Abstract
Clinical studies have found there still exists a lack of gene therapy dose-toxicity and dose-efficacy data that causes gene therapy dose selection to remain elusive. Model informed drug development (MIDD) has become a standard tool implemented throughout the discovery, development, and approval of pharmaceutical therapies, and has the potential to inform dose-toxicity and dose-efficacy relationships to support gene therapy dose selection. Despite this potential, MIDD approaches for gene therapy remain immature and require standardization to be useful for gene therapy clinical programs. With the goal to advance MIDD approaches for gene therapy, in this review we first provide an overview of gene therapy types and how they differ from a bioanalytical, formulation, route of administration, and regulatory standpoint. With this biological and regulatory background, we propose how MIDD can be advanced for AAV-based gene therapies by utilizing physiological based pharmacokinetic modeling and quantitative systems pharmacology to holistically inform AAV and target protein dynamics following dosing. We discuss how this proposed model, allowing for in-depth exploration of AAV pharmacology, could be the key the field needs to treat these unmet disease populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It’s been almost 200 years since the start of the modern pharmaceutical industry. Since its inception, pharmaceutical companies have been primarily develo** therapies to treat the symptoms of disease, not cure disease. Although some therapies, like insulin to treat diabetes, have been developed to treat the basis of disease, these therapies are short-acting and require chronic treatment over a patient’s lifetime. The pharmaceutical industry today is on the cusp of treating disease right at its heart – to curing some diseases completely. Gene therapy, which when you think about it, is the stuff of science fiction, targets the nucleus of a patient’s cells and uses the patient’s natural biochemistry to produce, turn on, or turn-off proteins that lead to disease. Imagine getting a single injection of a gene therapy product and then never needing another treatment for that disease for the rest of your life. This is the goal of gene therapy.
The “five rights” of health care are: the right patient, the right drug, the right time, the right dose, and the right route [1]. In many ways this adage is the pledge of pharmacokinetic modelers, regardless their area of specialty. However, with cell and gene therapies, the answer to many of these “five rights” can become muddled, especially at early phases of development. For this reason, systems pharmacology has become an essential tool to answer these critical questions. Although the area of application is still emerging with minimal regulatory guidance, it is important for the advancement of the community to offer guidance to those looking to utilize modeling to aid the development of gene therapies.
For this reason, the purpose of this review is to introduce gene therapy, to highlight the systems pharmacology models that have been developed (and not developed) for gene therapy, including physiological-based pharmacokinetic models, how these models have been used to support model-informed drug development, give recommendations on how to build these types of models, and to discuss the limitations and future related to systems pharmacology of gene therapy products.
Overview of common gene therapy technologies
The definition of gene therapy according to the FDA is “the administration of genetic material to modify or manipulate the expression of gene product or to alter the biological properties of living cells for therapeutic use [2].” Gene therapies involve the administration of designated genetic material to the target tissues via a carrier or “vector.” The vector can take many forms but this review will focus on two types: viral-based and plasmid-based with more emphasis placed on adeno-associated virus (AAV) vectors. Vector delivery can also be broken down into in vivo and ex vivo as illustrated in Fig. 1. For in vivo delivery, the genetic material is delivered directly to the patient using viral or non-viral vectors. For ex vivo delivery, the patient’s cells are extracted, then modified with the desired genetic material before being re-introduced back to the patient. A summary of some common terms in gene therapy is presented in Table 1.

Adapted from the FDA(https://www.fda.gov/biologicsbloodvaccines/cellulargenetherapyproducts/ucm573960.htm)
Visual representation of gene therapy types: ex vivo and in vivo therapies.
Virus-based gene therapy
When virus-based vectors are used for the transfer of a therapeutic gene, or a transgene, into a nucleus, the process is called transduction [3]. As a vehicle, vectors for gene therapy must ideally target the right cell with adequate onset and duration of expression, and be non-toxic [4]. Although viral vectors are attractive in gene therapy because of their higher efficiency and specificity, challenges remain in choosing a vector that is capable of meeting all requirements of the ideal vector since viral vectors are generally associated with more toxicity and higher technical demands than non-viral vectors [3, 5]. A list of vectors in gene therapy and their characteristics is summarized in Table 2.
Viral vectors can be classified into integrating or non-integrating vectors. Integrating vectors, such as retrovirus and about 10% of AAV, can integrate transgenes into the chromosomal DNA allowing permanent expression of the transgene resulting insertional mutagenesis [4, 6]. One notable example of insertional mutagenesis can be found from a trial in which young patients developed T-cell leukemia after three years of receiving the retroviral vector-mediated cell therapy for X-linked severe combined immunodeficiency (SCID). The cancer developed due to the unexpected vector insertion into the LMO-2 gene that is known to cause childhood cancers.
On the other hand, non-integrating vectors such as adenovirus (AV), herpes simplex virus (HSV), and the remaining 90% of associated adenoviruses (AAV, which will be discussed later in the section on formulation; Fig. 2) are maintained as episomes, and expression of the transgene is lost during cell division resulting in a lower risk of insertional mutagenesis [6]. Immune mediated adverse events most often occur with AV vectors but can happen with any viral vectors [7]. A clinical trial conducted in 1999 at the University of Pennsylvania using the first-generation adenoviral vector expressing the OTC gene resulted in the death of a patient after experiencing systemic inflammation and multi-organ failure [8]. For this reason, assessment of the immunogenicity potential is essential during gene therapy development.
Electron microscopy of two adenoviruses and their associated icosahedral structure. Middle drawing is a cartoon commonly used to illustrate the capsule structure of adenoviruses. Figure courtesy of Graham Beards and Wikipedia Creative Commons (https://commons.wikimedia.org/wiki/File:Icosahedral_Adenoviruses.jpg)
Another factor to consider when choosing a viral vector is their package capacity and tropism. Retroviral vectors can only target dividing cells while most of the other vectors, including AAV, AV, and lentivirus (a genus of retrovirus), can target both diving and non-dividing cells and can selectively target specific cells or tissues of interest by altering the vector system through pseudoty** or engineering [4]. Among different viral vectors, AAV is versatile and different serotypes can be engineered to demonstrate low immunogenicity, target specificity, and have discrete genome insertion sites [3, 9]. There are several different AAV serotypes as demonstrated in Table 3. Each AAV serotype exhibits differences in transgene expression level, tissue tropism (target tissues), and potential for immune reaction.
Disadvantages of AAV include a selection of serotypes and small package size of about 5 kb that limits the insertion of large genes [10]. However, its small size allows the in vivo injection into certain types of cells (i.e., hepatocytes and retinal cells) more favorable than other vectors. A wild-type AAV is not known to have a harmful effect on humans, but recombinant or engineered AAV vectors can induce T-cell responses, mostly due to the interaction between its capsid and cellular receptors [11]. A summary of selected approved gene therapies currently on the market can be found in Table 2.
Plasmid-based gene therapy
Although this review will focus on the computational modeling of AAV, models developed for AAV can be translated to other types of gene therapy delivery, including plasmid-based. When transgenes are delivered by non-viral means, the process is called transfection. There are several non-viral vectors, with plasmids being one of them. According to Gene Therapy Clinical Trials Worldwide by the Journal of Gene medicine, about 15% of all clinical gene therapy trials are conducted by plasmid DNA alone without a helper viral-vector. Plasmids are circular double stranded DNA (dsDNA) (denoted pDNA) that are rapidly degraded via endocytosis when administered systemically unprotected. For this reason, they must be to be injected directly in vivo to the target site or administered systemically by encapsulating within liposomal systems such as lipoplexes or polyplexes [12, 13]. Other technical methods for delivery of transgene, such as gene gun, electroporation, nanoparticles have also been developed and used in preclinical and clinical studies [14].
Due to the inherent negative charge of nucleic-acid-based molecules (i.e., DNA and RNA), cationic lipids or polymers have been utilized to encapsulate plasmid DNA molecules to enhance the delivery into the cell membranes [12]. Although the positive charge in liposomes enhances the cellular uptake of negatively charged genetic materials, nonspecific interaction with other serum proteins or enzymes that are negatively charged can result in hemolysis or low transfection efficiency [5]. Only a portion of injected pDNA can enter the nucleus due to cellular and extracellular membranes and matrices that hinder entry. Once they reach the nucleus, pDNA often stay episomal resulting in only transient expression of the gene [12].
The major disadvantage of plasmid vectors is delivery efficiency, such as cellular uptake, but a pDNA can have high capacity of gene size and production ability, as well as low risk of immunotoxicity [12]. To overcome the challenges, a combination of pDNA with a viral vector or other technique such as electroporation, ultrasound, or microbubbles is used to improve the efficiency of delivery [15]. Initially, many trials for cardiovascular diseases had high hopes for plasmid-based gene therapy; however, more recent studies attested that due to rapid clearance with pDNA alone or accumulation of lipoplexes and polyplexes into other tissues, as well as unpredictable results with various techniques, confirmed the inefficiency even when administered directly in vivo [16].
Interplay between formulation, route of administration, and patient factors
Although gene therapy is talked about as if it were one thing, it is not. Gene therapy is complex, and its safety and efficacy are affected by the formulation, how the formulation is administered, and by patient characteristics. It is beyond the scope of this review to present all the issues related to the interplay of these factors (the reader is referred to the Handbook of Gene and Cell Therapy for more information [17]) so what will be presented herein will be a brief overview of the topic, some of which has already been briefly discussed in Sect. 3 and will be expanded in this section.
For gene therapy to be successful, the gene or genetic material (which will be referred to hereafter as the genetic payload), whether it is encoding genes, transgene, or small-interference RNA (siRNA), must be delivered to the target, e.g., liver or muscle, it must be taken up by the cell and cross into the nucleus, and then be activated. This activation can come in many different forms:
-
the genetic payload can be transcribed and then translated into a gene product replacing a genetically deficient product in a patient,
-
the payload could work to silence a deleterious gene in the patient (gene silencing),
-
the payload could edit a malfunctioning gene in the patient, or.
-
the payload could introduce a suicide gene into the genome leading to cell death (such as for an oncolytic virus).
For lifelong effect to occur, the activation must be long-acting. Further, this entire process must occur safely and have a high rate of efficiency that translates to clinical effect, i.e., the genetic payload has the desired clinical effect.
For now, the ‘formulation’ will refer to the genetic payload, which may or may not be surrounded by a carrier, like a liposome or viral capsid, administered as a single-use suspension. The first step in the process is the administration of the formulation and delivery of the genetic payload to the target cell. Direct systemic administration of DNA or siRNA is difficult because of their low bioavailability, low ability of cross cell membranes, and limited circulation half-life due to the presence of circulating nucleases [18, 19]. Hence, a carrier is often used to augment delivery of the genetic payload; this is referred to as the ‘vector’. A vector is the system used to deliver the genetic payload to the nucleus. How that happens is one of the many different complexities of gene therapy as delivery can be either viral or non-viral in nature.
Non-viral delivery methods can be physical or chemical in nature. Physical methods use physical methods to cross cell membranes and include such methods as microneedle delivery of the material into the cell interior or microneedles that deliver material across the skin. Chemical methods are combination systems of the gene or DNA with chemical systems like liposomal delivery or polymer based nanocarriers. But by far, the major delivery vehicle for genetic payloads is viral delivery. Viruses have evolved with man and have efficient means of inserting and replicating their genetic material within the host. Viral delivery takes advantage of this by using the virus as the vehicle for delivery. There are a whole host of potential viruses to choose from: adenovirus, lentivirus, retrovirus, adeno-associated viruses (AAV), vaccinia, poxvirus, herpes virus, and others. Each of these viruses have their own safety profiles. Again, it is beyond the scope of this review to cover the pros, cons, and issues related to every virus delivery system, so this review will focus on adenovirus and AAV delivery, two of the most common viral delivery systems used today. As an aside, gene therapy has lots of jargon, like any scientific field, and two terms that are sometimes used interchangeably, but should not be, are transfection and transduction. Transduction refers to delivery of the genetic payload to the nucleus by viral mechanisms, whereas transfection refers to delivery by non-viral mechanisms.
Adenoviruses, the viruses most often associated with the common cold, are medium-sized, nonenveloped viruses with an icosahedral nucleocapsid (capsid for short) containing a double-stranded linear DNA as their genetic material (Fig. 2). Adenoviruses have been the most common payload delivery in clinical studies since their initial report in 1993. Ronald Crystal and colleagues first demonstrated the use of an adenovirus vector coding for the normal human CFTR cDNA to the nasal epithelium in a 23 year. old patient with cystic fibrosis [20]. Adenoviral vectors have many advantages including high transduction (high formation of gene product), do not integrate with host DNA, and can be produced at high levels pharmaceutically, but are limited by the transient expression of the transgene product, and they stimulate a strong immune and inflammatory response. Since adenoviruses do not integrate into their host’s DNA, they exist in the nucleus in a transient extrachromosomal state being transcribed like any other gene in the nucleus, but they are not replicated when the cell divides. Going back to the patient with cystic fibrosis, at the time of the study it was not appreciated how highly immunogenic adenovirus vectors were, and that subsequent administration of the product resulted in a waning of effect over time with repeated administration, such that by the time of the 3rd administration about 2 months later, almost no gene product could be detected. Despite many attempts to make adenovirus vectors less immunogenic, adenovirus has so far proven to be too strongly immunogenic to the human immune system. Nevertheless, adenovirus is still used today as a delivery vehicle for many gene therapies under clinical development.
AAVs were identified in 1965 and were initially thought to be a contaminant in the isolation of adenoviruses. AAVs are much smaller than adenoviruses and require a helper virus, which could be an adenovirus, for replication. AAVs were initially thought of as “satellite” viruses since their life cycle revolved around other viruses [21]. They are similar in structure to adenoviruses but have smaller capsids and carrying capacity. Many different AAV serotypes have been isolated and identified, each defined by their capsid motif proteins and the organs they target (Table 3). Because of their high seroprevalence in humans, no illnesses have been attributed to them. Although they have smaller carrying capacities, AAVs are less immunogenic, have a reduced inflammatory response, and are overall safer compared to adenoviruses.
One last factor related to formulation that may affect transduction, and possibly safety, is empty capsids [22]. Ideally, all of the gene product will be loaded into AAV capsids, but sometimes this is not the case. For any dose, some percent of the formulation will be a capsid without payload, so-called empty capsids. Empty capsids are taken up into cells but have no therapeutic benefit because they contain no payload. The role of these empty capsids on dosing, safety, and efficacy is not completely known. If capsids are responsible for the immune response to gene therapy, then a high empty capsid ratio may be leading to an unnecessarily high risk of immune response. Empty capsids may also be a safety concern, as empty capsids have been shown to increase hepatic transaminases in mice [23]. In a clinical study in 23 healthy volunteers who were administered empty capsids (n = 8) or empty capsids coadministered with tolerogenic ImmTOR nanoparticles (n = 15), no serious adverse events were noted but dosing with empty capsids did appear to induce proliferation of CD4 + and CD8 + lymphocytes which peaked about a week after dosing [24]. But there is also the argument that empty capsids may act as “effective decoys” for pre-existing antibodies to AAV capsids [25]. Whatever their role, and there will be a lot more to say about this in the future [26], it is clear that manufacturers must be able to control the process of their capsid formation so that the empty capsid ratio remains constant across lots [27].
Once you have the vector, a route of administration needs to be chosen, of which intravenous (IV), subcutaneous (SC), intra-arterial (IA), and intramuscular (IM) are the usual choices. With each route the pharmacokinetics (PK) will be different. Chen et al. [28] argued that the typical concept of PK does not “adequately describe the physiological processes that apply to [recombinant AAV] therapy” because AAV is not one thing, but many things: the AAV capsid, the genetic payload, transgene mRNA, and transgene protein. So, when discussing gene therapy PK you need to consider the PK of each of these components.
With regards to the vector, and again this will focus on viral vectors, the issue of bioavailability, biodistribution, and time course must be considered. Different routes of administration will have different bioavailability for the vector. Usually, it is stated (for small molecules) that IV administration has 100% bioavailability, but this is because it is assumed that venous concentrations equal arterial concentrations, i.e., there is no first pass from the lungs. But this is not the case with viral vectors; it is entirely possible that vector uptake and metabolism occurs in the lungs during the oxygenation of venous to arterial blood. However, this is highly dependent on the AAV serotype as demonstrated by Zincarelli C, et al. [29]. Hence, IV may not be 100% for all viral vectors. Only IA administration should have 100% bioavailability, and all others are expected to be less than that.
With each route, the biodistribution of the vector may change and with this change in biodistribution, an effect on transduction efficiency occurs as well. For example, Huard et al. [30] reported that transduction efficiency was higher in the heart, diaphragm, and intercostal muscles after intra-arterial administration of adenovirus vectors into the left cardiac ventricle compared to IV administration, but liver showed higher transduction after IV administration. Another example of the role route of administration plays in delivering gene products to key regions is with expression in the central nervous system [31]. Burstein and colleagues reported that the biodistribution of AAV9 into the CNS and peripheral nervous system (PNS) differs by the route of administration in cynomolgus monkeys. Their study compared different routes: three different intrathecal routes, intravenous, and intraocular administration. AAV9-CLN5 was administered as a single dose and biodistribution was studied 30 days later. Intracerebroventricular (ICV) and intracisternal magna (ICM) administration achieved broad and comparable distribution across most brain regions, whereas intrathecal and intravenous administration resulted in 10- to 100-fold lower levels of AAV9 in these same brain regions. All routes of administration resulted in similar levels in the PNS. That the route of administration affects the biodistribution of the vector, and subsequent transgene product formation, may come as no surprise to pharmaceutical scientists involved in small molecule or biologics development, but there is a genuine sense of surprise by this observation in the early gene therapy literature.
There is a remarkable lack of pharmacokinetic time-course data for viral vectors, but it would be expected that the time-course of the vector concentration changes with route of administration and with different serotypes, especially comparing intravenous or intra-arterial administration to intramuscular administration. Ni and colleagues [32] reported peak blood copy numbers 1 day after intramuscular administration of rAAV1 or rAAV8 in mice, whereas Kotchey and colleagues [33] reported peak copy numbers 1–2 h after intravenous administration of rAAV8 in mice.
Route of administration is also an important factor in safety through its off-target drug effects. For example, suppose the gene target is the muscle and the route of administration is intravenous or intra-arterial. Administration by these routes will invariably lead to significant distribution to non-muscle tissues. For example, the AAV9 capsid attaches to an unidentified glycan receptor in muscle for transfection to occur, but high levels of transduction have also been observed in liver and heart, which may lead to off-target safety effects. This is also borne out by epidemiological analysis – different routes of administration have different safety profiles for viral vectors. Kuzmin et al. [34] analyzed data from 149 clinical trials using AAV. Of these, 21% reported an administration-related adverse event, which was defined as an adverse event within 28 days of administration. IV administration was deemed the safest route with only 12% of studies reporting an administration serious adverse event, compared to 27% for intramuscular and 33% for intra-arterial.
In addition to formulation and route of administration, patient factors may affect transduction efficiency. Davidoff et al. [35] showed that male mice when dosed with AAV2 or AAV8 had 5- to 13-fold higher expression of the target protein in male mice compared to females, which may be a differential effect of androgens. Maguire et al. [36] also showed that females expressed greater protein expression than males after AAV9 administration in two different mice species. Surprisingly, whether these sex effects can hold in humans has not been studied. Age has also been shown to play a role – at least in animals. Polinski et al. [37] showed that protein expression was lower in aged rats compared to younger rats, which did not appear to be capsid mediated since the experiment was repeated using different capsids: AAV2, AAV5, AAV9, and lentivirus. Laz and Tuszynski [38] delivered AAV9-eGFP and AAV-PhP.eB-eGFP intrathecally or intravenously to aged and juvenile mice. Aged mice intravenously dosed with AAV9 had a reduction in brain protein expression compared to young mice. Surprisingly, they found no difference when AAV9 was administered intrathecally or using intravenous AAV.PhP.eB-eGFP.
Another patient-specific factor that could affect the safety and efficacy of a gene therapy product is the prevalence of preexisting neutralizing antibodies, which neutralize the effect of a gene therapy through the action of antibodies against the viral capsid. Adenoviruses and AAVs are modified viral capsules. It’s entirely possible for broad segments of a population to already have been exposed to a recombinant adenovirus or AAV capsid that is similar enough in nature, prior to receiving treatment, and the body has developed antibodies to them (innate immunity). Table 3 shows the prevalence of pre-existing neutralizing antibodies in the population. Once the treatment is administered, the body may also develop antibodies against the delivered capsid, which may prevent future repeated administration of the vector from working (adaptive immunity). In fact, repeated administration will prime the immune system making it better and better at attacking the capsid and neutralizing it.
The presence of these neutralizing antibodies starts early in life and is long-lasting. Calcedo et al. [39] demonstrated that neutralizing antibodies to AAV2 and AAV8 (in the absence of any gene therapy) are moderate at birth, decrease between 7 and 11 months of age, but progressively increase thereafter through adolescence. In 2006, 7 men received gene therapy using rAAV2 to treat hemophilia B. The trial never progressed because the effect of the therapy was short-lived; by 14 weeks the Factor IX activity was no longer detected [40]. Over a decade later, the same investigators brought those patients back and tested them for neutralizing antibodies to the therapy they received [41]. Three subjects demonstrated persistent neutralizing antibodies of high titer to AAV2. Because of the high degree of conservation among AAV capsids in the amino acid sequence the patients demonstrated cross-reactivity to AAV5 and AAV8. Even though patients received AAV2, over time they developed a polyclonal response to AAV5 and AAV8. This means in these patients, even if a new gene therapy for hemophilia is developed, they most likely won’t be able to benefit from it because of their neutralizing antibodies.
Are there other patient-specific factors that may affect product expression after gene therapy? Quite possibly. Could there be drug interactions with small molecules or biologics to viral vectors? Maybe. It seems unlikely, but it would be naïve to say, ‘absolutely not’. We used to believe, back when monoclonal antibodies (mABs) were first introduced, that there would be no drug interactions with small molecules because of the high specificity MAbs exhibit for their target. We now know that mABs targeting T-cells can affect cytokine expression, which in turn can affect cytochrome p450 expression, which in turn can affect a drug’s metabolism, such that a mAB can have a drug interaction with a small molecule under certain conditions. Can the reverse be true? Can a small molecule affect gene therapy? Could prior administration of an immunosuppressant like tacrolimus suppress the immune response and decrease the effect of neutralizing antibodies, possibly improving the efficacy of gene therapy? What about a patient’s weight? Could obese patients respond differently to gene therapy? Obesity induces a low-level inflammatory state. Could this low-level inflammatory state affect expression of the target protein? Maybe. And what about race? Could a patient’s race affect gene therapy? Could there be a different efficacy and safety profile between Japanese and those of Western descent? Any of these could be possible. Gene therapy is too new at this time for all of the factors affecting its safety and efficacy to be known.
Regulatory guidance
Although at the time of writing there are no regulatory or organizational guidances on the modeling of gene therapies, there are several industry guidance documents available to advise companies on the pre-clinical and clinical studies recommended for approval and to help guide model development. Some of the guidance documents relevant to gene therapy are summarized below in Table 4. Of note, in addition to guidance on gene therapy, there may also be guidance documents related to specific diseases; however, in the interest of brevity only general guidances as they pertain to gene therapy development have been listed. It is important to familiarize oneself with the studies conducted and required for regulatory submission as indicated by the guidances.
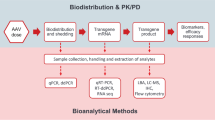
Bioanalytical considerations
By now, everyone knows the story of how Kary Mullis invented polymerase chain reaction (PCR) in the 1980s. One of the most interesting scientific figures in the last century, Dr Mullis initially had the idea for PCR while driving one night as he drove through the hills in Northern California – a classic “Eureka” moment in science. Initially dismissed by his colleagues at Cetus Corp. because the idea seemed perhaps too simple, he had success in December 1985 and the rest is history. His original paper has been cited more than 17,000 times [42]. Like any groundbreaking achievement there was debate as to whether he truly “discovered” PCR, and there were lawsuits trying to bust Cetus’ patent on the method, but nevertheless Dr. Mullis won the Nobel Prize for Chemistry for his discovery in 1993.
The idea behind PCR is to first heat DNA so the DNA in the sample separates into its individual strands. Taq polymerase, a heat-resistant enzyme which has been added to the system, builds two new double strands – one strand being an original strand and the other being a copy. Think of this as molecular photocopying. The process is then repeated many times creating multiple copies of the original sample creating as many as a billion copies of the original DNA sample in just a few hours. While revolutionary, PCR has its limitations. PCR is useful to determine whether a particular stand of DNA is present in a sample, like with genoty**, paternity testing, or molecular sequencing, but cannot tell you how much is present.
Quantitative PCR (qPCR), sometimes called real-time PCR, was developed by Russell Higuchi and colleagues at Roche Molecular Systems and Chiron to quantify the amount of a particular DNA sequence present in a sample [43]. By adding a fluorescent dye to the sample that stains nucleic acids and fluoresces upon binding, a fluorometer can be used to quantify the fluorescence of a sample and when compared to standards of known quantity, an estimate of the amount of DNA in a sample can be obtained. Hence, one of the major uses of qPCR is quantitative measurement of gene expression. Today, qPCR is a mature technique and entire books can be written on its use. Simply stated, there are a variety of different instrumentation manufacturers that put their own flavor on the basic method, e.g., TaqMan by Applied Biosystems and LightCycler by Roche, and can process thousands of samples for different probes simultaneously (multiplexing) in a day.
A new competing method has recently appeared – droplet digital PCR (ddPCR). Both qPCR and ddPCR are useful to measure gene expression. qPCR has a wider dynamic range and process more samples than ddPCR, but ddPCR is much more precise and provides absolute quantitation (does not need calibration curves). Like PCR, ddPCR uses a Taq polymerase to amplify DNA fragments but ddPCR partitions the reaction into thousands of droplets and the fluorescence of each droplet can then be counted (each drop is either negative or positive). ddPCR and qPCR give identical results when there are low levels of contamination [44].
When using AAV as the viral vector, the results from a qPCR or ddPCR are usually reported as a “physical titer” in viral genomes per mL (vg/mL) or vector copy number per mL (VCN/mL, which is equal to the vg standardized to the mass of the genomic DNA input or some housekee** gene, i.e., vg/dg, where dg is the diploid genome). VCN is often used interchangeably with genome copies (gc/mL or GC/mL). Other types of gene therapy might report different numerators. For example, adenovirus titers are reported as plaque-forming units per ml (pfu/mL), whereas lentivirus titers are reported as “infectious” or transducing units per mL (TU/mL). Typical values reported for vg/mL are often greater than 1010 and may cover a dynamic range of over 100,000. For example, Greig et al. [45] reported on the pharmacokinetics of an AAV8.TBG.eGFP vector into the saphenous vein of male cynomolgus monkeys following a dose of 7.5 × 1012 genome copies (GC) per kg at a concentration of 7.5 × 1012 GC per mL over intervals that varied from 1, 10, and 90 min. Peak concentrations were on the order of 1012 vg/mL and by 100 h had decreased to about 100 vg/mL, a drop of ten billion! Readers looking for additional guidance or resources on bioanalytical considerations for AAV and other gene therapies can refer to the publications by Gorovits B, et al. and Kavita U, et al. [46, 47].
Modeling platforms and techniques
Model informed drug development (MIDD) is a process regularly employed throughout the development lifecycle of a drug to expedite development, enhance scientific understanding of the drug, and ultimately ensure drug benefit is maximized for patients [48]. Computational modeling approaches in gene and cell therapy have become possible with the increased understanding of cellular and genetic processes and advances in processing capabilities of computers. Classical modeling approaches for small molecules and PK are not always applicable to gene therapies. Therefore, several modeling approaches have emerged to capture and explain these types of complex therapies.
One such methodology is quantitative and systems pharmacology (QSP). QSP or more generally, systems pharmacology, is a discipline that uses mathematical and computational modeling with a goal “to understand, in a precise, predictive manner, how drugs modulate cellular networks in space and time and how they impact human pathophysiology” [49]. QSP models endeavor to represent the biological system, including cellular and receptor interactions if needed, to answer the question of interest, leading to a better representation of physiological changes following cell and gene therapies. QSP has been applied in several cases to support MIDD [50]. Models focusing on viral diffusion or immune biology response were previously reported [51,52,53,54]. In these early reports, gene therapy related to immune cancer therapy through treatment with oncolytic viruses or combination therapy with dendritic cells were explored computationally.
Another type of modeling approach utilized for cell and gene therapy is agent-based modeling (ABM), which is a system-based modeling approach where a collection of autonomous decision-making entities called agents make decisions on the basis of a set of rules [55]. The agents collectively represent the desired biological system and provide confirmative and/or predictive results about the system. Predicting cancer and tumor growth is one area that has been explored extensively using ABM [56]. Modeling in infectious disease and viral behavior within tissues has also been explored using ABM [57].
Mechanistic pharmacokinetic – pharmacodynamics (PKPD) modeling is applicable when a biomarker or pDNA is observable systemically. A well-characterized biomarker assay can be incorporated into mechanistic PKPD models [58]. Plasma biomarkers have been explored for use in modeling most extensively in oncology [59], but exploration has begun in other areas as well such as viral vectors/plasmids. Mechanistic modeling was explored for HSV distribution in solid tumors [60]. In this report, diffusion reaction equations were used to identify factors to improve vector efficiency.
The remainder of this section will focus on the combination of PK modeling, particularly physiologically based pharmacokinetic (PBPK) modeling, and systems pharmacology for the application of modeling AAV therapies. PBPK is an MIDD approach that incorporates physiological and biochemical principles, like organ size, organ blood flow, how the organs are connected, degree of drug ionization, protein binding, and lipophilicity, to name a few, to explain a drug’s pharmacokinetics. Applications of PBPK include first-in-man dose selection, prediction of drug interactions, extrapolation of adult doses to children, prediction of drug exposure in patients with renal or hepatic impairment, and fetal exposure in pregnant women [61]. No public applications for PBPK being applied in gene therapy clinical development exist to the authors’ knowledge. However, PBPK models have been published that could help guide development of gene therapy PBPK models due to overlap** biological mechanisms; some examples include a PBPK model exploring antibody ocular disposition could guide model development for AAV therapies administered ocularly [62], a cell therapy PBPK model with tissue level parameters that can be repurposed for AAV PBPK models [63], and a PBPK model of siRNA therapy that showcases how mRNA measurements can be incorporated into model calibration [64].
Additionally, a recent meta-analysis across AAV usages in clinical settings found there still exists a lack of dose-toxicity and dose-efficacy data that causes AAV dosing regimens to remain elusive [65]. As such, there exists a large unmet opportunity to standardize PBPK strategies to support gene therapy dose selection and clinical trial design. As such, this section focuses on recommendations for applying PBPK modeling to support AAV-based gene therapy development.
PBPK models seek to mathematically represent absorption, distribution, metabolism, and excretion (ADME) of administered therapies, often to support dose optimization [66]. Due to the mechanism of action through which AAV-based gene therapies work, we recommend PBPK modeling for AAV-based gene therapies include ADME considerations for both (1) the AAV capsid and (2) the expressed protein. In addition, it may be necessary to consider the effect of the empty capsid, as mentioned earlier. As such, we recommend PBPK modeling for AAV-based gene therapies include multiple biological processes and compartments as depicted in Fig. 3, which would require the model parameters listed in Table 5. Briefly, these biological processes include AAV biodistribution, AAV cellular uptake, uncoating and transduction of packaged gene, and biodistribution, relevant pharmacodynamic effects, and elimination of the transduced protein. Here considerations for modeling these biological processes will be explored in greater detail.
Example schematic of systemic AAV PBPK distribution with suggested applicable compartments based on AAV tropism and frequently targeted tissues of AAV therapy. Applicable modeling parameters as referred to in Table 5. Created with BioRender.com
PBPK modeling of pDNA
There have been few studies where pDNA concentrations were quantified over time, and even fewer in humans [67]. One of the few human reports of pDNA pharmacokinetics was by Bonate et al. [68] who reported on ASP0113, a pDNA vaccine against cytomegalovirus, in dialysis patients and healthy volunteers after intramuscular dosing (Fig. 4). What was interesting about that study was the observation of double peaks after pDNA dosing, with the second peak having higher concentrations than the first peak. The authors rationalized that the first peak was due to rapid absorption from the injection site and the later peak was due to lymphatic absorption since it occurred much later. There have been no reports of PBPK models for pDNA gene therapy products.
ASP0113 plasmid concentrations. Mean (SD) ASP0113 plasmid concentration in CMV-seropositive (CMV+) and CMV-seronegative (CMV–) healthy subjects and CMV-seronegative dialysis patients measured by polymerase chain reaction. Time values have been jittered for each analysis point for graphical presentation only to distinguish among the subject groups. Values below the limit of quantification were treated as 0 for calculation purposes. CMV indicates cytomegalovirus; LLOQ, lower limit of quantification. Data reported in Bonate et al. [68]
PBPK modeling of AAV capsids
Despite the lack of published PBPK models for AAV gene therapy, it is possible to envision what such a model must look like and entail which is show in Fig. 3. The compartments included represent the commonly targeted tissues for AAV gene therapies and are driven by the tropism of the available AAV serotypes. Therefore, Fig. 3 graphically represent an example schematic of a platform-based model design that allows translation to many different types of AAV therapies. To expand on the PBPK distribution, the mechanistic behavior of the AAV once it reaches the targeted cells is depicted in Fig. 5. Therefore, to develop an AAV PBPK-mechanistic model, we recommend the model scope include the following for AAV capsids: biodistribution of the administered AAV capsids across tissues (Fig. 3), intracellular uptake through receptor-mediated endocytosis or pinocytosis, escape from endosomes into cytoplasm, uptake from cytoplasm into the nucleus, and nuclear uncoating (Fig. 5). The distribution and compartments illustrated in Fig. 3 can be adapted to different types of AAV by removing or adding compartments as they apply to the specific case. Since different AAV serotypes exhibit different tropism, accounting for serotype specific receptor parameters is necessary [69, 70]. Such parameters include AAV-AAV receptor (AAVR) binding affinity, AAVR expression across tissues/cell types, and AAVR synthesis and internalization rates (Table 5) would affect capsid uptake across tissues. A recent review by Chowdhury et al. describes how such AAVR parameters are critical towards dictating AAV tropism and their importance in PK/PD considerations [71]. Considerations specific to how the capsid is engineered may need to be modeled; for example, engineered AAV variants can also affect AAVR binding and tropism [72, 73]. It is important to note that AAVR-independent pathways, such as micropinocytosis, may be used to facilitate AAV cellular uptake; however, there are diametric findings on the role micropinocytosis plays on AAV transduction and may be serotype or cell type specific [74, 75]. Thus, we propose PBPK modeling focuses on AAVR-dependent endocytic uptake (Fig. 5; Table 5).
Graphical schematic of AAV cellular behavior and physiology with various routes of administration. Example schematic of systemic AAV PBPK distribution with suggested applicable compartments based on AAV tropism and frequently target tissues of AAV therapy. Applicable modeling parameters as referred to in Table 5. Created with BioRender.com
Once AAV capsids are endocytosed, they undergo translocation from early endosomes ultimately to the nucleus where they are uncoated. While the mechanism of nuclear entry remains not fully defined, evidence indicates that AAV capsids residing in early endosomes are sorted towards the trans-Golgi network along a retrograde transport pathway. Within the trans-Golgi network capsid conformational changes occur that allow export to the cytoplasm followed by nuclear import [76,77,78]. Interestingly, endocytosed AAVs do not seem to undergo recycling to the cell membrane [79] and typically escape from early/late endosomes prior to trafficking to lysosomes [80,81,82]. Therefore, models for intracellular trafficking of AAV capsids are proposed to include AAV escape from endosomes into the cytoplasm followed up uptake into the nucleus. Modeling AAV escape from endosomes as a single rate is beneficial as it reduces model complexity and allows the trans-Golgi network processes to be represented by a single model parameter (Table 5), reducing likelihood of model identifiability issues.
The eye compartment included within the model is a special case. The retina is protected by barriers (blood-retinal barrier (BRB)) which are made of tight junctions preventing systemic absorption of proteins and other large molecules, including AAV [83]. Generally, AAV gene therapy targeted for ocular conditions must be administered intraocularly and not systemically [84,85,86]. However, effects from systemic administration are possible. An example of ocular effects following systemic administration of an AAV therapy was explored by Simpson CP, et al. [87]. In this study, they found that systemic delivery led to robustly transduced cells throughout the retina with limited ability to further penetrate the retina and reach the photoreceptors. For this reason, ocular exposure of systemic administered AAV should be considered where applicable. In addition, as mentioned in Sect. 7, with the help of other modeling approaches it is possible to reproduce the distribution and intracellular processes of intraocular administer gene therapies [62]. It is also important to consider the systemic exposure and systemic effects of intraocular administered AAV therapies [88, 89].
Immune response following AAV administration may be necessary to include in the PBPK model. Wild-type AAVs are common and there is a high native prevalence of neutralizing anti-AAV antibodies in the general population [90] and is serotype dependent [91] (Table 3). Anti-AAV neutralizing antibodies can interfere with therapeutic efficacy, resulting in difficulty with dose selection and subsequently increased toxicity risk [92]. One strategy to overcome decreased efficacy by anti-AAV antibodies that is gaining popularity is to purposefully co-dose capsids containing the gene with empty capsids. Evidence has shown that protein transduction is dependent on the full/empty capsid ratio, and may increase protein transduction via empty capsids acting as a decoy to anti-AAV antibodies [25], although this is currently highly debatable. Incorporating anti-AAV antibodies into the PBPK model may be necessary depending on the target population, serotype, and empty to full capsid ratio and should be carefully considered.
Modeling the transduced protein
Once AAV capsids are localized to cellular nuclei, capsids are uncoated, releasing packaged genes and allowing target protein transduction. AAV uncoating remains poorly understood and appears to be a rate-limiting step in a serotype and tissue-specific manner [82]. Ultimately, AAV uncoating results in release of the packaged single-stranded DNA (ssDNA), ssDNA is converted through double-stranded form to either episomal DNA or integrated into the host genome, transcribed to mRNA, and mRNA is exported from the nucleus and translated to protein (Fig. 5; Table 5). Preclinical experiments suggest that AAV derived ssDNA and dsDNA are unstable, and degradation of these is a rate-limiting step in AAV transduction efficacy [93, 94]. Conversely, once converted episomal DNA is relatively stable and can persist in tissues for years [95]. Likewise, transcribed mRNA degradation does not appear to be a significant rate-limiting step [96]. Therefore, computational models for protein transduction should include degradation on ssDNA/dsNDA, and ssDNA and dsDNA can be lumped together for model reduction and identifiability optimization.
Considerations for modeling the transduced protein will be highly dependent on the type of transduced protein and mechanism of action it exerts. Generally, once the protein is transduced it may undergo efflux from production cells into surrounding tissue and ultimately back to systemic circulation, where biodistribution, elimination, and pharmacodynamic effects continue. Depending on the expressed protein and desired outcomes to capture with the PBPK model, biological processes such as protein-transporter interactions, enzymatic metabolism, and pharmacodynamic effects can be incorporated [97]. Local concentrations of the transduced protein in specific tissues are critical to the dynamics of transporter, metabolic, or pharmacodynamic responses, and as such transduction in specific tissues based on AAV biodistribution is necessary to model. Biomarker or clinical endpoint outcomes can be incorporated into the model based on transduced protein pharmacodynamic effects as desired.
The development of an AAV PBPK model capturing the relevant biological processes would allow for multiple MIDD applications. Such a PBPK model would capture relevant biology and mechanisms of action for both the administered AAV and transduced protein. This PBPK model would be a powerful tool to support dose optimization, allowing considerations such as transduced protein concentrations or pharmacodynamic response necessary to achieve clinical efficacy. Doses achieving target protein concentration could be explored with respect to full/empty AAV capsid ratio, route of administration, or serotype tropism. Virtual populations using this PBPK model could be developed to inform clinical population selection based on projected safety/efficacy profiles; for example, PBPK modeling could inform a threshold of preexisting anti-AAV antibodies above which clinical efficacy is anticipated to be unachievable. With the recent difficulties in selecting safe and effective doses for AAV-based gene therapies seen clinically, PBPK models allowing for in-depth exploration of AAV pharmacology could be the key the field needs to treat these unmet disease populations.
Future/gaps/limitations
There are so many gaps in the development and modeling of gene therapy products it’s difficult to know where to begin. Three areas we have identified that need immediate attention are with regards to clinical pharmacology, basic science, and safety of AAVs.
First, the concepts of clinical pharmacology in gene therapy, treating the gene therapy product as you would any other biologic, is practically non-existent. One might think that since a patient receives only a single dose of the drug that tremendous effort would be spent in getting the dose right, but in discussions with many key opinion leaders in the area, this is not the case. There is a great deal of latitude in the dose administered. Indeed, an internal review of all AAV gene therapy studies in clincaltrials.gov showed a dose range of 2 × 1010 to 3 × 1014 vg/kg (internal data not shown), a ~ 10,000 fold range. Translation of doses in animals to humans is a black art, often with the clinically used human dose being the same as a dose in animals that showed efficacy, i.e., the dose used in animals that demonstrated an effect (vg/kg) is the same dose used in humans. Much more work could be done regarding the proper dose to take into humans.
Second, with regards to building a systems pharmacology model, conceptually it is understood how gene therapy works, but many of the basic biology and parameter values needed to build such a model are unknown. For instance, the receptor that binds AAV7 to cells is unknown. Since the receptor is unknown, its density on cells is unknown, which makes models of cell uptake difficult to build. For this reason, many parameters and processes can/are lumped together during the modeling process. This leads to less parameters requiring optimization/ parameterization; however, this can lead to a model being unidentifiable. Not only is parameter identifiability an issue, but the ability for in vitro derived parameters to be translated to the in vivo setting is limited. For one example, in vivo affinities between therapeutic antibodies and their targets measure via surface plasmon resonance have been shown to not always be translatable to in vivo affinity due to the additional environmental factors and co-receptors not accounted for with in vitro settings [98]. Predicting AAV tissue distribution and systemic PK using only in vitro data is also a large challenge, as such in vitro-in vivo extrapolation requires an understanding of pharmacology [99] that is currently lacking for AAV therapies. Much more basic science is needed regarding AAV biodistribution and uptake into cells to allow AAV PBPK/QSP models to be built with high confidence.
Lastly, there have been concerns about the safety of vector-based delivery with some recent trials being put on clinical hold due to deaths and safety concerns. It has been speculated that the sheer volume of genetic material delivered could be the cause, but this is not known with any degree of certainty. Hence, more research needs to be done on the safety of vector-based products, the reasons for safety issues, and how to prevent them in the future. PBPK and QSP based models may help in this regard by better understanding how a vector-based product distributes in the body and how it is transduced to a transgene product.
Conclusions/summary
You might have noticed that, despite what the title of this paper suggests, there isn’t a lot of detail regarding gene therapy models in this review. That’s because there are few published gene therapy models at the time of this publication (2023). There have been a few more modeling-related posters presented at meetings, but most lack details and cannot be formally evaluated. Computational models of gene therapy are an open area for research, but with a dire lack of biological data upon which to build these models, their development is problematic and will require ingenuity and model assumptions that may not be verifiable. We hope by presenting this review we will stimulate further research and publication in the area.
References
Grissinger M (2010) The Five Rights. Pharm Ther 35:542
Sinclair A, Islam S, Jones S (2016) Gene Therapy: an overview of approved and Pipeline Technologies. CADTH Issues in Emerging Health Technologies. Canadian Agency for Drugs and Technologies in Health, Ottawa (ON)
Mali S (2013) Delivery systems for gene therapy. Indian J Hum Genet 19:3–8. https://doi.org/10.4103/0971-6866.112870
Bouard D, Alazard-Dany N, Cosset F-L (2009) Viral vectors: from virology to transgene expression. Br J Pharmacol 157:153–165. https://doi.org/10.1038/bjp.2008.349
Ramamoorth M, Narvekar A (2015) Non viral vectors in Gene Therapy- An Overview. J Clin Diagn Res JCDR 9:GE01–GE06. https://doi.org/10.7860/JCDR/2015/10443.5394
Anson DS (2004) The use of retroviral vectors for gene therapy-what are the risks? A review of retroviral pathogenesis and its relevance to retroviral vector-mediated gene delivery. Genet Vaccines Ther 2:9. https://doi.org/10.1186/1479-0556-2-9
Somia N, Verma IM (2000) Gene therapy: trials and tribulations. Nat Rev Genet 1:91–99. https://doi.org/10.1038/35038533
Wilson JM (2009) Lessons learned from the gene therapy trial for ornithine transcarbamylase deficiency. Mol Genet Metab 96:151–157. https://doi.org/10.1016/j.ymgme.2008.12.016
Naso MF, Tomkowicz B, Perry WL, Strohl WR (2017) Adeno-Associated Virus (AAV) as a Vector for Gene Therapy. BioDrugs Clin Immunother Biopharm Gene Ther 31:317–334. https://doi.org/10.1007/s40259-017-0234-5
Wu Z, Yang H, Colosi P (2010) Effect of genome size on AAV vector packaging. Mol Ther J Am Soc Gene Ther 18:80–86. https://doi.org/10.1038/mt.2009.255
Colella P, Ronzitti G, Mingozzi F (2018) Emerging issues in AAV-Mediated in vivo gene therapy. Mol Ther Methods Clin Dev 8:87–104. https://doi.org/10.1016/j.omtm.2017.11.007
Wang D, Gao G (2014) State-of-the-art human gene therapy: part II. Gene therapy strategies and clinical applications. Discov Med 18:151–161
Fenske DB, MacLachlan I, Cullis PR (2001) Long-circulating vectors for the systemic delivery of genes. Curr Opin Mol Ther 3:153–158
Godbey WT (2014) Gene Delivery. An introduction to Biotechnology. Elsevier, pp 275–312
Ginn SL, Amaya AK, Alexander IE et al (2018) Gene therapy clinical trials worldwide to 2017: an update. J Gene Med 20:e3015. https://doi.org/10.1002/jgm.3015
Rincon MY, Sarcar S, Danso-Abeam D et al (2015) Genome-wide computational analysis reveals cardiomyocyte-specific transcriptional Cis-regulatory motifs that enable efficient cardiac gene therapy. Mol Ther J Am Soc Gene Ther 23:43–52. https://doi.org/10.1038/mt.2014.178
Nóbrega C, Mendonça L, Matos CA (2020) A handbook of gene and cell therapy. Springer International Publishing, Cham
Zhang MM, Bahal R, Rasmussen TP et al (2021) The growth of siRNA-based therapeutics: updated clinical studies. Biochem Pharmacol 189:114432. https://doi.org/10.1016/j.bcp.2021.114432
Park J, Park J, Pei Y et al (2016) Pharmacokinetics and biodistribution of recently-developed siRNA nanomedicines. Adv Drug Deliv Rev 104:93–109. https://doi.org/10.1016/j.addr.2015.12.004
Crystal RG (2014) Adenovirus: the first effective in vivo gene delivery vector. Hum Gene Ther 25:3–11. https://doi.org/10.1089/hum.2013.2527
Gonçalves MAFV (2005) Adeno-associated virus: from defective virus to effective vector. Virol J 2:43. https://doi.org/10.1186/1743-422X-2-43
Wright JF (2014) AAV empty capsids: for better or for worse? Mol Ther J Am Soc Gene Ther 22:1–2. https://doi.org/10.1038/mt.2013.268
Gao K, Li M, Zhong L et al (2014) Empty virions in AAV8 Vector Preparations reduce transduction efficiency and may cause total viral particle dose-limiting Side-Effects. Mol Ther Methods Clin Dev 1:20139. https://doi.org/10.1038/mtm.2013.9
Schroeder H, Johnston L, Clyde E et al (2022) 37: functional assessment of T cell responses to AAV8 empty capsids in healthy volunteers
Mingozzi F, Anguela XM, Pavani G et al (2013) Overcoming preexisting humoral immunity to AAV using capsid decoys. Sci Transl Med 5:194ra92. https://doi.org/10.1126/scitranslmed.3005795
Food and Drug Administration (2013) Toxicity risks of adeno-associated virus (AAV) vectors for gene therapy. GT)
Schofield M (2021) Empty/full separation: gene therapy’s hidden challenge. Cell Gene Ther Insights 6:1715–1722. https://doi.org/10.18609/cgti.2020.189
Chen N, Sun K, Chemuturi NV et al (2022) The perspective of DMPK on recombinant Adeno-Associated Virus-Based gene therapy: past learning, current support, and future contribution. AAPS J 24:31. https://doi.org/10.1208/s12248-021-00678-7
Zincarelli C, Soltys S, Rengo G, Rabinowitz JE (2008) Analysis of AAV serotypes 1–9 mediated gene expression and tropism in mice after systemic injection. Mol Ther 16:1073–1080. https://doi.org/10.1038/mt.2008.76
Huard J, Lochmüller H, Acsadi G et al (1995) The route of administration is a major determinant of the transduction efficiency of rat tissues by adenoviral recombinants. Gene Ther 2:107–115
Dyson LP (2021) Neurogene’s AAV Biodistribution Study Shows Route of Administration Essential Component in Optimizing Gene Therapy Treatment for Neurological Disease. In: Neurogene. https://www.neurogene.com/press-releases/neurogenes-aav-biodistribution-study-shows-route-of-administration-essential-component-in-optimizing-gene-therapy-treatment-for-neurological-disease/. Accessed 18 Aug 2022
Ni W, Le Guiner C, Gernoux G et al (2011) Longevity of rAAV vector and plasmid DNA in blood after intramuscular injection in nonhuman primates: implications for gene do**. Gene Ther 18:709–718. https://doi.org/10.1038/gt.2011.19
Kotchey NM, Adachi K, Zahid M et al (2011) A potential role of distinctively delayed blood clearance of recombinant adeno-associated virus serotype 9 in robust cardiac transduction. Mol Ther J Am Soc Gene Ther 19:1079–1089. https://doi.org/10.1038/mt.2011.3
Kuzmin DA, Shutova MV, Johnston NR et al (2021) The clinical landscape for AAV gene therapies. Nat Rev Drug Discov 20:173–174. https://doi.org/10.1038/d41573-021-00017-7
Davidoff AM, Ng CYC, Zhou J et al (2003) Sex significantly influences transduction of murine liver by recombinant adeno-associated viral vectors through an androgen-dependent pathway. Blood 102:480–488. https://doi.org/10.1182/blood-2002-09-2889
Maguire CA, Crommentuijn MH, Mu D et al (2013) Mouse gender influences brain transduction by intravascularly administered AAV9. Mol Ther J Am Soc Gene Ther 21:1470–1471. https://doi.org/10.1038/mt.2013.95
Polinski NK, Manfredsson FP, Benskey MJ et al (2016) Impact of age and vector construct on striatal and nigral transgene expression. Mol Ther Methods Clin Dev 3:16082. https://doi.org/10.1038/mtm.2016.82
Laz NB (2020) Impact of Age on AAV Gene Transfer to Mouse Brain. UC San Diego
Calcedo R, Morizono H, Wang L et al (2011) Adeno-associated virus antibody profiles in newborns, children, and adolescents. Clin Vaccine Immunol CVI 18:1586–1588. https://doi.org/10.1128/CVI.05107-11
Manno CS, Pierce GF, Arruda VR et al (2006) Successful transduction of liver in hemophilia by AAV-Factor IX and limitations imposed by the host immune response. Nat Med 12:342–347. https://doi.org/10.1038/nm1358
George LA, Ragni MV, Rasko JEJ et al (2020) Long-term Follow-Up of the First in Human Intravascular Delivery of AAV for Gene transfer: AAV2-hFIX16 for severe Hemophilia B. Mol Ther J Am Soc Gene Ther 28:2073–2082. https://doi.org/10.1016/j.ymthe.2020.06.001
Saiki RK, Scharf S, Faloona F et al (1985) Enzymatic amplification of beta-globin genomic sequences and restriction site analysis for diagnosis of sickle cell anemia. Science 230:1350–1354. https://doi.org/10.1126/science.2999980
Higuchi R, Fockler C, Dollinger G, Watson R (1993) Kinetic PCR analysis: real-time monitoring of DNA amplification reactions. Biotechnol Nat Publ Co 11:1026–1030. https://doi.org/10.1038/nbt0993-1026
Taylor SC, Laperriere G, Germain H (2017) Droplet Digital PCR versus qPCR for gene expression analysis with low abundant targets: from variable nonsense to publication quality data. Sci Rep 7:2409. https://doi.org/10.1038/s41598-017-02217-x
Greig JA, Nordin JM, Bote E et al (2016) Impact of intravenous infusion time on AAV8 vector pharmacokinetics, safety, and liver transduction in cynomolgus macaques. Mol Ther Methods Clin Dev 3:16079. https://doi.org/10.1038/mtm.2016.79
Gorovits B, Marshall J-C, Smith J et al (2019) Bioanalysis of adeno-associated virus gene therapy therapeutics: regulatory expectations. Bioanalysis 11:2011–2024. https://doi.org/10.4155/bio-2019-0135
Kavita U, Sun K, Braun M et al (2023) PK/PD and bioanalytical considerations of AAV-Based gene therapies: an IQ Consortium industry position paper. AAPS J 25:78. https://doi.org/10.1208/s12248-023-00842-1
Lesko LJ (2021) Perspective on model-informed drug development. CPT Pharmacomet Syst Pharmacol 10:1127–1129. https://doi.org/10.1002/psp4.12699
Sorger PK, Allerheiligen SRB, Abernethy DR et al (2011) Quantitative and Systems Pharmacology in the Post-genomic Era: New Approaches to Discovering Drugs and Understanding Therapeutic. 48
Friedrich CM (2016) A model qualification method for mechanistic physiological QSP models to support model-informed drug development. CPT Pharmacomet Syst Pharmacol 5:43–53. https://doi.org/10.1002/psp4.12056
Kim PS, Lee PP, Levy D (2007) Modeling regulation mechanisms in the immune system. J Theor Biol 246:33–69. https://doi.org/10.1016/j.jtbi.2006.12.012
Wares JR, Crivelli JJ, Yun C-O et al (2015) Treatment strategies for combining immunostimulatory oncolytic virus therapeutics with dendritic cell injections. Math Biosci Eng 12:1237–1256. https://doi.org/10.3934/mbe.2015.12.1237
Gevertz JL, Wares JR (2018) Develo** a minimally structured Mathematical Model of Cancer Treatment with Oncolytic Viruses and dendritic cell injections. Comput Math Methods Med 2018:1–14. https://doi.org/10.1155/2018/8760371
Parra-Guillen ZP, Freshwater T, Cao Y et al (2021) Mechanistic modeling of a Novel Oncolytic Virus, V937, to describe viral kinetic and dynamic processes following Intratumoral and Intravenous Administration. Front Pharmacol 12:705443. https://doi.org/10.3389/fphar.2021.705443
Bonabeau E (2002) Agent-based modeling: methods and techniques for simulating human systems. Proc Natl Acad Sci 99:7280–7287. https://doi.org/10.1073/pnas.082080899
Wang Z, Butner JD, Kerketta R et al (2015) Simulating cancer growth with multiscale agent-based modeling. Semin Cancer Biol 30:70–78. https://doi.org/10.1016/j.semcancer.2014.04.001
Beauchemin C, Forrest S, Koster FT (2006) Modeling influenza viral Dynamics in tissue. In: Bersini H, Carneiro J (eds) Artificial Immune Systems. Springer, Berlin Heidelberg, pp 23–36
Roskos LK, Schneider A, Vainshtein I et al (2011) PK–PD modeling of protein drugs: implications in assay development. Bioanalysis 3:659–675. https://doi.org/10.4155/bio.11.28
Jackson RC (2012) Pharmacodynamic Modelling of Biomarker Data in Oncology. ISRN Pharmacol 2012:. https://doi.org/10.5402/2012/590626
Mok W, Stylianopoulos T, Boucher Y, Jain RK (2009) Mathematical modeling of herpes simplex virus distribution in solid tumors: implications for Cancer Gene Therapy. Clin Cancer Res 15:2352–2360. https://doi.org/10.1158/1078-0432.CCR-08-2082
Lin W, Chen Y, Unadkat JD et al (2022) Applications, Challenges, and Outlook for PBPK modeling and Simulation: A Regulatory, Industrial and Academic Perspective. Pharm Res 39:1701–1731. https://doi.org/10.1007/s11095-022-03274-2
Bussing D, K Shah D (2020) Development of a physiologically-based pharmacokinetic model for ocular disposition of monoclonal antibodies in rabbits. J Pharmacokinet Pharmacodyn 47:597–612. https://doi.org/10.1007/s10928-020-09713-0
Singh AP, Zheng X, Lin-Schmidt X et al (2020) Development of a quantitative relationship between CAR-affinity, antigen abundance, tumor cell depletion and CAR-T cell expansion using a multiscale systems PK-PD model. mAbs 12:1688616. https://doi.org/10.1080/19420862.2019.1688616
Ayyar VS, Song D, Zheng S et al (2021) Minimal physiologically based pharmacokinetic-pharmacodynamic (mPBPK-PD) model of N-Acetylgalactosamine-conjugated small interfering RNA Disposition and Gene silencing in preclinical species and humans. J Pharmacol Exp Ther 379:134–146. https://doi.org/10.1124/jpet.121.000805
Au HKE, Isalan M, Mielcarek M (2021) Gene therapy advances: a Meta-analysis of AAV usage in clinical settings. Front Med 8:809118. https://doi.org/10.3389/fmed.2021.809118
Jones H, Rowland-Yeo K (2013) Basic concepts in physiologically based pharmacokinetic modeling in drug discovery and development. CPT Pharmacomet Syst Pharmacol 2:e63. https://doi.org/10.1038/psp.2013.41
Parra-Guillén ZP, González-Aseguinolaza G, Berraondo P, Trocóniz IF (2010) Gene therapy: a Pharmacokinetic/Pharmacodynamic modelling overview. Pharm Res 27:1487–1497. https://doi.org/10.1007/s11095-010-0136-4
Bonate PL, Van Sant C, Cho K et al (2020) Pharmacokinetics and immunogenicity of ASP0113 in CMV-Seronegative Dialysis patients and CMV-Seronegative and -seropositive healthy subjects. Clin Pharmacol Drug Dev 9:444–455. https://doi.org/10.1002/cpdd.792
Srivastava A (2016) In vivo tissue-tropism of adeno-associated viral vectors. Curr Opin Virol 21:75–80. https://doi.org/10.1016/j.coviro.2016.08.003
Summerford C, Johnson JS, Samulski RJ (2016) AAVR: a multi-serotype receptor for AAV. Mol Ther J Am Soc Gene Ther 24:663–666. https://doi.org/10.1038/mt.2016.49
Chowdhury EA, Meno-Tetang G, Chang HY et al (2021) Current progress and limitations of AAV mediated delivery of protein therapeutic genes and the importance of develo** quantitative pharmacokinetic/pharmacodynamic (PK/PD) models. Adv Drug Deliv Rev 170:214–237. https://doi.org/10.1016/j.addr.2021.01.017
Brown D, Altermatt M, Dobreva T et al (2021) Deep parallel characterization of AAV tropism and AAV-Mediated transcriptional changes via single-cell RNA sequencing. Front Immunol 12:730825. https://doi.org/10.3389/fimmu.2021.730825
Castle MJ, Turunen HT, Vandenberghe LH, Wolfe JH (2016) Controlling AAV Tropism in the Nervous System with Natural and Engineered Capsids. Methods Mol Biol Clifton NJ 1382:133–149. https://doi.org/10.1007/978-1-4939-3271-9_10
Weinberg MS, Nicolson S, Bhatt AP et al (2014) Recombinant adeno-associated virus utilizes cell-specific infectious entry mechanisms. J Virol 88:12472–12484. https://doi.org/10.1128/JVI.01971-14
Nonnenmacher M, Weber T (2011) Adeno-associated virus 2 infection requires endocytosis through the CLIC/GEEC pathway. Cell Host Microbe 10:563–576. https://doi.org/10.1016/j.chom.2011.10.014
Sanlioglu S, Benson PK, Yang J et al (2000) Endocytosis and nuclear trafficking of adeno-associated virus type 2 are controlled by rac1 and phosphatidylinositol-3 kinase activation. J Virol 74:9184–9196. https://doi.org/10.1128/jvi.74.19.9184-9196.2000
Nonnenmacher M, Weber T (2012) Intracellular transport of recombinant adeno-associated virus vectors. Gene Ther 19:649–658. https://doi.org/10.1038/gt.2012.6
Junod SL, Saredy J, Yang W (2021) Nuclear Import of Adeno-Associated Viruses imaged by high-speed single-molecule Microscopy. Viruses 13:167. https://doi.org/10.3390/v13020167
Nonnenmacher ME, Cintrat J-C, Gillet D, Weber T (2015) Syntaxin 5-dependent retrograde transport to the trans-golgi network is required for adeno-associated virus transduction. J Virol 89:1673–1687. https://doi.org/10.1128/JVI.02520-14
Ding W, Zhang L, Yan Z, Engelhardt JF (2005) Intracellular trafficking of adeno-associated viral vectors. Gene Ther 12:873–880. https://doi.org/10.1038/sj.gt.3302527
Liu Y, Joo K-I, Wang P (2013) Endocytic processing of adeno-associated virus type 8 vectors for transduction of target cells. Gene Ther 20:308–317. https://doi.org/10.1038/gt.2012.41
Riyad JM, Weber T (2021) Correction: intracellular trafficking of adeno-associated virus (AAV) vectors: challenges and future directions. Gene Ther 28:771. https://doi.org/10.1038/s41434-021-00252-y
Hui F, Nguyen CTO, He Z et al (2017) Retinal and cortical blood Flow Dynamics following systemic blood-neural barrier disruption. Front Neurosci 11:568. https://doi.org/10.3389/fnins.2017.00568
Bordet T, Behar-Cohen F (2019) Ocular gene therapies in clinical practice: viral vectors and nonviral alternatives. Drug Discov Today 24:1685–1693. https://doi.org/10.1016/j.drudis.2019.05.038
Willett K, Bennett J (2013) Immunology of AAV-Mediated gene transfer in the Eye. Front Immunol 4:261. https://doi.org/10.3389/fimmu.2013.00261
Rodrigues GA, Shalaev E, Karami TK et al (2018) Pharmaceutical Development of AAV-Based gene Therapy Products for the Eye. Pharm Res 36:29. https://doi.org/10.1007/s11095-018-2554-7
Simpson CP, Bolch SN, Zhu P et al (2019) Systemic delivery of genes to retina using Adeno-Associated Viruses. Adv Exp Med Biol 1185:109–112. https://doi.org/10.1007/978-3-030-27378-1_18
Seitz IP, Michalakis S, Wilhelm B et al (2017) Superior Retinal Gene transfer and Biodistribution Profile of Subretinal Versus Intravitreal Delivery of AAV8 in Nonhuman Primates. Investig Opthalmology Vis Sci 58:5792. https://doi.org/10.1167/iovs.17-22473
Ail D, Ren D, Brazhnikova E et al (2022) Systemic and local immune responses to intraocular AAV vector administration in non-human primates. Mol Ther - Methods Clin Dev 24:306–316. https://doi.org/10.1016/j.omtm.2022.01.011
Weber T (2021) Anti-AAV antibodies in AAV Gene Therapy: current Challenges and possible solutions. Front Immunol 12:658399. https://doi.org/10.3389/fimmu.2021.658399
Kruzik A, Fetahagic D, Hartlieb B et al (2019) Prevalence of Anti-Adeno-Associated Virus Immune responses in international cohorts of healthy donors. Mol Ther Methods Clin Dev 14:126–133. https://doi.org/10.1016/j.omtm.2019.05.014
Mingozzi F, High KA (2013) Immune responses to AAV vectors: overcoming barriers to successful gene therapy. Blood 122:23–36. https://doi.org/10.1182/blood-2013-01-306647
Wang J, **e J, Lu H et al (2007) Existence of transient functional double-stranded DNA intermediates during recombinant AAV transduction. Proc Natl Acad Sci U S A 104:13104–13109. https://doi.org/10.1073/pnas.0702778104
Hauck B, Zhao W, High K, **ao W (2004) Intracellular viral processing, not single-stranded DNA accumulation, is crucial for recombinant adeno-associated virus transduction. J Virol 78:13678–13686. https://doi.org/10.1128/JVI.78.24.13678-13686.2004
Penaud-Budloo M, Le Guiner C, Nowrouzi A et al (2008) Adeno-associated virus vector genomes persist as episomal chromatin in primate muscle. J Virol 82:7875–7885. https://doi.org/10.1128/JVI.00649-08
Zhong G, Wang H, He W et al (2020) A reversible RNA on-switch that controls gene expression of AAV-delivered therapeutics in vivo. Nat Biotechnol 38:169–175. https://doi.org/10.1038/s41587-019-0357-y
Taskar KS, Harada I, Alluri RV (2021) Physiologically-based Pharmacokinetic (PBPK) modelling of transporter mediated drug absorption, clearance and drug-drug interactions. Curr Drug Metab 22:523–531. https://doi.org/10.2174/1389200221999210101233340
Singh AP, Krzyzanski W, Martin SW et al (2015) Quantitative prediction of human pharmacokinetics for mAbs exhibiting target-mediated disposition. AAPS J 17:389–399. https://doi.org/10.1208/s12248-014-9690-8
Choi G-W, Lee Y-B, Cho H-Y (2019) Interpretation of Non-Clinical Data for Prediction of Human pharmacokinetic parameters: in Vitro-In vivo extrapolation and allometric scaling. Pharmaceutics 11:168. https://doi.org/10.3390/pharmaceutics11040168
Boutin S, Monteilhet V, Veron P et al (2010) Prevalence of serum IgG and neutralizing factors against adeno-associated virus (AAV) types 1, 2, 5, 6, 8, and 9 in the healthy population: implications for gene therapy using AAV vectors. Hum Gene Ther 21:704–712. https://doi.org/10.1089/hum.2009.182
Merkel SF, Andrews AM, Lutton EM et al (2017) Trafficking of adeno-associated virus vectors across a model of the blood-brain barrier; a comparative study of transcytosis and transduction using primary human brain endothelial cells. J Neurochem 140:216–230. https://doi.org/10.1111/jnc.13861
Pillay S, Meyer NL, Puschnik AS et al (2016) An essential receptor for adeno-associated virus infection. Nature 530:108–112. https://doi.org/10.1038/nature16465
Havlik LP, Das A, Mietzsch M et al (2021) Receptor switching in newly evolved Adeno-associated viruses. J Virol 95:e00587–e00521. https://doi.org/10.1128/JVI.00587-21
Bartlett JS, Wilcher R, Samulski RJ (2000) Infectious entry pathway of adeno-associated virus and adeno-associated virus vectors. J Virol 74:2777–2785. https://doi.org/10.1128/jvi.74.6.2777-2785.2000
Stahnke S, Lux K, Uhrig S et al (2011) Intrinsic phospholipase A2 activity of adeno-associated virus is involved in endosomal escape of incoming particles. Virology 409:77–83. https://doi.org/10.1016/j.virol.2010.09.025
Johnson JS, Gentzsch M, Zhang L et al (2011) AAV exploits subcellular stress Associated with inflammation, endoplasmic reticulum expansion, and misfolded proteins in models of cystic fibrosis. PLoS Pathog 7:e1002053. https://doi.org/10.1371/journal.ppat.1002053
Sonntag F, Bleker S, Leuchs B et al (2006) Adeno-Associated Virus type 2 capsids with externalized VP1/VP2 trafficking domains are generated prior to passage through the cytoplasm and are maintained until uncoating occurs in the Nucleus. J Virol 80:11040–11054. https://doi.org/10.1128/JVI.01056-06
Sidaway-Lee K, Costa MJ, Rand DA et al (2014) Direct measurement of transcription rates reveals multiple mechanisms for configuration of the Arabidopsis ambient temperature response. Genome Biol 15:R45. https://doi.org/10.1186/gb-2014-15-3-r45
Lefaudeux D, Sen S, Jiang K et al (2022) Kinetics of mRNA nuclear export regulate innate immune response gene expression. Nat Commun 13:7197. https://doi.org/10.1038/s41467-022-34635-5
Metelev M, Lundin E, Volkov IL et al (2022) Direct measurements of mRNA translation kinetics in living cells. Nat Commun 13:1852. https://doi.org/10.1038/s41467-022-29515-x
Monahan PE, Sun J, Gui T et al (2015) Employing a gain-of-function factor IX variant R338L to advance the efficacy and safety of hemophilia B human gene therapy: preclinical evaluation supporting an ongoing adeno-associated virus clinical trial. Hum Gene Ther 26:69–81. https://doi.org/10.1089/hum.2014.106
Nathwani AC, Reiss UM, Tuddenham EGD et al (2014) Long-term safety and efficacy of factor IX gene therapy in Hemophilia B. N Engl J Med 371:1994–2004. https://doi.org/10.1056/NEJMoa1407309
Author information
Authors and Affiliations
Contributions
All authors wrote and reviewed the manuscript. All figures were made by the authors or are creative commons images.
Corresponding author
Ethics declarations
Competing interests
All authors are employees of Astellas, which own Astellas Gene Therapy, a gene therapy company.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choules, M.P., Bonate, P.L., Heo, N. et al. Prospective approaches to gene therapy computational modeling – spotlight on viral gene therapy. J Pharmacokinet Pharmacodyn (2023). https://doi.org/10.1007/s10928-023-09889-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10928-023-09889-1