Abstract
This paper focuses on acute-care local public hospitals in Japan and evaluates differences in hospital technology, as reflected in the productivity of labor specialties, physical capital and medicines, and in the impact of teaching activities and other hospital characteristics on hospital output. We use panel data quantile regressions with fixed effects to model a range of technologies for the multi-product output function of hospitals. The analysis reveals technological heterogeneity across high-output and low-output hospitals. We discover inexpedient labor/capital and labor/medicines mix, and vast opportunities for cost savings. The results contribute to scant empirical literature on variation in the hospital production.



Similar content being viewed by others
Data availability
The links to all publicly available datasets used in the current paper and the list of variables are provided in the appendices. The data on financial information of Japanese local public hospitals (Annual Surveys of Local Public Enterprises. Hospitals) have been publicly available on the website of the Japanese Ministry of Internal Affairs and Communications on a rolling basis for most recent years (2014 onwards as of July 2021). The data for 2002–2013 are publicly available through the Web Archiving Project of the National Diet Library (Tokyo) https://warp.da.ndl.go.jp/?_lang=en. Data for earlier years can be obtained from the Statistics Department of the Japanese Ministry of Internal Affairs and Communications upon request: https://www.stat.go.jp/library/faq/faq05/faq05b06.html. The publicly available data used in the current paper can be requested from the corresponding author.
Notes
Specifically, in this paper we use the fact that \({Q}_{\tau }(\ln y| x)=\ln ({Q}_{\tau }(y| x))\), where Qτ is the conditional τth quantile of the dependent variable y under fixed x.
The Galvao and Kato (2016) smoothing technique for reducing the asymptotic bias of the estimator is applicable for a more restricted model with quantile-independent fixed effects: it is used in the Chen and Huo (2020) estimator. Note that a different approach for creating a quantile-independent fixed effects estimator, which could apply to short panels, was proposed by Canay (2011), but the estimator was shown to have asymptotic bias (Besstremyannaya and Golovan 2019).
Galvao and Kato (2016) do not touch on the choice of the bandwidth. So our estimations follow the methodology of Koenker (2005), section 4.10.1 for computing the asymptotic covariance matrix, which specifies the bandwidth as h = κ(Φ(τ + h1) − Φ(τ − h1)). We take h1 from Bofinger (1975) and κ from Koenker (2005).
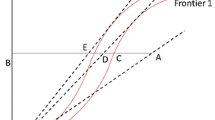
An alternative approach is the use of normalization that requires homogeneity of degree 1 in inputs. Consideration of an input distance function under this approach leads to very similar results, as both approaches approximate the same production possibility frontier.
The numerical values of the estimated coefficients depend on the order of outputs, but qualitative results concerning the typology of technologies and other findings related to the analysis with the output distance function hold regardless of the order of outputs.
The use of the translog function may cause a multicollinearity problem. Our analysis deals with the panel data regression with fixed effects, so to assess the problem we compute correlation coefficients after the within-group transformation: the subtraction of the per-hospital mean from each regressor. The values of the correlation coefficients do not exceed 0.48.
The approach assumes that the use of an electronic data system has a multiplicative effect on production. A more detailed analysis requires the inclusion of interaction terms of the variable and each input (as well as the products of pairs of inputs). However, it substantially increases the degrees of freedom and so the approach becomes unfeasible given the size of the sample available for estimations.
The asymptotic inference works poorly for extreme quantiles outside the (0.2, 0.8) range, as it is shown in Chernozhukov (2005).
Additionally, we compute the pseudo R2 statistic, which compares the full model with the model with only a constant term (the statistic is employed for evaluating the fit of pooled models in the quantile regression approach and is calculated solely for reference purposes).
The general linear hypothesis \({{{{\rm{H}}}}}_{0}:R[{{{\boldsymbol{\beta }}}}{^\prime} (\tau ),{{{\boldsymbol{\beta }}}}{^\prime} (\tau {^\prime} )]{^\prime} =r\) can be evaluated using the Wald statistic (Koenker 2005; section 3.3): \(W=(R[{{{\boldsymbol{\beta }}}}{^\prime} (\tau ),{{{\boldsymbol{\beta }}}}{^\prime} (\tau {^\prime} )]{^\prime} -r){^\prime} {(R\hat{VR}{^\prime} )}^{-1}(R[{{{\boldsymbol{\beta }}}}{^\prime} (\tau ),{{{\boldsymbol{\beta }}}}{^\prime} (\tau {^\prime} )]{^\prime} -r)\), where the matrix \(\hat{V}\) is constructed by estimating the covariance function of the stochastic process β(τ): \(\hat{V}=\left(\begin{array}{ll}\hat{V}(\tau ,\tau )&\hat{V}(\tau ,\tau {\prime} )\\ \hat{V}(\tau {\prime} ,\tau )&\hat{V}(\tau {\prime} ,\tau {\prime} )\end{array}\right)\).
Nonparametric methods construct a hull of observations (Charnes et al. 1978) and hence consider the observations on the constructed frontier as fully efficient, do not account for measurement error, are sensitive to outliers and require large samples estimations. An alternative parametric method, that of stochastic frontier analysis, imposes distributional or other restrictions on the error term (Aigner et al. 1977). See the debate in the Journal of Health Economics 1994:13(3).
Japanese per diem variant of the prospective payment system, based on diagnosis-procedure combinations, DPCs.
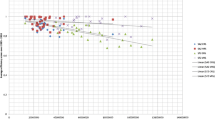
We focus on a group of hospitals, which may comprise the whole sample or a certain category of hospitals in terms of the number of beds: small, medium-sized, and large.
This residual is the log of total factor productivity.
The boundary condition in the cost minimization problem is essentially the equation for the production function and it ensures the production of a given amount of output. It should be noted that the estimated log of the translog production function is not globally quasiconvex, so the optimum allocation of inputs in the cost minimization problem with translog production function does not exist (Boisvert 1982). Accordingly, the approximation of the translog production function is employed in the cost minimization problem: we use the Cobb–Douglas production function which has the returns to each input equal to the mean factor returns estimated under the translog model.
The prefecture grants the status of designated hospital and financial support of 10,000 yen per each admission to a local hospital that satisfies the following requirements: (1) has over 200 beds; (2) the share of patients referred from other facilities is over 60–80%; (3) shares its beds and expensive equipment (e.g., MRI and CT scanner) with other hospitals; (4) trains local healthcare officials; and (5) has emergency status.
The standard financial need is the product of unit cost of public services, the demand for public services and adjustment coefficient (which accounts for socio-economic and geographic factors), see https://www.soumu.go.jp/main_content/000363663.pdf.
The number of hospitals is steadily decreasing since 2003 owing to merging of municipalities and restructuring of hospitals.
Commonly, hospitalization in Japan lasts no less than a week, so shorter hospital stays may reflect only preliminary diagnostics or an anticipated transfer to specialized hospital facility (Nawata et al. 2006).
Hospital stays corresponding to long-term care.
We choose 0.1 as the minimal bound for bed occupancy in order for a hospital to be considered as providing inpatient care. Mean bed occupancy in our sample is 0.75.
Takatsuka and Nishimura (2008) propose reconstructing the arithmetic mean of the number of admissions and discharges using the MHLW definitions of average length of stay (available for acute-care beds only) and bed occupancy.
Our data show that pairwise correlation coefficients between the logarithms of the numbers of physicians, nurses and other staff—after subtraction of hospital means from each variable as we deal with panel-data fixed effects regression—are in a range of 0.33–0.48 in various years.
According to Ikegami and Buchan (2014), there are certain differences in requirements for qualifying as a registered nurse or a licensed practical nurse (3 years of medical education and a national exam versus 2 years of education and a prefectural exam), but the skills of the two types are very similar overall.
This composite group of all non-doctor and non-nurse labor specialties is used in the analysis owing to the size of our sample and the total count of estimated parameters: the inclusion of technicians, administrative personnel and other workers as separate inputs would considerably increase the number of covariates due to the appearance of numerous interaction terms.
The cost of medicines per se constitutes about 70% of all medical materials at local public hospitals, and the correlation between cost of medicines and cost of all medical materials is 0.96.
Although there is a slight fall in 2003.
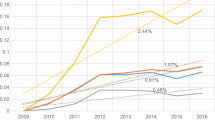
See Supplementary material: productivity of physicians (Supplementary Tables S26 and S27), other staff (Supplementary Tables S32 and S33), capital (Supplementary Tables S38 and S39), medicines (Supplementary Tables S41 and S42). We use the criterion that the differences across the values in adjacent years were observed at least 7 pairs of years out of 19. This way the differences across annual values cannot be attributed to random variation.
The only exception is one value of the highest output quantile for two input pairs: total labor and physical capital; and physical capital and medicines.
Observed in all output quantiles with the exception of τ = 0.8
The choice of only three groups is justified by the desire to have a sufficient number of observations in each group and to make the size of groups comparable in terms of number of hospitals.
Additionally, Becker and Murphy (1994) state that the extent of labor specialization is explained by the balance between higher productivity (owing to the division of labor) and increased costs of labor coordination.
References
Acemoglu D, Autor D (2011) Skills, tasks and technologies: implications for employment and earnings. In Card D, Ashenfelter O (eds.) Handbook of labor economics, vol 4, Part B. Elsevier, Amsterdam, p 1043–1171
Acemoglu D, Finkelstein A (2008) Input and technology choices in regulated industries: Evidence from the health care sector. J Political Econ 116:837–880
Aigner D, Lovell C, Schmidt P (1977) Formulation and estimation of stochastic frontier production function models. J Econom 6:21–37
Baumgardner JR (1988) The division of labor, local markets, and worker organization. J Political Econ 96:509–527
Baumgardner JR (1988) Physicians’ services and the division of labor across local markets. J Political Econ 96:948–982
Becker GS, Murphy KM (1994) The division of labor, coordination costs, and knowledge. In Becker GS (ed.) Human capital: a theoretical and empirical analysis with special reference to education, 3rd ed. The University of Chicago Press, p 299–322
Bernini C, Freo M, Gardini A (2004) Quantile estimation of production function. Empir Econ 29:373–381
Besstremyannaya G (2013) The impact of Japanese hospital financing reform on hospital efficiency. Jpn Econ Rev 64:337–362
Besstremyannaya G, Golovan S (2019) Reconsideration of a simple approach to quantile regression for panel data. Econom J 22:292–308
Biørn E, Hagen TP, Iversen T, Magnussen J (2003) The effect of activity-based financing on hospital efficiency: A panel data analysis of DEA efficiency scores 1992–2000. Health Care Manag Sci 6:271–283
Blank JLT, Valdmanis VG (2008) Evaluating hospital policy and performance: Contributions from hospital policy and productivity research, Amsterdam: Elsevier JA
Blank JLT, Valdmanis VG (2010) Environmental factors and productivity of Dutch hospitals: A semi-parametric approach. Health Care Manag Sci 13:27–34
Blank JLT, van Hulst BL (2017) Balancing the health workforce: Breaking down overall technical change into factor technical change for labour: An empirical application to the Dutch hospital industry. Hum Resour Health 15:1–14
Bloom N et al. (2017) What drives differences in management? Working Paper, National Bureau of Economic Research
Bloom N et al. (2019) What drives differences in management practices? Am Econ Rev 109:1648–83
Bloom N, Dorgan S, Dowdy J, Van Reenen J (2007) Management practice and productivity: Why they matter. Working Paper, McKinsey&Company, LSE. https://cep.lse.ac.uk/management/Management_Practice_and_Productivity.pdf
Bloom N, Propper C, Seiler S, Van Reenen J (2015) The impact of competition on management quality: Evidence from public hospitals. Rev Econ Stud 82:457–489
Bloom N, Sadun R, Van Reenen J (2014) Does management matter in healthcare? In Chandra A, Cutler D, Huckman R, Martinez E (eds) Hospital organization and productivity. NBER Conference. https://prod-edxapp.edx-cdn.org/assets/courseware/v1/dd428dcc44daa742d5c5c91aeb9dcd21/c4x/HarvardX/PH555x/asset/Management_Healthcare_June2014.pdf
Bofinger E (1975) Optimal condensation of distributions and optimal spacing of order statistics. J Am Stat Assoc 70:151–154
Boisvert RN (1982) The translog production function: Its properties, its several interpretations and estimation problems. Working Paper, Charles H. Dyson School of Applied Economics and Management, Cornell University
Campbell J, Ikegami N (1998) The art of balance in health policy. Maintaining Japan’s low-cost, egalitarian system. Cambridge University Press, Cambridge
Canay I (2011) A simple approach to quantile regression for panel data. Econom J 14:368–386
Charnes A, Cooper W, Rhodes E (1978) Measuring the efficiency of decision making units. Eur J Oper Res 2:429–444
Chen L, Huo Y (2020) A simple estimator for quantile panel data models using smoothed quantile regressions. Econom J 24:247–263
Chernozhukov V (2005) Extremal quantile regression. Ann Stat 33:806–839
Chiang AC (1984) Fundamental methods of mathematical economics. McGraw-Hill
Christensen EW (2004) Scale and scope economies in nursing homes: A quantile regression approach. Health Econ 13:363–377
Cleverley WO, Harvey RK (1992) Competitive strategy for successful hospital management. J Healthc Manag 37:53
Coelli T, Perelman S (1999) A comparison of parametric and non-parametric distance functions: With application to European railways. Eur J Oper Res 117:326–339
Coelli T, Perelman S (2000) Technical efficiency of European railways: A distance function approach. Appl Econ 32:1967–1976
Dhaene G, Jochmans K (2015) Split-panel jackknife estimation of fixed-effect models. Rev Econ Stud 82:991–1030
Doi S, Ryubori M, Umetsuna K, Hayashi S (2005) DPC dounyu-ga oyobosu kyuuseikibyouin-no eikyou-to kongo-no kadai [The impact of DPC introduction on emergency hospitals and future issues. in Japanese]. Nihon Byouin Gakkaishi 52:72–79
Dorgan S et al. (2010) Management in healthcare: Why good practice really matters. Working Paper, McKinsey&Company, LSE. https://cep.lse.ac.uk/textonly/_new/research/productivity/management/PDF/Management_in_Healthcare_Report.pdf
Feldstein M (1974) Econometric studies of health economics., in Frontiers of Quantitative Econometrics, vol. 2, eds. Intriligator M, Kendrick D, Amsteram: North-Holland, 377–434
Ferrier GD, Valdmanis V (1996) Rural hospital performance and its correlates. J Product Anal 7:63–80
Fujii A (2001) Stochastic cost frontier and cost inefficiency of Japanese hospitals: A panel data analysis. Appl Econ Lett 8:801–812
Galvao AF, Kato K (2016) Smoothed quantile regression for panel data. J Econom 193:92–112
Hames DS (1991) Productivity-enhancing work innovations: Remedies for what ails hospitals? J Healthc Manag 36:545
Harding M, Lamarche C (2014) Estimating and testing a quantile regression model with interactive effects. J Econom 178:101–113
Harding M, Lamarche C (2016) Penalized quantile regression with semiparametric correlated effects: An application with heterogeneous preferences. J Appl Econ 32:342–358
Hendricks W, Koenker R (1992) Hierarchical spline models for conditional quantiles and the demand for electricity. J Am Stat Assoc 87:58–68
Higuchi S (2010) Chuusho jichitai byouin-no genjo-to kadai (current situation and tasks for small and medium local public hospitals). J Jpn Hosp Assoc 5:95–101
Hisamichi S (2010) Byouin keiei koto hajime. Byouin jigyou kanri-no tachiba kara. (Starting hospital management. Point of view of a hospital manager). J Jpn Hosp Assoc 2:98–119
Hollingsworth B (2008) The measurement of efficiency and productivity of health care delivery. Health Econ 17:1107–1128
Hollinsworth B, Peacock S (2008) Efficiency measurement in health and health care. Routledge
Hsu A, Dass AR, Berta W, Coyte P, Laporte A (2017) Efficiency estimation with panel quantile regression: An application using longitudinal data from nursing homes in Ontario, Canada. Working Paper No. 170003. Canadian Centre for Health Economics
Ikegami N (ed.) (2014) Universal health coverage for inclusive and sustainable development: Lessons from Japan. The World Bank
Ikegami N, Buchan J (2014) Licensed practical nurses: One option for expanding the nurses workforce in Japan. In Ikegami N (ed.) Universal health coverage for inclusive and sustainable development: Lessons from Japan. The World Bank, p 133–148
Ikegami N, Campbell JC (1999) Health care reform in Japan: The virtues of muddling through. Health Aff 18:56–75
Ikegami N et al. (2011) Japanese universal health coverage: Evolution, achievements, and challenges. Lancet 378:1106–1115
Iwane T (1976) Wa-ga kuni-no kouritsu byouin-ni tsuite. Byouin koudou-no riron-to jisshotekikenkyu (on the public hospitals in Japan: a behavior model of hospitals and some empirical studies). Osaka Economic Papers. p 35–54
Jacobs R, Smith P, Street A (2006) Measuring efficiency in health care. Analytic techniques and health policy. Cambridge University Press
Jensen GA, Morrisey MA (1986) Medical staff specialty mix and hospital production. J Health Econ 5:253–276
Kanagawa Y (2008) Chiikiiryouwo Mamoru. Jichitaibyouin Keiei Bunseki. (Defending Local Health Care. Management Analysis of Local Public Hospitals). Jichitai kenkyusha, Tokyo
Kaneko K, Onozuka D, Shibuta H, Hagihara A (2018) Impact of electronic medical records (EMRs) on hospital productivity in Japan. Int J Med Inform 118:36–43
Kato K, Galvao Jr AF, Montes-Rojas GV (2012) Asymptotics for panel quantile regression models with individual effects. J Econom 170:76–91
Kawabuchi K, Kajitani K (2003) Time of changes–health care reform in Japan. Jpn Hosp 22:11–18
Kawaguchi H, Tone K, Tsutsui M (2014) Estimation of the efficiency of Japanese hospitals using a dynamic and network data envelopment analysis model. Health Care Manag Sci 17:101–112
Kawaguchi K (2008) Iryo-no Koritsusei Sokutei. Keisoushobou [Estimating Healthcare Efficiency, in Japanese]. Keisoshobo Publishing House, Tokyo
Knox K, Blankmeyer E, Stutzman J (2007) Technical efficiency in Texas nursing facilities: A stochastic production frontier approach. J Econ Finance 31:75–86
Kodera T, Yoneda K (2019) Efficiency and the quality of management and care: Evidence from Japanese public hospitals. App Econ Lett 26:1418–1423
Koenker R (2004) Quantile regression for longitudinal data. J Multivar Anal 91:74–89
Koenker R (2005) Quantile regression. Cambridge University Press
Koenker R, Bassett G (1978) Regression quantiles. Econometrica 46:33–50
Koenker R, Machado JA (1999) Goodness of fit and related inference processes for quantile regression. J Am Stat Assoc 94:1296–1310
Kumazawa M (2010) Kouei-kara minei-he. Ayumi-no shokai. (From public to private management. Description of the change). J Jpn Hosp Assoc 5:88–95
Lee J, McCullough JS, Town RJ (2013) The impact of health information technology on hospital productivity. RAND J Econ 44:545–568
Li H, Lindsay BG, Waterman RP (2003) Efficiency of projected score methods in rectangular array asymptotics. J R Stat Soc Series B (Stat Methodol) 65:191–208
Liu C, Laporte A, Ferguson BS (2008) The quantile regression approach to efficiency measurement: Insights from Monte Carlo simulations. Health Econ 17:1073–1087
Liu J, Tone K (2008) A multistage method to measure efficiency and its application to Japanese banking industry. Socio-Econ Plan Sci 42:75–91
Machado JAF, Santos Silva JMC (2019) Quantiles via moments. J Econom 213:145–173
Mandai N, Watanabe M (2019) Relationship between current account balance ratio and salary ratio in Japanese municipal hospitals. Health 11:1591–1597
Martin C, Jérôme T (2016) Cost (in) efficiency and institutional pressures in nursing home chains. Eur Account Rev 25:687–718
Mas-Colell A, Whinston MD, Green JR (1995) Microeconomic theory. Oxford University Press
Ministry of Health, Labor and Welfare (2012) Heisei 24nendo sinryouhoushuu kaitei-niokeru DPC seido (DPC/PDPS)-no taiyou-nitsuite (gaiyou) (An outline of DPC/PDPS system within the 2012 revision of fee schedule, Mar 28). http://www.mhlw.go.jp/stf/shingi/2r98520000025zci-att/2r98520000025zn7.pdf
Ministry of Internal Affairs and Communications (2007) Kouritsubyouin kaikaku gaidorain [Guidelines for the reform of local public hospitals, in Japanese]. https://www.soumu.go.jp/main_sosiki/c-zaisei/hospital/guidline.html
Ministry of Internal Affairs and Communications (2015) Shinkouritsubyouin kaikaku gaidorain [New guidelines for the reform of local public hospitals, in Japanese]. https://www.soumu.go.jp/main_sosiki/c-zaisei/hospital/guidline.html
Morikawa M (2010) Economies of scale and hospital productivity: An empirical analysis of medical area level panel data. RIETI Discussion Paper Series 10-E-050. The Research Institute of Economy, Trade and Industry
Motohashi H (2009) Productivity of medical services: TFP (total factor productivity) and DEA (data envelopment analysis) of Japanese hospitals. ESRI Discussion Paper Series 210, Economic and Social Research Institute Cabinet Office
Nabemi K (2010) Seimei kagayakasou nihon-no byouincho. (Head of Japanese hospital, which lights up the life). J Jpn Hosp Assoc 1:29–38
Nawata K, Nitta A, Watanabe S, Kawabuchi K (2006) An analysis of the length of stay and effectiveness of treatment for hip fracture patients in japan: Evaluation of the 2002 revision of the medical service fee schedule. J Health Econ 25:722–739
Otto AK (1996) Management style, decision processes, and hospital effectiveness. PhD thesis. Kent State University
Panzar JC, Willig RD (1977) Economies of scale in multi-output production. Q J Econ 91:481–493
Pauly M (1980) Doctors and their workshops: Economic models of physician behavior. University of Chicago Press, A National Bureau of Economic Research Monograph
Rosko M, Mutter R (2008) Stochastic frontier analysis of hospital inefficiency. A review of empirical issues and an assessment of robustness. Med Care Res Rev 65:131–166
Rosko MD (1999) Impact of internal and external environmental pressures on hospital inefficiency. Health Care Manag Sci 2:63–74
Rosko MD (2004) Performance of us teaching hospitals: a panel analysis of cost inefficiency. Health Care Manag Sci 7:7–16
Saito J (2007) DPC-to kyuuseiki byouin-no iryou (DPC and health care at acute hospitals). J Jpn Hosp Assoc 4:12–26
Shima Y et al. (2006) DPCdounyugo-no shinryouhouyshuu seikyuu-no genjou-to mondaiten [Current situation and issues with the fee schedule claims after the introduction of DPCs, in Japanese]. Nihon Byouin Gakkaishi 53:67–71
Stigler GJ (1951) The division of labor is limited by the extent of the market. J Political Econ 59:185–193
Suwabe A (2004) Our efforts on DPC in Iwate Medical University hospital. Rinsho Byouri 52:1011–1014
Takatsuka N, Nishimura S (2008) Oderingu shistemu ga byoinseisansei, kouristusei nioyobosu eikyono hyouka. (Effect of order entry system on hospital productivity and efficiency for inpatient care in Japan). Jpn J Health Econ Policy 20:15–33
Tersigni AR (1992) The effect of leadership styles on hospital labor productivity. PhD thesis. Western Michigan University
Thurston NK, Libby AM (2002) A production function for physician services revisited. Rev Econ Stat 84:184–191
Tomioka T, Mano T, Yamada Y (2008) Medico-economic evaluation on efficient management of large acute care hospitals [in Japanese]. Nihon Iryou Byouin Kanri Gakkaishi 45:55–63
Tsionas EG (2002) Stochastic frontier models with random coefficients. J Appl Econ 17:127–147
Vita MG (1990) Exploring hospital production relationships with flexible functional forms. J Health Econ 9:1–21
Wang H, He X (2007) Detecting differential expressions in GeneChip microarray studies: A quantile approach. J Am Stat Assoc 102:104–112
Weisbrod BA (1992) Productivity and incentives in the medical care sector. Scand J Econ 94:S131–S145
Wooldridge J (2007) Quantile methods. NBER Summer Institute, Lecture Notes 14. http://www.nber.org/WNE/lect_14_quantile.pdf
Worthington A (2004) Frontier efficiency measurement in healthcare: A review of empirical techniques and selected applications. Med Care Res Rev 61:135–170
Yamada T, Yamada T, Kim C, Noguchi H (1997) Efficiency and costs in hospitals: A stochastic frontier approach. Discussion Paper 748. University of Tsukuba, Institute of Policy and Planning Sciences
Zhang X, Tone K, Lu Y (2018) Impact of the local public hospital reform on the efficiency of medium-sized hospitals in Japan: An improved slacks-based measure data envelopment analysis approach. Health Serv Res 53:896–918
Acknowledgements
The paper originated from the PhD dissertation in Economics, defended by the corresponded author at Keio University, Tokyo. Access to the Annual Surveys of Local Public Enterprises (fiscal years 1999–2001) was granted to the corresponding author by Keio University Library in 2008–2010.
Funding
The paper was prepared in the framework of the Basic Research Program of the National Research University HSE.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design, data collection, data analysis and writing the earlier versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Appendix
Appendix
1.1 Data sources
Figures 4 and 5 and Tables A.1, A.2 and A.3
1.2 Results of the estimation
Tables B.1, B.2, B.3, B.4, B.5, B.6, B.7, B.8 and B.9
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Besstremyannaya, G., Golovan, S. Measuring heterogeneity in hospital productivity: a quantile regression approach. J Prod Anal 59, 15–43 (2023). https://doi.org/10.1007/s11123-022-00650-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11123-022-00650-3