is the reverse for the rich.
Second, comparing Figs. 2 and 3, in general, the graphs involve a larger U-shape for the working age group than those for the elderly. This implies that inequality is generally larger in the working age group.
Third, in Fig. 2, the curves at income levels around the top 20% are the most sharply upward slo**, which implies that the 20–59-years age group in this income bracket spend far more on health care than justified by their needs. In Fig. 3, the curves are moderately upward slo**, which implies that individuals over the top 50% asset level in the age group of over 60 years old spend slightly more than their needs. Conversely, both in Figs. 2 and 3, at income/asset levels around the bottom 20%, the curves are the most sharply downward slo**, implying that the expenditure of the individuals in this income/asset bracket is far below their needs.
Fourth and finally, regarding the time-series trend in Figs. 2 and 3, the graphs are decreasing around the bottom 30%–60% income/asset levels in 2010 and 2011 (i.e., the global financial crisis period), although they are increasing in 2008 and 2009. Note that this is observed for both age groups that we study. On the other hand, for the 20–59-years age group, the graphs start increasing at the bottom 40% income level in 2012 and 2013 (i.e., during the recovery period). This implies that even the middle-income class group is forced to reduce the health-care utilization during the global financial crisis. From a different perspective, for the 20–59 years age group, the graphs increase sharply around the middle-income level in 2012 and during the period 2014–2017. The latter two trends are not observed for the group aged over 60 years.
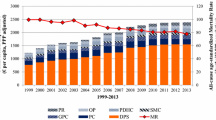
Then, the inequality index HIWV is calculated as twice the area between the two curves LM(R) and LN(R). Figures 4 shows the HIWV (red line) and the average household equivalence-adjusted income for each year (blue line) for those aged 20–59 years. Figure 5 is an analogous figure for those over 60 years old, where the blue line is the average household equivalence-adjusted assets for each year. For both age groups, the average household equivalence-adjusted income/assets are calculated using JHPS.
4 Discussion
The implications of our results are as follows.
-
(1)
The rich (the top 20% income/asset class) spend far above their needs on health care, whereas the poor (bottom 20%) spend far below their needs. This is especially noticeable for the working age group.
-
(2)
During the global financial crisis (2010–2011), the bottom 30–60% income/asset classes began to spend below their needs, resulting in large inequality.
-
(3)
Inequality is more severe for the working age group than for those 60 years old and above.
-
(4)
During the other sample periods, there seems to be no relationship between health-care inequality and the business cycles.
Cleeren et al. (2015) report that the effects of business cycles on health care vary across countries and situations. We found that in the global financial crisis period, the inequality became larger for both the 20–59-years age group and those over 60 years old. Our results show that in 2010–2011, the slopes of the graphs in Figs. 2 and 3 became negative for the middle-income/asset class (30–60%), although prior to the crisis, in 2008–2009, it was positive. This means that the middle-income/asset class began to spend below their needs, resulting in a large value for the inequality index. During the depression, household income decreased, and not only the low-income but also the middle-income class became unable to pay for health care, which increased health-care inequality. This is also consistent with Kondo et al. (2008) that shows an economic recession increased health disparity between the top and middle working groups in men.
Next, the values of the HIWV are higher for 20–59-years age group than for those 60 years and above. There are several explanations for this. First, for those over 60 years old, the income/asset shock caused by the depression was relatively small because the majority of them were already retired. Second, healthcare for this group is more critical, involving life-and-death decisions, than it is for the younger, 20–59-years age group. This is consistent with the previous literature: Watanabe and Hashimoto (2012) also show that the inequality level is smaller for retired people than for working people, despite employing a different data source to ours. Watanabe and Hashimoto (2012) employ the Japan Comprehensive Survey of Living Conditions, which reports only whether each person has visited a physician more than once in a year and, thus, health-care utilization takes a value of either zero or one. By contrast, our database, the JHPS, reports individuals’ health-care expenditure, and is more detailed than that utilized by Watanabe and Hashimoto (2012). Based on our more detailed data source, we confirm that the inequality among the retired generation is smaller than among the working generation.
In summary, we measure the health-care inequality index from 2008 to 2017 and investigate how the global financial crisis affected health inequality in Japan. First, the health-care expenditure of the lowest income class (bottom 20%) is below such individuals’ needs during these years, whereas that of the highest income class (top 20%) is far above such individuals’ needs. Second, in the 2010–2011 depression, health-care inequality among the working generation widened as health-care expenditure fell short of the needs of even the middle-income class.
References
Allin, S., Grignon, M., & Le Grand, J. (2010). Subjective unmet need and utilization of health care services in Canada: What are the equity implications? Social Science and Medicine, 70(3), 465–472. https://doi.org/10.1016/j.socscimed.2009.10.027
Burgard, S. A., & Kalousova, L. (2015). Effects of the great recession: health and well-being. Annual Review of Sociology, 41(1), 181–201. https://doi.org/10.1146/annurev-soc-073014-112204.
Cleeren, K., Lamey, L., Meyer, J., & Ruyter, K. (2015). How business cycles affect the healthcare sector: A cross-country investigation. Health Economics, 25(7), 787–800. https://doi.org/10.1002/hec.3187
Fujita, M., Sato, Y., Nagashima, K., Takahashi, S., Hata, A., & Virgili, G. (2016) Income related inequality of health care access in Japan: A retrospective cohort study. PLOS ONE, 11(3), e0151690. https://doi.org/10.1371/journal.pone.0151690
Fukuda, Y., Nakano, H., Yahata, Y., & Imai, H. (2007). Are health inequalities increasing in Japan? The trends of 1955 to 2000. Bioscience Trends, 1(1), 38–42.
Hanibuchi, T., Nakaya, T., & Honjo, K. (2016). Trends in socioeconomic inequalities in self-rated health smoking and physical activity of Japanese adults from 2000 to 2010. SSM - Population Health, 2, 662–673. https://doi.org/10.1016/j.ssmph.2016.09.002
Hiyoshi, A., Fukuda, Y., Shipley, M.J., & Brunner, E.J. (2014). Health inequalities in Japan: The role of material psychosocial social relational and behavioural factors. Social Science & Medicine, 104, 201–209. https://doi.org/10.1016/j.socscimed.2013.12.028
Ikegami, N., Yoo, B. K., Hashimoto, H., Matsumoto, M., Ogata, H., Babazono, A., Watanabe, R., Shibuya, K., Yang, B. M., Reich, M. R., & Kobayashi, Y. (2011). Japanese universal health coverage: Evolution, achievements and challenges. The Lancet, 378(9796), 1106–1115. https://doi.org/10.1016/S0140-6736(11)60828-3
Kanchanachitra, C., & Tangcharoensathien, V. (2017). Health inequality across prefectures in Japan. The Lancet, 390(10101), 1471–1473. https://doi.org/10.1016/S0140-6736(17)31792-0.
Kondo, N., Subramanian, S. V., Kawachi, I., Takeda, Y., & Yamagata, Z. (2008). Economic recession and health inequalities in Japan: analysis with a national sample 1986–2001. Journal of Epidemiology and Community Health, 62(10), 869–875. https://doi.org/10.1136/jech.2007.070334.
Macinko, J., Starfield, B., & Shi, L. (2003). The contribution of primary care systems to health outcomes within organization for economic cooperation and development (OECD) countries 1970–1998. Health Services Research, 38(3), 831–865. https://doi.org/10.1111/1475-6773.00149.
Morris, S., Sutton, M., & Gravelle, H. (2005). Inequity and inequality in the use of health care in England: An empirical investigation. Social Science & Medicine, 60(6), 1251–1266. https://doi.org/10.1016/j.socscimed.2004.07.016
Murray, C. J. L. (2011). Why is Japanese life expectancy so high? The Lancet, 378(9797), 1124–1125. https://doi.org/10.1016/S0140-6736(11)61221-X.
Nakaya, T., & Ito, Y. (eds). (2020) The atlas of health inequalities in Japan. Springer International Publishing. https://doi.org/10.1007/978-3-030-22707-4.
Ohkusa, Y., & Honda, C. (2003). Horizontal inequality in health care utilization in Japan. Health Care Management Science, 6(3), 189–196. https://doi.org/10.1023/A:1024492224790
Van Doorslaer, E., Masseria, C., & Koolman, X. (2006). Inequalities in access to medical care by income in developed countries. Canadian Medical Association Journal, 174(2), 177–183. https://doi.org/10.1503/cmaj.050584
Van Doorslaer, E., Wagstaff, A., Bleichrodt, H., Colonge, S., Gerdtham, U. G., Gerfin, M., Geurts, J., Gross, L., Häkkinen, U., Leu, R. E., O’Donnell, O., Propper, C., Puffer, F., Rodríguez, M., Sundberg, G., & Winkelhake, O. (1997). Income-related inequalities in health: Some international comparisons. Journal of Health Economics, 16(1), 93–112. https://doi.org/10.1016/S0167-6296(96)00532-2
Van Doorslaer, E., Masseria C., & the OECD Health Equity Research Group Members (2004). Income-related inequality in the use of medical care in 21 OECD countries. In OECD (Ed.), Towards high-performing health systems: Policy Studies (pp.109–166). OECD.
Van Doorslaer, E., Wagstaff, A., Van der Burg, H., et al. (2000). Equity in the delivery of health care in Europe and the US. Journal of Health Economics, 19(5), 553–583. https://doi.org/10.1016/S0167-6296(00)00050-3
Watanabe, R., & Hashimoto, H. (2012). Horizontal inequality in healthcare access under the universal coverage in Japan; 1986–2007. Social Science and Medicine, 75, 1372–1378. https://doi.org/10.1016/j.socscimed.2012.06.006.
Xu, X. (2013). The business cycle and health behaviors. Social Science and Medicine, 77, 126–136. https://doi.org/10.1016/j.socscimed.2012.11.016.
Acknowledgements
This paper was supported by JSPS KAKENHI Grant Number 16K17132 and 18K01666. In this paper, we use panel data from the Japan Household Panel Survey compiled by the Panel Data Research Center at Keio University https://www.pdrc.keio.ac.jp/en/. We are grateful to the center. Needless to say, any remaining errors are the responsibility of the authors.
Funding
This work was supported by JSPS KAKENHI Grant Number 16K17132 and 18K01666.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial conflicts of interest to disclose concerning the paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakoda, S., Tamura, M. & Wakutsu, N. The Global Financial Crisis and Healthcare Inequality in Japan. Soc Indic Res 161, 273–286 (2022). https://doi.org/10.1007/s11205-021-02823-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-021-02823-3